Abstract
Objective
Poor sleep quality has been linked to inflammatory processes and worse disease outcomes in the context of many chronic illnesses, but less is known in conditions such as chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). This study examines the relationships between sleep quality, pro-inflammatory cytokines, and CFS/ME symptoms.
Methods
Sixty women diagnosed with CFS/ME were assessed using the Pittsburgh Sleep Quality Index (PSQI), Fatigue Symptom Inventory (FSI) and Center for Disease Control and Prevention (CDC)-based CFS/ME symptom questionnaires. Circulating plasma pro-inflammatory cytokine levels were measured by ELISA. Multiple regression analyses examined associations between sleep, cytokines and symptoms, controlling for age, education, and body mass index.
Results
Poor sleep quality (PSQI global score) was associated with greater pro-inflammatory cytokine levels: interleukin-1β (IL-1β) (β=0.258, p=0.043), IL-6 (β=0.281, p=0.033), and tumor necrosis factor-alpha (TNF-α) (β=0.263, p=0.044). Worse sleep quality related to greater fatigue severity (β=0.395, p=0.003) and fatigue-related interference with daily activities (β=0.464, p<0.001), and more severe and frequent CDC-defined core CFS/ME symptoms (β=0.499, p<0.001, and β=0.556, p<0.001, respectively).
Conclusions
Results underscore the importance of managing sleep-related difficulties in this patient population. Further research is needed to identify the etiology of sleep disruptions in CFS/ME and mechanistic factors linking sleep quality to symptom severity and inflammatory processes.
Keywords: chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME), poor sleep quality, pro-inflammatory cytokines, inflammation, fatigue
Graphical Abstract
1. Introduction
Poor sleep quality has been implicated in worse health outcomes in various clinical populations and also contributes to diminished physical and psychological well-being in otherwise healthy individuals (Lorton et al., 2006, Okun et al., 2013). In a variety of clinical populations, disrupted sleep has been linked to greater fatigue and poorer health (Lorton, Lubahn, 2006). Poor sleep quality can be ascertained objectively by overnight polysomnography and subjectively by questionnaires such as the Pittsburgh Sleep Quality Index (PSQI), which measures sleep quality overall and many of its components (Buysse et al., 1989).
Sleep is commonly disrupted during the course of a chronic illnesses (Polo-Kantola et al., 2014) and can also be an important etiological, precipitating, or maintaining factor of disease (Lorton, Lubahn, 2006). Sleep deprivation and loss results in an activation of the immune system, which is evident on a cellular and genomic level (Irwin et al., 2006). In the context of inflammatory disorders such as ankylosing spondylitis, sleep quality overall and its composite parts (PSQI subscales) are positively correlated with symptom severity and with circulating C-Reactive Protein (CRP) levels (Aydin et al., 2015).
Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is a chronic unremitting condition with an estimated worldwide prevalence of 0.8–3.5% (Bhui et al., 2011), and is overrepresented among women (Klimas and Koneru, 2007). The disorder is a poorly misunderstood and debilitating inflammatory illness with no known etiology or cure. CFS/ME symptoms include post-exertional malaise, sore throat, and unrefreshing sleep, among other varied somatic symptoms. Research has revealed physiological manifestations of CFS/ME, such as dysregulated cortisol awakening response (CAR) and cytokine expression imbalance, which are associated with sleep disturbances in other contexts (Klimas and Koneru, 2007, Mariman et al., 2013, Wright et al., 2015). CFS/ME patients’ sleep is typically reported as unrefreshing and/or frequently disturbed (Mariman, Vogelaers, 2013). Recent research has identified subjective and objective accounts of poor sleep quality in CFS/ME—possibly identifying different sleep phenotypes (e.g. hypersomnia, insomnia-like phenotypes) (Gotts et al., 2013, Mariman, Vogelaers, 2013). Other studies found that CFS/ME patients report poor sleep, even while demonstrating otherwise normal sleep by polysomnography, as compared to healthy age-and gender-matched controls (Maes et al., 2012a, Neu et al., 2007).
In addition to experiencing somatic symptoms and poor sleep, CFS/ME patients reveal increased pro-inflammatory cytokine levels when compared to healthy controls (Fletcher et al., 2009, Klimas and Koneru, 2007, Maes, Twisk, 2012a, Maes et al., 2012b). Elevations in pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), and relatively lower levels of anti-inflammatory cytokines (including IL-13) were shown most consistently in CFS/ME patients vs. healthy controls (Fletcher, Zeng, 2009, Gupta et al., 1997, Moss et al., 1999). However, no individual cytokine, set of cytokine expression profiles, or biomarker has been consistently and conclusively found to be a diagnostic marker or known etiological factor in CFS/ME (Broderick et al., 2010). Discrepancies in the CFS/ME cytokine research may be due in part to cytokine measurement issues, including the use of different assays, which change in sensitivity and specificity over time due to methodological and laboratory advances, or the time of day when samples are collected (Fletcher, Zeng, 2009, Klimas et al., 2012, Nakamura et al., 2010, Pandi-Perumal et al., 2007). Inflammatory cytokine levels can also differ by gender, in part because of estrogen’s immunomodulatory effects, including in the context of CFS/ME (Klimas and Koneru, 2007, Smylie et al., 2013). The sleep and inflammation literature is not always stratified by gender, which may account for some inconsistencies in the literature.
Poor sleep quality has been shown to contribute to greater inflammation in healthy, and in acutely and chronically ill individuals, though there is evidence for a bi-directional relationship (Irwin, 2002, Irwin, Wang, 2006, Lorton, Lubahn, 2006). In general, pro-inflammatory cytokines promote sleep while anti-inflammatory cytokines prevent sleep (Krueger, 2008, Krueger et al., 2007). IL-1 and TNF-α are consistently found to be directly somnogenic when administered centrally or peripherally (Krueger and Majde, 2003). In rats, IL-6 modulates NREM sleep and is known to contribute to sleepiness, but does not meet full criteria for a sleep regulating substance (Hogan et al., 2003).
Inflammatory control can be disturbed in individuals who suffer from primary sleep disorders, such as insomnia (Vgontzas et al., 2002, Weil et al., 2009). Chronic insomnia can result in a shift and disruption in the circadian release of IL-6 and TNF-α (Vgontzas, Zoumakis, 2002). Inflammatory cytokines IL-6 and TNF-α are typically elevated in sleep disorders that result in excessive daytime sleepiness, such as sleep apnea and narcolepsy (Vgontzas et al., 1999, Vgontzas, Zoumakis, 2002). In healthy adults, these cytokines are usually elevated after sleep deprivation and may mediate sleep propensity and fatigue the next day (Vgontzas, Papanicolaou, 1999). It is reasonable that sleep disruptions in CFS/ME patients may therefore promote increased pro-inflammatory signaling and symptomology, yet little is known about the precise relationship between aspects of sleep disruption and specific inflammatory and symptomologic indicators in this population.
Present study
Given the association between sleep disruptions and illness severity and also with inflammation, we hypothesized that among women with CFS/ME poor sleep quality (higher PSQI global scores) would be associated with greater circulating pro-inflammatory cytokine levels, and more severe and frequent CFS/ME-related symptoms. Specifically, we hypothesized that poor sleep quality overall and certain subscales (i.e. sleep disturbances, sleep duration, and sleep latency) would predict (a) greater levels of circulating pro-inflammatory cytokines, including IL-1β, IL-6 and TNF-α, and (b) greater CFS/ME symptom burden including Centers for Disease Control and Prevention (CDC) core CFS/ME symptom severity and frequency, and greater fatigue severity and fatigue-related interference in daily life.
2. Methods
2.1. Participants and Procedures
Female participants in this study were recruited from a larger study of stress and coping processes in CFS/ME patients and study findings have been previously published (Hall et al., 2014, Lattie et al., 2012). This is the first report on sleep-related phenomena from this study. All participants received a physician-determined CFS/ME diagnosis, as defined by the CDC criteria (Fukuda et al., 1994). Recruitment methods included physician referral, support groups, CFS/ME conferences, and advertisements in CFS/ME-related websites. Participants were eligible if they were fluent in English, lived within the study area, and were between the ages of 21 and 75 years.
Potential participants were excluded from the study if they met criteria for schizophrenia, bipolar disorder, or substance abuse, or if they were actively suicidal, as assessed by a brief screening measure adapted from the Structured Clinical Interview for the DSM-IV (First et al., 1997). Participants were also excluded if they showed markedly diminished cognitive capabilities, as evidenced by making four or more errors on the Short Portable Mental Status Questionnaire (Pfeiffer, 1975). Presence of another condition (e.g. AIDS, lupus, rheumatoid arthritis) that might influence biological processes associated with CFS/ME symptomatology, or taking medications that would modulate immune or neuroendocrine functioning excluded participants from the study. Potential participants were also excluded from the study if they were suffering from untreated obstructive sleep apnea (OSA).
Participants who met criteria signed an informed consent form and scheduled a home visit between the hours of 11:00am and 3:00pm. During this visit, study personnel administered a battery of measures, and a certified phlebotomist drew a blood sample. After completing survey answers and providing blood samples, participants were compensated with $50.
2.2. Measures
2.2.1. Pittsburgh Sleep Quality Index (PSQI)
The 19-item PSQI (Buysse, Reynolds, 1989) was used to assess 7 components of sleep difficulties during the past 30 days, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. The seven component scores were rated from 0–3, with 0 signifying no difficulty and 3 indicating severe difficulty. The composite score added these seven subscale scores to provide a global score ranging from 0–21, where higher numbers indicated poorer sleep quality. The PSQI has been validated in many different populations (α=0.83 in healthy individuals), including CFS/ME patients (α=0.64) (Mariman et al., 2012b). The reliability coefficient for the PSQI in our sample was α=0.613 for CFS/ME women (α=0.709, if the “use of sleep medication” item was removed). This is a relatively low alpha, but is comparable to what was shown in the other sample of CFS/ME men and women, and might provide further support of the assertion that the global PSQI score is not as useful on its own for measuring subjective sleep quality in CFS/ME patients. This is the first time the PSQI has been validated in CFS/ME women only.
2.2.2. Fatigue Symptom Inventory (FSI)
The 14-item FSI assessed fatigue intensity using a 4-item subscale and fatigue interference using a 7-item subscale (Hann et al., 1998). Both subscales were scored on an 11-point scale, where 0 indicated feeling “not at all fatigued” and 10 indicated feeling “as fatigued as I could be” for the 4 fatigue intensity items. For the 7 fatigue interference items, 0 indicated “no interference” and 10 indicated “extreme interference.” The FSI has been validated for many populations, including women with and without cancer (α>0.90). In our sample, the FSI was valid α=0.869.
2.2.3. Center for Disease Control and Prevention (CDC) CFS Symptom Inventory
The 21-item CDC CFS Symptom Inventory was used to assess the frequency and severity of CFS/ME symptoms over the last 30 days (Wagner et al., 2005). Participants were asked yes or no questions about specific symptoms. If the symptom was present, the symptom was rated based on how often the symptom was present, with 1 indicating “a little of the time” and 5 indicating “all the time.” Then, the participants rated the severity of the symptom on a 5-point scale, with 1 indicating “very mild” and 5 indicating “very severe.” The CDC CFS Symptom Inventory has been validated previously (α=0.88) (Wagner, Nisenbaum, 2005). For all items, in our sample the scale was valid (α=0.85) and remained valid, even when the two sleep-related items were removed (α=0.84).
2.2.4. Circulating Pro-Inflammatory Cytokines
Blood was centrifuged and plasma stored at −80°C within 4 hours of collection until the samples were assayed in batches and in duplicate. Circulating pro-inflammatory cytokines IL-1β, IL-6 and TNF-α were measured from blood plasma as previously described (Fletcher, Zeng, 2009) using the an ELISA-based test (Q-Plex™ Human Cytokine –Screen, Quansys Biosciences Logan, Utah). Images were captured using Quansys Imager, driven by an 8.4 megapixel Canon 20D digital SLR camera, and analyzed using Quansys Software. In order to assure compatibility with measurements of cytokines in previously published studies in the field (Chiswick et al., 2012, Trune et al., 2011, Wong et al., 2008), the antigen standard concentrations used by Quansys (R&D) were referenced to “gold standard” for each cytokine represented on the multiplex plate as previously described (Lattie, Antoni, 2012).
2.3. Statistical Analyses
Statistical analyses were performed using SPSS version 22.0. Fatigue interference data were winsorized and cytokine data were log- transformed (i.e. ln (IL-6+1)) and then winsorized(Wilcox, 1993). The CDC CFS Symptom variables (severity and frequency) were calculated with the two items related to sleep quality removed. We used multiple regression to test our study hypotheses that higher global PSQI scores (indicating worse sleep quality) were associated with greater levels of circulating pro-inflammatory cytokines, more severe and frequent CFS/ symptoms, and more severe and interfering fatigue. As post-hoc analyses, we repeated the multiple regression analyses using PSQI subscales including: subjective sleep quality, sleep disturbances, sleep latency, and sleep duration. Participants’ age, educational level, and body mass index (BMI) were used as covariates, as sleep quality and inflammation are associated with those variables, differentially by gender (O'Connor et al., 2009, Vitiello et al., 2004).
3. Results
3.1 Sample Characteristics
As shown in Table 1, the mean age of the sample is 50.5 years, and 78.3% were non-Hispanic White. This was a highly educated sample, with 63% of the sample having attended at least some college, which is not atypical for this patient population (Jason et al., 2007, Servaes et al., 2001). Descriptive information on sleep quality, fatigue severity and interference, and CFS/ME symptom severity and frequency is provided in Table 1. Mean levels for cytokines were 31.91pg/mL, 8.79pg/mL, and 18.51pg/mL for IL-1β, IL-6, and TNF-α, respectfully, which were slightly higher than levels previously reported for CFS/ME cases (Fletcher, Zeng, 2009), as shown in Table 2. Fully 95% (57/60) of the sample had clinically-significant poor sleep quality as indicated by PSQI sleep quality scores > 5 (Buysse, Reynolds, 1989).
Table 1.
Demographic, Sleep-Related and Symptom-Related Characteristics of the Sample
| Participant Characteristics | |
|---|---|
| Age in years, M ± SD | 50.52 ± 10.88 |
| BMI (kg/in2), M ± SD | 26.66 ± 5.41 |
| Attended at least part of college, n (%) | 38 (63%) |
| White non-Hispanic, n (%) | 47 (78.3 %) |
| Married/Partnered, n (%) | 24 (40%) |
| Employed full-time, n (%) | 9 (15%) |
| PSQI Global Score, M ± SD | 12.18 ± 4.08 |
| Fatigue Severity, M ± SD | 6.94 ± 1.35 |
| Fatigue Interference, M ± SD | 6.98 ± 1.92 |
| CFS/ME Symptom Severity≠, M ± SD | 36.75 ± 14.67 |
| CFS/ME Symptom Frequency≠, M ± SD | 37.93 ± 15.53 |
CDC CFS Core Symptoms with sleep-related items removed
Table 2.
Descriptive Statistics of Cytokines
| (pg/mL) | Mean | SD | Range | Expected for CFS/ME Women* |
Expected for Female Controls* |
|---|---|---|---|---|---|
| IL-1β | 31.91 | 42.09 | 4.30–152.55 | 13.4 (4.5–38.3) | 6.2 (4.2–38.3) |
| IL-6 | 8.79 | 8.71 | 0.20–32.31 | 6.4 (3.8–14.4) | 3.2 (2.1–5.9) |
| TNF-α | 18.51 | 19.88 | 0.50–71.75 | 7.3 (3.4–22.6) | 6.4 (4.5–38.3) |
Expressed as 25th and 75th percentiles (Fletcher, Zeng, 2009)
3.2. Main Analyses
3.2.1. Sleep and symptoms
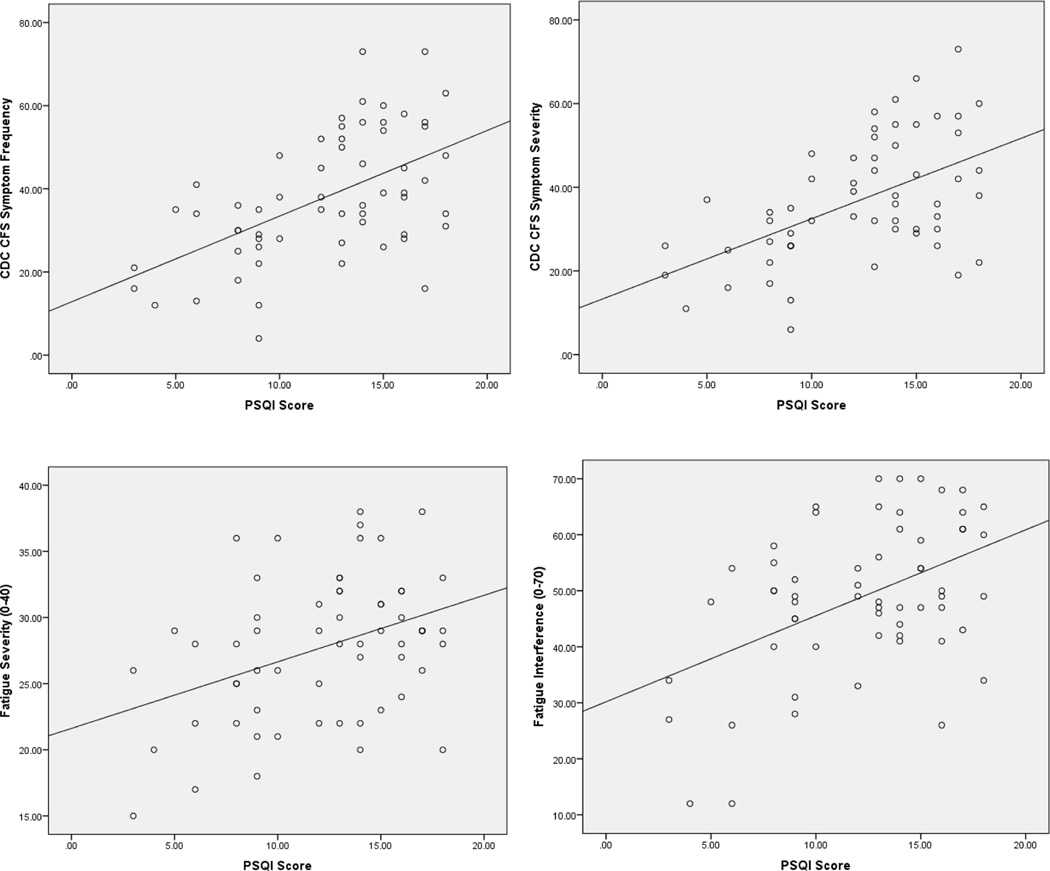
Multiple regression analyses showed that worse sleep quality predicted more severe and more frequent CFS/ME symptoms, and more fatigue severity and interference in daily life. Specifically, poorer sleep quality related to greater fatigue severity (β=0.395, p=0.003) and fatigue-related interference with daily activities (β=0.464, p<0.001), when controlling for age, educational level, and BMI (Table 3, Figure 1). Poorer sleep quality also predicted greater CDC core symptom severity (β=0.499, p<0.001) and frequency (β=0.556, p<0.001), when controlling for age, educational level, and BMI (Table 3, Figure 1).
Table 3.
Standardized Regression Coefficients of Fatigue and CDC Core Symptom Indices and PSQI Global and Subscale Score in Women with CFS/ME Controlling for Age, Education, and BMI
| Global | Sleep Quality | Sleep Latency | Sleep Duration | Sleep Disturbances | |
|---|---|---|---|---|---|
| Fatigue Severity |
.395** | .377** | .349** | .162 | .414** |
| Fatigue Interference |
.464** | 0.259* | .349** | .158 | .217 |
| CFS/ME Severitya |
.499** | .435** | .394** | .400** | .388** |
| CFS/ME Frequencya |
.556** | .432** | .340** | .434** | .508** |
CDC CFS Core Symptoms with sleep-related items removed
Significant at the p<0.05 level;
Significant at the p<0.01 level
Figure 1.
Relationships between CFS-Related Symptoms and Global PSQI Score
3.2.2. Sleep and cytokines
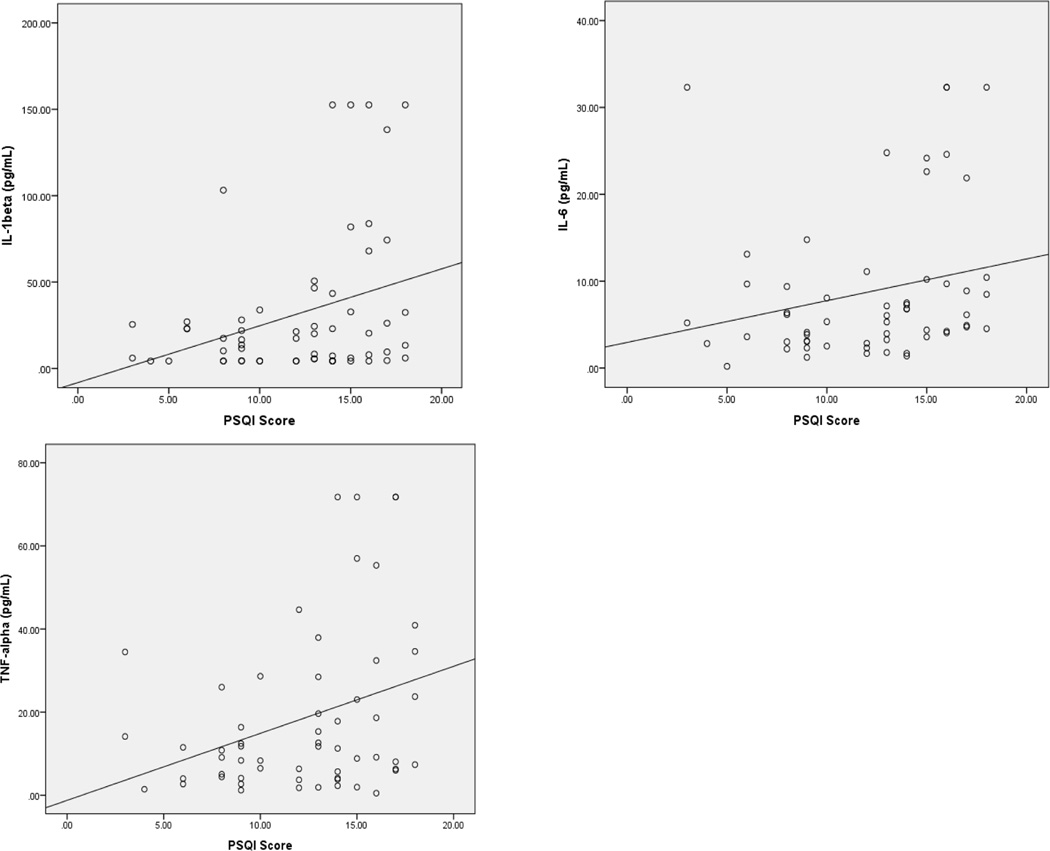
Poorer sleep quality was related to greater levels of pro-inflammatory cytokines, including IL-1β (β=0.258, p=0.043), IL-6 (β=0.281, p=0.033), and TNF-α (β=0.263, p=0.044), when controlling for age, educational level, and BMI (Table 4, Figure 2). Neither index of fatigue nor CDC-based symptomology was correlated with inflammatory cytokines (all p’s>0.050). At the subscale level, sleep latency, sleep duration and sleep disturbance subscales were related to greater cytokines levels, such that longer sleep latencies related to greater circulating IL-1β and IL-6, more frequent sleep disturbances were related to greater IL-6, and shorter sleep duration was associated with greater levels of all three cytokines (Table 4).
Table 4.
Standardized Regression Coefficients of Cytokines and PSQI Global and Subscale Scores in Women with CFS/ME Controlling for Age, Education, and BMI
| Global | Sleep Quality | Sleep Latency | Sleep Durationa | Sleep Disturbances | |
|---|---|---|---|---|---|
| IL-1β | .258* | .122 | .281* | .245* | .156 |
| IL-6 | .281* | .199 | .297* | .268* | .266* |
| TNF-α | .263* | .043 | .209 | .282* | .081 |
Significant at the p<0.05 level;
Significant at the p<0.01 level
Higher PSQI Sleep Duration Scores Indicate Shorter Sleep Duration
Figure 2.
Relationships between Circulating Serum Cytokine Levels and Global PSQI Score
4. Discussion
Here we report that poor sleep quality is independently associated with more severe and interfering fatigue, greater severity and frequency of CFS/ME symptoms, and greater inflammatory cytokine levels in women suffering from CFS/ME. Concordant with previous research, we found that perceived poor sleep quality is highly prevalent in women suffering from CFS/ME. In this sample, nearly all cases were clinically defined “poor sleepers,” as defined by global PSQI score > 5. Characterization of sleep difficulties in the context of CFS/ME is virtually as complex and idiosyncratic as the experience of the illness itself (Gotts, Deary, 2013). Previous research has demonstrated evidence of disrupted sleep by polysomnography and sleep questionnaires in CFS/ME, albeit not consistently (Aerenhouts et al., 2014, Ball et al., 2004, Fossey et al., 2004, Jackson and Bruck, 2012, Mariman et al., 2012a, Neu, Mairesse, 2007, Neu et al., 2014, Neu et al., 2015, Watson et al., 2004, Watson et al., 2003). This is the first study of CFS/ME to analyze subjective sleep quality components at the subscale level. We observed that increased sleep latency is highly prevalent in CFS/ME women with more than half the sample reporting difficulty falling asleep (sleep latency > 30 min.).
We also found that sleep parameters related to plasma inflammatory cytokine levels. The global subjective sleep quality score predicted significantly higher levels of all pro-inflammatory cytokines studied, as hypothesized. Multivariate subscale analysis showed that greater sleep latencies predicted higher circulating IL-1β and IL-6 levels, which is concordant with literature showing that insomniacs show increased inflammation; however, greater sleep latencies were not associated with TNF-α. This discrepancy could be explained by the somnogenic effects of TNF-α as a sleep regulatory substance (Krueger et al., 1998). Increased TNF-α levels in CFS/ME women might reflect an actively occurring homeostatic process, where chronic insufficient sleep leads to increased sleep propensity and therefore, shorter sleep latencies via increased, upregulated TNF-α. Possibly, the synergistic effects of other cytokines negate sleep initiation, which perpetuate longer sleep latencies and sleep disruption, further contributing to greater inflammation and symptom severity (Kapsimalis et al., 2008). Shorter sleep duration was associated with greater IL-1β, IL-6 and TNF-α levels, which may suggest that short, insufficient sleep covaries with more inflammation in this patient population. Finally, the sleep disturbance subscale was associated with greater IL-6 levels, possibly in accordance with the finding that IL-6 can disturb sleep in mammals, or that IL-6 expression is increased with disturbed, non-refreshing sleep (Clevenger et al., 2012).
As hypothesized, all subjective sleep parameters correlated positively with CFS/ME symptom measures, but with not all fatigue measures. Poorer global subjective sleep quality scores were associated with greater CFS/ME symptom expression (severity and frequency), fatigue severity, and fatigue-related interference in daily activities. Longer sleep latencies were associated with greater CFS/ME symptom severity and frequency, and fatigue severity and interference. Shorter sleep duration was also associated with greater CFS/ME symptom severity and frequency, but interestingly was not associated with either of the fatigue measures. These findings might shed light on precipitating and perpetuating factors of CFS/ME symptomology.
We were surprised that none of the CFS/ME symptom measures or fatigue measures were directly associated with pro-inflammatory cytokine levels. These results suggest that poor sleep may be linked with inflammation, independent of its relationship with CFS/ME symptomology, but do not rule out the plausibility of a neuroimmune mechanism underlying the relationship between sleep and these symptoms in the context of CFS/ME. Further research is needed to determine whether a third variable is mediating sleep’s influence on both inflammation and symptomology. One candidate may be altered HPA axis functioning, which has been associated with CFS/ME symptoms in recent work (Papadopoulos and Cleare, 2012). Dysregulated HPA axis functioning could link sleep to inflammation via alterations in immune cell sensitivity to glucocorticoid signaling (Hermann et al., 2006, Juster and McEwen, 2015), and at the same time link sleep to symptomology via alterations in di-urnal cortisol secretion patterns (Hermann, von Aulock, 2006, Marshall and Born, 2002, Nater et al., 2008, Powell et al., 2013, Rahman et al., 2011).
The present results underscore the importance of subjective poor sleep quality in the experience of CFS/ME on both a symptom and biomarker level. Overall, our results provide support for the hypothesis that poor sleep is linked with greater illness burden in a population of women with CFS/ME. Sleep is commonly disrupted during the course of many chronic medical conditions, and sleep dysregulation is a commonly reported complaint among women with chronic diseases (Polo-Kantola, Laine, 2014). Sleep disruption and/or dysregulation may be due to the symptoms of the illness and/or physiological dysfunction underlying the illness (Lorton, Lubahn, 2006). Disturbed sleep can also play an etiological, precipitating, or maintaining role in many medical conditions (Lorton, Lubahn, 2006) and it is plausible that it could cause or exacerbate some CFS/ME symptoms.
4.1. Strengths and Limitations
This study is the first of its kind to examine the overall and specific effects of poor sleep quality on multiple indices of CFS/ME symptomology and inflammation in a sample of women diagnosed with CFS/ME. The work provides many leads on the role of disturbed sleep in the maintenance of this poorly understood condition, which may pave the way for ameliorative interventions. However, any interpretations should be tempered by the limitations of our study.
Our study did not include a CFS/ME control group to determine if the effects of poor sleep in women with CFS/ME were significantly different from age- and gender matched poor sleepers who are otherwise healthy. The fact that these results were obtained in a relatively small cross-sectional study warrant caution in assigning temporal relations between the measured variables. Notably, the PQSI, which was administered at the time of the blood draw, asks participants to reflect back on their sleep for the past 30 days, therefore, we suggest that poor sleep may predict inflammatory cytokine levels and the magnitude of CFS/ME symptoms. Even so, longitudinal research is needed to follow-up on any of the associations reported herein.
The study is also limited by the lack of polysomnography and actigraphy data, which could have helped identify if there are objectively-defined sleep specific phenotypes in CFS/ME patients that map onto specific symptom patterns and inflammatory processes (Gotts, Deary, 2013, Mariman, Vogelaers, 2012a). These phenotypes may be reflected by or due, in part, to different cytokine expression profiles in CFS/ME patients, as different sleep-regulating cytokines (alone or in combination) may contribute to different sleep difficulty profiles (Lorton, Lubahn, 2006). Similar analyses conducted with cytokines measured directly before sleep, or throughout the night, might have revealed different patterns (Nakamura et al., 2013, Nakamura, Schwander, 2010).
While we excluded potential subjects with untreated obstructive sleep apnea (OSA), previous research has shown that primary sleep disorders are underdiagnosed in primary care settings (Fossey, Libman, 2004, Qanneta, 2014). In a recent study, primary sleep disorders, such as OSA, psychophysiologic insomnia or periodic limb movement disorder, were found in 49.8% of a sample of CFS/ME subjects (Mariman, Vogelaers, 2013). If there were a large percentage of women in our sample with undiagnosed OSA, our results may be biased, as OSA affects inflammatory cytokine levels, and subjective psychological, sleep and fatigue-related variables (Kapsimalis, Basta, 2008). Therefore, future research should substantiate our results with polysomnography or actigraphy data. Importantly, our subjects were recruited indiscriminate of fibromyalgia diagnosis, which may affect the generalizability of our results, as there are cytokine expression differences between CFS/ME patients with and without fibromyalgia under certain conditions (Nakamura, Schwander, 2013). Additionally, while the majority of our sample was middle-aged and presumed to be post-menopausal, we did not have information on menopausal status in this study. Hormonal fluctuations in women, especially during menopause, can disrupt sleep (Kravitz et al., 2008); therefore, future studies should control for this, as well as other hormonal indices such as point in menstrual cycle and contraceptive use. Finally, the future studies may investigate whether the present findings are moderated by psychological states (e.g., depression or distress) or traits (e.g., coping styles), as these variables have previously been related to many of the variables investigated here (Benhayon et al., 2013, Dantzer et al., 2008, Papadopoulos and Cleare, 2012).
5. Conclusion
Our preliminary findings of significant associations between self-reported sleep quality components and inflammatory indicators on the one hand and CFS/ME symptomology on the other justify further research in sleep medicine for CFS/ME patients, specifically addressing the mechanism behind these associations. The interpretations of our results are limited by a cross-sectional design; and the lack of a matched healthy control comparison group, nocturnal cytokine measurements, overnight polysomnography data, and important covariates (e.g., fibromyalgia, menopausal status). Using these results as a guide, it is important to conduct longitudinal research on this patient population in the future to identify mediating variables for these relationships using neuroendocrine and mood-related indicators. To realize the clinical implications of these associations, future work might identify and optimize interventions (e.g., Cognitive Behavior Therapy for Insomnia, CBT-I) (Wu et al., 2015) aimed at improving sleep latency, or other interventions known to improve overall sleep quality in other populations (e.g., Cognitive Behavioral Stress Management, CBSM) (Vargas et al., 2014) in order to modulate neuroimmune processes and CFS/ME-related symptoms.
Highlights.
Sleep quality, inflammation, and CFS/ME symptoms were analyzed.
Poor sleep quality predicted pro-inflammatory cytokines IL-1β, IL-6, and TNF-α.
Worse sleep quality related to greater fatigue severity and daily interference.
Worse sleep quality related to more severe and frequent CFS/ME symptoms.
Further research is needed to identify the etiology of sleep disruptions in CFS/ME.
Acknowledgments
Sources of Funding:
This research was supported by the National Institutes of Health [grant number 1R01 NS055672].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
The authors report no conflicts of interest.
REFERENCES
- Aerenhouts D, Ickmans K, Clarys P, Zinzen E, Meersdom G, Lambrecht L, et al. Sleep characteristics, exercise capacity and physical activity in patients with chronic fatigue syndrome. Disabil Rehabil. 2014:1–7. doi: 10.3109/09638288.2014.993093. [DOI] [PubMed] [Google Scholar]
- Aydin E, Bayraktar K, Turan Y, Omurlu I, Tastaban E, Sendur OF. Sleep quality in patients with ankylosing spondylitis. Revista Brasileira de Reumatologia (English Edition) 2015;55:340–345. doi: 10.1016/j.rbr.2014.12.007. [DOI] [PubMed] [Google Scholar]
- Ball N, Buchwald DS, Schmidt D, Goldberg J, Ashton S, Armitage R. Monozygotic twins discordant for chronic fatigue syndrome: objective measures of sleep. J Psychosom Res. 2004;56:207–212. doi: 10.1016/S0022-3999(03)00598-1. [DOI] [PubMed] [Google Scholar]
- Benhayon D, Youk A, McCarthy FN, Davis S, Keljo DJ, Bousvaros A, et al. Characterization of Relationships Between Sleep, Inflammation, and Psychiatric Dysfunction in Depressed Youth with Crohn’s Disease. J Pediatr Gastroenterol Nutr. 2013;57:335–342. doi: 10.1097/MPG.0b013e31829641df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhui KS, Dinos S, Ashby D, Nazroo J, Wessely S, White PD. Chronic fatigue syndrome in an ethnically diverse population: the influence of psychosocial adversity and physical inactivity. BMC Med. 2011;9:26. doi: 10.1186/1741-7015-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broderick G, Fuite J, Kreitz A, Vernon SD, Klimas N, Fletcher MA. A Formal Analysis of Cytokine Networks in Chronic Fatigue Syndrome. Brain Behav Immun. 2010;24:1209–1217. doi: 10.1016/j.bbi.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Chiswick EL, Duffy E, Japp B, Remick D. Detection and quantification of cytokines and other biomarkers. Methods Mol Biol. 2012;844:15–30. doi: 10.1007/978-1-61779-527-5_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clevenger L, Schrepf A, Christensen D, DeGeest K, Bender D, Ahmed A, et al. Sleep disturbance, cytokines, and fatigue in women with ovarian cancer. Brain Behav Immun. 2012;26:1037–1044. doi: 10.1016/j.bbi.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL. User's Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders: SCID-II: American Psychiatric Pub. 1997 [Google Scholar]
- Fletcher MA, Zeng XR, Barnes Z, Levis S, Klimas NG. Plasma cytokines in women with chronic fatigue syndrome. J Transl Med. 2009;7:96. doi: 10.1186/1479-5876-7-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossey M, Libman E, Bailes S, Baltzan M, Schondorf R, Amsel R, et al. Sleep quality and psychological adjustment in chronic fatigue syndrome. J Behav Med. 2004;27:581–605. doi: 10.1007/s10865-004-0004-y. [DOI] [PubMed] [Google Scholar]
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med. 1994;121:953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- Gotts ZM, Deary V, Newton J, Van der Dussen D, De Roy P, Ellis JG. Are there sleep-specific phenotypes in patients with chronic fatigue syndrome? A cross-sectional polysomnography analysis. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-002999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Aggarwal S, See D, Starr A. Cytokine production by adherent and non-adherent mononuclear cells in chronic fatigue syndrome. Journal of Psychiatric Research. 1997;31:149–156. doi: 10.1016/s0022-3956(96)00063-5. [DOI] [PubMed] [Google Scholar]
- Hall DL, Lattie EG, Antoni MH, Fletcher MA, Czaja S, Perdomo D, et al. Stress management skills, cortisol awakening response, and post-exertional malaise in Chronic Fatigue Syndrome. Psychoneuroendocrinology. 2014;49:26–31. doi: 10.1016/j.psyneuen.2014.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hann DM, Jacobsen PB, Azzarello LM, Martin SC, Curran SL, Fields KK, et al. Measurement of fatigue in cancer patients: development and validation of the Fatigue Symptom Inventory. Qual Life Res. 1998;7:301–310. doi: 10.1023/a:1024929829627. [DOI] [PubMed] [Google Scholar]
- Hermann C, von Aulock S, Dehus O, Keller M, Okigami H, Gantner F, et al. Endogenous cortisol determines the circadian rhythm of lipopolysaccharide-- but not lipoteichoic acid--inducible cytokine release. Eur J Immunol. 2006;36:371–379. doi: 10.1002/eji.200535470. [DOI] [PubMed] [Google Scholar]
- Hogan D, Morrow JD, Smith EM, Opp MR. Interleukin-6 alters sleep of rats. J Neuroimmunol. 2003;137:59–66. doi: 10.1016/s0165-5728(03)00038-9. [DOI] [PubMed] [Google Scholar]
- Irwin M. Effects of sleep and sleep loss on immunity and cytokines. Brain Behav Immun. 2002;16:503–512. doi: 10.1016/s0889-1591(02)00003-x. [DOI] [PubMed] [Google Scholar]
- Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med. 2006;166:1756–1762. doi: 10.1001/archinte.166.16.1756. [DOI] [PubMed] [Google Scholar]
- Jackson ML, Bruck D. Sleep Abnormalities in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: A Review. Journal of Clinical Sleep Medicine. 2012 doi: 10.5664/jcsm.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Torres-Harding S, Friedberg F, Corradi K, Njoku MG, Donalek J, et al. Non-pharmacologic interventions for CFS: a randomized trial. Journal of Clinical Psychology in Medical Settings. 2007;14:275–296. [Google Scholar]
- Juster RP, McEwen BS. Sleep and chronic stress: new directions for allostatic load research. Sleep Med. 2015;16:7–8. doi: 10.1016/j.sleep.2014.07.029. [DOI] [PubMed] [Google Scholar]
- Kapsimalis F, Basta M, Varouchakis G, Gourgoulianis K, Vgontzas A, Kryger M. Cytokines and pathological sleep. Sleep Medicine. 2008;9:603–614. doi: 10.1016/j.sleep.2007.08.019. [DOI] [PubMed] [Google Scholar]
- Klimas NG, Broderick G, Fletcher MA. Biomarkers for chronic fatigue. Brain Behav Immun. 2012;26:1202–1210. doi: 10.1016/j.bbi.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimas NG, Koneru AOB. Chronic fatigue syndrome: Inflammation, immune function, and neuroendocrine interactions. Curr Rheumatol Rep. 2007;9:482–487. doi: 10.1007/s11926-007-0078-y. [DOI] [PubMed] [Google Scholar]
- Kravitz HM, Zhao X, Bromberger JT, Gold EB, Hall MH, Matthews KA, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31:979–990. [PMC free article] [PubMed] [Google Scholar]
- Krueger JM. The Role of Cytokines in Sleep Regulation. Curr Pharm Des. 2008;14:3408–3416. doi: 10.2174/138161208786549281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger JM, Fang J, Taishi P, Chen Z, Kushikata T, Gardi J. Sleep: A Physiologic Role for IL-1β and TNF-αa. Annals of the New York Academy of Sciences. 1998;856:148–159. doi: 10.1111/j.1749-6632.1998.tb08323.x. [DOI] [PubMed] [Google Scholar]
- Krueger JM, Majde JA. Humoral Links between Sleep and the Immune System. Annals of the New York Academy of Sciences. 2003;992:9–20. doi: 10.1111/j.1749-6632.2003.tb03133.x. [DOI] [PubMed] [Google Scholar]
- Krueger JM, Rector DM, Churchill L. SLEEP AND CYTOKINES. Sleep Med Clin. 2007;2:161–169. doi: 10.1016/j.jsmc.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie EG, Antoni MH, Fletcher MA, Penedo F, Czaja S, Lopez C, et al. Stress management skills, neuroimmune processes and fatigue levels in persons with chronic fatigue syndrome. Brain Behav Immun. 2012;26:849–858. doi: 10.1016/j.bbi.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorton D, Lubahn CL, Estus C, Millar BA, Carter JL, Wood CA, et al. Bidirectional communication between the brain and the immune system: implications for physiological sleep and disorders with disrupted sleep. Neuroimmunomodulation. 2006;13:357–374. doi: 10.1159/000104864. [DOI] [PubMed] [Google Scholar]
- Maes M, Twisk FNM, Kubera M, Ringel K. Evidence for inflammation and activation of cell-mediated immunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopterin. Journal of Affective Disorders. 2012a;136:933–939. doi: 10.1016/j.jad.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Maes M, Twisk FNM, Ringel K. Inflammatory and Cell-Mediated Immune Biomarkers in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Depression: Inflammatory Markers Are Higher in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome than in Depression. Psychotherapy and Psychosomatics. 2012b;81:286–295. doi: 10.1159/000336803. [DOI] [PubMed] [Google Scholar]
- Mariman A, Vogelaers D, Hanoulle I, Delesie L, Pevernagie D. Subjective sleep quality and daytime sleepiness in a large sample of patients with chronic fatigue syndrome (CFS) Acta Clin Belg. 2012a;67:19–24. doi: 10.2143/ACB.67.1.2062621. [DOI] [PubMed] [Google Scholar]
- Mariman A, Vogelaers D, Hanoulle I, Delesie L, Tobback E, Pevernagie D. Validation of the three-factor model of the PSQI in a large sample of chronic fatigue syndrome (CFS) patients. J Psychosom Res. 2012b;72:111–113. doi: 10.1016/j.jpsychores.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Mariman AN, Vogelaers DP, Tobback E, Delesie LM, Hanoulle IP, Pevernagie DA. Sleep in the chronic fatigue syndrome. Sleep Med Rev. 2013;17:193–199. doi: 10.1016/j.smrv.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Marshall L, Born J. Brain-immune interactions in sleep. Int Rev Neurobiol. 2002;52:93–131. doi: 10.1016/s0074-7742(02)52007-9. [DOI] [PubMed] [Google Scholar]
- Moss RB, Mercandetti A, Vojdani A. TNF-alpha and chronic fatigue syndrome. J Clin Immunol. 1999;19:314–316. doi: 10.1023/a:1020595709352. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Schwander S, Donnelly R, Cook DB, Ortega F, Togo F, et al. Exercise and sleep deprivation do not change cytokine expression levels in patients with chronic fatigue syndrome. Clin Vaccine Immunol. 2013;20:1736–1742. doi: 10.1128/CVI.00527-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura T, Schwander SK, Donnelly R, Ortega F, Togo F, Broderick G, et al. Cytokines across the night in chronic fatigue syndrome with and without fibromyalgia. Clin Vaccine Immunol. 2010;17:582–587. doi: 10.1128/CVI.00379-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nater UM, Maloney E, Boneva RS, Gurbaxani BM, Lin JM, Jones JF, et al. Attenuated morning salivary cortisol concentrations in a population-based study of persons with chronic fatigue syndrome and well controls. J Clin Endocrinol Metab. 2008;93:703–709. doi: 10.1210/jc.2007-1747. [DOI] [PubMed] [Google Scholar]
- Neu D, Mairesse O, Hoffmann G, Dris A, Lambrecht LJ, Linkowski P, et al. Sleep quality perception in the chronic fatigue syndrome: correlations with sleep efficiency, affective symptoms and intensity of fatigue. Neuropsychobiology. 2007;56:40–46. doi: 10.1159/000110727. [DOI] [PubMed] [Google Scholar]
- Neu D, Mairesse O, Montana X, Gilson M, Corazza F, Lefevre N, et al. Dimensions of pure chronic fatigue: psychophysical, cognitive and biological correlates in the chronic fatigue syndrome. Eur J Appl Physiol. 2014;114:1841–1851. doi: 10.1007/s00421-014-2910-1. [DOI] [PubMed] [Google Scholar]
- Neu D, Mairesse O, Verbanck P, Le Bon O. Slow wave sleep in the chronically fatigued: Power spectra distribution patterns in chronic fatigue syndrome and primary insomnia. Clin Neurophysiol. 2015 doi: 10.1016/j.clinph.2014.12.016. [DOI] [PubMed] [Google Scholar]
- O'Connor M-F, Bower JE, Cho HJ, Creswell JD, Dimitrov S, Hamby ME, et al. To assess, to control, to exclude: effects of biobehavioral factors on circulating inflammatory markers. Brain Behav Immun. 2009;23:887–897. doi: 10.1016/j.bbi.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okun ML, Luther JF, Wisniewski SR, Wisner KL. Disturbed Sleep and Inflammatory Cytokines in Depressed and Nondepressed Pregnant Women: An Exploratory Analysis of Pregnancy Outcomes. Psychosom Med. 2013;75:670–681. doi: 10.1097/PSY.0b013e31829cc3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandi-Perumal SR, Cardinali DP, Chrousos GP. Neuroimmunology of sleep. Springer; 2007. [Google Scholar]
- Papadopoulos AS, Cleare AJ. Hypothalamic-pituitary-adrenal axis dysfunction in chronic fatigue syndrome. Nat Rev Endocrinol. 2012;8:22–32. doi: 10.1038/nrendo.2011.153. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Polo-Kantola P, Laine A, Aromaa M, Rautava P, Markkula J, Vahlberg T, et al. A population-based survey of sleep disturbances in middle-aged women--associations with health, health related quality of life and health behavior. Maturitas. 2014;77:255–262. doi: 10.1016/j.maturitas.2013.11.008. [DOI] [PubMed] [Google Scholar]
- Powell DJH, Liossi C, Moss-Morris R, Schlotz W. Unstimulated cortisol secretory activity in everyday life and its relationship with fatigue and chronic fatigue syndrome: a systematic review and subset meta-analysis. Psychoneuroendocrinology. 2013;38:2405–2422. doi: 10.1016/j.psyneuen.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Qanneta R. Obstructive sleep apnea syndrome manifested as a subset of chronic fatigue syndrome: a comorbidity or an exclusion criterion? Rheumatol Int. 2014;34:441–442. doi: 10.1007/s00296-013-2746-8. [DOI] [PubMed] [Google Scholar]
- Rahman K, Burton A, Galbraith S, Lloyd A, Vollmer-Conna U. Sleep-wake behavior in chronic fatigue syndrome. Sleep. 2011;34:671–678. doi: 10.1093/sleep/34.5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servaes P, van der Werf S, Prins J, Verhagen S, Bleijenberg G. Fatigue in disease-free cancer patients compared with fatigue in patients with chronic fatigue syndrome. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2001;9:11–17. doi: 10.1007/s005200000165. [DOI] [PubMed] [Google Scholar]
- Smylie AL, Broderick G, Fernandes H, Razdan S, Barnes Z, Collado F, et al. A comparison of sex-specific immune signatures in Gulf War illness and chronic fatigue syndrome. BMC Immunol. 2013;14:29. doi: 10.1186/1471-2172-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trune DR, Larrain BE, Hausman FA, Kempton JB, MacArthur CJ. Simultaneous measurement of multiple ear proteins with multiplex ELISA assays. Hear Res. 2011;275:1–7. doi: 10.1016/j.heares.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas S, Antoni MH, Carver CS, Lechner SC, Wohlgemuth W, Llabre M, et al. Sleep quality and fatigue after a stress management intervention for women with early-stage breast cancer in southern Florida. International journal of behavioral medicine. 2014;21:971–981. doi: 10.1007/s12529-013-9374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vgontzas AN, Papanicolaou DA, Bixler EO, Lotsikas A, Zachman K, Kales A, et al. Circadian interleukin-6 secretion and quantity and depth of sleep. J Clin Endocrinol Metab. 1999;84:2603–2607. doi: 10.1210/jcem.84.8.5894. [DOI] [PubMed] [Google Scholar]
- Vgontzas AN, Zoumakis M, Papanicolaou DA, Bixler EO, Prolo P, Lin HM, et al. Chronic insomnia is associated with a shift of interleukin-6 and tumor necrosis factor secretion from nighttime to daytime. Metab Clin Exp. 2002;51:887–892. doi: 10.1053/meta.2002.33357. [DOI] [PubMed] [Google Scholar]
- Vitiello MV, Larsen LH, Moe KE. Age-related sleep change: Gender and estrogen effects on the subjective–objective sleep quality relationships of healthy, noncomplaining older men and women. J Psychosom Res. 2004;56:503–510. doi: 10.1016/S0022-3999(04)00023-6. [DOI] [PubMed] [Google Scholar]
- Wagner D, Nisenbaum R, Heim C, Jones JF, Unger ER, Reeves WC. Psychometric properties of the CDC Symptom Inventory for assessment of chronic fatigue syndrome. Popul Health Metr. 2005;3:8. doi: 10.1186/1478-7954-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson NF, Jacobsen C, Goldberg J, Kapur V, Buchwald D. Subjective and objective sleepiness in monozygotic twins discordant for chronic fatigue syndrome. Sleep. 2004;27:973–977. doi: 10.1093/sleep/27.5.973. [DOI] [PubMed] [Google Scholar]
- Watson NF, Kapur V, Arguelles LM, Goldberg J, Schmidt DF, Armitage R, et al. Comparison of subjective and objective measures of insomnia in monozygotic twins discordant for chronic fatigue syndrome. Sleep. 2003;26:324–328. doi: 10.1093/sleep/26.3.324. [DOI] [PubMed] [Google Scholar]
- Weil ZM, Norman GJ, Karelina K, Morris JS, Barker JM, Su AJ, et al. Sleep deprivation attenuates inflammatory responses and ischemic cell death. Exp Neurol. 2009;218:129–136. doi: 10.1016/j.expneurol.2009.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox RR. Some results on a Winsorized correlation coefficient. British Journal of Mathematical and Statistical Psychology. 1993;46:339–349. [Google Scholar]
- Wong H-L, Pfeiffer RM, Fears TR, Vermeulen R, Ji S, Rabkin CS. Reproducibility and correlations of multiplex cytokine levels in asymptomatic persons. Cancer Epidemiol Biomarkers Prev. 2008;17:3450–3456. doi: 10.1158/1055-9965.EPI-08-0311. [DOI] [PubMed] [Google Scholar]
- Wright KP, Drake AL, Frey DJ, Fleshner M, Desouza CA, Gronfier C, et al. Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain Behav Immun. 2015 doi: 10.1016/j.bbi.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive Behavioral Therapy for Insomnia Comorbid With Psychiatric and Medical Conditions: A Meta-analysis. JAMA Intern Med. 2015 doi: 10.1001/jamainternmed.2015.3006. [DOI] [PubMed] [Google Scholar]