Abstract
The endogenous social support systems of young Black men who have sex with men (YBMSM), like surrogate families and social networks, are considered crucial assets for HIV prevention in this population. Yet, the extent to which these social systems foster sexual health protections or risks remains unclear. We examine the networked patterns of membership in ballroom houses and independent gay families, both Black gay subcultures in the United States, and how these memberships are related to HIV protective and risk traits of members. Drawing from a population-based sample of 618 YBMSM living in Chicago between June 2013 and July 2014, we observe a suite of protective and risk traits and perform bivariate analyses to assess each of their associations with being a member of a house or family. We then present an analysis of the homophilous and heterophilous mixing on these traits that structures the patterns of house and family affiliations among members. The bivariate analyses show that members of the house and family communities were more likely than non-members to report protective traits like being aware of PrEP, having health coverage, having a primary care doctor, and discouraging sex drug use among peers. However, members were also more likely to engage in the use of sex drugs. With respect to how these traits inform specific house/family affiliations, results show that members who had a recent HIV test, who were PrEP aware, or who engaged in exchange sex were more likely to belong to the same house or family, while HIV positive individuals were less likely to cluster within houses or families. These findings provide insights regarding the strengths and vulnerabilities of the house and gay family communities that can inform more culturally specific interventions that build on the existing human and social capital in this milieu.
INTRODUCTION
Despite indications that new HIV infections in the United States are plateauing, some groups remain disproportionately affected. One such group is young Black men who have sex with men (YBMSM), for whom rates of new infection continue to climb (Millett et al., 2012). Between 2005 and 2014 new HIV diagnoses among YBMSM increased 87% (CDC, 2014) and data suggest that if current rates continue, about 1 in 2 Black gay or bisexual men in the U.S. will be diagnosed with HIV in their lifetime (CDC, 2016). Taken together, these statistics paint a picture of intersectional risk based on race and sexual orientation for a population facing further marginalization on the basis of disproportionate rates of HIV infection.
Existing public health interventions to disrupt and reverse rates of new infection in this population have some noteworthy limitations. First, interventions for YBMSM are often appropriated from models devised for White MSM or MSM in general. This ignores important differences between YBMSM and their White counterparts, particularly with respect to their complex intersectional identity structures (Bowleg, 2008; Peek et al., 2016; Purdie-Vaughns & Eibach, 2008). For example, an African American, gay or bisexual, cisgender man whose masculine presentation conforms to social expectations of Black masculinity may choose to not challenge assumptions that he is straight or declare his sexual orientation within Black heterosexual spaces in an effort to avoid discrimination. Their management of the potential threat of heterosexist discrimination may affect their willingness to engage in HIV preventive care in Black heterosexual spaces while their management of the potential threat of racist discrimination may affect their willingness to engage in HIV preventive care in White spaces. Thus, interventions that ignore the interactive effects of multiple social identities run the risk of misunderstanding how the cumulative lived experience of YBMSM contributes to HIV disparities and within-group differences among LGBT individuals (Peek et al., 2016).
Relatedly, most intervention approaches ignore the endogenous social and cultural systems that could be leveraged to reduce risk and offer support for YBMSM, for example the elective kinship structures that exist among African American LGBT peoples, most notably those in the house and ballroom communities and in independent gay families. Systems of queer kinship play an important role in the Black gay community, namely as responses to disenfranchisement from biological and other heteronormative systems of support. In these social environments, YBMSM (re)construct kinship, forging homes and family ties on their own terms (Arnold & Bailey, 2009). Learning how these systems of resilience factor into the sexual health decisions of YBMSM would enable more culturally appropriate responses to HIV prevention and outreach and bring much needed attention to methods of support that already exist within at-risk communities.
Despite their promise, however, public health officials have paid little attention to kinship groups, especially with respect to the prevention practices that emerge therein (Arnold & Bailey, 2009; Friedman et al., 2004). Rather, where attention is paid, it tends to underscore rates of risk in these communities as a mandate for outside intervention (Murrill et al., 2008). Thus, there is a need to leverage and perturb these systems, warranting a closer examination of the relationship between membership in these communities and protective and risk behaviors.
Our study takes a step toward filling these knowledge gaps so that more effective and culturally specific HIV interventions can be developed that meet the needs of YBMSM while harnessing systems of support already in place. We take as our starting point the notion that membership in kinship groups is yet another possible socio-cultural grouping in the complex intersectional identity structures of YBMSM that is likely to affect the sexual health practices among its members. Specifically, we examine kinship structures within ballroom houses, which adopt family-like structures and support the larger competitive ballroom scene (Arnold & Bailey, 2009), and their independent, non-ball counterparts, herein referred to as families.
This paper seeks to fill two noticeable gaps in the established literature. First, although studies have explored the behavioral characteristics of members of the house and family communities, little to no work exists that compares members of these communities to their non-member YBMSM counterparts. We argue that understanding the differences between members and non-members is a crucial step toward unpacking the diversity of the larger YBMSM community and the relative benefits and challenges that come with identifying with this subcultural community. For this reason,, we observe a suite of HIV-related protective and risk factors among a large cohort of YBMSM and determine whether they are more or less associated with membership in the house and/or family communities..
Second, individual houses and families provide contexts, or social foci (Feld, 1981), that anchor social interactions among members. As such, it is important to understand how house-and family-based relationships can confer HIV related risks and/or protections to its members. That said, research has been limited with respect to studying the relational dynamics within these settings and their implications for HIV prevention. To help fill this void, we present a network clustering analysis to demonstrate the tendency for members who exhibit various risk and protective traits to concentrate within individual houses and families. We conclude with some implications of our findings and delineate some directions for future research.
Houses and Families and their HIV Prevention Potential
For young Black gay, bisexual and transgender individuals, the challenges of being African American, a sexual or gender minority, young, and low socio-economic status can result in a host of stressors that impact individual well-being (Horne, Levitt, Sweeney, Puckett, & Hampton, 2014; Wong, Schrager, Holloway, Meyer, & Kipke, 2014). In many ways, gay families emerge in response to these challenges and help their members overcome rejection from mainstream cultural communities (Horne et al., 2014; Kubicek, McNeeley, Holloway, Weiss, & Kipke, 2013; Levitt, Horne, Puckett, Sweeney, & Hampton, 2015). Like their heteronormative counterparts, gay family structures embrace specific family roles (e.g., mother, father, sibling) that are used as vehicles to communicate norms and values across generations (Stack & Burton, 1993). For these reasons, kinship structures may also serve as culturally relevant mechanisms for conveying norms around HIV.
The limited scholarly attention given to queer kinship among African American LGBT youth is concentrated around the house and ballroom communities (Horne et al., 2014). House culture (or ballroom culture) is a clandestine, minoritarian community of African American and (in some locations) Latino/a LGBT people (Arnold & Bailey, 2009; Bailey, 2009). House culture is organized around two interdependent features: (1) the anchoring family-like structures, called houses, and (2) the competitive performances of gender and sexuality, dance and fashion that houses participate in (Arnold & Bailey, 2009). In addition to families that emerge within ballroom houses, independent gay families provide the same kind of familial support and relational structure as ballroom houses but without the added pressures of competition. In that their support is not contingent on winning competitions, it has been posited that independent gay families may be more stable sources of guidance (Dickson-Gomez et al., 2014; Horne et al., 2014).
Research regarding the role that kinship groups play in promoting sexual health and HIV prevention can be organized into two strands. One strand focuses on the prevalence of HIV and other related risk factors in the community. In general, these studies note high rates of seroprevalence, lower rates of testing, engagement in condomless sex, as well as practices like age-discordant coupling and exchange sex that increase exposure to risk (Castillo, Palmer, Rudy, & Fernandez, 2012; Lemos, Hosek, & Bell, 2015).
Another strand of research focuses on the cultural practices within the house community that enable or constrain their own prevention efforts. Out of this, there is widespread agreement that as the sources of care and service to its members, houses and independent gay families provide essential ingredients for dealing with HIV (Arnold & Bailey, 2009; Bailey, 2009; Kubicek et al., 2013). However, concern has also been raised about dynamics in these spaces that may hamper prevention efforts if not simultaneously addressed, for example status hierarchies that motivate young members to achieve acceptance at all costs (Lemos et al., 2015). Dynamics like thissuggest a more complicated picture of the HIV prevention potential of these support structures. For this reason, we focus our attention on the ability of houses and families to support the traits and behaviors that will either enable or constrain HIV prevention for its members.
METHODS
Data Collection Procedures
The data used in this study were collected from June 2013 to July 2014 as part of the the uConnect study, a network cohort study of young Black men who have sex with men (YBMSM) living on the southside of Chicago and adjacent Black suburbs (Khanna et al., 2016). Participants were recruited using a variant of classic link-tracing called Respondent Driven Sampling (RDS) (Heckathorn, 1997). Widely used in public health studies (Goel & Salganik, 2010), RDS enables valid statistical inference of “hard to reach” populations (e.g., intravenous drug-users, sex workers, men who have sex with men) by providing a design for sampling as well as a methodology for estimating statistical properties of the target population.
To generate our sample, we began with a group of 62 RDS seeds drawn from a variety of social spaces that YMSM occupy, including community social spaces, online venues, community-based organizations, and HIV treatment and prevention programs. Focal participants were eligible to be interviewed if they: 1) self-identified as African American or Black, 2) were assigned male at birth, 3) were between 16 and 29 years of age (inclusive), 4) reported oral or anal sex with a male within the past 24 months, and 5) were willing and able to provide informed consent at the time of the study visit. Each respondent was given up to six vouchers to recruit others who met the same eligibility criteria. Respondents received $60 for their participation and $20 for each successful recruit enrolled into the study (Khanna et al., 2016).
RDS sampling procedures resulted in a final sample of 618 YBMSM. Each participant completed an interviewer-administered questionnaire, which included modules pertaining to individual demographics, sexual health and risk behaviors, affiliations with minority subcultures within the gay community, and relational information about participants’ sexual and social networks.
Measures
YBMSM Attributes
Socio-structural conditions
Participants were asked about several socio-structural factors deemed relevant to HIV vulnerability, including whether they had ever been incarcerated, whether they had been homeless at any point in the last 12 months, whether they were currently unemployed (i.e., not working, not a student), whether they had experienced instances of financial hardship in the last 6 months (i.e., running out of money to meet their basic needs), and whether they had health insurance.
Sexual health
Sexual health variables pertaining to the current study included whether participants were HIV seropositive (based on lab results) and whether they had been tested for HIV within the last 6 months if the participant was HIV negative. Also included in the suite of sexual health variables are measures of whether participants reported having heard of pre-exposure prophylaxis (PrEP), whether they have a primary care doctor, whether they had ever participated in an HIV program or intervention, and whether they reported having had a counseling session with a prevention counselor in the past 12 months.
Sex Behaviors
The study examined four measures of sexual risk-taking. Condomless sex was measured on the basis of frequency of condom use with named anal sex partners in the past 6 months. If the respondent indicated not always using condoms with any of their partners, he/she was coded as having had condomless sex. Similarly, respondents were asked about their use of drugs to enhance their sexual experience or make sex easier to get (Schneider et al., 2013). Respondents who indicated having done so with at least one partner were coded as having used sex drugs. Group sex is a self-reported measure of whether or not a respondent indicated having engaged in sex with two or more partners at the same time at least once in the past 12 months (Schneider et al., 2013). Finally, respondents were asked to indicate whether they had engaged in exchange sex (i.e., “sex for favors”) as a source of income in the past 12 months.
Intravention behaviors
We examined a suite of intraventions pertaining to three of the sex behaviors described above. Regarding condom use, participants were asked to indicate (i) whether they have encouraged condom use among the MSM they know and (ii) whether they have received encouragement to use condoms from the MSM they know. Intraventions pertaining to sex related substance use were measured on the basis of (iii) whether they have discouraged drug use or alcohol use to enhance sexual experience among the MSM they know. Finally, the group sex intravention was operationalized as (iv) having discouraged group sex among the other MSM they know.
Membership in Houses and Families
The first portion of the analysis features a binary independent measure of House/Family Membership. Respondents were asked to indicate (yes or no) whether they were members of the house and/or family communities by answering the following two questions: 1) “Are you a member of a House in the Ballroom Community?” and 2) “Are you a member of a Gay Family?.” Responses to these questions were then used to construct a dummy variable to represent whether a participant was a member of either a house or family (House or Family member = 1, not a member of a House or Family = 0).
The house/family social affiliation network
In the second portion of the analysis, House and Family memberships are operationalized as dependent network ties between YBMSM and the specific ballroom houses and/or indepentent gay families to which they belong. As such, only the individuals who named, when prompted, the house or family to which they belonged were included in this network. This yielded a two-mode network of 168 YBMSM and a total of 37 houses and families. Analysis is performed on a transformation of this two-mode network, which converts its two-mode rectangular data structure into a one-mode adjacency matrix of YBMSM whose ties to one another represent membership in the same house or family.
Statistical Analysis
Univariate and bivariate analyses were performed in the Stata Statistical Software package, Version 14. The bivariate analyses allowed us to see whether the attributes described above were more or less likely to exist among members than among non-members. We report odds ratios to show the extent to which individual factors associated with HIV prevention and risk increase the likelihood of being a member of the house or gay family communities. RDS weights were calculated using Gile’s Sequential Sampling (SS) estimator (Gile & Handcock, 2010)(Gile & Handcock, 2010)(Gile & Handcock, 2010)(Gile & Handcock, 2010)(Gile & Handcock, 2010) and all models were estimated using these weights.
Network statistical techniques were performed in UCINET 6.596 for Windows (Borgatti, Everett, & Freeman, 2002). Specifically, we use the join-count procedure in UCINET to test for homophilous and heterophilous mixing on binary actor attributes in the one-mode transformation of the house/family affiliation network. Join-count statistics relate mixing on a binary actor attribute in an observed undirected network matrix to a distribution of matrices generated randomly. For each protective or risk trait tested, p-values are produced for three possible trait combinations, yes-yes, no-no, and yes-no. We refer to these combinations as homophily+, homophily-, and heterophily, respectively. A homophily+ combination (yes-yes) corresponds to a co- house/family membership tie between two people that have the behavioral trait (e.g., having condomless sex). Conversely, a homophily- combination (no-no) corresponds to a co-membership tie between individuals that do not adopt the behavior (e.g., not having condomless sex). Meanwhile, a heterophily combination (yes-no) represents a co-membership tie between a person that does engage in the behavior and a person that does not.
RESULTS
Risk and protective factors associated with being a house or family member
To begin, Table 1 shows the prevalence of risk and protective traits among the full YBMSM sample (N=618) as well as the stratified breakdown between house and family members and non-members. In Table 2 we report the associations between each protective and risk factor with house/family membership in terms of odds ratios derived from bivariate logistic regression analysis. In total, 206 respondents reported being a member of a ballroom house and/or gay family, 408 reported not being members of either. Four respondents did not give a response to these questions and were, therefore, excluded from the analysis.
Table 1.
Prevalence of HIV-related protective and risk factors among YBMSM, non-stratified results and results stratified by membership in a ballroom house or independent gay family
| YBMSM Attributes | Full sample (n=618) |
Member of a House or Family |
|
|---|---|---|---|
| Yes (n=206) |
No (n=408) |
||
| Socio-structural factors | |||
| Criminal justice involvement | 285 (46.2) | 104 (50.5) | 179 (43.9) |
| Housing instability (last 12 months) | 155 (25.2) | 57 (27.8) | 96 (23.7) |
| Unemployment | 194 (31.4) | 72 (35.0) | 120 (29.4) |
| Financial hardship | 264 (43.3) | 89 (44.3) | 171 (42.2) |
| No Health Insurance | 271 (44.9) | 88 (43.8) | 181 (45.8) |
| Sexual health traits | |||
| HIV seropositive | 213 (34.5) | 79 (38.4) | 134 (32.8) |
| Timely testing (in last 6 months, if HIV-) | 247 (70.0) | 88 (69.3) | 156 (56.9) |
| Prep awareness | 250 (40.8) | 103 (50.2) | 146 (36.1) |
| Primary care doctor | 341 (55.7) | 128 (62.8) | 211 (52.0) |
| Participation in an HIV prevention program | 171 (27.9) | 71 (34.5) | 100 (24.6) |
| Counseling session with a prevention counselor | 276 (45.7) | 105 (52.0) | 170 (42.5) |
| Sex behaviors | |||
| Condomless sex | 299 (49.9) | 99 (50.0) | 199 (49.9) |
| Sex drug use | 251 (41.9) | 90 (45.5) | 159 (39.9) |
| Group sex | 113 (18.5) | 33 (16.0) | 80 (19.9) |
| Exchange sex | 73 (11.9) | 33 (15.2) | 42 (10.5) |
| Intravention behaviors | |||
| Encouraged condom use | 515 (85.0) | 182 (89.7) | 330 (82.7) |
| Received encouragement to use condoms | 462 (76.4) | 162 (79.8) | 297 (74.6) |
| Discouraged alcohol or drug use to enhance sex | 242 (39.9) | 93 (45.8) | 148 (37.0) |
| Discouraged group sex | 211 (34.8) | 75 (37.0) | 135 (33.8) |
Table 2.
Associations between being a member of a ballroom house or independent gay family and HIV-related risk and protection factors
| Respondent is a member of a ballroom house or independent gay family |
|
|---|---|
| Odds Ratio (95% CI) | |
| Socio-structural factors | |
| Criminal justice involvement | 1.10 (0.71–1.70) |
| Housing instability (last 12 months) | 1.39 (0.85–2.27) |
| Unemployment | 1.18 (0.73–1.90) |
| Financial hardship | 0.89 (0.57–1.39) |
| No Health Insurance | 0.58 (0.37–0.91)* |
| Sexual health traits | |
| HIV seropositive | 1.33 (0.84–2.13) |
| Timely testing (in last 6 months, if HIV-) | 1.53 (0.86–2.73) |
| Prep awareness | 1.86 (1.18–2.92)** |
| Primary care doctor | 1.80 (1.13–2.86)* |
| Participation in an HIV prevention program | 1.15 (0.71–1.87) |
| Counseling session with a prevention counselor | 1.03 (0.66–1.61) |
| Sex behaviors | |
| Condomless sex | 1.14 (0.73–1.79) |
| Sex drug use | 1.60 (1.01–2.52)* |
| Group sex | 0.80 (0.43–1.47) |
| Exchange sex | 1.12 (0.56–2.12) |
| Intravention behaviors | |
| Encouraged condom use | 1.31 (0.66–2.62) |
| Received encouragement to use condoms | 1.25 (0.72–2.17) |
| Discouraged alcohol or drug use to enhance sex | 1.58 (1.00–2.48)* |
| Discouraged group sex | 0.85 (0.61–1.20) |
p<.05;
p<.01
Socio-structural factors
Of the socio-structural factors we examined, only health coverage was significantly associated with membership in the house and family communities. Specifically, our results show that uninsured individuals were less likely than expected to be house or family members (OR=0.58; 95% CI: [0.37–0.91]). All other socio-structural vulnerabilities seemed to be experienced equivalently among YBMSM, irrespective of their house/family membership status.
Sexual health
Members of houses and families were no more or less likely than their non-member counterparts to be HIV positive, to engage in timely testing (if HIV negative), to have participated in an HIV prevention program, or to have received counseling from an HIV prevention counselor. However, house and family members were more likely to have heard of PrEP (OR=1.86; 95% CI: [1.18–2.92]) and to have a primary care doctor (OR=1.80; 95% CI: [1.13–2.86]). The later finding makes further sense when considered in light of what we know about health coverage among members.
Sex behaviors
The analysis revealed that house and family members were more likely to use sex drugs than non-members (OR=1.60; 95% CI: [1.01–2.52]). However, house and family members were no more or less likely to engage in condomless sex, group sex, or exchange sex.
Intravention behaviors
Although a majority of house and family members encourage their peers to use condoms and receive the same encouragement from their peers, results show that house and family members were no more likely to engage in these behaviors than non-members. The same can be said for the act of discouraging group sex. However, relative to non-members, members of houses or families were more likely to discourage their peers from using sex drugs (OR=1.58; 95% CI: [1.00–2.48]).
House and family differences
Additional analysis was performed to determine whether measures of association change when house and family memberships are disaggregated and examined separately. This enabled an examination of potential differences between these two communities with respect to their HIV prevention strengths and challenges that would otherwise go unnoticed in the primary analysis. With respect to health coverage, although both house and family members were less likely to be uninsured, only for family members was the relationship significant (OR=0.62; 95% CI: [0.38–0.98]). House members were more likely to be aware of PrEP than non-house members (OR=2.31; 95% CI: [1.24–4.32]), as were family members more likely than non-family members (OR=1.61; 95% CI: [1.01–2.55]). Further, family members only were more likely than their non-member counterparts to have a primary care doctor (OR=1.81; 95% CI: [1.13–2.91]) and more likely to use sex drugs (OR=1.59; 95% CI: [1.00–2.54]). And finally, of the intravention behaviors, house members only were more likely to discourage sex drug use (OR=2.23; 95% CI: [1.20–4.14]) relative to their non-member counterparts.
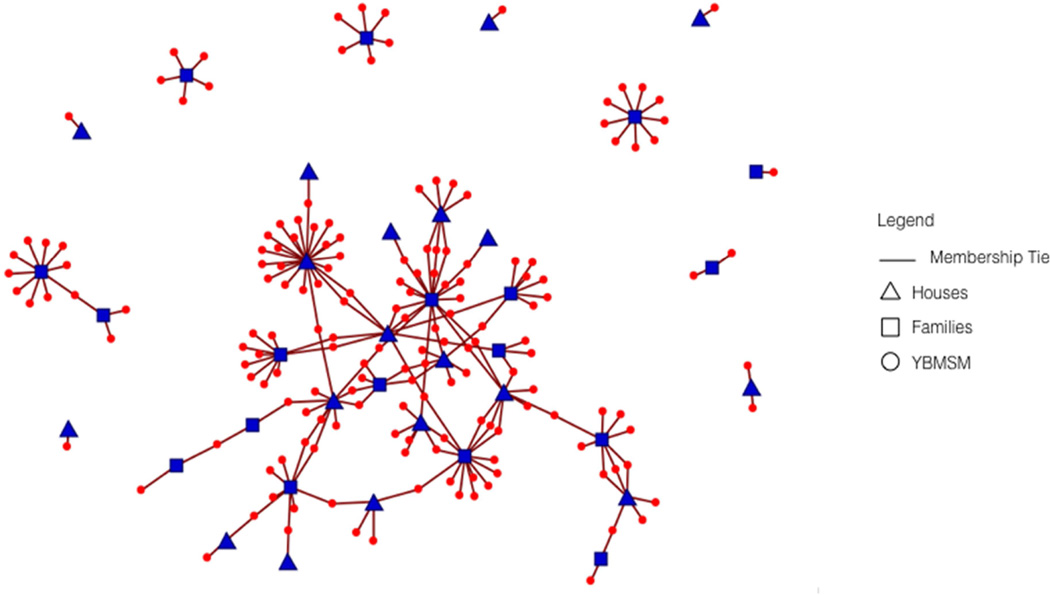
Homophily and heterophily in the house/family network
While the first portion of the analysis illuminates which types of people are more or less likely to belong to houses or families, the second portion of the analysis demonstrates whether individuals with traits related to HIV prevention cluster around the same houses or families. The network on which this analysis is based is shown in Figure 1. Of the 206 respondents who originally self-reported belonging to a ballroom house and/or a gay family, 168 provided the name of the houses or families to which they belonged, resulting in a total of 19 houses and 18 families. This yields a two-mode house/family membership network comprised of 168 YBMSM and 37 houses and families. In total, there are 214 house/family membership ties out of a possible 6216, resulting in a network density of 3.4%. Although we anticipated that affiliations with multiple houses and/or families would be infrequent, largely due to members’ loyalties to their adoptive kin groups, results show that some individuals do belong to more than one kin group. On average, YBMSM were members of 1.27 houses and/or families and 25 of the 37 kin groups shared between 1 and 3 members. Where multiple affiliations do occur they tend to be individuals with ties to two different independent families or ties with an independent family and a ballroom house. This reinforces what others have noted about the potential for intersection between houses and gay families in some regions (Horne et al., 2014).
Figure 1.
The network structure of house/family membership among 168 young Black men who have sex with men shown as a 2-mode house/family membership network: Chicago, IL; June 2013–July 2014.1
1 The two 2-mode house/family membership network is comprised of 168 young Black men who have sex with men and 37 houses and families. Among these nodes there are a total 214 house/family membership ties. YBMSM are shown as circles colored in red, houses are shown as triangles colored in blue, and families are shown as squares colored in blue.
Table 3 presents the results of the join-count analysis, which tells us whether certain traits cluster around the same houses or families. We discuss our join count findings in terms of the direction and statistical significance of the difference value for each combination. The difference is the observed tie count minus the expected tie count. A positive difference means that more co-membership ties characterized by the particular combination were observed than expected. Conversely, a negative difference means that more of a particular combination was expected than were actually observed in the graph. Differences are marked as significant if a difference that size or greater (in either direction) occurs in less than 5 percent (p<0.05), 1 percent (p<0.01), and .10 percent (p<0.001) of 40,000 random permutations of the network.
Table 3.
Homophilous and heterophilous mixing by risk and protective factors in the 1-mode YBMSM house/family affiliation network
| Variable | Expected | Observed | Difference |
|---|---|---|---|
| Sexual health traits | |||
| HIV seropositive | |||
| Homophily+ | 146.79 | 113.00 | −33.79* |
| Homophily- | 353.51 | 393.00 | 40.49 |
| Heterophily | 460.70 | 454.00 | −6.70 |
| Timely testing (if HIV-) | |||
| Homophily+ | 144.28 | 171.00 | 26.72* |
| Homophily- | 59.51 | 59.00 | −0.51 |
| Heterophily | 189.21 | 163.00 | −26.21* |
| PrEP Aware | |||
| Homophily+ | 207.91 | 266.00 | 58.10* |
| Homophily- | 246.64 | 208.00 | −38.64* |
| Heterophily | 458.46 | 439.00 | −19.46 |
| Primary Care Doctor | |||
| Homophily+ | 314.19 | 286.00 | −28.19 |
| Homophily- | 153.72 | 173.00 | 19.28 |
| Heterophily | 445.10 | 454.00 | 8.90 |
| Participation in an HIV prevention program | |||
| Homophily+ | 117.09 | 119.00 | 1.91 |
| Homophily- | 402.81 | 448.00 | 45.19 |
| Heterophily | 440.10 | 393.00 | −47.10* |
| Counseling Session with a prevention counselor | |||
| Homophily+ | 240.90 | 182.00 | −58.90** |
| Homophily- | 213.24 | 313.00 | 99.76*** |
| Heterophily | 458.86 | 418.00 | −40.86* |
| Sex behaviors | |||
| Condomless Sex | |||
| Homophily+ | 234.46 | 226.00 | −8.46 |
| Homophily- | 207.22 | 211.00 | 3.78 |
| Heterophily | 446.32 | 451.00 | 4.68 |
| Sex drug use | |||
| Homophily+ | 176.75 | 162.00 | −14.75 |
| Homophily- | 269.37 | 279.00 | 9.63 |
| Heterophily | 441.88 | 447.00 | 5.12 |
| Group sex | |||
| Homophily+ | 20.53 | 14.00 | −6.53 |
| Homophily- | 694.82 | 728.00 | 33.19 |
| Heterophily | 244.65 | 218.00 | −26.65 |
| Exchange sex | |||
| Homophily+ | 25.75 | 41.00 | 15.25* |
| Homophily- | 644.01 | 601.00 | −43.01 |
| Heterophily | 263.24 | 291.00 | 27.76 |
| Intravention behaviors | |||
| Encourages condoms | |||
| Homophily+ | 749.56 | 718.00 | −31.56 |
| Homophily- | 9.25 | 11.00 | 1.75 |
| Heterophily | 172.20 | 202.00 | 29.80 |
| Receives condom encouragement | |||
| Homophily+ | 570.02 | 555.00 | −15.02 |
| Homophily- | 42.83 | 43.00 | 0.17 |
| Heterophily | 318.15 | 333.00 | 14.85 |
| Discourages sex drug use | |||
| Homophily+ | 209.45 | 202.00 | −7.45 |
| Homophily- | 254.32 | 284.00 | 29.68 |
| Heterophily | 467.23 | 445.00 | −22.23 |
| Discourages group sex | |||
| Homophily+ | 132.77 | 109.00 | −23.77 |
| Homophily- | 357.10 | 384.00 | 26.90 |
| Heterophily | 441.13 | 438.00 | −3.13 |
p<05,
p<.01,
p<.001
Sexual health
The analysis of how sexual health traits organize within houses and families yields several noteworthy results. To begin, results show that HIV positive YBMSM are less likely than expected to belong to the same house/family (Homphily+, Diff = −33.79, p<.05), suggesting that HIV positive individuals are more distributed across houses and families than concentrated within them. Also noteworthy is that serostatus heterophily is not significant, which contradicts existing stereoptypes that serostatus-based disassortative sex is common within houses and families.
Clustering characterized by positive homophily was found for traits like timely HIV testing and PrEP awareness. With respect to timely HIV testing, results show that timely testers were more likely to belong to the same houses or families (Homophily+, Diff = 26.72, p<0.05). And, perhaps because house members are often presented with opportunities to test together at their own events, houses and families were actually less likely to foster co-membership ties between timely and delayed testers (Heterophily, Diff = −26.21, p<0.05). Similarly, individuals who had heard of PrEP had a greater tendency to cluster within the same houses and families (Homophily+, Diff = 58.10, p<0.05), while those who were unaware of PrEP were less likely to do so (Homophily-, Diff = −38.64, p<0.05). Results also provide evidence for clustering characterized by negative homophily. Individuals who had not received counseling from a prevention counselor were more likely to be members of the same house or family (Homophily-, Diff = 99.76, p<0.001), while those who had counseling were less likely to belong to the same house or family (Homophily+, Diff = −58.90, p<0.01).
Sex Behaviors
Three of the four sex behaviors showed no sign of organizing house/family-based social affiliations among YBMSM. Specifically, neither homophilous mixing nor heterophilous mixing related to condomless sex, sex drug use, or group sex were any more or less likely to occur. However, results do show that individuals who engaged in exchange sex as a means of income were more likely to be members of the same house or family (Homophily+, Diff = 15.25, p<0.05).
Intravention Behaviors
In our comparison of affiliated and non-affiliated YBMSM, it was shown that house and family members were more likely to engage in their own form of internal intervention (i.e., intraventions) than non-members. However, these intravention behaviors do not seem to structure patterns of house and family affiliations among members of this community. Specifically, results show for all four intravention behaviors, neither homophily nor heterophily were more likely to occur than expected by chance.
DISCUSSION
Our study advances understanding of the protective and risk potentials of ballroom houses and independent gay families in two important ways. First, to our knowledge, this analysis is the first to adopt a comparative approach to ascertaining the extent to which houses and families offer YBMSM added protection. While prior studies of the house and ballroom communities in cities like Chicago (Lemos et al., 2015), Los Angeles (Holloway, Schrager, Wong, Dunlap, & Kipke, 2014; Kubicek et al., 2013), New York (Murrill et al., 2008) and Philadelphia (Castillo et al., 2012) have identified and investigated practices and behaviors within these settings that span the protective-risk spectrum, little to no work has compared the prevalence of these traits to what exists in the non-affiliated YBMSM community. In taking this step, we develop a clearer picture of intra-population differences and the added value that houses and families introduce into the lives of its members.
Second, we adopt a network perspective that houses and families act as social foci (Feld, 1981) – i.e., social contexts that anchor joint activities and communicative interactions. From a public health standpoint, the interactions that derive from social foci like gay families are likely to perpetuate both protections and risks, depending on the mixing of traits among the individuals involved. With this in mind, we explored the degree to which trait similarities (homophily) and trait differences (heterophily) organized interactions within distinct houses or families. This investigation into the clustering of protective and risk traits in culturally specific social settings like houses and families contributes to an existing line of research that examines similar patterns in the social and sexual affiliations among MSM via the social venues they patronize (Frost, 2007; Fujimoto, Wang, Ross, & Williams, 2015; Fujimoto, Williams, & Ross, 2013).
The analyses suggest several main findings that have important implications for eliminating HIV within these communities. First, with respect to sexual health traits, YBMSM who are members of the house and gay family communities seem to have greater awareness of preventive methods like PrEP and greater connection to primary health care than their non-member counterparts. In analysis not featured here, we know that having a primary care doctor does increase the odds of having heard about PrEP, so it is quite possible that access to primary care serves as an important conduit through which information about PrEP is passed onto the individual. That said, we also intuit that testing events hosted at ballroom competitions enable members to engage with HIV prevention workers, during which they are likely to be introduced to PrEP for prevention as well. Also encouraging is that YBMSM who have heard about PrEP are more likely to be members of the same house or family, which may signal that the diffusion of information about PrEP is happening within these structures.
Conversely, we find that YBMSM who are HIV positive are less likely to be members of the same house or family. Empirically, this suggests that seropositive members of this community are more distributed across houses and families as opposed to clustered within them. However, in that houses and families create supportive environments for their members, they can be crucial for providing people living with HIV/AIDS (PLWHA) with opportunities to counsel one another as they cope with their status and their treatment (Bailey, 2009; Kalichman, Sikkema, & Somlai, 1996). Unfortunately, given our findings, seropositive house/family members in our sample may find locating and activating this form of support difficult. Thus, opportunities should be created to enable PLWHA members of the house and gay family communities to meet and support one another.
Internet platforms, particularly social networking sites like Facebook, are aptly set up to foster this type of support (Kalichman et al., 2003). Designed to bring together people with similar interests and/or experiences and create a safe space for expression, we argue that online groups have the potential to serve as a safe, protected space to bring together disconnected HIV positive members of the house and family communities. Further, our research has shown that the Ballroom and House communities already have a large group-based presence on social media. As such, the virtual setting should fit within an established repertoire of communication and social interaction.
Our findings around internally sustained intravention practices also provide insight into the protective potential of houses and families. As discussed at the outset of this paper, a contention held by house and family leaders is that interventions conducted by outsiders (e.g., community-based organizations, public health agencies) delegitimize the internal intervention work (i.e., intraventions) already performed by and for members of the community itself. Our univariate analysis reveals that intraventions regarding condom use and sex drug use are widely practiced by all YBMSM, including house and family members. However, the bivariate analysis shows that with respect to discouraging peers from using sex drugs, house and family members do so more than their non-member counterparts. Whether this kind of peer-to-peer prevention messaging developed organically within the house and family communities or was learned as part of programmatic outreach is difficult to discern. However, we argue, as others have previously, that any modality of prevention messaging that becomes internally sanctioned and sustained ought to be leveraged by public health officials to reinforce their outreach in the House and Family communities more broadly.
That said, results from the join count analysis suggest that these same internal prevention practices do not concentrate within individual houses and families, at least not among the house and family members included in our sample. Rather, the members in our sample who practice informal prevention messaging seem to be more distributed across different houses and families. A possible explanation for this can be found in the composition of respondents’ confidant networks. Data not featured in this study reveal that house and family members in our sample tended to name as confidants (i.e., the people with whom they discuss important matters) people from outside the house and family communities. It is plausible, then, that intravention communication like discouraging a peer from using sex drugs is not practiced with one’s house and family members because this kind of interpersonal encouragement is reserved for people with whom they consider their main sources of support.
In order for houses and families to take charge of their own internal prevention outreach, a “critical mass” (Markus, 1987; Oliver, Marwell, & Teixeira, 1985) of members in each house and family will need to engage in these prevention behaviors with their house and family peers such that others will reciprocate and a system of behavioral norms emerges that can sustain an ethos of prevention within the house and/or family setting. It has been posited that the diffusion of a new behavior like peer-to-peer prevention messaging will reach a self-generating and irreversible “tipping point” (Markus, 1987) when about 16% of the targeted population has adopted the behavior. A more complete survey of the member base of a house or family would be required to determine whether something like a “critical mass” actually exists in these settings or whether more work needs to be done internally to motivate members to practice these behaviors.
A third set of key findings pertain to sex behaviors. Results from the comparative analysis challenge assumptions that houses and families are particularly vulnerable to HIV due to the heightened prevalence of risky sex behaviors among their members. Although we do find evidence that house and family members do engage in forms of sexual risk, three of these behaviors -- condomless sex, group sex, and exchange sex – are no more or less prevalent among house/family members than they are among non-members. Nor are these three behaviors any more or less likely to be found within specific houses and families. Although the difference is not significant, these sex behaviors are actually observed less often in the house/family network than expected.
However, when we examine a sex behavior like sex drug use, we learn that house members in particular are more likely than non-members to have used alcohol or drugs to enhance the sexual experience or make it easier. At first glance, this seems out of place given what we already know about the tendency for house and family members to discourage their peers from engaging in this behavior. However, when we disaggregated house and family members we learned that the use of sex drugs was primarily a family phenomenon, whereas discouraging peers from using sex drugs was primarily a house phenomenon. This finding is suggestive of the need for more research to better understand the different vulnerabilities and assets that each community possesses.
This study has some limitations that should be considered understood when interpreting the results and that suggest future research directions. First, since these data are cross-sectional inferences about cause and effect cannot be made. Therefore, we are unable to determine whether the risk and protective traits associated with membership in the house and family communities are the adopted outcomes of membership or the antecedents. Second, with respect to our study samples, the houses and families included in the join count analysis only include those groups that were named by individuals in the sample. As such, there may be groups that we missed, particularly the less formal “constructed” families (Dickson-Gomez et al., 2014) that provide the same kind of support for individuals but that are lesser known. Further, we did not survey the full member base for each kin group named in the study. Rather, we only assessed house/family affiliations among the YBMSM in the initial population-based sample. In that no comprehensive or representative study of the Chicago house and family populations exists to our knowledge, however, it is difficult to determine how biased our sub-sample may be. And third, the join count technique featured in the second portion of the analysis only enables the examination of mixing patterns for one variable at a time, leaving unanswered how homophily or heterophily on different attributes interact as predictors of house/family co-membership. Further, join count analysis ignores the way in which networks self-organize through mechanisms like balance or centralization. In the future, bipartite (or two-mode) exponential random graph modeling (ERGM) could be used to enable testing, simultaneously, the effects of network structure and multiple actor attributes on membership tie formation.
In spite of these limitations, we believe that the analysis presented here provides researchers and practitioners with some important insights regarding the strengths and vulnerabilities of the house and independent gay family communities in Chicago. With this information, programs and interventions can be designed that build on existing human and social capital in this community in order to prevent the spread of HIV. As systems of social support and identity-affirmation, houses and families are considered sources of resilience that support and protect their members from the stresses that YBMSM often endure (Arnold, Sterrett-Hong, Jonas, & Pollack, 2016; Kubicek et al., 2013; Wong et al., 2014). For many, the stability a house or family provides cannot be overstated. As such, they have potential to be purveyors of HIV prevention messaging for their own members. And with rates of HIV still on the rise among YBMSM, the efficacy of standard modalities of HIV prevention that rely solely on the expertise of third party officials is subject to scrutiny. Adopting approaches that leverage the strengths of a targeted community and the patterns of affiliation that offer members emotional and physical protections may be an efficacious approach to HIV prevention.
Highlights.
Members were more likely to know about PrEP and have a primary care doctor.
Members were more likely to discourage peers from using sex drugs.
Members were more likely to use sex drugs.
Members who knew about PrEP clustered within the same houses or families.
Members who had exchange sex clustered within the same houses or families.
Acknowledgments
This work was supported in part by the NIH (R01DA033875, R01MH100021 and R01 DA039934). We would like to thank Ishida Robinson, Eve Zurawski, Billy Davis and Michelle Taylor for their invaluable support. We also thank study participants for contributing to the network cohort study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arnold E, Bailey MM. Constructing Home and Family: How the Ballroom Community Supports African American GLBTQ Youth in the Face of HIV/AIDS. J Gay Lesbian Soc Serv. 2009;21(2–3):171–188. doi: 10.1080/10538720902772006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold E, Sterrett-Hong E, Jonas A, Pollack LM. Social networks and social support among ball-attending African American men who have sex with men and transgender women are associated with HIV-related outcomes. Global public health. 2016:1–15. doi: 10.1080/17441692.2016.1180702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey MM. Performance as intravention: Ballroom culture and the politics of HIV/AIDS in Detroit. Souls. 2009;11(3):253–274. [Google Scholar]
- Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: Software for social network analysis. 2002 [Google Scholar]
- Bowleg L. When Black+ lesbian+ woman≠ Black lesbian woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles. 2008;59(5–6):312–325. [Google Scholar]
- Castillo M, Palmer BJ, Rudy BJ, Fernandez MI. Creating partnerships for HIV prevention among YMSM: the connect to protect project and House and Ball community in Philadelphia. Journal of prevention & intervention in the community. 2012;40(2):165–175. doi: 10.1080/10852352.2012.660126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. HIV Surveillance Report. 2014 Retrieved from http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf.
- CDC. Lifetime Risk of HIV Diagnosis in the United States [Press release] 2016 Retrieved from http://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html.
- Dickson-Gomez J, Owczarzak J, Lawrence JS, Sitzler C, Quinn K, Pearson B, Amirkhanian YA. Beyond the ball: implications for HIV risk and prevention among the constructed families of African American men who have sex with men. AIDS and Behavior. 2014;18(11):2156–2168. doi: 10.1007/s10461-014-0836-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feld SL. The focused organization of social ties. American Journal of Sociology. 1981:1015–1035. [Google Scholar]
- Friedman SR, Maslow C, Bolyard M, Sandoval M, Mateu-Gelabert P, Neaigus A. Urging others to be healthy:“Intravention” by injection drug users as a community prevention goal. AIDS Education and Prevention. 2004;16(3):250–263. doi: 10.1521/aeap.16.3.250.35439. [DOI] [PubMed] [Google Scholar]
- Frost SDW. Using sexual affiliation networks to describe the sexual structure of a population. Sexually transmitted infections. 2007;83(suppl 1) doi: 10.1136/sti.2006.023580. [DOI] [PubMed] [Google Scholar]
- Fujimoto K, Wang P, Ross MW, Williams ML. Venue-mediated weak ties in multiplex HIV transmission risk networks among drug-using male sex workers and associates. Journal Information. 2015;105(6) doi: 10.2105/AJPH.2014.302474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto K, Williams ML, Ross MW. Venue-based affiliation networks and HIV risk-taking behavior among male sex workers. Sexually transmitted diseases. 2013;40(6):453. doi: 10.1097/OLQ.0b013e31829186e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gile KJ, Handcock MS. Respondent-Driven Sampling: An Assessment of Current Methodology. Sociol Methodol. 2010;40(1):285–327. doi: 10.1111/j.1467-9531.2010.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel S, Salganik MJ. Assessing respondent-driven sampling. Proc Natl Acad Sci U S A. 2010;107(15):6743–6747. doi: 10.1073/pnas.1000261107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Social Problems. 1997;44(2):174. [Google Scholar]
- Holloway IW, Schrager SM, Wong CF, Dunlap SL, Kipke MD. Network correlates of sexual health advice seeking and substance use among members of the Los Angeles House and Ball communities. Health education research. 2014:cyt152. doi: 10.1093/her/cyt152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne SG, Levitt HM, Sweeney KK, Puckett JA, Hampton ML. African American Gay Family Networks: An Entry Point for HIV Prevention. The Journal of Sex Research. 2014;52(7):807–820. doi: 10.1080/00224499.2014.901285. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Benotsch EG, Weinhardt L, Austin J, Luke W, Cherry C. Health-related Internet use, coping, social support, and health indicators in people living with HIV/AIDS: Preliminary results from a community survey. Health Psychology. 2003;22(1):111. doi: 10.1037//0278-6133.22.1.111. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Sikkema KJ, Somlai A. People living with HIV infection who attend and do not attend support groups: A pilot study of needs, characteristics and experiences. AIDS care. 1996;8(5):589–600. doi: 10.1080/09540129650125542. [DOI] [PubMed] [Google Scholar]
- Khanna AS, Michaels S, Skaathun B, Morgan E, Green K, Young L, Schneider JA. Preexposure Prophylaxis Awareness and Use in a Population-Based Sample of Young Black Men Who Have Sex With Men. JAMA internal medicine. 2016;176(1):136–138. doi: 10.1001/jamainternmed.2015.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubicek K, McNeeley M, Holloway IW, Weiss G, Kipke MD. “It’s like our own little world”: resilience as a factor in participating in the ballroom community subculture. AIDS and Behavior. 2013;17(4):1524–1539. doi: 10.1007/s10461-012-0205-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemos D, Hosek SG, Bell M. Reconciling Reality With Fantasy: Exploration of the Sociocultural Factors Influencing HIV Transmission Among Black Young Men Who Have Sex With Men (BYMSM) Within the House Ball Community: A Chicago Study. Journal of gay & lesbian social services. 2015;27(1):64–85. doi: 10.1080/10538720.2015.988837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt HM, Horne SG, Puckett J, Sweeney KK, Hampton ML. Gay Families: Challenging Racial and Sexual/Gender Minority Stressors through Social Support. Journal of GLBT Family Studies. 2015;11(2):173–202. [Google Scholar]
- Markus ML. Toward a “critical mass” theory of interactive media universal access, interdependence and diffusion. Communication research. 1987;14(5):491–511. [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WLt, Wilson PA, Remis RS. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- Murrill CS, Liu K-l, Guilin V, Colón ER, Dean L, Buckley LA, Torian LV. HIV prevalence and associated risk behaviors in New York City's house ball community. American Journal of Public Health. 2008;98(6):1074–1080. doi: 10.2105/AJPH.2006.108936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver P, Marwell G, Teixeira R. A theory of the critical mass. I. Interdependence, group heterogeneity, and the production of collective action. American Journal of Sociology. 1985:522–556. [Google Scholar]
- Peek ME, Lopez FY, Williams HS, Xu LJ, McNulty MC, Acree ME, Schneider JA. Development of a Conceptual Framework for Understanding Shared Decision making Among African-American LGBT Patients and their Clinicians. Journal of general internal medicine. 2016;31(6):677–687. doi: 10.1007/s11606-016-3616-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purdie-Vaughns V, Eibach RP. Intersectional invisibility: The distinctive advantages and disadvantages of multiple subordinate-group identities. Sex Roles. 2008;59(5–6):377–391. [Google Scholar]
- Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, Friedman S. Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. American Journal of Public Health. 2013;103(1):e28–e36. doi: 10.2105/AJPH.2012.301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack CB, Burton LM. Kinscripts. Journal of Comparative Family Studies. 1993:157–170. [Google Scholar]
- Wong CF, Schrager SM, Holloway IW, Meyer IH, Kipke MD. Minority stress experiences and psychological well-being: The impact of support from and connection to social networks within the Los Angeles house and ball communities. Prevention Science. 2014;15(1):44–55. doi: 10.1007/s11121-012-0348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]