Abstract
Objective:
To investigate the impact of radiographer advanced practice on patient outcomes and health service quality.
Methods:
Using the World Health Organization definition of quality, this review followed the Centre for Reviews and Dissemination guidance for undertaking reviews in healthcare. A range of databases were searched using a defined search strategy. Included studies were assessed for quality using a tool specifically developed for reviewing studies of diverse designs, and data were systematically extracted using electronic data extraction pro forma.
Results:
407 articles were identified and reviewed against the inclusion/exclusion criteria. Nine studies were included in the final review, the majority (n = 7) focusing on advanced radiography practice within the UK. Advanced practice activities considered were radiographer reporting, leading patient review clinics and barium enema examinations. The articles were generally considered to be of low-to-moderate quality, with most evaluating advanced practice within a single centre. With respect to specific quality dimensions, the included studies considered cost reduction, patient morbidity, time to treatment and patient satisfaction. No articles reported data relating to time to diagnosis, time to recovery or patient mortality.
Conclusion:
Radiographer advanced practice is an established activity both in the UK and internationally. However, evidence of the impact of advanced practice in terms of patient outcomes and service quality is limited.
Advances in knowledge:
This systematic review is the first to examine the evidence base surrounding advanced radiography practice and its impact on patient outcomes and health service quality.
INTRODUCTION
Advanced radiographic practice has been the focus of much discussion and debate over the past 15 years,1–6 not only within the UK, where advanced practitioner roles are recognized within the national career framework,7 but also internationally.8–12 Today, advanced radiographer practitioners are an integral part of the imaging and oncology workforce, with an estimated 3662 diagnostic radiographers in the UK employed in advanced practice roles and 86 in consultant roles.13 A further 1288 radiographers are also reported to be undertaking postgraduate education with the intention of working as an advanced practitioner and providing clinical expertise and leadership within a defined area of practice on qualification.13
The introduction of advanced practice roles is often cited as being driven by increasing demands for imaging services and the concomitant shortage of radiologists.14–16 It has also been argued that efficiencies within healthcare delivery can be achieved only through developing new models of care that build on the knowledge and skills of the whole workforce.17,18 This is particularly true within diagnostic imaging, if the UK Government aspirations for 7-day working19 are to be achieved without accruing excessive costs. However, despite the validity of this efficiency argument, advanced practice opportunities for radiographers have historically been driven by the limited availability of radiologists within a local setting. As a result, much of the research literature surrounding advanced radiography practice has focused on specific advanced practice roles,20–22 often comparing the technical skills and competencies of radiographers with those of the delegating radiologist.23–25
This direct comparison of outcome, where one profession has been substituted for another with regard to a specific task, has been criticized in the nursing literature.26 Spilsbury and Meyer26 argued that when substituting doctors with nurses, it cannot be presumed that nurses will provide care in the same way as doctors, as activities undertaken by nurses are performed so within the context of a nursing, rather than the medical, framework. As such, nurses will bring different skills and experiences to the task and thus deliver the service in a different way to doctors, making direct comparison problematic. The same argument could be directed towards radiographer advanced practice, where radiologist role substitution has occurred. This does not imply that the task undertaken is of a greater or lesser quality, but instead suggests that it will be different as a consequence of differing professional paradigms. As a result, Spilsbury and Meyer26 argued that research exploring advanced practice needs to extend beyond direct professional comparisons and capture the way service quality improvement or enhancement has occurred, particularly with respect to patient outcomes and processes of care. This systematic review is the first to examine the evidence base surrounding advanced radiography practice and its impact on patient outcomes and health service quality.
METHODS AND MATERIALS
This review followed the Centre for Reviews and Dissemination guidance for undertaking reviews in healthcare27 and is reported in accordance with the Preferred Reporting Items for Systematic Reviews statement.28
Research questions
Before the research questions could be articulated, a clearly defined interpretation of quality was required. There are many definitions of quality, but for the purposes of this systematic review, the World Health Organization (WHO) definitions based on six quality dimensions were adopted (Table 1).29 These definitions reflect the components of high-quality care as identified by National Health Service England30 and were developed to enable reflection on strategies for improving healthcare delivery systems and patient outcomes. Consequently, they do not relate to a specific task or competency. This is an important contextual point, as the perception of whether a specific task or activity represents advanced practice will vary internationally. However, advanced radiography practice as a concept can be considered a strategy for improving service quality and therefore, assessment against these six quality dimensions is appropriate.
Table 1.
Quality dimensions and definitions29
| Quality dimension | Definition |
|---|---|
| Effective | Delivering healthcare that is adherent to an evidence base and results in improved health outcomes, for individuals and communities, based on need |
| Efficient | Delivering healthcare in a manner which maximizes resource use and avoids waste |
| Accessible | Delivering healthcare that is timely, geographically reasonable and provides in a setting where skills and resources are appropriate to medical need |
| Acceptable/patient centred | Delivering healthcare which takes into account the preferences and aspirations of individual service users and the cultures of their communities |
| Equitable | Delivering healthcare which does not vary in quality because of personal characteristics such as gender, race, ethnicity, geographical location or socioeconomic status |
| Safe | Delivering healthcare which minimizes risks and harm to service users |
Using the WHO dimensions of service quality29 (Table 1), seven research questions (Table 2) were identified to provide a comprehensive response to the overarching question of “does advanced radiography practice improve patient outcomes and health service quality?” No research question related to the “equitable” dimension, as our interpretation of this dimension was that the inherent variation in healthcare service delivery, practice and outcomes globally rendered equitability unlikely.
Table 2.
Research questions and related quality dimension
| Research question | Quality dimension(s) addressed |
|---|---|
| Does radiography advanced practice reduce patient mortality? | Effective Safe |
| Does radiography advanced practice reduce patient morbidity? | Effective Safe |
| Does radiography advanced practice reduce time to diagnosis? | Accessible |
| Does radiography advanced practice reduce time to treatment? | Accessible |
| Does radiography advanced practice reduce time to recovery? | Accessible |
| Does radiography advanced practice reduce service costs? | Efficient |
| Does radiography advanced practice improve patient satisfaction with service? | Acceptable |
Search strategy
The database searches were designed in collaboration with the university information specialist (DI) and the following databases were searched: Medline; Cinahl; Embase; Social Science and Citation Indexes; Health Management Information Consortium; Cochrane Central Register of Controlled Trials; Allied and Complementary Medicine Database; PsychINFO; and Applied Social Science Index and Abstracts. Index to Theses and OpenGrey were also searched to identify relevant grey literature. The search terms combined medical subject headings with free text words, as shown in Table 3, and were adapted for use across the different databases. Hand searching of the last year of key journals (Radiography; Journal of Medical Imaging and Radiation Sciences; and British Journal of Radiology), including articles in press, was undertaken, and the reference lists of included studies were scrutinized for additional studies. Where the searches identified a potentially relevant conference proceeding or academic thesis, the authors were contacted to request a copy of the presentation or thesis and any published articles pertaining to the work. The search was completed in September 2015 and was limited to articles published in English. No limitation on year of publication was applied, as the time frame for implementing advanced radiography practice globally has been varied. Articles were included in the review, if the PICOS (Population, Intervention, Comparator, Outcome, Study design) criteria (Table 3) were met.
Table 3.
PICOS (Population, Intervention, Comparator, Outcome, Study design) characteristics, inclusion criteria and search terms
| Characteristic | Inclusion criteria | Search terms |
|---|---|---|
| Population | Radiography profession | Professional title |
| Radiographer | ||
| Medical radiation technologist/MRT | ||
| Medical radiation practitioner | ||
| Medical radiation scientist | ||
| Medical imaging technologist | ||
| Radiation technologist/RT | ||
| Radiologica technologist | ||
| Radiation therapist | ||
| Radiation technician | ||
| Radiologist assistant | ||
| Physician assistant | ||
| Mammographer | ||
| Sonographer | ||
| Intervention | Advanced practice, role or scope | Advanced practice |
| Extenda practia | ||
| Extenda role | ||
| Role extension | ||
| Extenda scope | ||
| Expanda role | ||
| Role expansion | ||
| Expanda scope | ||
| Role development | ||
| Developa role | ||
| Advanca practia | ||
| Advanca Role | ||
| Advanca scope | ||
| Delegata role | ||
| Delegata practia | ||
| Role advancement | ||
| Non-medical consultant | ||
| Consultant practia | ||
| Delegata role | ||
| Delegata practia | ||
| Adjectives implying advanced practice—searched in combination with professional title to identify naming anomalies (e.g. extended role reporting radiographer) | Adjective extensions | |
| Extenda (N3) | ||
| Expanda (N3) | ||
| Advanca (N3) | ||
| Consultant (N3) | ||
| Clinical specialist (N3) | ||
| Comparator | Standard practice—not defined | Not searched |
| Outcomes | Service quality dimensions as specified in research questions | Not searched |
| Study design | Any primary study | Not searched |
Includes all words with preceding phrase.
N3 indicates identified words within three places of each other in a sentence.
Study selection
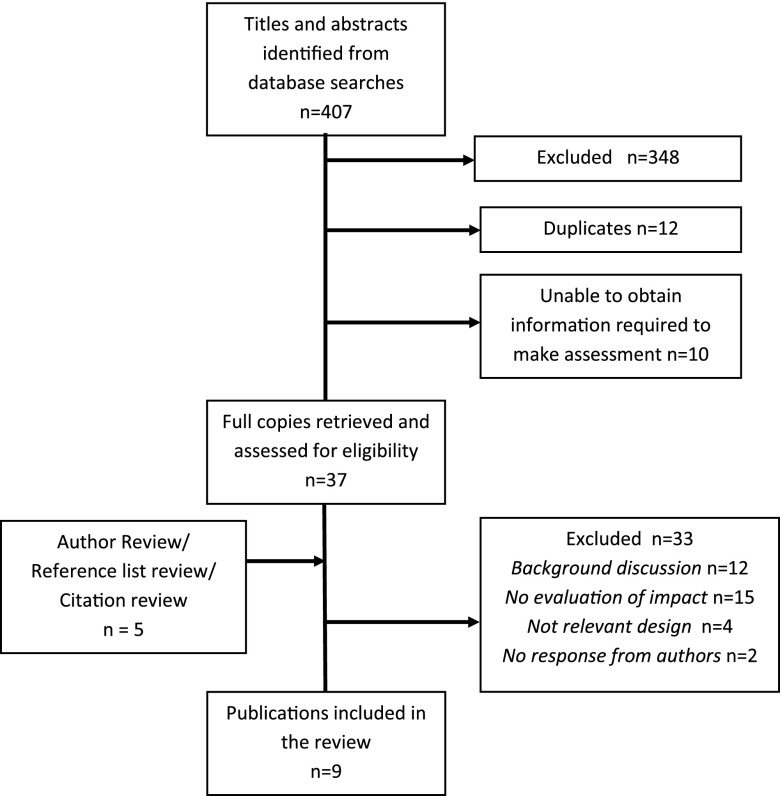
Inclusion eligibility was independently assessed by title and then abstract by two reviewers (LJ and RS). The reviewers were not blinded to authors or employing institutions during the study selection process. Decision-making around inclusion was based on the “rule out” principle, with articles being rejected only where lack of relevance to the study was certain. If uncertainty existed over whether an article should be included in the review, the article was retained. The full text of all retained articles was examined independently by at least two reviewers (LJ, RS, SB and MH) to make the final decision on inclusion. At each stage, any discrepancy in decision to include an article was resolved through consensus discussion. The flow diagram of the study selection process is detailed in Figure 1.
Figure 1.
Flow chart of the study selection process.
Quality assessment
The quality of each article was assessed by two reviewers. Where a member of the review team was also an author of an included study (MH) they were excluded from quality assessing their own work. Because of the variation in methodological design and content of included studies, quality assessment was undertaken using the Quality Assessment Tool for Studies with Diverse Designs developed by Sirriyeh et al.31 While this tool has not been widely utilized, the components fulfil the criteria for quality assessment as defined within Centre for Reviews and Dissemination guidance.27 The mean reviewer score was calculated to determine the quality score and articles were categorized as being of low (mean score: from 0% to <35.0%); moderate (mean score: from 35.0% to <70.0%) and high (mean score >70.0%) quality. Reviewer interrater agreement on article quality was high (kappa = 0.89). No articles were excluded from the final evaluation based on quality assessment ranking or score. Instead, quality assessment was used to determine the strength of evidence and relative confidence in findings in light of this.
Data extraction and synthesis
A purposeful data extraction form was designed to ensure that data relevant to answer the research questions were extracted. Data extraction was performed independently and blindly by two reviewers, with any differences of opinion being resolved by consensus discussion. Extracted data were inputted into a Microsoft Excel® (Microsoft, Redmond, WA) spreadsheet for comparison across studies. Owing to the heterogeneous nature of the studies and data, analysis was restricted to a narrative summary and synthesis.
RESULTS
Nine studies met the inclusion criteria (Figure 1; Table 4). The majority of studies (n = 7) focused on advanced radiography practice within the UK healthcare system, while two studies reflected North American practice (USA and Canada). The advanced practice activities considered were radiographer reporting;32–35 leading patient review clinics;36,37 and barium enema examination.38 Two articles considered the generic attributes of an advanced practice role per se, with a view to service efficiencies.39,40
Table 4.
Study characteristics
| Study | Country of origin | Advanced practice activity/focus | Study aim and overview | Research question addressed (service quality dimension) | Mean quality assessment grading |
|---|---|---|---|---|---|
| Brown and Desai, 200238 | UK | Radiographer-led barium enema examination | A single-site prospective study to determine the cost effectiveness of radiographer-performed barium enemas compared with those undertaken by a consultant radiologist | Reduction in service costs (efficient) | Low (26.2%) |
| Brealey et al, 200532 | UK | Radiographer reporting of appendicular skeletal radiographs | To determine the effect on patient management and costs of introducing radiographer appendicular reporting for patients with trauma at a single hospital site. A retrospective review of trauma cases 2 years before and after intervention | Reduction in patient morbidity (effective; safe) Reduction in service costs (efficient) |
Moderate (61.9%) |
| Jones and Robinson, 200839 | UK | Consultant radiographer | Reflective case study to illustrate the value of the four domains of non-medical consultant practice with respect to improving patient care and service delivery; specifically, examined a local (single site) intervention to reduce the volume of chest radiography referrals for NG tube position confirmation by replacing litmus paper with pH paper on wards and introducing radio-opaque NG tubes as standard across hospital. Costs of intervention determined relative to standard practice | Reduction in service costs (efficient) | Low (29.8%) |
| Leadership | |||||
| Service change | |||||
| Ludwig and Ferrara, 200840 | USA | RA role | A retrospective audit of clinical activity of RAs in training to associate a monetary value to their activity as an impact estimate for private practices mentoring advanced practice radiographers (RAs). Data included all procedures undertaken by an RA that could potentially be reimbursed by Medicare/Medicaid insurance | Reduction in service costs (efficient) | Low (27.4%) |
| McIlroy et al, 200836 | UK | Radiographer-/nurse-led treatment review clinic | A single-site prospective survey to determine the effectiveness of non-medical review during adjuvant radiotherapy for breast cancer | Patient satisfaction (acceptable) | Moderate (35.7%) |
| Hardy et al, 201333 | UK | Radiographer-led immediate reporting service for patients with musculoskeletal trauma | Pragmatic multicentre randomized controlled trial to determine if a radiographer-led immediate reporting service for patients with emergency musculoskeletal trauma is a cost-effective service improvement initiative. Individual variations in health outcomes between arms were calculated using EuroQol EQ-5D™ (EuroQol, Rotterdam, Netherlands) survey tool |
Reduction in patient morbidity (effective; safe) Reduction in service costs (efficient) Reduction in time to treatment (accessible) |
High (71.5%) |
| Hardy et al, 201334 | UK | Radiographer-led immediate reporting service for patients with musculoskeletal trauma | Pragmatic multicentre randomized controlled trial to determine if a radiographer-led immediate reporting service for patients with emergency musculoskeletal trauma reduces emergency department image interpretation errors and positively impacts on patient referral and treatment pathways | Reduction in patient morbidity (effective; safe) Reduction in time to treatment (accessible) |
High (71.5%) |
| Rozanec et al, 201437 | Canada | CSRT clinical review service | A prospective patient survey to determine patient satisfaction with a CSRT-led communication, review and support service for palliative patients at a single regional cancer centre | Patient satisfaction (acceptable) | Low (22.7%) |
| Lockwood, 201635 | UK | Radiographer CT head reporting | A retrospective analysis of audit data to determine the cost, risk and feasibility of introducing a skills mix approach to CT head reporting in clinical practice | Reduction in service costs (efficient) | Moderate (52.4%) |
CSRT, clinical specialist radiation therapist; NG, nasogastric; RA, radiologist assistant.
The articles were generally considered to be of low-to-moderate quality, evaluating advanced practice activities within a single centre and providing limited robust methodological information required to confirm study quality. With respect to the WHO quality dimensions,29 six studies considered cost reduction;32,33,35,38–40 three studies considered reduction in patient morbidity;32–34 two studies considered reduction in time to treatment;33,34 and two studies considered patient satisfaction.36,37 No studies considered or reported data relating to time to diagnosis, time to recovery or patient mortality.
Reduction in service costs
A summary of data related to service costs is provided in Table 5. Three studies focused on the impact of radiographer reporting on service costs, two studies in relation to musculoskeletal (MSK) trauma reporting (Brealey et al 200532; Hardy et al, 201333) and one study in relation to CT head reporting (Lockwood, in press35). All of these studies were considered to be of moderate-to-high quality, but the unique methodological and economic evaluation designs adopted prevented direct comparison of findings. However, all studies demonstrated that the implementation of radiographer reporting as an advanced practice activity had the potential to reduce service costs without compromising service quality. Importantly, opportunities for cost reduction identified by Brealey et al32 and Lockwood35 were predominantly as a consequence of the hourly earnings differential between radiographers and radiologists calculated as part of the role substitution model presented. As a result, the long-term potential for continued cost reduction in these models is limited by the number of reporting radiographers employed and volume and distribution of reporting workload. In contrast, the study by Hardy et al33 compared the economic impact of two reporting models (routine practice delayed reporting and radiographer-led immediate reporting). The cost reductions noted in this study reflected a reduction in short-stay hospital bed days and variation in treatment pathways between the two reporting models. Consequently, the identified opportunities for continued future cost reduction were not directly attributable to role substitution (radiographer for radiologist), but instead reflected the optimization of service delivery, both within and without the radiology department, through the use of advanced practice (reporting) radiographers.
Table 5.
Reduction in service costs
| Study | Country of origin | Advanced practice activity/focus | Service cost assessment | Study conclusions | ||
|---|---|---|---|---|---|---|
| Brown and Desai, 200238 | UK | Radiographer-led barium enema examination | Service cost was calculated as examination time × hourly staff salary costs (midpoint of scales using 2000/2001 salaries). The proportion of all staff costs was summed to determine the total examination cost and establish potential annual savings No consideration was given to examination reporting time, patient pre- or post- examination assistance, costs of using two rooms for radiologist arm; cost of antispasmodics in radiographer arm |
No significant difference in mean examination time between radiologist and radiographer Cost of radiologist-performed barium enema £17.87; cost of radiographer-performed barium enema £14.06. Cost saving of 21% Annual potential saving to hospital (assuming 1500 enema examination per year) by employing radiographers to undertake barium enema examinations = £5715 |
||
| Brealey et al, 200532 | UK | Radiographer reporting of appendicular skeletal radiographs | Radiographer reporting costs were based on time taken to report radiographic images plus capital and training costs related with service implementation. These were compared with radiologist costs related to interpreting and dictating report for a radiographic image. Costs were inflated to common year 2001/2002 Radiologist dictation time was used as proxy for secretarial report typing time but was not taken into account within baseline cost model. Radiographers typed own reports Three practice models compared to determine costs; developed to costs related to radiology department only and not to wider hospital economy (e.g. reduction in admissions and bed stays) |
Radiographer reporting costs/saving: base case analysis—£361 saving per annum; worst case scenario—£4524 cost per annum; best case scenario—£4528 saving per annum If radiographers had secretarial support for report typing, then cost per radiograph reported would decrease from £0.73 to £0.66 |
||
| Jones and Robinson, 200839 | UK | Consultant radiographer • Leadership • Service change |
Service cost equated to number of chest radiograph referrals before and after intervention Cost of 100 chest radiographs = £2100 (£21.00 each) Cost of 100 strips of pH paper = £15.85 (15.85p each) Post introduction of pH paper testing, chest radiography referrals reduced from 120 per month (£2520) to 50 per month (£1050) Cost reduction = £2520 − £1050 + £19.02 (120 pH papers) = £1489.02 per month |
“College of radiographers [reference 1 in jones paper] states that a consultant radiographer will initiate service developments and improve patient outcomes by implementing findings of clinical audit and clinical risk assessment” Case study demonstrates success of consultant role in achieving this but evaluation limited to service costs and does not evaluate patient outcomes |
||
| Ludwig and Ferrara, 200840 | USA | RA role | Procedures undertaken by RA were correlated with the most likely “CPT” code and associated professional component rate Total amount of potential reimbursement was estimated for each RA in training on the basis of the volume of procedures performed multiplied by the participant rate. Total RAs in training = 8 (single academic institution) Number of procedures performed per RA over 1500 clinical hours ranged from 501 to 711 (mean 581, median 536). Potential professional fee reimbursement ranged from $43,484 to $72,613 (mean $58,957, median $58,277) |
Reimbursement costs for some examinations include image reporting not undertaken by RA; therefore, reimbursement may be slightly overinflated Actual reimbursement may be higher once RAs are established in workforce Radiologists benefit most from participating in education of RAs, if practice is to employ RA on qualification |
||
| Hardy et al, 201333 | UK | Radiographer-led immediate reporting service for patients with MSK trauma | For cost-effectiveness analysis, patient health gain was measured in terms of change in utilities derived from EQ-5D™ responses at baseline and 8-week follow-up Resources used and costs of immediate reporting service were analyses at the patient level and compared with standard reporting practice. Measures included patient journey time, admission and recall rates. Standard NHS costs (2009/2010) were used to calculate financial cost of intervention and control arm reporting practice |
Using NHS unit costs, whole-episode costs for patients in the intervention arm were on average £23.40 less than for those in the control arm. Cost reduction was associated with a significant reduction in short-stay admissions Potential annual savings to the NHS was calculated to be £117 million (approximately £468,000 per hospital trust) Assuming annual trauma MSK attendance of 20,000 per hospital trust, 5–6 WTE reporting radiographers required to operate extended day reporting service (8 am–2 am) 7 days per week Assuming midpoint band 7 salary scale of £35,184 and 20% on costs, savings to hospital trust after employing additional reporting radiographers to operate service was £214,674 |
||
| Lockwood, 201635 | UK | Radiographer CT head reporting | Economic analysis based on annual number of CT head referrals at a single hospital trust and radiographer reporting of non-complex CT head examinations Modelling for radiologist and radiographer hourly costs was based on Netten et al ready reckoner for NHS staff costs and Unit Costs for Health and Social Care 2014 Three reporting time models (RCR; Department of Health; and CfWI) were compared |
Using RCR model, radiographer reporting would reduce cost of reporting activity by between £17 and £34 per patient and using CfWI between £20 and £41 per patient depending on reporting time taken Annual CT head referral data from NHS trust organization did not differentiate complex from non-complex examinations and therefore potential savings per hospital trust quoted (£124,757–£299,359) are likely to be overinflated |
CfWI, Centre for Workforce Intelligence; CPT, current procedural technology; MSK, musculoskeletal; NHS, National Health Service; RA, radiologist assistant; RCR, Royal College of Radiologists; WTE, whole time equivalent.
Considering advanced practice beyond image reporting, Brown and Desai38 considered the cost effectiveness of radiographers undertaking barium enema examinations. As no significant difference in examination time was noted between radiographers and radiologists, cost effectiveness was once again determined by the hourly earnings differential across the staff groups contributing to the examination predominantly as a role substitution initiative rather than service redesign and optimization.
Ludwig40 also considered the cost effectiveness of role substitution within the North American healthcare framework, calculating the potential health insurance reimbursement charges that might be attributable to employing a radiologist assistant (RA). Ludwig acknowledged limitations with the study design, specifically that the reimbursement values used included charges for image reporting, a task currently outside the scope of practice for RAs. The study was also based on a small cohort (n = 8) of RAs in training and therefore does not reflect actual costs and potential reimbursement levels post employment.
The final article (Jones and Robinson39) considered a more generic attribute of advanced and consultant radiographer practice—leadership in promoting service developments that improve patient outcomes. This study represented a personal reflection on the role of a consultant practitioner leading a practice change initiative related to reducing the number of chest radiograph referrals received at a single hospital trust for nasogastric tube positioning. The article demonstrated the benefits of multidisciplinary working and, like Hardy et al,33 demonstrated how a change in practice in one hospital area (the introduction of pH article for testing nasogastric tube exudate on the ward) can positively impact on resource use and cost effectiveness of services in another area (radiology). While the quality of this study was considered low and the cost reduction demonstrated relatively small, the principle of viewing cost effectiveness through the organizational lens rather than from the perspective of unidepartmental budgets is key to introducing the wider service efficiencies expected of healthcare organizations.
Reduction in patient morbidity
Three articles pertaining to two studies considered patient morbidity as a research outcome (Brealey et al32 and Hardy et al33,34). In both studies, the advanced practice activity was the reporting of trauma MSK images and evidence was considered to be of moderate-to-high quality. Brealey et al32 considered reattendance of patients to the emergency department (ED) or the X-ray department with the same complaint within 3 months of first attendance as a proxy for morbidity. Where this occurred, case notes and images were scrutinized to determine whether a reporting discrepancy had occurred. Where a discrepancy was found, the case was discussed by three independent radiologists to reach consensus opinion on whether any error in initial report was the cause of patient morbidity. 56 discrepant image reports were identified (27 reports before intervention and 29 reports after), but only 4 reports (2 reports before and 2 reports after implementing radiographer reporting) were considered to be clinically significant errors that affected patient management. The consistency in the volume of discrepant reports suggests that the accuracy of radiographer reporting is consistent with previous radiologist reporting and did not impact on patient morbidity. However, Brealey et al32 acknowledged that this approach to determining morbidity was flawed, owing to incomplete and missing patient notes and failure to capture non-reattendance data or reattendance at another hospital.
Hardy et al33,34 undertook a prospective randomized controlled trial and explored the influence of access to a radiographer report at the time of patient attendance (immediate reporting) on clinical decision-making within the ED compared with standard practice, as a determinant of potential morbidity. Patient reattendance with the same complaint within 2 weeks of initial attendance was also used as a proxy measure of morbidity along with completion of EQ-5D™ (EuroQol, Rotterdam, Netherlands41) health outcome survey at the time of attendance and 8 weeks post attendance. While EQ-5D™ is predominantly used for determining health gain through change in utility scores as part of cost-effectiveness analysis, any significant difference in score changes between the two arms of the study may represent persistent morbidity in one group. Hardy et al33,34 found that the number of interpretive errors by both radiographers and ED clinicians was significantly reduced in the intervention (immediate reporting) arm, suggesting that access to both patient and report was advantageous in clinical decision-making. Seven patients in each arm reattended within 2 weeks of initial attendance but in all cases, even where further tests and imaging were undertaken, no changes to diagnoses or treatment plans were made and patients were discharged as previously. Only 50.8% of initial EQ-5D™ survey respondents completed and returned the follow-up questionnaire at 8 weeks. Analysis of characteristics of survey respondents identified a significant reduction in follow-up responses from persons living in relatively deprived socioeconomic areas. While this finding suggested survey response bias, it was impossible to determine bias direction and therefore, it was assumed that follow-up data were representative of the whole sample. No significant difference was noted in the relative improvement of patients’ perceived health status across the study arms, suggesting that the intervention neither improved nor reduced reported patient morbidity.
Reduction in time to treatment
Only Hardy et al33,34 considered time to treatment as a measureable outcome. They defined this as time from arrival at the ED to time of discharge/referral from the ED. While the distribution of overall patient journey times was slightly positively skewed, no significant difference was noted in patient journey times between the two arms of the study. The additional time that a patient spent in the X-ray department while the images were being reported was estimated to be 5 min, but this time was balanced by a reduction in time spent in the ED awaiting a clinical decision. Importantly, the number of interpretive errors, and as a result patient recalls to the ED, was significantly reduced in the intervention arm, suggesting that while time to treatment is comparable, the correct treatment was more likely to be applied within the intervention arm.
Improvement in patient satisfaction
Two studies (McIlroy et al36 and Rozanec et al37) evaluated patient satisfaction in relation to new radiographer- or radiographer-/nurse-led treatment and review activities within the radiotherapy setting. McIlroy et al36 surveyed all patients attending for adjuvant breast or chest wall radiotherapy over a calendar year between July 2003 and June 2004 at a single centre in Scotland. As well as detail of patient experience, the survey explored patient satisfaction with clinical review process and any onward referral to medical/non-medical staff. In addition, patient demographic details were captured and treatment-induced skin reactions and patient well-being were monitored. 865 (n = 865/1095; 79.0%) questionnaires were returned and high patient satisfaction scores were noted in relation to time spent with review staff (99.7%) and ability to discuss all aspects of treatment and concerns with radiographers/nurses (99.1%). While the article was considered to be of moderate quality, limited data detail restricted the volume of evidence available for consideration in this review.
Rozanec et al37 was a peer-reviewed Canadian conference abstract. The full conference presentation was received from the authors on request, but no journal publication was available. The study explored patient satisfaction with the clinical specialist radiation therapist role as the main contact for patients attending a single centre in ON for palliative radiation treatment. 33 patients were recruited into the study between April and November 2013 (19 patients into clinical specialist radiation therapist intervention arm and 14 patients into standard treatment arm). A modified patient satisfaction survey based on a validated survey used within the Rheumatism research unit at the University of Leeds, UK, was distributed to each patient on their last day of radiotherapy. Patient responses indicated significant improvement in satisfaction within the intervention group in relation to the statements “I was told everything that I want to know about my condition” and “I felt that the problem that I came with was sorted out properly”, with no difference between arms in relation to other survey questions. Despite the low-quality grading of this study and small sample size, the findings of the studies by both Rozanec et al37 and McIlroy et al36 suggest that radiographer role expansion to include greater patient interaction as part of the clinical review process is of some benefit to patients.
DISCUSSION
While a large number of articles related to advanced practice in radiography were identified, very few considered the impact of advanced practice, or a defined advanced practice activity, on service quality or patient outcomes. Instead, studies regularly compared task outcomes between the delegating and substituting professions. While these data may have some value for service organizations auditing task achievement levels across multidisciplinary groups, caution is urged when using these data to evidence service quality. Radiographer role advancement is often linked with undertaking tasks and roles previously undertaken by medical colleagues but as radiographers undertake these tasks within a radiography rather than medical paradigm, it can be argued that the outcomes are not directly comparable. A further criticism of the large majority of studies, both included and excluded from this review, is the reporting of practice interventions at a single clinical site with relatively small sample sizes and little transferability within country or across global regions. Combine this with the multiple research designs, data collection tools and approaches to analysis adopted, the evidence base surrounding the impact of advanced practice in radiography on patient outcomes and health service quality is limited.
Interestingly, the majority of studies reviewed addressed the efficiency domain of service quality, with six studies32,33,35,38–40 considering the potential cost effectiveness of advanced practice. In contrast, only two studies36,37 considered the acceptable domain and evaluated patient satisfaction, with an intervention undertaken by advanced practice radiographers. The emphasis on cost effectiveness and interprofessional comparison perhaps reflects the professional priorities at the time when advanced practice roles were being introduced and the questions of “are radiographers as good as…?” and “will this cost [the organization] money?” were paramount. The evidence considered in this review suggests that significant cost efficiencies are possible to both the hospital organization and department through service redesign, role substitution and pay differentials. Consequently, while service efficiency remains a priority to address austerity measures within healthcare globally, researchers looking to evaluate the impact of advanced practice in radiography need to look beyond role comparison and cost efficiencies to determine the wider impact of advanced practice working.
Only two studies comprising three articles32–34 explored patient morbidity. Both studies were of moderate-to-high quality, and the evidence presented suggests that patient morbidity episodes do not increase when radiographer reporting of trauma MSK images is introduced, regardless of the timing of report availability. Similarly, time to treatment was not adversely affected, although importantly, in the study by Hardy et al,33,34 the introduction of radiographer-led immediate reporting and availability of an image report at the time of patient attendance within the ED did reduce the number of false-negative diagnoses and subsequent patient recalls for treatment. Consequently, it might be assumed that patient morbidity may be reduced owing to improvements in clinical diagnosis and treatment at initial presentation, and the findings of this study have been incorporated within National Institute for Health and Care Excellence guidance.42
Limitations
The search terms used in this review did not define the advanced practice activity or task but instead accepted that variation in understanding of what tasks and roles constitute advanced practice exist globally. Consequently, articles that did not include reference to the radiographer as an advanced practitioner or similar (Table 3) or the task as advanced practice will not have been recovered and considered for inclusion. Importantly, no articles meeting the inclusion criteria considered sonography as advanced practice. This perhaps reflects the established nature of the sonographer's role in the UK and limited non-medical sonography development in Europe and globally.
CONCLUSION
Radiographer advanced practice is an established role across both the diagnostic and therapeutic arms of the profession in the UK and internationally. However, evidence of the impact of these roles in terms of patient outcomes and service quality is limited. Despite this, there is some evidence to support the positive contribution of advanced practice in terms of service efficiencies, patient outcomes and acceptability. If advanced practice in radiography is to be based on a robust evidence base, more work is required to look at the impact of service innovations through the lens of assuring service quality and patient outcomes. In addition, this needs to be considered beyond individual hospitals and trusts and adopt robust research designs, if the evidence is to represent the profession as a whole and be used confidently to promote future radiography role innovations. Without greater exploration of the impact of advanced practice on service quality and patient outcomes, and a move away from comparing task achievement across delegatory and substitute professional groups, we are in danger of prioritizing task over contribution to service when defining advanced practice roles within radiography and limiting the future potential of the profession.
Contributor Information
Maryann Hardy, Email: M.L.Hardy1@bradford.ac.uk.
Louise Johnson, Email: loobyloo13@icloud.com.
Rachael Sharples, Email: Rachael.Shaples@suerydercare.org.
Stephen Boynes, Email: S.boynes@bradford.ac.uk.
Donna Irving, Email: D.Irving@bradford.ac.uk.
REFERENCES
- 1.Alderson CJ, Hogg P. Advanced radiographic practice—the legal aspects. Radiography 2003; 9: 305–14. doi: 10.1016/j.radi.2003.10.001 [DOI] [Google Scholar]
- 2.Nightingale J, Hogg P. Clinical practice at an advanced level: an introduction. Radiography 2003; 9: 77–83. doi: 10.1016/S1078-8174(03)00005-1 [DOI] [Google Scholar]
- 3.Dixon AM. Education and training for advanced practice: principles of course design and assessment applied to a ‘stereotactic needle core biopsy of the breast’ module. Radiography 2006; 12: 79–87. doi: 10.1016/j.radi.2005.03.001 [DOI] [Google Scholar]
- 4.Hardy M, Snaith B. Role extension and role advancement—is there a difference? A discussion paper. Radiography 2006; 12: 327–31. doi: 10.1016/j.radi.2005.09.004 [DOI] [Google Scholar]
- 5.Snaith B, Hardy M. How to achieve advanced practitioner status: a discussion paper. Radiography 2007; 13: 142–6. doi: 10.1016/j.radi.2006.01.001 [DOI] [Google Scholar]
- 6.Eddy A. Advanced practice for therapy radiographers—a discussion paper. Radiography 2008; 14: 24–31. doi: 10.1016/j.radi.2006.07.001 [DOI] [Google Scholar]
- 7.Department of Health. Agenda for change—final agreement. London: HMSO; 2004. [Google Scholar]
- 8.Smith T, Yielder J, Ajibulu O, Caruana E. Progress towards advanced practice roles in Australia, New Zealand and the Western Pacific. Radiography 2008; 14(Suppl. 1): e20–3. doi: 10.1016/j.radi.2008.04.002 [DOI] [Google Scholar]
- 9.May L, Martino S, McElveny C. The establishment of an advanced clinical role for radiographers in the United States. Radiography 2008; 14(Suppl. 1): e24–7. doi: 10.1016/j.radi.2008.04.007 [DOI] [Google Scholar]
- 10.Canadian Association of Medical Radiation Technologists. Advanced Practice in Medical Radiation Technology: A Canadian Framework. Available from: http://www.camrt.ca/mrt-profession/professional-resources/advanced-practice/. Updated 17th December 2015. [Google Scholar]
- 11.Australian Institute of Radiography. Pathway to Advanced Practice: summary document and guidelines for application for accreditation 2014. [Updated 1 April 2016.] Available from: http://www.air.asn.au/advanced.php [Google Scholar]
- 12.American Society of Radiologic Technology. The practice standards for medical imaging and radiation therapy (Glossary), 2014. [Updated 1 April 2016.] Available from: http://www.asrt.org/docs/default-source/Practice-Standards-Proposed/glossary_postpubliccomment.pdf?sfvrsn=2 [Google Scholar]
- 13.Society & College of Radiographers. Diagnostic Radiography UK workforce report 2014. Available from: https://www.sor.org/learning/document-library/diagnostic-radiography-uk-workforce-report-2014. Updated 17th December 2015. [Google Scholar]
- 14.Department of Health. Radiography skills mix: a report on the four-tier service delivery model. London, UK: HMSO; 2003. [Google Scholar]
- 15.Royal College of Radiologists. Investing in the clinical radiology workforce: the quality and efficiency case, 2012. Available from: https://www.rcr.ac.uk/sites/default/files/RCR_CRWorkforce_June2012.pdf. Updated 18th December 2015. [Google Scholar]
- 16.Centre for Workforce Intelligence. Securing the future workforce supply: clinical radiology stocktake, 2012. Available from: http://www.cfwi.org.uk/publications/securing-the-future-workforce-supply-clinical-radiology-stocktake. Updated 18th December 2015. [Google Scholar]
- 17.National Health Service. Five year forward view. London, UK: NHS; 2014. [Google Scholar]
- 18.Department of Health. Liberating the NHS: developing the healthcare workforce from design to delivery. London, UK: Department of Health; 2012. [Google Scholar]
- 19.National Imaging Clinical Advisory Group. Implementing 7 day working in imaging departments: good practice guidance. London, UK: Department of Health; 2013. [Google Scholar]
- 20.Gill E. Radiographer role extension in gynaecological brachytherapy. Clin Oncol 2007; 19(Suppl. 3): s30. doi: 10.1016/j.clon.2007.01.361 [DOI] [Google Scholar]
- 21.Lawson S. Consultant radiographer-led ultrasound-guided vacuum assisted excision biopsy. Ultrasound 2008; 16: 234–7. doi: 10.1179/174313408X321012 [DOI] [Google Scholar]
- 22.Monk CM, Wrightson SJ, Smith TN. An exploration of the feasibility of radiation therapist participation in treatment reviews. J Med Radiat Sci 2013; 60: 100–7. doi: 10.1002/jmrs.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy M, Loughran CF, Birchenough H, Savage J, Sutcliffe C. A comparison of radiographer and radiologist reports on radiographer conducted barium enemas. Radiography 2002; 8: 215–21. doi: 10.1053/radi.2002.0384 [DOI] [Google Scholar]
- 24.England A, Best A, Friend C. A comparison of radiographers and radiologists in CT based measurements of abdominal aortic aneurysms. Radiography 2010; 16: 321–6. doi: 10.1016/j.radi.2010.02.008 [DOI] [Google Scholar]
- 25.Lauridsen C, Lefere P, Gerke O, Hageman S, Karstoft J, Gryspeerdt S. Comparison of the diagnostic performance of CT colonography interpreted by radiologists and radiographers. Insights Imaging 2013; 4: 491–7. doi: 10.1007/s13244-013-0260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spilsbury K, Meyer J. Defining the nursing contribution to patient outcome: lessons from a review of the literature examining nursing outcomes, skill mix and changing roles. J Clin Nurs 2001; 10: 3–14. doi: 10.1046/j.1365-2702.2001.00423.x [DOI] [PubMed] [Google Scholar]
- 27.Centre for Reviews and Dissemination. Systematic Reviews: CRD’s guidance for undertaking reviews in health care, 2009. Available from: https://www.york.ac.uk/crd/guidance/. Updated 17th December 2015. [Google Scholar]
- 28.University of Oxford. PRISMA: transparent reporting of systematic reviews and meta-analysis, 2009. [Updated 1 April 2016.] Available from: http://prisma-statement.org/ [Google Scholar]
- 29.World Health Organization. Quality of Care: a process for making strategic choices in health systems. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 30.NHS England. What do we mean by high quality care? Available from: https://www.england.nhs.uk/about/our-vision-and-purpose/imp-our-mission/high-quality-care/. Updated 17th December 2015. [Google Scholar]
- 31.Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract 2012; 18: 746–52. doi: 10.1111/j.1365-2753.2011.01662.x [DOI] [PubMed] [Google Scholar]
- 32.Brealey S, King DG, Hahn S, Godfrey C, Crowe MT, Bloor K, et al. The costs and effects of introducing selectively trained radiographers to an A&E reporting service: a retrospective controlled before and after study. Br J Radiol 2005; 78: 499–505. doi: 10.1259/bjr/51196310 [DOI] [PubMed] [Google Scholar]
- 33.Hardy M, Hutton J, Snaith B. Is a radiographer led immediate reporting service for emergency department referrals a cost effective initiative? Radiography 2013; 19: 23–7. doi: 10.1016/j.radi.2012.11.002 [DOI] [Google Scholar]
- 34.Hardy M, Snaith B, Scally A. The impact of immediate reporting on interpretive discrepancies and patient referral pathways within the emergency department: a randomised controlled trial. Br J Radiol 2013; 86: 20120112. doi: 10.1259/bjr.20120112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lockwood P. An economic evaluation of introducing a skills mix approach to CT head reporting in clinical practice. Radiography 2016; 22: 124–30. doi: 10.1016/j.radi.2015.09.004 [DOI] [Google Scholar]
- 36.McIlroy P, McIntyre A, Ross A, Gallagher C, Brown C. Breast radiotherapy: a single centre survey of non-medical weekly patient review. J Radiother Pract 2008; 7: 19–29. doi: 10.1017/S146039690700622X [DOI] [Google Scholar]
- 37.Rozanec N, Smith S, Wells W, Moyo E, Zychla L, Harnett N. Patient satisfaction with the role of a clinical specialist radiation therapist in palliative care, J Med Imaging Radiat Sci 2014; 45: 167–8. doi: 10.1016/j.jmir.2014.03.026 [DOI] [Google Scholar]
- 38.Brown L, Desai S. Cost-effectiveness of barium enemas performed by radiographers. Clin Radiol 2002; 57: 129–31. doi: 10.1053/crad.2001.0831 [DOI] [PubMed] [Google Scholar]
- 39.Jones HC, Robinson L. A reflection on the role of an emergency care consultant radiographer in achieving appropriate imaging conditions for nasogastric tube positioning. Radiography 2008; 14(Suppl. 1): e11–4. doi: 10.1016/j.radi.2008.11.001 [DOI] [Google Scholar]
- 40.Ludwig R, Ferrara TL. What is your radiologist assistant worth to you? J Am Coll Radiol 2008; 5: 115–8. doi: 10.1016/j.jacr.2007.10.018 [DOI] [PubMed] [Google Scholar]
- 41.Euroquol. What is EQ-5D? Available from: http://www.euroqol.org/. Updated 18th December 2015. [Google Scholar]
- 42.National Institute for Health & Care Excellence. Fractures (non-complex): assessment and management [NG38]. Available from: https://www.nice.org.uk/guidance/NG38. Updated 1st March 2016. [Google Scholar]