Abstract
Background The carpal boss is an osseous protuberance occurring variably along the dorsum of the second or third metacarpal base, lacking a standardized definition.
Aim We sought to characterize the dorsal second and third carpometacarpal joints in the general population on computed tomography (CT) to better define this variant anatomy.
Patients and Methods A total of 129 wrist CT studies were reviewed. Note was made of the dorsal second/third carpometacarpal osseous anatomy, the presence of regional bursitis or tenosynovitis, and relationship of the extensor carpi radialis brevis attachment to the base of the third metacarpal.
Results Out of the 129 wrists, 106 (82.2%) demonstrated a dorsal protuberance arising from the base of the third metacarpal, in isolation. Out of the 129 wrists, 14 (10.9%) lacked a dorsal protuberance or nonunited ossicle at the level of the second or third carpometacarpal joint. Out of the 129 wrists, 9 (7%) wrists demonstrated more complex anatomy—8 wrists (6.2%) with a dorsal protuberance at the base of the third metacarpal seen in combination with an adjacent nonunited ossicle and/or dorsal protuberance arising from the capitate, and 1 wrist (0.8%) with an isolated ossicle at the base of the third metacarpal. Of these nine wrists, eight (6.2%) demonstrated arthritis at the resultant pseudoarticulation(s).
Conclusion The majority of wrists demonstrated an isolated protuberance arising from the dorsal base of the third metacarpal, with a small minority with a nonunited ossicle at this level and/or dorsal protuberance of the capitate. The presence of secondary arthritis (8 out of 129 wrists, 6.2%) may reflect a pain generator.
Level of Evidence Cross-sectional study; level 2.
Keywords: carpal boss, os styloideum, computed tomography, wrist, carpometacarpal joints
There are a variety of causes of dorsal wrist pain that may present a diagnostic dilemma for clinicians. When pain is accompanied by the presence of a dorsal wrist mass, the carpal boss should be considered a potential cause.
The carpal boss has been most frequently described as an osseous protuberance along the dorsal base of the second or third metacarpal, with variable involvement of the adjacent trapezoid or capitate, respectively.1 2 3 4 5 In the orthopedic and radiology literature, the pathogenesis is reportedly uncertain, with multiple theories, including sequela of trauma, osteoarthritis, chronic remodeling of the bone related to extensor carpi radialis brevis (ECRB) attachment (when the abnormality occurs at the base of the third metacarpal), exostosis, coalition, accessory capitate bone, or accessory ossicle at the dorsal quadrangular trapezoid–capitate–metacarpal joint termed an “os styloideum” or ninth carpal bone.1 2 3 4 5 6 7 8 9 10 11 12 13
The carpal boss can be asymptomatic and incidental, or a potential cause of dorsal wrist pain with a palpable mass. Purported causes of pain attributable to the carpal boss include altered biomechanics, extensor tendon irritation/tenosynovitis (ECRB or extensor carpi radialis longus), irritation following trauma or repetitive use, and secondary arthritis. Additionally, the formation of an adventitial bursitis has been implicated.1 6 7 9 12 13
Both cadaveric and radiographic studies have attempted to elucidate the characteristics and occurrence of the carpal boss. However, a universal flaw in determining the occurrence of this entity lies in the fact that there is no standardized definition of what constitutes a carpal boss. This at least in part explains the disparate reported rates of carpal boss ranging from 1 to 19% in the orthopedic and radiology literature.1 14 15
Through review of a series of computed tomography (CT) studies of the wrist, the purpose of our study was to:
Qualitatively and quantitatively assess the spectrum of anatomy of the dorsal wrist at the level of the second and third carpometacarpal (CMC) joints in the general population.
Identify specific features, if any, suggestive of a symptomatic “carpal boss,” including potential features of arthritis at the level of the osseous protuberance, or soft tissue changes that may generate pain, including tenosynovitis of the regional extensor tendons or adventitial bursal formation.
Finally, we sought to characterize the relationship of the adjacent extensor tendon when a dorsal protuberance was identified at the third metacarpal base, as chronic remodeling related to ECRB attachment has been cited as a proposed etiology of the osseous disorder.2 7 9
Materials and Methods
This study was approved by the Investigational Review Board at the University of Washington.
Clario Zvision (version 1.4.80, Seattle, WA) was used to identify noncontrast-enhanced CT scans of the wrist performed within the University of Washington medical system during March 1, 2014 to January 1, 2015. A total of 163 wrist CT studies were identified, which included both single (155 studies) and bilateral wrist CTs (8 studies), for a total of 171 wrists. CT technique included 1.25 to 2.5 mm axial slices with 1.25 to 2.5 mm coronal and sagittal reformatted imaging. All CT studies were performed on one of three CT systems, including a General Electric (GE) Medical Systems Discovery CT750 HD, GE Medical Systems Lightspeed VCT (GE Corporate Headquarters, Fairfield, CT), and Siemens SOMATOM Definition AS (Siemens Medical Solutions USA, Inc., Malvern, PA).
Exclusion criteria included patients who were under the age of 18 at the time of the examination, repeat/follow-up examinations of the same wrist performed during the study time frame, or any factor that prohibited effective and standardized evaluation of the unaltered second or third CMC joints. The latter included examinations with hardware obscuring the second or third CMC joints, fractures involving the carpal or metacarpal bones at the level of the second and third CMC joints, inadequate sagittal and/or coronal reformatted imaging, examinations optimized for the forearm rather than the wrist, studies performed at outside institutions, and the presence of severe imaging artifact. Inclusion and exclusion data were tabulated, and presented by way of flowchart (Fig. 1).
Fig. 1.
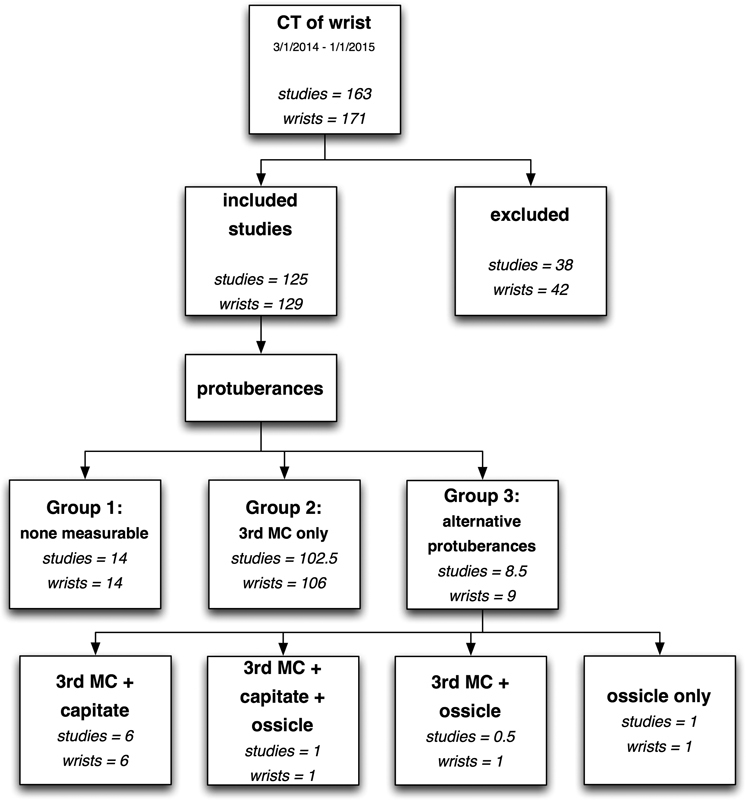
Inclusion and exclusion flowchart.
In total, 38 CT studies were excluded. Of these excluded studies, 4 were bilateral wrist CTs, resulting in 42 total wrists excluded from the evaluation. After exclusions, this yielded a total of 125 CT studies, 4 of which were bilateral, for a total of 129 wrists (Table 1).
Table 1. Studies/wrists excluded and cause of exclusion.
| Exclusions | ||
|---|---|---|
| Reason | Studies | Wrists |
| Under 18 | 5 | 6 |
| Repeated scans | 8 | 8 |
| Obscuring hardware | 5 | 5 |
| Limited resolution | 2 | 2 |
| Obscuring fractures | 4 | 4 |
| Severe arthritis | 1 | 1 |
| Unavailable images | 3 | 3 |
| Inadequate reformats | 3 | 6 |
| Outside hospital imaging | 2 | 2 |
| Obscuring artifact | 1 | 1 |
| Carpal fusions | 4 | 4 |
| Total | 38 | 42 |
In a consensus fashion, the 129 wrist CTs were evaluated by a fellowship trained musculoskeletal radiologist (J. P.) and a postgraduate year 4 radiology resident (C. G.).
Imaging indication, patient age, gender, and wrist side were recorded on all CT studies evaluated following exclusions. All three planes on a GE Centricity Picture Archiving and Communication System (PACS, GE Healthcare, Barrington, IL) workstation were utilized for the qualitative and quantitative assessment of the dorsal second and third CMC joints.
First, the general morphology of the base of the second and third CMC joints was qualitatively assessed. If a dorsal protuberance was present at either the second or third metacarpal base that extended both dorsally and proximally to the remainder of the metacarpal base, and was also measureable in all three planes, this structure was quantified. Specifically, measurements of the dorsal protuberance obtained in the axial plane were acquired on the first image of the protuberance identifiable in which there was no continuity of the protuberance with the adjacent metacarpal base, scrolling from distal to proximal through the affected metacarpal. An estimate of the maximal anteroposterior (AP) and coronal length of the protuberance was obtained by drawing lines parallel to the deep cortices of the triangular-shaped protuberance in the axial plane (Fig. 2).
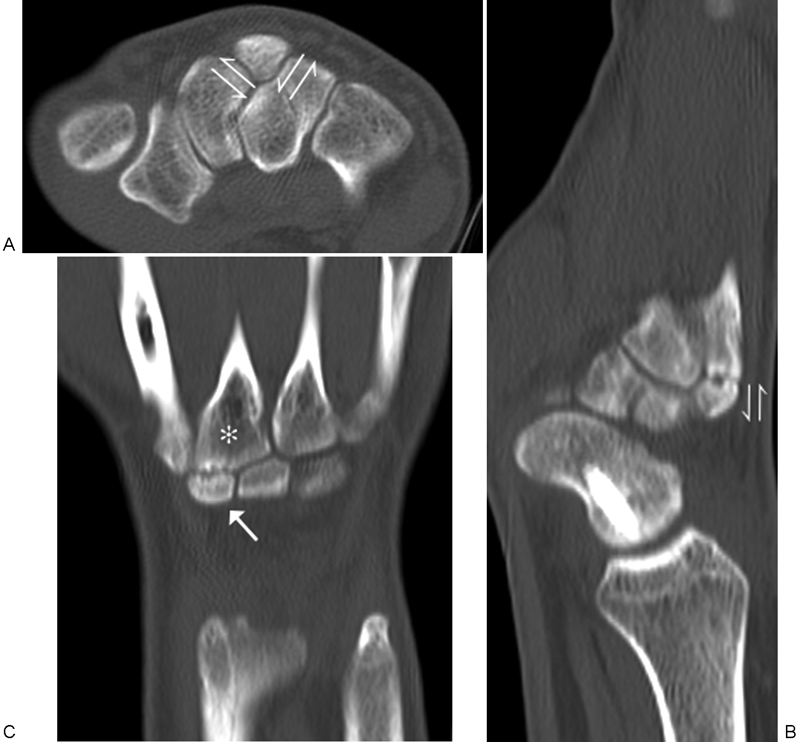
Fig. 2.

A 51-year-old man with left-sided distal radius fracture and CT study acquired for preoperative planning. Axial (A) and sagittal (B) unenhanced CT imaging at the level of the base of the third metacarpal demonstrates the technique used to acquire a relative volume of the dorsal protuberance. An estimate of the AP and coronal length was obtained from the axial plane (A; harpoon arrows), while CC length was acquired from the center of the protuberance in the sagittal plane (B; harpoon arrows designate length; straight arrow designates interface of sclerosis within the protuberance and the adjacent medullary bone). AP, anteroposterior; CC, craniocaudal; CT, computed tomography.
To obtain an estimate of maximal craniocaudal (CC) length, the center of the protuberance was identified on the axial image used during transverse measurement acquisition, and the “cross reference” feature within PACS was then used to localize the central portion of the dorsal protuberance on sagittal imaging. The CC length was measured by drawing the longest line extending from the proximal tip of the protuberance to the most distal region of sclerosis associated with the protuberance, which often reflected a clear demarcation of protuberance from remaining metacarpal medullary bone. When a well-defined sclerotic protuberance was not present, the CC line was drawn as the longest line extending from the proximal tip of the protuberance to the estimated distal margin of the protuberance, based on adjacent metacarpal base morphology (Fig. 2).
Subsequently, the product of these three measurements was tabulated to achieve an estimate of size. A true volume was not estimated secondary to the inconsistent and irregular morphology of these protuberances. Attaining the product of the three orthogonal measurements enabled a generic assessment of size for relative comparisons. An absolute volume should not be inferred from these data, however.
In a similar fashion, any separate ossicles that were identified at the dorsal, second or third CMC joint were measured in three planes using the axial and sagittal reformatted imaging. Using the axial images, an estimate of the maximal AP and coronal measurements were obtained utilizing the two largest orthogonal measurements. To obtain an estimate of maximal CC length, the center of the ossicle was identified on the axial image used during transverse measurement acquisition, and the “cross reference” feature within PACS was then used to localize the central portion of the ossicle on sagittal imaging, where an estimate of the maximal CC length was acquired (Fig. 3). The product of these three measurements was tabulated to determine an estimate of size for relative comparisons.
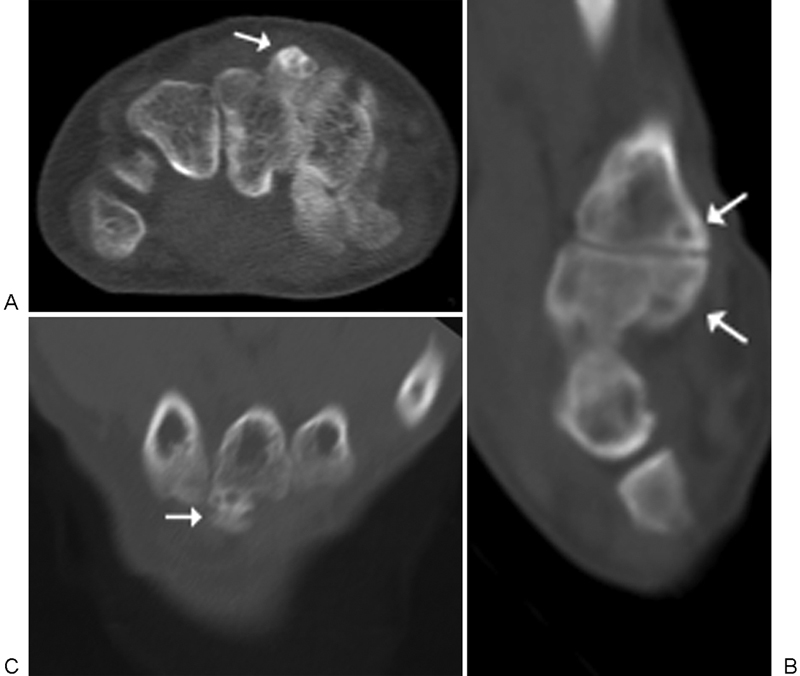
Fig. 3.
A 22-year-old man with CT study obtained to assess healing of a scaphoid fracture. Axial (A) and sagittal (B) unenhanced CT imaging at the level of a nonunited ossicle (arrow) below the dorsal base of the third metacarpal (star). An estimate of the AP and coronal length was obtained from the axial plane (A; harpoon arrows), while CC length was acquired from the center of the protuberance in the sagittal plane (B; harpoon arrows). Coronal image (C) demonstrates the relationship of the ossicle with the dorsal base of the third metacarpal. AP, anteroposterior; CC, craniocaudal; CT, computed tomography.
When present, a protuberance arising from the trapezoid or capitate was also examined and measured in three planes. The largest cross section of the carpal bone protuberance was identified in the axial plane and measured using the two largest orthogonal measurements in an effort to obtain an estimate of the maximal AP and coronal dimensions. Again, to obtain an estimate of maximal CC length, the center of the carpal protuberance was identified on the axial image used during transverse measurement acquisition, and the “cross reference” feature within PACS was then used to localize the central portion of the carpal protuberance on sagittal imaging, where an estimate of the maximal CC length was acquired (Fig. 4). The product of these three measurements was tabulated to determine an estimate of size for relative comparisons.
Fig. 4.

A 20-year-old man with left-sided scaphoid and capitate fractures related to football injury. Axial (A) and sagittal (B) unenhanced CT imaging at the level of a dorsal protuberance arising from the capitate (star). An estimate of the AP and coronal length was obtained from the axial plane (A; harpoon arrows), while CC length was acquired from the center of the protuberance in the sagittal plane (B; harpoon arrows). AP, anteroposterior; CC, craniocaudal; CT, computed tomography.
For analysis purposes, each wrist was classified into one of three predefined groups based on findings:
Group 1: No measurable dorsal protuberance at the base of the second or third metacarpal, no separate dorsal ossicle at the second or third CMC joint, and no dorsal protuberance arising from the trapezoid or capitate.
Group 2: A measurable dorsal protuberance arising from the second and/or third metacarpal base, in isolation.
-
Group 3:
Any wrist with a dorsal protuberance at the base of the second and/or third metacarpal seen in combination with an adjacent separate nonunited dorsal ossicle and/or dorsal protuberance from the trapezium and/or capitate.
Any wrist with a separate nonunited ossicle at the dorsum of the second or third CMC joint.
Any wrist with a trapezoid and/or capitate dorsal protuberance, in isolation.
Additional findings that were interrogated and tabulated included the location of the insertion of the ECRB, the presence or absence of a dorsal wrist ganglion/regional adventitial bursa, and the presence or absence of extensor tendon tenosynovitis.
An unpaired t-test was used to assess differences between two groups. A general linear model was used to assess differences in age among multiple study groups. Contingency tables and the chi-square were used to assess associations among categorical variables. Logistic regression was used to assess associations between categorical and numeric variables.
All statistical calculations were performed using the R language and environment for statistical computing.16
Results
Of the 129 wrists studied (from 125 patients), none were ordered for the purposes of evaluating a dorsal wrist mass, carpal boss, ganglion, or any history suggestive of “carpal boss.” The overwhelming majority of studies were obtained for fracture evaluation or fracture follow-up, which included 117 of 129 (90.7%) wrists. Of the 129 wrists, 4 (3.1%) wrist CTs were obtained to evaluate arthritis, 5/129 (3.9%) to evaluate nonspecific wrist pain, and 2/129 (1.6%) for follow-up of previously performed arthroplasty. Finally, a single wrist CT (1/129, 0.8%) was performed to evaluate for soft tissue infection.
The median age was 43.3 years with a range of 18.4 to 85 years. There were 88/125 (70.4%) male patients, and 37/125 (29.6%) female patients. Finally, for the 125 patients (including four bilateral wrist CTs) there were a total of 129 wrists, divided into 67 right wrists, and 62 left wrists.
Group 1
Of the 129 wrists, 14 wrists (10.9%) from 14/125 patients were classified into group one (Fig. 5). Of the 14 patients in group 1, the median age was 46.6 years with a range of 22.7 to 71.8 years. Of the 14 wrists, 12 (85.8%) belonged to males and 2/14 (14.3%) to females. There were eight (57.1%) right wrists and six (42.9%) left wrists.
Fig. 5.
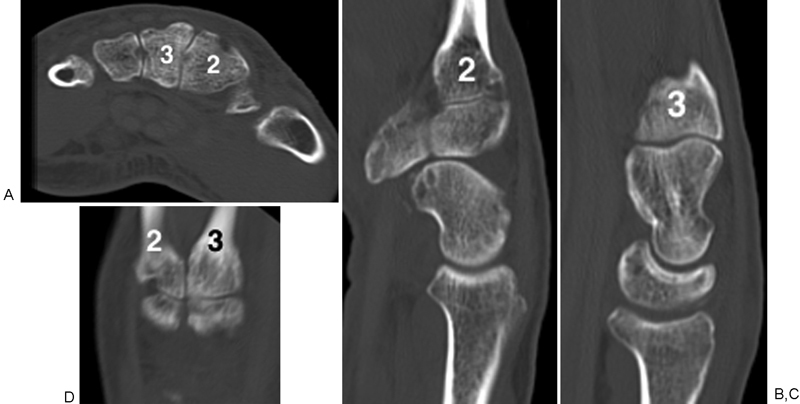
A 71-year-old man with right-sided pisiform and triquetral fractures following ground level fall. Axial (A), sagittal (B and C), and coronal (D) unenhanced CT imaging at the level of the base of the second and third CMC joints. There is no measurable dorsal protuberance at the base of the second or third metacarpal, no separate dorsal ossicle at the second or third CMC joint, and no dorsal protuberance arising from the trapezoid or capitate. (2 = 2nd metacarpal; 3 = 3rd metacarpal). CMC, carpometacarpal; CT, computed tomography.
None of the 14 wrists within group one demonstrated a dorsal wrist ganglion/regional adventitial bursitis, nor tenosynovitis. In all of the 14 wrists, the ECRB attached to the base of the third metacarpal along the dorsal, radial margin.
Group 2
Of the 129 wrists, 106 wrists (82.2%) from 103/125 patients were categorized into group two. Although the intention was to identify those with a measurable dorsal protuberance at either the second or third metacarpal base for group 2, all of the wrists within this category constituted a dorsal protuberance arising solely from the third metacarpal base (Fig. 2). Of the 103 patients in group 2, the median age was 40.9 years with a range of 18.4 to 85.0 years. Of the 106 wrists, 70 (66%) belonged to males, while 36/106 (34%) belonged to females. There were 54/106 (41.9%) right wrists and 52/106 (40.3%) left wrists.
None of the 106 wrists demonstrated findings compatible with a dorsal wrist ganglion/regional adventitial bursa. Findings of tenosynovitis were demonstrated in 17/106 (16%) wrists. In each of these 17 instances, there were concomitant fractures about the wrist, presumably the cause of the tenosynovitis. In all 106 wrists, the ECRB tendon attached to the proximal third metacarpal along the dorsal and the radial margin of the protuberance (Fig. 6).
Fig. 6.
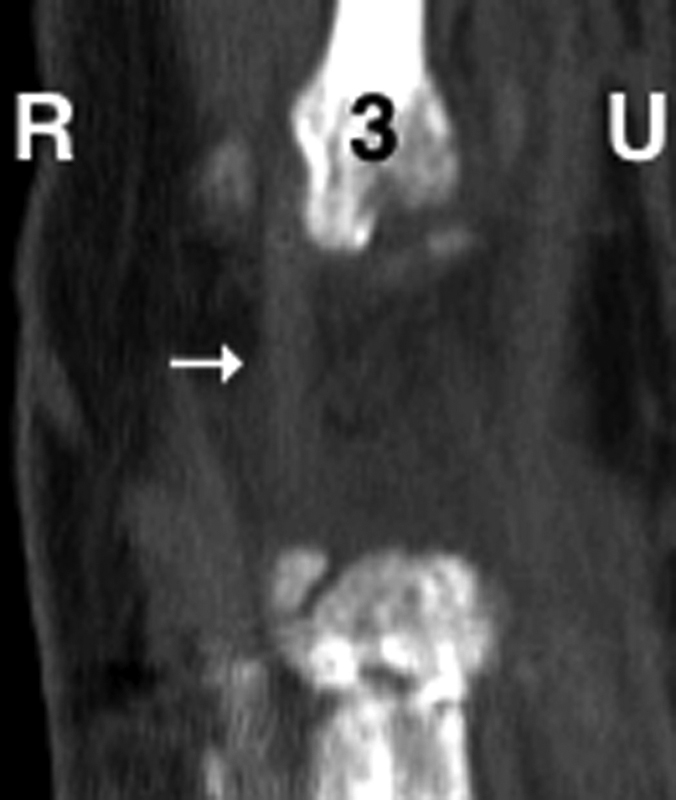
A 65-year-old woman with left-sided distal radius fracture following open reduction and internal fixation. Coronal unenhanced CT image at the dorsal base of the third metacarpal demonstrates attachment of the ECRB (arrow) to the radial and dorsal margins about the protuberance. (R = radial side; U = ulnar side; 3 = 3rd metacarpal). CT, computed tomography; ECRB, extensor carpi radialis brevis.
Group 3
Of the 129 wrists, 9 wrists (7%) from 9/125 patients were categorized into group 3. Of the nine wrists within group 3, seven out of nine (77.8%) demonstrated a dorsal protuberance from the base of the third metacarpal with an adjacent protuberance from the capitate, forming a pseudoarticulation (Fig. 7). One of these seven wrists demonstrated an interposed nonunited ossicle at the pseudoarticulation (Fig. 8). Six of these seven wrists demonstrated variable degrees of cortical irregularity, subcortical sclerosis, and subcortical cystic change at the pseudoarticulation suggestive of secondary arthritis.
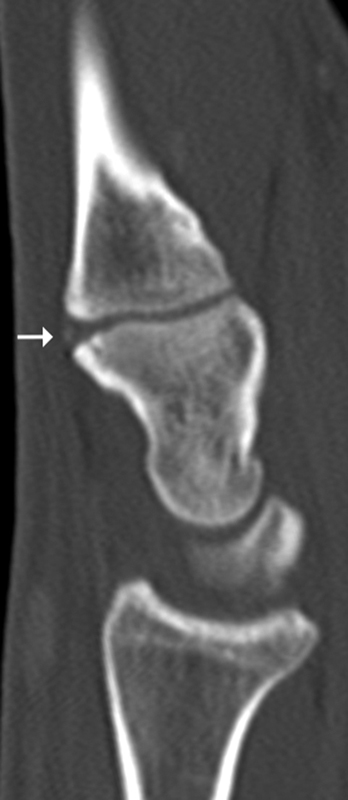
Fig. 7.
A 53-year-old man with left-sided distal radius fracture. Axial (A), sagittal (B), and coronal (C) unenhanced computed tomography images at the third carpometacarpal joint demonstrate a dorsal protuberance from the base of the third metacarpal with an adjacent protuberance from the capitate, forming a pseudoarticulation. Changes suggestive of secondary arthritis are present (arrows).
Fig. 8.
A 38-year-old man with left-sided wrist abscess. Sagittal unenhanced computed tomography image at the third carpometacarpal joint demonstrates a dorsal protuberance from the base of the third metacarpal with an adjacent protuberance from the capitate, and with an intervening ossicle (arrow).
One of nine (11.1%) wrists in group 3 demonstrated a prominent nonunited ossicle adjacent to a dorsal third metacarpal base protuberance (Fig. 9). Finally, one of nine (11.1%) wrists within group 3 demonstrated an isolated nonunited ossicle situated along the dorsal aspect of the third CMC joint (Fig. 3). Both of these wrists demonstrated cortical irregularity, subcortical sclerosis, and subcortical cystic change at the pseudoarticulations suggestive of secondary arthritis.
Fig. 9.
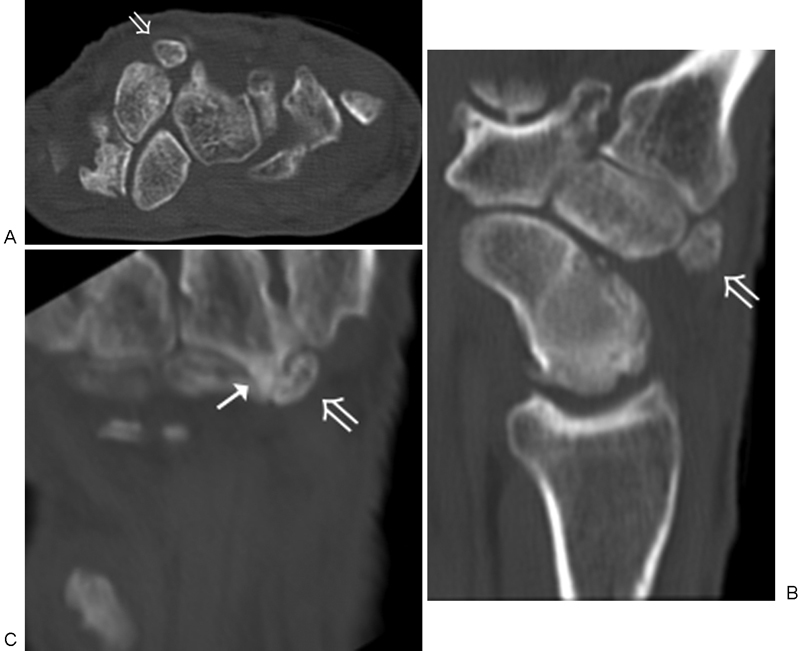
A 65-year-old man with CT study obtained to assess bilateral wrist osteoarthritis. Axial (A), sagittal (B), and coronal (C) unenhanced CT images at the third carpometacarpal joint demonstrate a dorsal protuberance from the base of the third metacarpal (arrow) with an adjacent nonunited ossicle (open arrow). CT, computed tomography.
Of the nine patients in group 3, the median age was 38.7 years with a range of 21.0 to 65.7 years. Eight of the nine (88.9%) wrists belonged to males, while one out of nine (11.1%) belonged to female. Of the nine wrists, five were (55.6%) right wrists and four were (44.4%) left wrists.
None within group 3 demonstrated CT evidence of a dorsal wrist ganglion/regional adventitial bursitis. Only one of the nine (11.1%) wrists within group 3 demonstrated extensor tenosynovitis, however, this involved the first through the third extensor compartment and was seen in combination with severe osteoarthritis throughout the wrist, and presumably not attributable to the presence of dorsal changes about the third CMC joint. In all nine wrists, the ECRB tendon attached to the proximal third metacarpal along the radial and dorsal margin of the protuberance.
Notably, seven of the nine wrist CTs in group 3 were obtained for fracture, while the remaining two wrist CTs were obtained for infection (cellulitis with abscess) and evaluation of arthritis.
Summary
Studies and wrists stratified into the three groups are summarized in Table 2. Relative size of seven capitate protuberances was 101.6 mm3. Relative size of 114 third metacarpal protuberances was 106.3 mm3. These relative sizes are not statistically significantly different (p = 0.48) (Fig. 10).
Table 2. Inclusion data subdivided by group.
| Subgroup analysis | Studies | Wrists | Percent wrists |
|---|---|---|---|
| Group 1 | 14 | 14 | 10.9 |
| Group 2 | 103a | 106 | 82.2 |
| Group 3 | 9a | 9 | 7 |
| Total evaluated | 125 | 129 | 100 |
One bilateral wrist computed tomography is included in both group 2 (right wrist) and group 3 (left wrist).
Fig. 10.
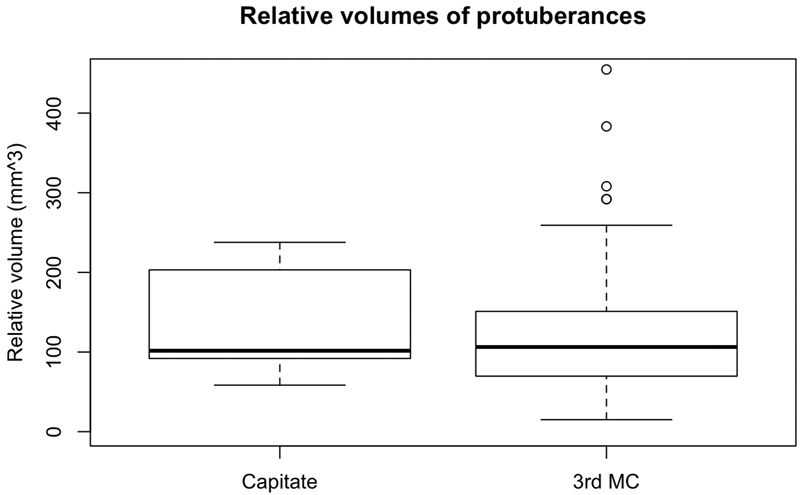
Relative sizes of protuberances from 7 capitates and 114 third metacarpals.
There was no statistically significant difference in age among the three protuberance groups (p = 0.46) (Fig. 11). There was no statistically significant association between sidedness and the three protuberance groups (p = 0.88). There was no statistically significant association between gender and the three protuberance groups (p = 0.14).
Fig. 11.
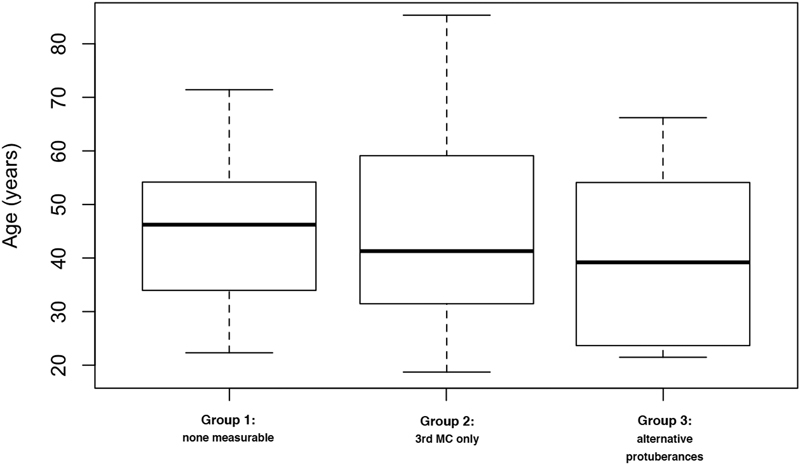
Boxplot for age for three groups.
Women in this study are statistically significantly older than the men (p = 0.00006) (Fig. 12).
Fig. 12.
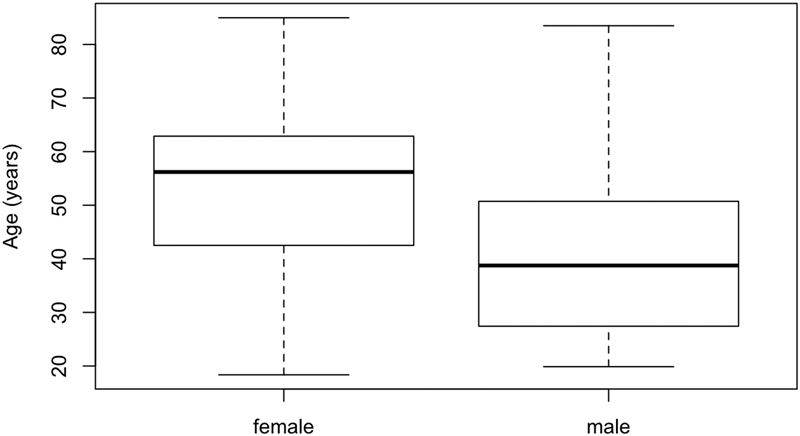
Boxplot of age differences between women and men in this study.
Logistic regression showed that neither gender, third metacarpal protuberance, capitate protuberance, ossicular presence, third metacarpal attachment of ECRB, tenosynovitis, or age were statistically significant predictors of arthritis at a pseudoarticulation formed by osseous protuberances at the dorsal third CMC joint. Likewise, neither gender, third metacarpal protuberance, capitate protuberance, ossicular presence, third metacarpal attachment of ECRB, arthritis at a pseudoarticulation formed by osseous protuberances at the dorsal third CMC joint, or age were statistically significant predictors of tenosynovitis.
Discussion
The lack of a standardized definition of what constitutes a carpal boss at least in part contributes to widely disparate occurrence rates reported in the orthopedic and radiology literature, ranging from 1 to 19%. For example, a review by Bassoe and Bassoe in 1955 reported a 1.3% occurrence of an “os styloideum” by radiography, in which the authors searched specifically for a nonunited separate ossicle within the region of the dorsal second or third CMC joint.14 More recent cadaveric studies quote rates of “partial osseous coalition” involving the second or third CMC joint, used interchangeably with carpal boss in the articles, of 18 to 19%.1 15 Notably, the aforementioned cadaveric studies report a relatively frequent “partial osseous coalition” at the second CMC joint. Conversely, of the 129 wrists that we reviewed, none exhibited a measurable dorsal protuberance arising from the base of the second metacarpal, nor the dorsum of the trapezoid. The exact explanation for the paucity of findings at the second CMC joint in our study relative to the cadaveric studies referenced is not clear, but once again highlights the necessity for a more refined and standardized definition of a carpal boss.
Because no explicit definition of the carpal boss currently exists, rather than attempt to provide a specific occurrence based on our CT analysis, we instead sought to describe findings at the dorsal base of the second and third CMC joint in a general population, and identify potential features that may contribute to symptomatology when an osseous protuberance is present.
Each wrist CT evaluated was categorized into one of three groups. Group 1 reflected those with no changes along the dorsum of the second or third CMC joint to suggest a carpal boss. There were 14 out of 129 wrists (10.9%) within this group, from a total of 14 out of 125 patients (11.2%).
Group 2 comprised the vast majority of the wrists; specifically, 106 of 129 wrists (82.2%) from a total of 103 out of 125 patients (82.4%). All CT wrist studies within this group demonstrated a measurable protuberance arising from the third metacarpal base, but without additional findings of a separate nonunited ossicle, or protuberance from adjacent carpal bones. Although our intention was to also classify those with an isolated dorsal protuberance arising from the second metacarpal base into this group based on previous reports suggesting “bossing” within this region as well, there were surprisingly no wrist CT studies with an isolated measurable dorsal protuberance at the second CMC joint.
Finally, group 3 was intended for wrist CT studies with more elaborate findings at the dorsal second or third CMC joint than those categorized into group 2, as detailed in our Methods section. Group 3 comprised a minority of wrists, representing 9 of the 129 wrists (7%) studied, and 9 of the total 125 patients (7.2%). Although none of the wrists within group 3 demonstrated a solid dorsal osseous fusion, in eight of nine, there were variable degrees of irregular appearing subcortical sclerosis and cystic change at the site(s) of narrow pseudoarticulation formed by the presence of osseous protuberances arising from the base of the third metacarpal and/or adjacent capitate, and/or the presence of a nonunited ossicle within this region. It is conceivable that irregularity seen about these pseudoarticulations within these eight wrists reflects changes capable of explaining symptoms in the context of a “carpal boss,” as arthritis has been implicated as a potential source of pain with “bossing.”
Also of note, of the 9 wrists within group 3, 3/129 (2.3%) wrists from 3/125 (2.4%) patients demonstrated a separate nonunited ossicle, a similar rate of occurrence to that reported by Bassoe and Bassoe of the “os styloideum” (1.3%).
While the etiology underlying the carpal boss appears uncertain in the medical literature, a more broad review of the biomedical literature, with specific attention paid to anatomical journals, suggests findings along the dorsum of the second and the third CMC joint are rather predictable and easily explained. In 2013, Ward et al provided a detailed description of the third metacarpal base dorsal “styloid process,” a reportedly well-known distinctive feature of modern human and Neanderthal hands, present in approximately 90% of modern humans at the dorsal base of the third metacarpal.17 The authors state that this styloid process develops from a separate ossification center at the dorsoradial corner of the third metacarpal base, occasionally fusing to the capitate (3.5%) or trapezoid (0.5%), or present as a separate ossicle (2%).17 Although we failed to demonstrate a complete osseous fusion with the capitate or trapezoid, in 7/129 (5.4%) wrists from 7/125 (5.6%) patients, a narrow pseudoarticulation existed at the dorsum of the third CMC joint, with contributions arising from both the third metacarpal base and the capitate, a very similar occurrence rate to that reported by the authors for those with dorsal fusion. Finally, 3/129 (2.3%) wrists from 3/125 (2.4%) patients exhibited a nonunited ossicle within this region in our study, which reflects a very similar occurrence to that reported by Ward et al (2%).17 Thus, our results utilizing CT mirror those in the anatomical and anthropological literature.
The clinical literature also suggests a potential role of the ECRB in producing bony changes at its attachment to the dorsal third metacarpal base.2 7 9 However, we have demonstrated a consistent anatomical relationship of the ECRB attachment to the base of the third metacarpal, always occurring along the radial margin, within all three groups of wrists analyzed. Specifically, the attachment was similar in those with and without a dorsal third metacarpal base protuberance, and as such, the pathophysiological role of the ECRB in producing an osseous excrescence at this location may not be valid.
In addressing symptomatic instances of carpal boss, the clinical literature suggests that the bony prominence may induce dorsal ganglion/regional adventitial bursal formation and/or tenosynovitis.1 6 7 9 12 13 In our evaluation of the soft tissues of the dorsal wrist, however, we found 0/129 (0%) instances with a dorsal wrist ganglion/regional adventitial bursa at the second or third CMC joint. While 18/129 (14.0%) wrists from 18/125 (14.4%) patients demonstrated tenosynovitis, in all but one instance (with significant osteoarthritis involving the wrist), these findings were most likely related to the presence of concomitant fractures. While we failed to demonstrate dorsal wrist ganglia/regional adventitial bursitis in the context of a dorsal protuberance, none of the CT studies obtained for our study were for an indication suggestive of a potential painful carpal boss. As such, the lack of these findings neither supports nor disputes the theory that such soft tissue abnormalities may serve as a cause of pain in those with a “carpal boss.”
Our study is limited by heterogeneity in CT acquisition protocol (slice thickness disparity ranging from 1.25 to 2.5 mm), which could lead to measurement bias. Additionally, no CT examinations performed in our study were for an indication of a painful dorsal wrist mass, limiting the assessment for potential causes of pain in the context of a “carpal boss.” Finally, while magnetic resonance imaging could have provided enhanced soft tissue detail with regards to extensor tendon attachment along the dorsum of the third CMC joint, one was not readily available to review for each CT inspected.
We examined the dorsum of the second and third CMC joints utilizing CT from a general population, none of which with a history suggestive of dorsal wrist pain or carpal boss, in an effort to further define the varied anatomy within this region. The overwhelming majority of the wrists examined (82.2%) demonstrated a dorsal protuberance arising from the base of the third metacarpal that is readily measurable on CT. A minority of the wrists 14/129 (10.9%) had no measurable dorsal protuberance at either the second or third CMC joint, while an even smaller subset of our population, 8/129 (6.2%) of the wrists from 8/125 (6.4%) patients exhibited arthritis at the pseudoarticulation formed by protuberances at the dorsal third CMC joint, a possible cause of dorsal wrist pain with a palpable mass attributable to a “carpal boss” based on prior reports. Interestingly, our osseous findings are consistent with those reported in the anatomical literature, where features along the dorsal aspect of the second and third CMC joints are attributed to a well-defined embryological explanation. The influence of alternative causes of “carpal bossing” previously proposed, such as trauma for instance, remains uncertain.
Footnotes
Ethical Review Committee Statement This study was approved by the Institutional Review Board at the University of Washington. Conflict of Interest None.
References
- 1.Alemohammad A M, Nakamura K, El-Sheneway M, Viegas S F. Incidence of carpal boss and osseous coalition: an anatomic study. J Hand Surg Am. 2009;34(1):1–6. doi: 10.1016/j.jhsa.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 2.Boggess B, Berkoff D. Dorsal wrist mass: The carpal boss. BMJ Case Rep. 2011 doi: 10.1136/bcr.01.2011.3695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Capo J T, Orillaza N S, Lim P K. Carpal boss in an adolescent: case report. J Hand Surg Am. 2009;34(10):1808–1810. doi: 10.1016/j.jhsa.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 4.Clarke A M, Wheen D J, Visvanathan S, Herbert T J, Conolly W B. The symptomatic carpal boss. Is simple excision enough? J Hand Surg [Br] 1999;24(5):591–595. doi: 10.1054/jhsb.1999.0238. [DOI] [PubMed] [Google Scholar]
- 5.Keupers M, Gelin G, Vandevenne J, Grieten M. Carpal boss syndrome. JBR-BTR. 2012;95(5):320–321. doi: 10.5334/jbr-btr.678. [DOI] [PubMed] [Google Scholar]
- 6.Conway W F, Destouet J M, Gilula L A, Bellinghausen H W, Weeks P M. The carpal boss: an overview of radiographic evaluation. Radiology. 1985;156(1):29–31. doi: 10.1148/radiology.156.1.3923555. [DOI] [PubMed] [Google Scholar]
- 7.Kissel P. Conservative management of symptomatic Carpal Bossing in an elite hockey player: a case report. J Can Chiropr Assoc. 2009;53(4):282–289. [PMC free article] [PubMed] [Google Scholar]
- 8.Hazlett J W. The third metacarpal boss. Int Orthop. 1992;16(4):369–371. doi: 10.1007/BF00189621. [DOI] [PubMed] [Google Scholar]
- 9.Park M J, Namdari S, Weiss A P. The carpal boss: review of diagnosis and treatment. J Hand Surg Am. 2008;33(3):446–449. doi: 10.1016/j.jhsa.2007.11.029. [DOI] [PubMed] [Google Scholar]
- 10.Citteur J M, Ritt M J, Bos K E. Carpal boss: destabilization of the third carpometacarpal joint after a wedge excision. J Hand Surg [Br] 1998;23(1):76–78. doi: 10.1016/s0266-7681(98)80225-8. [DOI] [PubMed] [Google Scholar]
- 11.Melone C P Jr Polatsch D B Beldner S Disabling hand injuries in boxing: boxer's knuckle and traumatic carpal boss Clin Sports Med 2009284609–621., vii [DOI] [PubMed] [Google Scholar]
- 12.Apple J S, Martinez S, Nunley J A. Painful os styloideum: bone scintigraphy in carpe bossu disease. AJR Am J Roentgenol. 1984;142(1):181–182. doi: 10.2214/ajr.142.1.181. [DOI] [PubMed] [Google Scholar]
- 13.Karmazyn B, Siddiqui A R. Painful os styloideum in a child. Pediatr Radiol. 2002;32(5):370–372. doi: 10.1007/s00247-001-0639-6. [DOI] [PubMed] [Google Scholar]
- 14.Bassoe E, Bassoe H H. The styloid bone and carpe bossu disease. Am J Roentgenol Radium Ther Nucl Med. 1955;74(5):886–888. [PubMed] [Google Scholar]
- 15.Nakamura K, Patterson R M, Viegas S F. The ligament and skeletal anatomy of the second through fifth carpometacarpal joints and adjacent structures. J Hand Surg Am. 2001;26(6):1016–1029. doi: 10.1053/jhsu.2001.26329. [DOI] [PubMed] [Google Scholar]
- 16.R Core Team R: A language and environment for statistical computingVienna, Austria R Foundation for Statistical Computing 2014. Available at: http://www.R-project.org/. Accessed October 19, 2015
- 17.Ward C V, Tocheri M W, Plavcan J M, Brown F H, Manthi F K. Early Pleistocene third metacarpal from Kenya and the evolution of modern human-like hand morphology. Proc Natl Acad Sci U S A. 2014;111(1):121–124. doi: 10.1073/pnas.1316014110. [DOI] [PMC free article] [PubMed] [Google Scholar]


