Abstract
Background The aim of this study is to evaluate the clinical and radiological midterm results of a combined dorsal tenodesis–capsulodesis for static and reducible scapholunate dissociation (SLD).
Patients and Methods We evaluated 20 of 22 consecutive patients with static SLD minimum with follow-up of 2 years operated between 2003 and 2012. The mean age was 40 years (range: 23–65 years). Seventeen were men. Final evaluation included comparative wrist range of motion (ROM) and grip strength, pre- and postoperative pain and function by visual analog scale, and QuickDASH and Wrightington scores. Radiographs included preoperative, early postoperative, and final X-rays. Scapholunate space (SLS) and scapholunate and radioscaphoid angles (SLA and RSA) were measured. Statistical significance was evaluated with Student t-test, considered significant when p < 0.05.
Results Mean follow-up was 67 months (range: 24–126 months). Mean final ROM was: flexion 55 degrees (73%), extension 62 degrees (90%), radial deviation 19 degrees (82%), and ulnar deviation 44 degrees (90%). Mean grip strength was 44 kg (92%). Pain at rest improved from 3.4 to 0.5 (p < 0.05). Pain in activity improved from 7 to 1.7 (p < 0.05). Final function was 8.5 (preoperative, 5.2; p < 0.05). Mean QuickDASH score improved from 38 to 8 (p < 0.05). Functional Wrightington score was as follows: 13 excellent, 3 good, 1 regular, and 3 poor. There were three postoperative minor complications. Radiological results (preoperative/early postoperative/final follow-up) were as follows: SLS, 4.7/1.6/1.8 mm; and SLA, 60/50/62 degrees; RSA, 39/45/37 degrees. Four patients showed arthritic changes (two SLAC wrist).
Conclusion The clinical and radiological results with more than 2-year follow-up suggest that this technique may be effective, reproducible, and safe for symptomatic static and reducible SLD.
Level of Evidence Level IV, case series.
Keywords: capsulodesis, carpal instability, scapholunate dissociation, tenodesis
Scapholunate dissociation (SLD) is the most common cause of wrist instability and severe dysfunction of the wrist in young patients.1
Numerous surgical strategies have been developed to address SLD. Many of these procedures may be grouped generically into bone and soft-tissue reconstructions. Unfortunately, so far no therapeutic alternatives have shown predictable long-term results in relieving the symptoms and preventing arthritic changes, especially in severe cases with a static instability.2 3 4 5 6 7 8 9 Thus, there is still no consensus about what is the ideal management of this complex problem.
Previously, we described an alternative for scapholunate ligament reconstruction that combined a novel tenodesis using a strip of the extensor carpi radialis longus (ECRL)10 with a Mayo-type capsulodesis11 through a single dorsal approach without tunneling the scaphoid, with good preliminary results (Figs. 1 and 2).
Fig. 1.
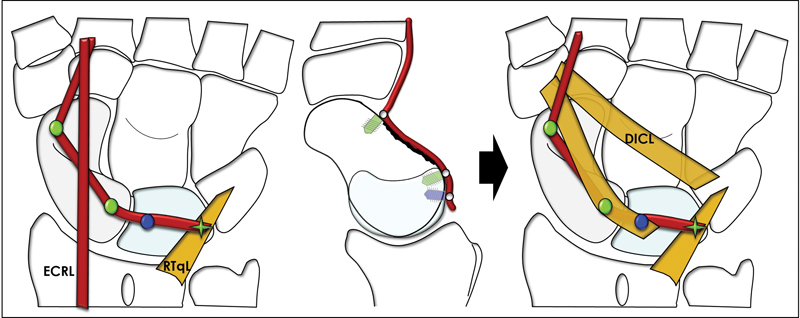
Tenodesis using a distally based strip of the ECRL fixed with three suture anchors to the proximal and distal pole of the scaphoid and lunate. Reinforcement is made with a dorsal capsulodesis as described by Walsh et al.11 DICL, dorsal intercarpal ligament; RTqL, radiotriquetral ligament.
Fig. 2.
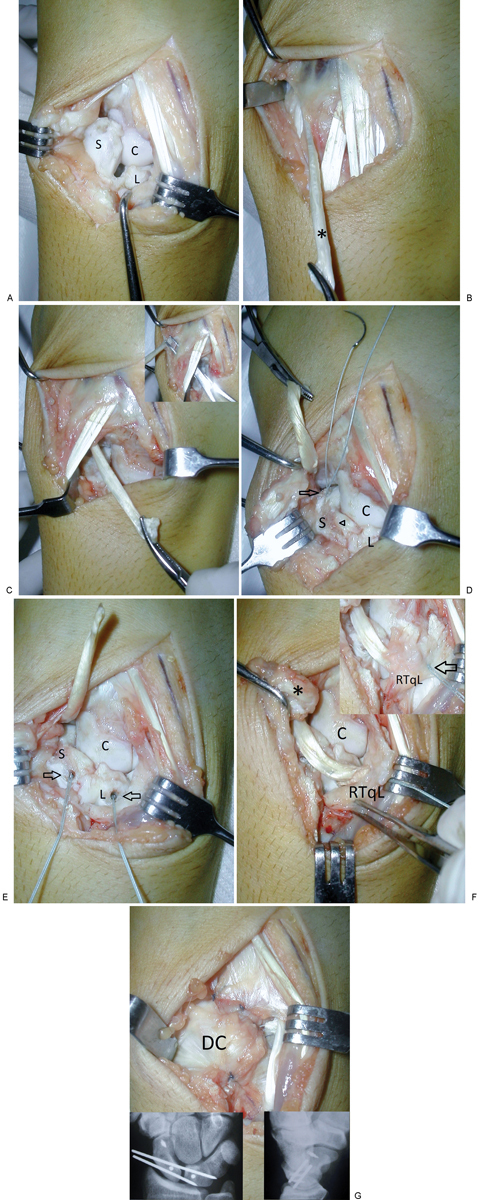
A 30-year-old man with static SLD in his right dominant wrist (case 3). (A) Dorsal approach demonstrating a complete irreparable SL ligament tear with rotary subluxation of the scaphoid (S, scaphoid; C, capitate; L, lunate). (B) After carpal reduction, a distally based strip of the ECRL (*) is harvested through the same dorsal approach. (C) The ECRL strip is passed below the extensor carpi radialis brevis and extensor digitorum. (D) A channel is carved over the dorsal aspect of the scaphoid and lunate to uncover cancellous bone (arrowhead). At first, the tendon strip is fixed on the distal pole of the scaphoid with an anchor suture (arrow) to prevent rotary subluxation. (E) Subsequently, the strip is fixed on the proximal pole of the scaphoid and lunate with another two anchor sutures (arrows) to reconstruct the dorsal SL ligament. (F) Thereafter, the tendon is sutured onto the distal portion of the RTqL to preclude ulnar translation and extension of the lunate (arrow). Once the tendon reconstruction is finished, reinforcement is made with a Mayo dorsal capsulodesis using a proximal radially based slip of the dorsal intercarpal ligament (*). (G) Finally, the dorsal capsular flap (DC) is then brought back to its original position and sutured.
The aim of this study is to describe the midterm clinical and radiological results of this technique in cases with static reducible rotary subluxation of the scaphoid.
Materials and Methods
We performed a retrospective analysis of 28 consecutive patients operated in our institution for SLD between September 2003 and July 2015 with the combined ligament reconstruction technique. Only those cases with an isolated complete tear with static-reducible carpal instability and a nonrepairable ligament, without preconditions, and with a minimum follow-up of 2 years were included in this study. Patients presenting with other stages of scapholunate injury at the time of surgery, those with associated injuries, patients treated with another surgical technique, and those with less than 2 years' follow-up were excluded.
Of the original 22 cases who met the inclusion and exclusion criteria, 20 were available for follow-up examination at an average of 65 months postoperatively (range: 24–126 months). There were 17 men and 3 women, and the mean age was 40 years (range: 23–65 years) at the time of surgery. The dominant hand was involved in 13 cases. The mean time from injury to operation was 9 months (range: 2–30 months). Table 1 presents the demographic data for the entire group.
Table 1. Demographic data.
| Patient | Gender | Age at surgery (y) | Injured limb/dominant limb | Delay for surgery (mo) | Follow-up (mo) |
|---|---|---|---|---|---|
| 1 | F | 43 | L/R | 15 | 126 |
| 2 | M | 43 | R/R | 6 | 108 |
| 3 | M | 30 | R/R | 6 | 105 |
| 4 | M | 31 | R/R | 30 | 106 |
| 5 | M | 40 | R/L | 12 | 93 |
| 6 | M | 45 | L/R | 6 | 72 |
| 7 | M | 32 | L/L | 8 | 87 |
| 8 | M | 35 | R/R | 10 | 29 |
| 9 | M | 49 | R/R | 12 | 91 |
| 10 | F | 36 | R/R | 8 | 72 |
| 11 | M | 48 | R/R | 29 | 60 |
| 12 | M | 30 | R/R | 4 | 60 |
| 13 | M | 39 | R/R | 6 | 56 |
| 14 | M | 48 | L/R | 3 | 50 |
| 15 | M | 65 | L/R | 2 | 41 |
| 16 | M | 48 | R/R | 10 | 34 |
| 17 | M | 34 | R/L | 2 | 34 |
| 18 | M | 23 | R/L | 2 | 33 |
| 19 | F | 41 | R/R | 6 | 24 |
| 20 | M | 34 | L/L | 3 | 24 |
| Mean | 17 M/3 F | 40 | 9 | 65 |
All patients were interviewed and examined by a single examiner not involved in the surgery. Objective clinical evaluation included range of flexion/extension and radial/ulnar deviation measured with a goniometer and grip strength using a Jamar dynamometer. Unfortunately, we could not find full retrospective information of these parameters in all patients before surgery; this is why, they were not included in the final analysis. Pain and function were evaluated pre- and postoperatively using a visual analog scale (VAS). All patients completed the QuickDASH questionnaire. Furthermore, the specific function of the wrist was evaluated with the Wrightington Hospital wrist scoring system that includes both objective and subjective parameters: pain, function, motion, and grip strength.12 13 Questions about working and sports activity status, and satisfaction with the operation were also included.
Radiological analysis included preoperative, immediate postoperative, and final studies. This involved posteroanterior and lateral views, “forced closing fist” stress views (in 16/20 cases), and radioulnar deviation of both wrists. All measurements were performed digitally by two investigators using the RAIM viewer software. On the lateral radiographs, the scapholunate and radioscaphoid angles (SLA and RSA, respectively) were measured using the tangential and axial methods, respectively.14 The scapholunate space (SLS) was measured on posteroanterior and stress views (distance between midpoints of the edge of each bone).15 The presence of osteoarthritic changes were also determined.
Statistical analysis of comparing clinical and radiologic parametric data was performed by the Student t-test. A p-value < 0.05 was considered as significant.
Results
Tables 2 and 3 described the objective and subjective results of the clinical evaluation. At the final follow-up examination, the mean range of wrist motion relative to the contralateral side was: flexion = 73%; extension = 90%; radial deviation = 82%; and ulnar deviation = 90%. The final grip strength was 92%, compared with the other side. Pain relief was statistically significant. At final evaluation, only two cases presented increase of pain at rest compared with preoperative values, and five cases referred increased pain during activities. The improvement of function was also statistically significant. In 16 cases, the final postoperative function was superior to preoperative.
Table 2. Final postoperative clinical results: objective parameters.
| Injured wrist | Uninjured wrist | Percentage relative to the contralateral side (%) | p | |
|---|---|---|---|---|
| Flexion (degree) | 55 (44–62) | 75 (55–90) | 73 | 0.00001 |
| Extension (degree) | 62 (38–75) | 68 (41–80) | 90 | 0.0005 |
| Radial deviation (degree) | 19 (14–32) | 24 (12–45) | 82 | 0.006 |
| Ulnar deviation (degree) | 44 (30–58) | 49 (30–66) | 90 | 0.002 |
| Grip strength (kg) | 44 (11–61) | 48 (29–69) | 92 | 0.003 |
Table 3. Clinical results: subjective parameters.
| Case | Pain-rest (VAS) | Pain-activity (VAS) | Function (VAS) | QuickDASH | ||||
|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | |
| 1 | 4 | 0 | 6 | 0 | 5 | 8 | 28 | 2 |
| 2 | 3 | 0 | 8 | 0 | 4 | 10 | 40 | 13 |
| 3 | 1 | 0 | 6 | 3 | 3 | 8 | 64 | 9 |
| 4 | 1 | 0 | 6 | 0 | 5 | 9 | 25 | 2 |
| 5 | 0 | 0 | 7 | 0 | 5 | 10 | 20 | 0 |
| 6 | 3 | 1 | 8 | 4 | 3 | 5 | 66 | 46 |
| 7 | 2 | 3 | 6 | 3 | 8 | 6 | 2 | 0 |
| 8 | 5 | 1 | 7 | 1 | 6 | 9 | 52 | 2 |
| 9 | 6 | 1 | 9 | 1 | 4 | 9 | 66 | 18 |
| 10 | 2 | 3 | 5 | 7 | 7 | 6 | 36 | 38 |
| 11 | 4 | 1 | 8 | 1 | 4 | 9 | 46 | 2 |
| 12 | 5 | 0 | 9 | 0 | 4 | 10 | 42 | 0 |
| 13 | 3 | 0 | 7 | 5 | 5 | 8 | 20 | 2 |
| 14 | 7 | 0 | 10 | 0 | 2 | 9 | 60 | 0 |
| 15 | 8 | 0 | 8 | 2 | 4 | 8 | 84 | 14 |
| 16 | 2 | 0 | 2 | 0 | 10 | 10 | 6 | 2 |
| 17 | 2 | 0 | 6 | 1 | 7 | 8 | 30 | 7 |
| 18 | 3 | 0 | 8 | 1 | 5 | 9 | 28 | 2 |
| 19 | 5 | 0 | 5 | 0 | 5 | 10 | 34 | 0 |
| 20 | 1 | 0 | 8 | 5 | 8 | 8 | 10 | 0 |
| Mean | 3.4 | 0.5 | 7 | 1.7 | 5.2 | 8.5 | 38 | 8 |
| Range | 0–8 | 0–3 | 5–10 | 0–7 | 3–10 | 5–10 | 0–84 | 0–46 |
| p-Value | <0.001 | <0.001 | <0.001 | <0.001 | ||||
Abbreviation: VAS, visual analog scale.
At final review, there was a significant decrease in the QuickDASH score, representing an improvement in the general function of the injured upper extremity. The functional results of the wrist according to the score of Wrightington were excellent in 13, good in 3, fair in 1, and poor in 3 cases. Before surgery, 11 patients reported a restricted work activity, while in the last assessment only 3 cases were restricted. Sports activity was restricted in 18 cases preoperatively and in 6 cases postoperatively. Fifteen patients (75%) returned to their labor or sports activities prior to the injury. Finally, 11 patients were very satisfied with the result, 5 patients satisfied, 3 patients mildly satisfied, and 1 patient dissatisfied.
Radiological outcomes are summarized in Table 4. Fig. 3 shows the radiological results of an exemplifying case. When comparing the preoperative with the immediate postoperative findings, there were significant reductions in the three parameters evaluated. Both SLA and RSA increased significantly thereafter, while the SLS remained without significant changes. Analyzing the data individually, all but one patient had a loss of the initial reduction in any of the three parameters evaluated: SLS in 6 cases (11 cases on stress views); SLA in 16 cases; and RSA in 14 cases. However, only three patients had a carpal collapse (loss of all three parameters simultaneously). Finally, four cases showed arthritic changes. One of these cases evolved into an scapholunate advanced collapse (SLAC) II wrist and another into an SLAC III (Fig. 4). Another case presented isolated advance midradiocarpal degenerative osteoarthritis but similar to the contralateral uninjured wrist (case 15, a man of 68 years at final evaluation). The last case showed osteoarthritis only in the midcarpal joint without significant widening of scapholunate gap, subluxation of the scaphoid, or carpal collapse (Fig. 5).
Table 4. Radiological results.
| Case | SLS (mm) | SLA (degree) | RSA (degree) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Immediate post-op | Final post-op | “Forced closing fist” | Pre-op | Immediate post-op | Final post-op | Pre-op | Immediate post-op | Final post-op | |
| 1 | 4 | 2 | 2 | – | 52 | 28 | 29 | 40 | 46 | 42 |
| 2 | 5.4 | 1.5 | 1.6 | – | 58 | 52 | 53 | 44 | 44 | 42 |
| 3 | 6.3 | 1.8 | 1.9 | 2 | 70 | 65 | 72 | 41 | 48 | 24 |
| 4 | 8.1 | 1.3 | 1.4 | – | 55 | 50 | 50 | 35 | 40 | 38 |
| 5 | 6.3 | 1.8 | 1.9 | 2 | 70 | 23 | 54 | 31 | 62 | 39 |
| 6 | 6.8 | 1.4 | 1.8 | 2.2 | 60 | 56 | 57 | 38 | 44 | 41 |
| 7 | 7.6 | 1.4 | 1.6 | 2.9 | 86 | 86 | 92 | 36 | 36 | 30 |
| 8 | 7.2 | 1.8 | 1.8 | 2.7 | 54 | 55 | 65 | 48 | 50 | 38 |
| 9 | 1.8 | 1.7 | 1.7 | 2.9 | 45 | 45 | 54 | 46 | 48 | 40 |
| 10 | 6.3 | 1.8 | 2.2 | 2.3 | 82 | 22 | 70 | 34 | 76 | 27 |
| 11 | 3.6 | 2.7 | 2.7 | – | 60 | 55 | 67 | 35 | 40 | 37 |
| 12 | 6.3 | 1 | 1 | 1.1 | 50 | 47 | 53 | 42 | 44 | 28 |
| 13 | 6.2 | 0.9 | 0.9 | 0.9 | 58 | 54 | 70 | 34 | 38 | 30 |
| 14 | 1.8 | 1.8 | 2.2 | 2.8 | 60 | 48 | 72 | 32 | 39 | 36 |
| 15 | 3.6 | 1.8 | 2 | 3.6 | 87 | 60 | 63 | 28 | 30 | 29 |
| 16 | 2.7 | 1.6 | 1.6 | 2 | 62 | 56 | 89 | 30 | 34 | 31 |
| 17 | 4.6 | 1.1 | 1.1 | 1.2 | 45 | 45 | 54 | 40 | 42 | 40 |
| 18 | 0.9 | 1 | 1.2 | 1.9 | 54 | 53 | 70 | 38 | 40 | 38 |
| 19 | 2.7 | 2 | 4.5 | 4.5 | 52 | 46 | 49 | 50 | 55 | 55 |
| 20 | 1.8 | 1.3 | 1.4 | 1.8 | 48 | 45 | 66 | 48 | 53 | 48 |
| Mean | 4.7 | 1.6 | 1.8 | 2.3 | 60 | 50 | 62 | 39 | 45 | 37 |
| Range | 0.9–8.1 | 0.9–2.7 | 0.9–4.5 | 0.9–4.5 | 45–87 | 22–86 | 29–92 | 28–50 | 30–76 | 27–55 |
| p-Value | <0.001 | 0.12 | 0.007 | 0.003 | 0.008 | 0.002 | ||||
Abbreviations: RSA, radioscaphoid angle; SLA, scapholunate angle; SLS, scapholunate space.
Fig. 3.
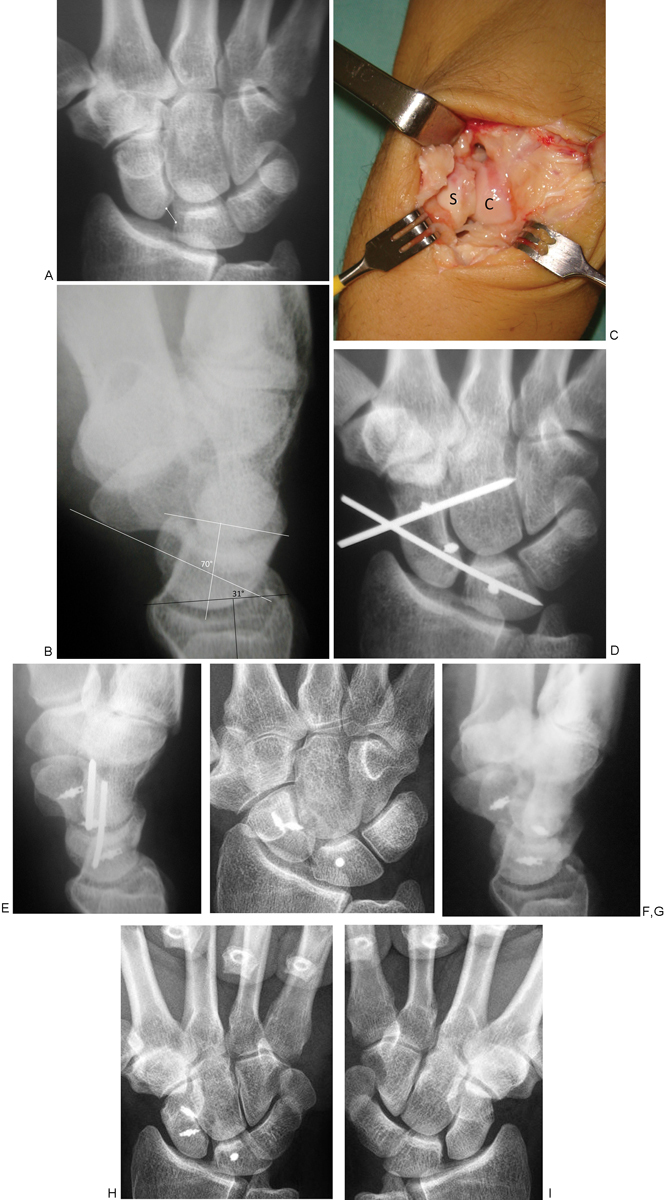
A 40-year-old man with static SLD in his right nondominant wrist (case 5). (A, B) Preoperative X-rays: SLS, 6.3 mm; SLA, 70 degrees; RSA, 31 degrees. (C) Intraoperative findings: total and irreparable ligament rupture with rotary subluxation of the scaphoid. (D, E) Immediate postoperative radiographs. Note some initial overcorrection. SLS, 1.8 mm; SLA, 23 degrees; RSA, 62 degrees. (F, G) Comparative X-rays at final assessment (93 months) appreciating an acceptable carpal alignment. SLS, 1.9 mm; SLA, 54 degrees; RSA, 39 degrees. (H, I) Comparative “forced closing fist” stress views. The scapholunate space is maintained.
Fig. 4.
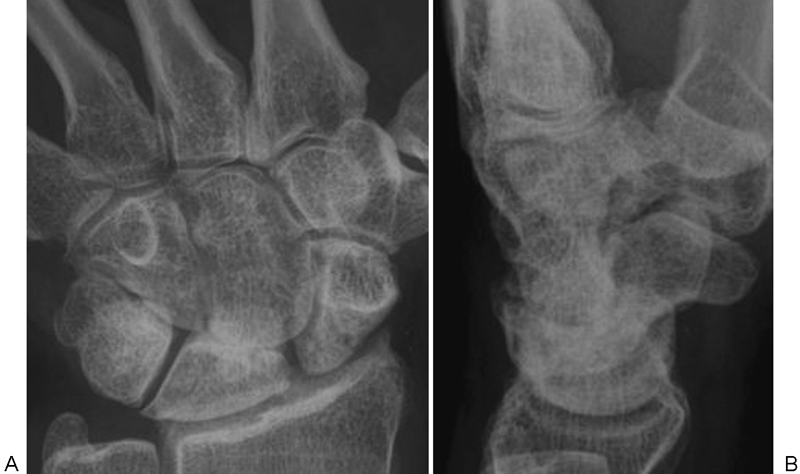
Case 10. A 36-year-old woman presenting an SLAC III right wrist at final evaluation (72 months). (A, B) SLS, 2.3 mm; SLA, 70 degrees; RSA, 27 degrees.
Fig. 5.

Case 3. Patient with isolated midcarpal arthritis at final follow-up (105 months). (A, B) Nevertheless, X-rays demonstrate acceptable carpal alignment. SLS, 1,9 mm; SLA, 72 degrees; RSA, 24 degrees.
There were three postoperative complications. One patient presented early migration of K-wires that did not seem to have affected the final outcome. Another two patients presented temporary radial sensory nerve dysesthesias that resolved spontaneously.
Discussion
The primary goals in the treatment of scapholunate instability are to relieve the patient's symptoms, thus preserving a functional wrist mobility, and to prevent carpal collapse, thereby avoiding osteoarthritic change.7 16 17 A variety of surgical techniques have been proposed to treat this complex problem, yet disagreement remains with respect to the best management.16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32
As mentioned by Kitay and Wolfe,16 in the presence of a flexible deformity (dynamic instability) without osteoarthritis some type of soft-tissue reconstruction may be indicated. The majority of the capsulodesis bring good results in these cases.13 22 33 34 35 36 However, long-term studies described severe deterioration of these results in cases with static instability.2 3 8
In an attempt to achieve a stronger reconstruction, numerous authors propose the utilization of some type of tenodesis. The short-term results using the different modern techniques show good clinical and radiological results.4 5 6 7 9 However, so far we have not found evidence in the literature that describes the evolution of these results in the medium- to long-term follow-up.
Preliminary results of our technique of combined dorsal tenodesis and capsulodesis with 2 years of mean follow-up were similar to the other alternatives.10 In this study, the results in the medium to long term were presented to determine whether they are maintained over time. According to the results obtained after an average 6-year follow-up, 16/20 patients were satisfied with the result, returning 15 of them to all their previous work and sports activities. No patient referred moderate or severe pain at rest (VAS [visual analog scale] > 4), and only four patients presented moderate or severe pain during activity. Two of them were those with an SLAC wrist. In the other two cases, the pain was probably related to his activities (golf and graphic design), as radiologically they did not have evidence of a severe carpal collapse.
This new tenodesis using an ECRL tendon slip gives some advantages over other techniques described previously: (1) only one dorsal approach is required; (2) scaphoid tunneling is not necessary, and thus it is technically less demanding and avoids the potential risk of fracture or necrosis of the bone; and (3) it is possible to combine the tenodesis with a dorsal capsulodesis to achieve a more consistent reconstruction through a single dorsal approach without increasing morbidity and complexity of the procedure.
In relation to the radiological findings, there are no reports of any surgical interventions for this problem that demonstrate consistent results to prevent or delay the progression to an SLAC wrist.8 16 The correction and maintenance of alignment (kinetic) and mobility (kinematic) of the carpus are particularly relevant considering that many of these patients are young active people. As with all techniques of ligament reconstruction, it is expected that some radiological deterioration occurs over time. In our series, the SLS remained without significant changes over time. Technically, to avoid rotatory subluxation of the scaphoid, we believe it is critical to set the first anchor radially to the distal pole of the scaphoid to control not only flexion but also pronation of the carpal bone. On the contrary, the loss of the initial reduction was significant in the SLA and RSA, demonstrating a major difficulty of the procedure to support the alignment of the scaphoid and lunate in the sagittal plane. Nevertheless, at the time of the final evaluation, only four patients (20%) presented carpal osteoarthritis. This percentage is similar to that presented by Garcia-Elias et al using the three-ligament reconstruction with a shorter follow-up,7 and lower than in previous studies using several capsulodesis with a long-term follow-up (27–50%).2 3 8 Further evaluation of our patients will reveal whether these osteoarthritic changes will be maintained over time.
An alternative to soft-tissue reconstruction techniques is to conduct some type of limited carpal arthrodesis. The results reported are very similar to the ligament reconstructions but with higher incidence of complications, including nonunion and radiocarpal arthrosis (4–51% and 15–35%, respectively).21 37 38 39 40 The major advantage of dorsal capsulodesis and tenodesis when compared with partial arthrodesis is the preservation of some intercarpal motion. To achieve this, the reconstruction should be strong enough to stabilize the carpus, and simultaneously flexible enough to preserve its dynamics. To evaluate both features, we considered not only static radiographs, but also dynamic radiographs in maximum radioulnar deviation. Two-thirds of the cases examined showed some kind of mobility for flexion and extension of the scaphoid, suggesting the possibility of preserving at least part of the carpal biomechanics with this type of soft-tissue reconstruction (Fig. 6).
Fig. 6.

Case 3. (A–D) Comparative radiographs in maximum radioulnar deviation of both wrists, showing certain mobility of the proximal carpal row (flexion-extension).
Regarding the level of evidence, this study presents all limitations associated with a case series retrospectively evaluated with no comparison group. In addition, the relatively small sample size determines some statistical limitations. However, some aspect must be considered to provide relevance to our results. While the technique presented would be also indicated in cases of SLD with dynamic instability (grade III of Garcia-Elias et al classification), in this study we decided to include only those with static reducible instability (grade IV), in which the prognosis is less predictable and therapeutic alternatives are more limited.
In conclusion, we believe that the results obtained justify the indication of this procedure in symptomatic patients, preserving in most cases pain relief and functional mobility of the wrist with acceptable radiographic changes for at least 5 years after average follow-up. However, re-evaluation of this result with a longer follow-up would be necessary in an attempt to determine its effectiveness in preventing or at least delaying the carpal collapse and osteoarthritic changes of the injured wrist, and also to define the surgical indication for asymptomatic patients.
Conflict of Interest None.
Note
All authors adhere to the ethical standards described by the Committee on Publication Ethics and the International Committee of Medical Journal Editors.
References
- 1.Gelberman R H, Cooney W P III, Szabo R M. Carpal instability. J Bone Joint Surg Am. 2000;82:578–594. [Google Scholar]
- 2.Megerle K, Bertel D, Germann G, Lehnhardt M, Hellmich S. Long-term results of dorsal intercarpal ligament capsulodesis for the treatment of chronic scapholunate instability. J Bone Joint Surg Br. 2012;94(12):1660–1665. doi: 10.1302/0301-620X.94B12.30007. [DOI] [PubMed] [Google Scholar]
- 3.Schweizer A, Steiger R. Long-term results after repair and augmentation ntercarpalsty of rotatory subluxation of the scaphoid. J Hand Surg Am. 2002;27(4):674–684. doi: 10.1053/jhsu.2002.34320. [DOI] [PubMed] [Google Scholar]
- 4.Brunelli G A Brunelli G R A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report J Hand Surg Am 199520(3, Pt 2):S82–S85. [DOI] [PubMed] [Google Scholar]
- 5.Van Den Abbeele K L, Loh Y C, Stanley J K, Trail I A. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg [Br] 1998;23(2):258–261. doi: 10.1016/s0266-7681(98)80191-5. [DOI] [PubMed] [Google Scholar]
- 6.Talwalkar S C, Edwards A T, Hayton M J, Stilwell J H, Trail I A, Stanley J K. Results of tri-ligament tenodesis: a modified Brunelli procedure in the management of scapholunate instability. J Hand Surg [Br] 2006;31(1):110–117. doi: 10.1016/j.jhsb.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Elias M, Lluch A L, Stanley J K. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Gajendran V K, Peterson B, Slater R R Jr, Szabo R M. Long-term outcomes of dorsal intercarpal ligament capsulodesis for chronic scapholunate dissociation. J Hand Surg Am. 2007;32(9):1323–1333. doi: 10.1016/j.jhsa.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Chabas J F, Gay A, Valenti D, Guinard D, Legre R. Results of the modified Brunelli tenodesis for treatment of scapholunate instability: a retrospective study of 19 patients. J Hand Surg Am. 2008;33(9):1469–1477. doi: 10.1016/j.jhsa.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 10.De Carli P, Donndorff A G, Gallucci G L, Boretto J G, Alfie V A. Chronic scapholunate dissociation: ligament reconstruction combining a new extensor carpi radialis longus tenodesis and a dorsal intercarpal ligament capsulodesis. Tech Hand Up Extrem Surg. 2011;15(1):6–11. doi: 10.1097/BTH.0b013e3181e6650c. [DOI] [PubMed] [Google Scholar]
- 11.Walsh J J, Berger R A, Cooney W P. Current status of scapholunate interosseous ligament injuries. J Am Acad Orthop Surg. 2002;10(1):32–42. doi: 10.5435/00124635-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Cooney W P. London: Martin Dunitz; 1995. Open reduction of distal radius fractures: indications, classifications and functional assessment; pp. 118–125. [Google Scholar]
- 13.Moran S L, Cooney W P, Berger R A, Strickland J. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg Am. 2005;30(1):16–23. doi: 10.1016/j.jhsa.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Larsen C F, Mathiesen F K, Lindequist S. Measurements of carpal bone angles on lateral wrist radiographs. J Hand Surg Am. 1991;16(5):888–893. doi: 10.1016/s0363-5023(10)80156-x. [DOI] [PubMed] [Google Scholar]
- 15.Lawand A Foulkes G D The “clenched pencil” view: a modified clenched fist scapholunate stress view J Hand Surg Am 2003283414–418., discussion 419–420 [DOI] [PubMed] [Google Scholar]
- 16.Kitay A, Wolfe S W. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2012;37(10):2175–2196. doi: 10.1016/j.jhsa.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 17.Moran S L, Ford K S, Wulf C A, Cooney W P. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg Am. 2006;31(9):1438–1446. doi: 10.1016/j.jhsa.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Watson H K, Ryu J, Akelman E. Limited triscaphoid intercarpal arthrodesis for rotatory subluxation of the scaphoid. J Bone Joint Surg Am. 1986;68(3):345–349. [PubMed] [Google Scholar]
- 19.Blatt G. Capsulodesis in reconstructive hand surgery. Dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3(1):81–102. [PubMed] [Google Scholar]
- 20.Almquist E E, Bach A W, Sack J T, Fuhs S E, Newman D M. Four-bone ligament reconstruction for treatment of chronic complete scapholunate separation. J Hand Surg Am. 1991;16(2):322–327. doi: 10.1016/s0363-5023(10)80120-0. [DOI] [PubMed] [Google Scholar]
- 21.Pisano S M, Peimer C A, Wheeler D R, Sherwin F. Scaphocapitate intercarpal arthrodesis. J Hand Surg Am. 1991;16(2):328–333. doi: 10.1016/s0363-5023(10)80121-2. [DOI] [PubMed] [Google Scholar]
- 22.Lavernia C J, Cohen M S, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg Am. 1992;17(2):354–359. doi: 10.1016/0363-5023(92)90419-p. [DOI] [PubMed] [Google Scholar]
- 23.Linscheid R L, Dobyns J H. Treatment of scapholunate dissociation. Rotatory subluxation of the scaphoid. Hand Clin. 1992;8(4):645–652. [PubMed] [Google Scholar]
- 24.Rotman M B, Manske P R, Pruitt D L, Szerzinski J. Scaphocapitolunate arthrodesis. J Hand Surg Am. 1993;18(1):26–33. doi: 10.1016/0363-5023(93)90240-4. [DOI] [PubMed] [Google Scholar]
- 25.Herbert T J, Hargreaves I C, Clarke A M. A new surgical technique for treating rotary instability of the scaphoid. Hand Surg. 1996;1:75–77. [Google Scholar]
- 26.Slater R R Jr, Szabo R M. Scapholunate dissociation: treatment with the dorsal intercarpal ligament capsulodesis. Tech Hand Up Extrem Surg. 1999;3(4):222–228. [PubMed] [Google Scholar]
- 27.Rosenwasser M P, Miyasajsa K C, Strauch R J. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Up Extrem Surg. 1997;1(4):263–272. [PubMed] [Google Scholar]
- 28.Wolf J M Weiss A P Bone-retinaculum-bone reconstruction of scapholunate ligament injuries Orthop Clin North Am 2001322241–246., viii [DOI] [PubMed] [Google Scholar]
- 29.Seradge H, Baer C, Dalsimer D, Seradge A, Shafi R A, Parker W. Treatment of dynamic scaphoid instability. J Trauma. 2004;56(6):1253–1260. doi: 10.1097/01.ta.0000075520.11052.64. [DOI] [PubMed] [Google Scholar]
- 30.Zarkadas P C, Gropper P T, White N J, Perey B H. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg Am. 2004;29(5):848–857. doi: 10.1016/j.jhsa.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Bleuler P, Shafighi M, Donati O F, Gurunluoglu R, Constantinescu M A. Dynamic repair of scapholunate dissociation with dorsal extensor carpi radialis longus tenodesis. J Hand Surg Am. 2008;33(2):281–284. doi: 10.1016/j.jhsa.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 32.Binder A C, Kerfant N, Wahegaonkar A L, Tandara A A, Mathoulin C L. Dorsal wrist capsular tears in association with scapholunate instability: results of an arthroscopic dorsal capsuloplasty. J Wrist Surg. 2013;2(2):160–167. doi: 10.1055/s-0032-1333426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wintman B I, Gelberman R H, Katz J N. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg Am. 1995;20(6):971–979. doi: 10.1016/S0363-5023(05)80145-5. [DOI] [PubMed] [Google Scholar]
- 34.Deshmukh S C, Givissis P, Belloso D, Stanley J K, Trail I A. Blatt's capsulodesis for chronic scapholunate dissociation. J Hand Surg [Br] 1999;24(2):215–220. doi: 10.1054/jhsb.1998.0183. [DOI] [PubMed] [Google Scholar]
- 35.Pomerance J. Outcome after repair of the scapholunate interosseous ligament and dorsal capsulodesis for dynamic scapholunate instability due to trauma. J Hand Surg Am. 2006;31(8):1380–1386. doi: 10.1016/j.jhsa.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Luchetti R, Atzei A, Cozzolino R, Fairplay T. Current role of open reconstruction of the scapholunate ligament. J Wrist Surg. 2013;2(2):116–125. doi: 10.1055/s-0033-1343092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fortin P T, Louis D S. Long-term follow-up of scaphoid-trapezium-trapezoid arthrodesis. J Hand Surg Am. 1993;18(4):675–681. doi: 10.1016/0363-5023(93)90317-V. [DOI] [PubMed] [Google Scholar]
- 38.Chantelot C, Becquet E, Leconte F, Lahoude-Chantelot S, Prodomme G, Fontaine C. Scaphocapitate arthrodesis for chronic scapholunate instability: a retrospective study of 13 cases [in French] Chir Main. 2005;24(2):79–83. doi: 10.1016/j.main.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Delétang F, Segret J, Dap F, Dautel G. Chronic scapholunate instability treated by scaphocapitate fusion: a midterm outcome perspective. Orthop Traumatol Surg Res. 2011;97(2):164–171. doi: 10.1016/j.otsr.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 40.Luegmair M, Saffar P. Scaphocapitate arthrodesis for treatment of scapholunate instability in manual workers. J Hand Surg Am. 2013;38(5):878–886. doi: 10.1016/j.jhsa.2013.01.013. [DOI] [PubMed] [Google Scholar]


