To the Editor
Patients 65 years old and older undergo over 30% of surgical procedures in the United States and undergo operations at a rate twice that of the general population.1 Postoperative delirium is an increasingly recognized postoperative occurrence in these patients, resulting in prolonged length of stay (LOS), functional decline, and increased mortality.2 Given that delirium may be preventable in over one-third of cases with proper intervention, increased attention has been focused on identification of at-risk, or frail, patients prior to surgery.3 Functional status can be used as a surrogate for frailty,4 though comprehensive geriatric assessment has not yet become part of standard preoperative protocols. Trunk muscle size, as defined by total psoas area (TPA) on CT scan, represents a novel, objective marker of surgical frailty5 and has previously been shown to correspond with functional status.6 The objective of this study was to examine the relationship between TPA and postoperative delirium in older patients planning to undergo elective general surgical procedures, controlling for other delirium risk factors identifiable by comprehensive geriatric assessment.
We conducted an observational cohort study on a subsample of patients included in the larger Vulnerable Elders Surgical Pathways and outcomes Assessment (VESPA) study at the University of Michigan from 2007–2011.6 Inclusion criteria were patient age >70 years, preoperative CT scan within 90 days prior to elective surgery, and LOS > 1 day (n=142 cases). TPA was calculated at the L4 vertebral level using validated analytic morphomic methods.5 In this study, TPA was defined as the sum of normal density muscle (31-100 Hounsfield Units (HU)) and low-density muscle (0-30 HU). A low TPA was defined as individuals falling within the lowest tertile of the gender-standardized study population. We used retrospective medical record review to assess for the incidence of delirium or acute confusional state in the postoperative period modified from the methodology described by Inouye et al.7 We used multivariate logistic regression to estimate the association between TPA and development of any signs or symptoms of post-operative delirium, controlling for extensiveness of surgery and known delirium risk factors. We adjusted for age (per 5 year increase), surgical complexity determined by Work Relative Value Units (WRVU), comorbidity using Charlson comorbidity index,8 degree of pre-operative functional impairment (having difficulty in 0-5 activities of daily living (bathing, walking, shopping, light housework, managing finances) modified from Saliba et al9) and cognitive impairment (documented dementia, cognitive impairment, or positive pre-operative Mini-Cog test10). A significance level of α=0.05 was used. As a sensitivity analysis, we identified influential observations using Pregibon influence statistics. All statistical analysis was performed using STATA version 13 (StataCorp LP, College Station, TX).
Among the 142 patients within the analytic sample, 22 (15.5%) developed documented signs or symptoms of post-operative delirium during their hospitalization. The delirious patients had a median length of stay of 12.2 days (versus 8 days for non-delirious patients, p=0.001) and were more likely to be discharged to destinations other than home (45.5% vs. 21.6%) (p=0.018).
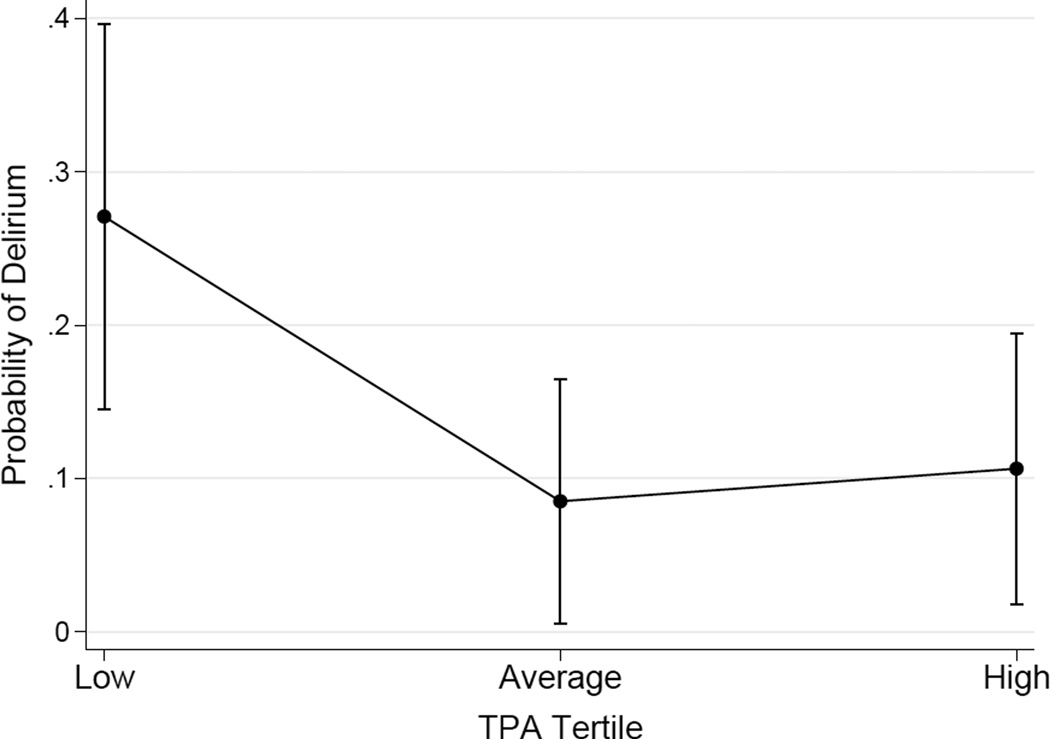
Post-operative signs and symptoms of delirium were associated with low TPA (versus normal or high TPA, OR 3.51 CI 1.37-8.95) and advanced age (OR 1.12, CI 1.02-1.21 per year increase). In the multivariate model controlling for age, co-morbidity, surgical complexity, cognitive impairment, and pre-operative functional status, the effect of low TPA remained substantial, however, confidence intervals included 1 (OR 2.63, CI 0.94-7.39, p=0.067), a loss of statistical significance that was sensitive to a single highly influential and outlying case (dbeta = 2.35) who had a middle-tertile TPA but high functional impairment. After removal of this patient, low psoas muscle area [OR 3.12, CI 1.02-9.56, p=0.046] was substantively and statistically independent of age and the other risk factors, with an area under the Receiver Operative Curve of 0.8077. Patients with TPA within the lowest tertile of the study population had a 27% risk of delirium during their during hospitalization, compared to a 10% risk for patients with the highest TPA (highest tertile) (Figure).
Figure 1.
Probability of Delirium by Tertile of Total Psoas Area (TPA). Predicted risk of developing delirium based on TPA after controlling for other risk factors. Patients with the lowest TPA (lowest tertile) had 2.7 times the risk of delirium as patients with the highest TPA (highest tertile of study population) (27% vs. 10%).
In this study, the addition of trunk muscle size to existing risk factors results in more robust prediction of patients at risk for delirium. We believe that trunk muscle size represents an innovative, objective metric that can potentially be used both to identify vulnerable patients and to subsequently guide anti-deliriogenic interventions, both behavioral and pharmacologic, following hospital admission. With a larger sample and further developments to increase availability of automated morphometric measures preoperatively (e.g. within the electronic medical record), this research indicates that psoas muscle size may represent a new tool to identify at-risk patients and prevent the development of postoperative delirium.
Acknowledgments
Financial disclosure: Supported by the Claude D. Pepper Older Americans Independence Center (NIA AG024824 (Yung)) (Min, Diehl), John A Hartford Foundation (Min), Medical Student Training in Aging Research (MSTAR) (Miller).
Appendix
Table.
| Elements of Financial/ Personal Conflicts |
Miller, A |
Englesbe, M |
Diehl, K |
Chan, C |
Cron, D |
Derstine, B |
Palazzolo, W |
Hall, K | Wang, S | Min, L | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Y | N | Y | N | Y | N | Y | N | Y | N | Y | N | Y | N | Y | N | Y | N | Y | N | |
| Employment or Affiliation |
X | X | X | X | X | X | X | X | X | X | ||||||||||
| Grants/Funds | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Honoraria | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Speaker Forum | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Consultant | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Stocks | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Royalties | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Expert Testimony |
X | X | X | X | X | X | X | X | X | X | ||||||||||
| Board Member | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Patents | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Personal Relationship |
X | X | X | X | X | X | X | X | X | X | ||||||||||
Footnotes
Conflict of Interest: The authors disclose the following; S.C.W. has one patent pertaining to technology described in this article (Wang SC, Holcombe SA, Huhdunpaa H, Sullivan JE, Kohoyda - Inglis C., inventors. The Regents of the University of Michigan, assignee. Analytic Morphomics: High Speed Medical Image Automated Analysis Method. United States PCT/US2013/057501. 2012 August 30). The remaining listed authors have no conflicts of interest to declare.
Author Contributions:
Study concept/design: Miller, Englesbe, Diehl, Hall, Wang, Min
Acquisition of data: Miller, Chan, Cron, Derstine, Palazzolo, Min
Analysis/interpretation of data: Miller, Englesbe, Chan, Cron, Derstine, Wang, Min
Drafting of manuscript: Miller, Englesbe, Cron, Min
Critical revision: All listed authors
Approval of paper for publication: All listed authors
Sponsor’s Role: The sponsor had no role in the study concept / design, methods, subject recruitment, data collection, analysis or preparation of this paper.
References
- 1.Weiss AJ, Elixhauser A, Andrews RM. Statistical Briefs. Rockville (MD): 2006. Characteristics of Operating Room Procedures in U.S. Hospitals, 2011: Statistical Brief #170. Healthcare Cost and Utilization Project (HCUP) [PubMed] [Google Scholar]
- 2.Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. 2009;249(1):173–178. doi: 10.1097/SLA.0b013e31818e4776. [DOI] [PubMed] [Google Scholar]
- 3.The American Geriatrics Society Expert Panel on Postoperative Delirium in Older A. American Geriatrics Society Abstracted Clinical Practice Guideline for Postoperative Delirium in Older Adults. J Am Geriatr Soc. 2015;63(1):142–150. doi: 10.1111/jgs.13281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malani PN. Functional status assessment in the preoperative evaluation of older adults. JAMA. 2009;302(14):1582–1583. doi: 10.1001/jama.2009.1453. [DOI] [PubMed] [Google Scholar]
- 5.Englesbe MJ, Lee JS, He K, et al. Analytic morphomics, core muscle size, and surgical outcomes. Ann Surg. 2012;256(2):255–261. doi: 10.1097/SLA.0b013e31826028b1. [DOI] [PubMed] [Google Scholar]
- 6.Miller AL, Min LC, Diehl KM, et al. Analytic morphomics corresponds to functional status in older patients. J Surg Res. 2014;192(1):19–26. doi: 10.1016/j.jss.2014.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST, Leslie DL, Agostini JV. A Chart-Based Method for Identification of Delirium: Validation Compared with Interviewer Ratings Using the Confusion Assessment Method. J Am Geriatr Soc. 2005;53(2):312–318. doi: 10.1111/j.1532-5415.2005.53120.x. [DOI] [PubMed] [Google Scholar]
- 8.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 9.Saliba D, Orlando M, Wenger NS, Hays RD, Rubenstein LZ. Identifying a short functional disability screen for older persons. J Gerontol A Biol Sci Med Sci. 2000;55(12):M750–M756. doi: 10.1093/gerona/55.12.m750. [DOI] [PubMed] [Google Scholar]
- 10.Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive 'vital signs' measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15(11):1021–1027. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]