Abstract
OBJECTIVES
To evaluate how the associations of adverse childhood events (ACEs) with smoking, overweight, obesity and binge drinking differ by race/ethnicity among women, including a large, understudied cohort of Asians and Native Hawaiians/Pacific Islanders (NHOPIs).
METHODS
The number and type (household dysfunction, and physical, verbal and sexual abuse) of ACEs were examined in relation to adulthood smoking, overweight, obesity and binge drinking among 3,354 women in Hawaii using the 2010 Behavioral Risk Factor Surveillance System data using Poisson regression. We additionally investigated for interaction by race/ethnicity. Covariates included age, race/ethnicity, education, emotional support, healthcare coverage, and the other health outcomes.
RESULTS
Overall, 54.9% reported at least 1 ACE. The prevalence of smoking (Prevalence Ratio [PR]=1.40 [1 ACE] to PR=2.55 [5+ ACEs]), overweight (PR=1.22 [1 ACE] to PR=1.31 [5+ ACEs]) and obesity (PR=1.00 [1 ACE] to PR=1.85 [5+ ACEs]) increased with increasing ACE count. Smoking was associated with household dysfunction (PR=1.67, CI=1.26–2.22), and physical (PR=2.04, CI=1.50–2.78) and verbal (PR=1.62, CI=1.25–2.10) abuse. Obesity was also significantly related to household dysfunction (PR=1.22, CI=1.01–1.48), and physical (PR=1.36, CI=1.10–1.70), verbal (PR=1.35, CI=1.11–1.64) and sexual (PR=1.53, CI=1.25–1.88) abuse. Among Asians, sexual abuse was associated with a lower prevalence of binge drinking (PR=0.26, CI=0.07, 0.93), which was significantly different from the null association among Whites (interaction p=0.02).
CONCLUSION
Preventing/addressing ACEs may help optimize childhood health, and reduce the likelihood of smoking/obesity among women including Asians/NHOPIs. Further studies are warranted to evaluate the sexual abuse-binge drinking association among Asians, which may support the need for culturally-tailored programs to address ACEs.
Keywords: Adverse Childhood Events, Women’s Health, Smoking, Obesity, Binge Drinking, Asians, Native Hawaiians and Pacific Islanders
INTRODUCTION
In the US, adverse childhood events (ACEs) have been linked to poor health factors including smoking, obesity and alcohol use [1–9]; however, little information exists on how this relationship may differ by race/ethnicity, particularly including understudied populations such as Asians and Native Hawaiians/Pacific Islanders (NHOPIs), or how it affects women, which is particularly important as it impacts preconception health, birth outcomes, and chronic diseases.
In a study by the Kauai Committee on the Status of Women, which captured a large sample of Asian and NHOPI women, Native Hawaiians accounted for 6% more domestic violence (i.e. 21% versus, 15%) compared to Caucasians, while Asians such as Filipino and Japanese fell below that of Caucasians (i.e. 11% and 5%, respectively) [10]. Rates as high as 56% for verbal abuse and 32% for physical abuse have been reported for Asians and NHOPIs, however [11]. Evidence from studies targeting Asian populations suggests that underreporting possibly due to conflict avoidance, acceptance of male domination, an aversion to seek help, prioritization of community over individual welfare, and less acculturation to Western norms among this population may explain the low rates [12–17].
The NHOPI population generally has the worst health-related outcomes in Hawaii. For example, in 2011, 11.8% of public high school students in Hawaii were current smokers, with higher estimates among Native Hawaiian (17.5%) and other Pacific Islander (19.5%) students [18]. Unique to Hawaii’s population, Native Hawaiians are the only ethnic group in the US in which women are more likely than men to smoke (23% vs. 20%) [19]. Although the prevalence of obesity in Hawaii overall is lower than that of the US (22.7%) [20], adult obesity among NHOPI (34.7%), is greater than the national average (27.9%) [21]. Further, the prevalence of ‘heavy drinking’ (2+ drinks for men and 1+ for women per day) in Hawaii is about 30% higher than that for the general US population [22]. The presence of ACEs may help explain, in part, the prevalence of adverse health factors in these populations.
The primary objective of this study was to investigate whether the relationship between ACEs and common health factors (i.e. smoking, overweight, obesity and binge drinking) among adult women in Hawaii might differ by race/ethnicity.
METHODS
Study Population
This study utilized data from the 2010 Hawaii BRFSS survey, coordinated and partially funded by the Centers for Disease Control and Prevention. This survey used a multistage probability sample method of non-institutionalized and non-hospitalized US adult population 18 years and older residing in households with a landline telephone. The Council of American Survey Research Organizations response rate, which reflects both telephone sampling efficiency and the degree of participation among eligible respondents contacted [23], was 49.1%, which was similar to other states where the BRFSS ACE module was employed [24]. Detailed information on the sampling methodology, weighting procedures, quality assurance, and other aspects of this survey is available online at http://www.cdc.gov/brfss/index.htm. The BRFSS survey is in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Participants gave informed consent prior to survey inclusion. This study consists of secondary analyses on publically available, de-identified data determined to be IRB exempt.
Adverse Childhood Events (ACEs)
Eleven questions/items were used to define ACEs (before age 18 years), adapted from validated survey instruments [1]. In the current study, an ordinal variable was developed based on the number of ACEs reported, which ranged from 0 to 8, with the classification of ‘substance abuse’ having 2 items and ‘sexual abuse’ having 3. The upper end of the distribution was combined to maintain adequate group size and, thus, ACE count was grouped as 0, 1, 2, 3, 4 and 5+. The 11 items were also grouped into 4 standard categories as in a previous study: household dysfunction, physical abuse, verbal abuse, and sexual abuse [1, 24]. A list of specific questions/items corresponding to these categories, which will be referred to as ACE types, is provided in Table 1 with corresponding response choices. The response for each category of household dysfunction, with the exception of the item, ‘Witness domestic violence’, was ‘Yes’ or ‘No’. For the household item, ‘Witness domestic violence’, and the categories of physical, verbal and sexual abuse, responses included ‘Once’, ‘More than once’ or ‘Never’. With the exception of verbal abuse, a response of at least ‘Once’ defined the presence of the corresponding ACE. For verbal abuse, a response of ‘More than once’ was necessary for verbal abuse to be considered present in the study [24]. For ACE categories with multiple items (i.e. household dysfunction, sexual abuse), adverse events were considered present if an affirmative answer was given to any of the items.
TABLE 1.
Adverse childhood event (ACE) question items and corresponding responses (BRFSS, 2010, Hawaii)
| ACE Type | Items: “Now, looking back before you were 18 years of age…” | Response Categoriesa |
|---|---|---|
| Household Dysfunction | ||
| • Mental illness in household member | • Did you live with anyone who was depressed, mentally ill, or suicidal? | Yes, No |
| • Substance abuse in household member | • Did you live with anyone who was a problem drinker or alcoholic? | Yes, No |
| • Did you live with anyone who used illegal street drugs or who abused prescription medications? | Yes, No | |
| • Incarceration of household member | • Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility? | Yes, No |
| • Divorce | • Were your parents separated or divorced? | Yes, No |
| • Witnessed abuse | • How often did your parents or adults in your home ever slap, hit, kick, punch or beat each other up? | Never, Once, More than Once |
| Physical Abuse | • Before age 18, how often did a parent or adult in your home ever hit, beat, kick, or physically hurt you in any way? Do not include spanking. Would you say… | Never, Once, More than Once |
| Verbal Abuseb | • How often did a parent or adult in your home ever swear at you, insult you, or put you down? | Never, Once, More than Once |
| Sexual Abuse | • How often did anyone 5 years older than you or an adult ever touch you sexually? | Never, Once, More than Once |
| • How often did anyone at least 5 years older than you or an adult try to make you touch them sexually? | Never, Once, More than Once | |
| • How often did anyone at least 5 years older than you or an adult force you to have sex? | Never, Once, More than Once | |
ACE, Adverse Childhood Event; BRFSS, Behavioral Risk Factor Surveillance Survey
Responses of ‘Don’t know/not sure’ and refusal to answer (not included in this table) were coded as missing values.
The occurrence of verbal abuse was defined by a “more than once” response versus “once” or “never”.
Health Factors
Current smoking was defined as reporting both having smoked at least 100 cigarettes in a lifetime and still smoking at the time of the survey. Self-reported weight (in kilograms [kg]) and height (in meters [m]) were used to calculate BMI. Overweight was defined as a BMI of at least 25 kg/m2 but <30 kg/m2, and obesity was defined as a BMI of ≥30 kg/m2. Binge drinking was defined as reporting the consumption of 4+ alcoholic drinks on at least one occasion during the past 30 days.
Covariates
Covariates were selected based on previous studies, as well as considerations of biological plausibility determined a priori. Adjustments included age, race/ethnicity (White, Asian, NHOPI, Other), education status (did not graduate from high school, high school graduate, attended college/technical school, graduated college/technical school); healthcare coverage (yes/no); meeting emotional support needs (categorized as always/usually, sometimes, rarely/never); and health factors (current smoking, BMI, and binge drinking when appropriate). Meeting emotional support needs was determined using the question: “How often do you get the social and emotional support you need?” Access to healthcare coverage was determined using the question: “Do you have any kind of healthcare coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?” Although ACEs have been shown associated with depression using this data [25], we did not include depression as a covariate as we were interested in both the direct and indirect magnitude of association between ACEs and health factors.
Statistical Analyses
Of the 6,552 participants interviewed, 59.0% (n=3,868) were women. We excluded 347 individuals who had missing values for any ACE item [1]. An additional 167 observations were removed due to missing covariates, resulting in a final sample size of 3,354 adult women.
The number of ACEs was evaluated as an ordinal variable, and ACE types were categorized as binary variables based on the presence of any corresponding item within each ACE type. Each item belonging to the categories of household dysfunction and sexual abuse were assessed individually for their impact within their respective ACE type; however, only results for categories were presented.
The distribution of population characteristics was compared by health factor status using Student’s ‘t’ and chi-square tests for continuous and categorical variables, respectively. Poisson regression with robust error variance was utilized to estimate prevalence ratios (PRs) to evaluate the relationship of ACE (count and type) with smoking, overweight, obesity and binge drinking in adulthood. Trends in the association between the number of ACEs and health factors were evaluated by treating the ordinal ACE variable as a continuous variable. We assessed interaction by race/ethnicity by creating dummy variables for Asian, NHOPI and Other race/ethnic cohorts with Whites being the referent group. These dummy variables were individually multiplied to each ACE variable, and the product terms were included in each model. Statistical evaluations included models adjusted for age, race/ethnicity, education, healthcare coverage and emotional support, as well as current smoking, BMI and binge drinking when appropriate.
There was no evidence of collinearity in the individual models between health factors (variance inflation factor [VIF] [current smoking vs. binge drinking] = 1.04; VIF [BMI or overweight or obesity vs. current smoking or binge drinking] = 1.00). All analyses took into account the complex sampling design and p-values were considered significant at a two-sided alpha <0.05. Analyses were performed using STATA (StataCorp. 2012. Stata Statistical Software: Release 12. College Station, TX) in 2014–2015.
RESULTS
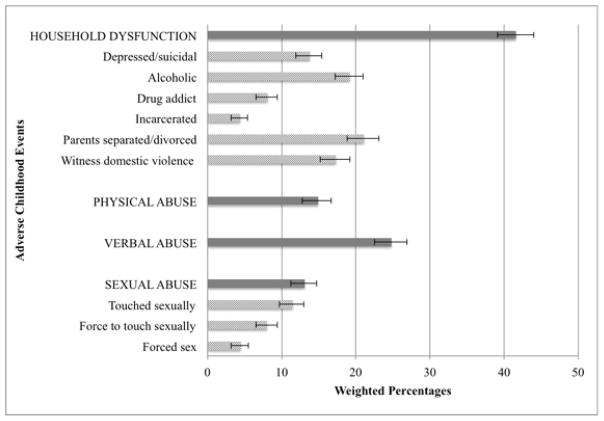
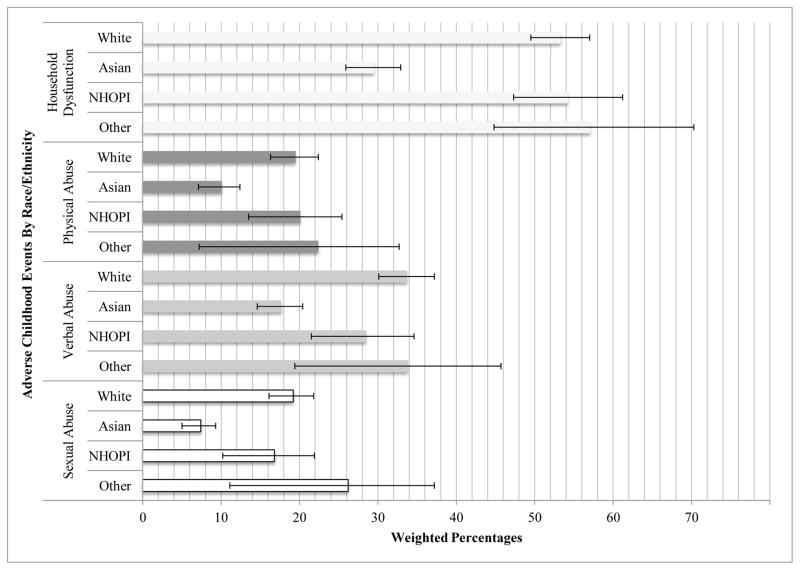
Over half of the study sample had ≥1 ACE (52.5%). Among these women, the mean number was 2.5 (standard deviation=1.7). Of the total sample, 20.8% had only 1 ACE, 11.4% with 2 ACEs, 7.5% with 3 ACEs, 5.5% with 4 ACEs and 7.4% who experienced 5+ ACEs. Overall, 41.6% reported experiencing household dysfunction during childhood, which was most commonly due to having divorced or separated parents and/or living with someone who was an alcoholic (Figure 1). There was 14.9% and 24.8% of reported physical and verbal abuse, respectively. Overall, 13.1% experienced some form of sexual abuse, which was primarily due to being touched sexually or someone trying to make the participant (as a child) touch him/her sexually. When stratified by race/ethnicity, Asians had the least frequency of any reported ACE categories (Figure 2). Whites and NHOPIs had similar percentages of reported household dysfunction and physical abuse, but Whites have slightly greater percentages of reported verbal and sexual abuse than NHOPIs. There were more reports of household dysfunction than physical, verbal or sexual abuse overall.
Figure 1. Weighted percentages of women in Hawaii reporting adverse childhood events by major categories (household dysfunction and physical, verbal and sexual abuse) and individual items within each category, Hawaii BRFSS, 2010.
NOTE: With the exception of the item, ‘Witness domestic violence’, the response for each household dysfunction item was ‘Yes’ or ‘No’. For the household item, ‘Witness domestic violence’, and the categories of physical, verbal and sexual abuse, responses included ‘Once’, ‘More than once’ or ‘Never’. With the exception of verbal abuse, a response of at least ‘Once’ defined the presence of the corresponding ACE. For verbal abuse, a response of ‘More than once’ was necessary to count as the presence of verbal abuse in the study.
Figure 2. Weighted percentages of women reporting adverse childhood events by race/ethnicity, Hawaii BRFSS, 2010.
NHOPI=Native Hawaiians and Pacific Islanders
The mean age overall was 48.6 years (median=48.0 years) with Asian women comprising the largest racial/ethnic group (50.3%; Table 2). An estimated 68.8% of the study sample had at least some college education, almost all had healthcare coverage (95.7%), and emotional support needs were mostly met always or usually (79.5%). There were 12.6% current smokers, 25.2% overweight, 20.3% obese, and 10.4% binge drinkers.
TABLE 2.
Weighted estimates of characteristic distributions of women in Hawaii, overall and by health factors
| Overall | Current Smoking | Obesec | Binge Drinking | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| na | Mean or %b | Nod | Yes | p | Nod | Yes | p | Nod | Yes | p | |
| Demographics | |||||||||||
| Mean Age (in years) | 3,354 | 48.6 | 49.3 | 44.4 | <0.001* | 48.9 | 45.7 | 0.014* | 49.9 | 38.1 | <0.001* |
| Median Age (in years) | 3,354 | 49 | 43 | --- | --- | 50 | 35 | --- | |||
| Race/ethnicity (%) | <0.001* | <0.001* | <0.001* | ||||||||
| White | 1,378 | 30.6 | 30.1 | 34.4 | 29.3 | 31.2 | 29.0 | 44.5 | |||
| Asian | 1,441 | 50.3 | 52.8 | 33.4 | 60.4 | 28.9 | 52.8 | 28.7 | |||
| NHOPI | 438 | 15.8 | 13.8 | 29.6 | 7.9 | 34.6 | 14.8 | 23.9 | |||
| Other | 97 | 3.3 | 3.4 | 2.6 | 2.3 | 5.3 | 3.4 | 2.9 | |||
| Education Status (%) | <0.001* | <0.001* | 0.165 | ||||||||
| Less than high school | 163 | 4.5 | 3.8 | 8.9 | 3.8 | 6.9 | 4.7 | 2.1 | |||
| High school graduate | 862 | 26.7 | 25.2 | 37.4 | 22.8 | 37.6 | 26.0 | 33.0 | |||
| Attended college/technical school | 997 | 29.9 | 29.2 | 35.0 | 29.2 | 30.8 | 30.2 | 27.1 | |||
| Graduated from college/technical school | 1,332 | 38.9 | 41.9 | 18.7 | 44.3 | 24.6 | 39.1 | 37.8 | |||
| Healthcare Coverage (% Yes) | 3,216 | 95.7 | 95.9 | 94.3 | 0.260 | 95.8 | 94.9 | 0.572 | 95.8 | 94.6 | 0.493 |
| Emotional Support (%) | 0.104 | 0.719 | 0.074 | ||||||||
| Rarely/never | 355 | 10.2 | 10.5 | 8.6 | 11.1 | 9.8 | 10.9 | 4.9 | |||
| Sometimes | 361 | 10.2 | 9.7 | 14.0 | 10.6 | 9.7 | 10.0 | 12.0 | |||
| Always/usually | 2,638 | 79.5 | 79.9 | 77.4 | 78.3 | 80.6 | 79.1 | 83.1 | |||
| Health Factors | |||||||||||
| Current Smoker (% Yes) | 407 | 12.6 | --- | --- | --- | 11.2 | 15.5 | 0.048* | 10.6 | 30.6 | <0.001* |
| Binge Drinker (% Yes) | 297 | 10.4 | 8.2 | 25.2 | <0.001* | 10.0 | 13.7 | 0.123 | --- | --- | --- |
| BMI | |||||||||||
| Mean (in kg/m2) | 3,354 | 25.8 | 25.6 | 26.7 | 0.012* | 21.6 | 34.9 | <0.001* | 25.7 | 26.0 | 0.657 |
| Categorical | 0.113 | --- | 0.092 | ||||||||
| Normal | 1,753 | 53.4 | 54.3 | 47.3 | --- | --- | 53.6 | 51.7 | |||
| Overweight | 949 | 25.2 | 26.0 | 27.8 | --- | --- | 26.8 | 21.5 | |||
| Obese | 652 | 20.3 | 20.0 | 24.9 | --- | --- | 19.6 | 26.7 | |||
| Adverse Childhood Events | |||||||||||
| Mean (count) | 3,354 | 1.6 | 1.4 | 2.6 | <0.001* | 1.3 | 2.3 | <0.001* | 1.5 | 2.1 | 0.002* |
| Categories (% Yes) | |||||||||||
| Household Dysfunction | 1,357 | 41.6 | 38.6 | 62.0 | <0.001* | 37.9 | 51.0 | <0.001* | 40.1 | 54.8 | 0.002* |
| Physical Abuse | 488 | 15.0 | 12.6 | 31.6 | <0.001* | 12.8 | 24.0 | <0.001* | 14.6 | 18.1 | 0.292 |
| Verbal Abuse | 838 | 24.8 | 22.7 | 39.6 | <0.001* | 21.7 | 32.2 | <0.001* | 23.7 | 34.2 | 0.008* |
| Sexual Abuse | 483 | 13.1 | 12.4 | 18.1 | 0.014* | 10.5 | 20.5 | <0.001* | 12.6 | 17.2 | 0.105 |
BMI, Body Mass Index; BRFSS, Behavioral Risk Factor Surveillance System; kg, Kilogram; m, Meter Analyses included t-tests for continuous variables and chi-square tests for categorical variables.
Unweighted number of women in Hawaii who participated in the BRFSS, 2010 with complete data, N=3,406
Weighted percentages
n=2,405 (excludes overweight participants)
No=Normal weight
Significant p-value < 0.05
Compared to current non-smokers, current smokers were significantly younger, more likely to be NHOPI, less educated, and more likely to binge drink. Similar differences were found when comparing characteristics by obesity status. Compared to those not reporting binge drinking, women who reported binge drinking were younger, more likely to be White or NHOPI, and more likely to be current smokers.
Table 3 illustrates the PRs for current smoking, overweight, obesity and binge drinking. ACE count and all four types were positively, significantly associated with current smoking taking into account socio-demographic characteristics, emotional support, healthcare coverage, BMI and binge drinking. Fully-adjusted, the magnitude of association between ACE count and smoking in adulthood increased gradually with increasing number of ACEs (p-trend<0.001). Experiencing physical abuse in childhood was associated with the highest prevalence of smoking in adulthood and sexual abuse with the highest prevalence of obesity among women in Hawaii compared to other ACE categories accounting for covariates. There was no significant interaction by race/ethnicity found between ACEs (count or categories) and current smoking.
TABLE 3.
Prevalence ratios (PR) of adverse childhood events (ACEs) with current smoking, binge drinking and overweight/obesity
| ACEs | Current Smoking PR (95% CI)b, f |
PR (95% CI)c
|
Binge Drinking PR (95% CI)e |
|
|---|---|---|---|---|
| Overweight vs. Normal Weight (n=2,702)d | Obese vs. Normal Weight (n=2,405)d, f | |||
| Model 1: Unadjusted | ||||
| Count | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 1.68 (1.13–2.50)* | 1.20 (0.99–1.46) | 1.09 (0.81–1.46) | 1.76 (1.13–2.74)* |
| 2 | 1.90 (1.25–2.87)* | 0.95 (0.73–1.24) | 1.24 (0.90–1.71) | 1.36 (0.80–2.31) |
| 3 | 2.36 (1.50–3.72)* | 1.37 (1.05–1.79)* | 1.67 (1.18–2.37)* | 2.24 (1.22–4.13)* |
| 4 | 3.11 (1.97–4.91)* | 1.31 (0.95–1.81) | 2.14 (1.56–2.95)* | 1.53 (0.82–2.85) |
| 5+ | 4.10 (2.87–5.84)* | 1.33 (0.99–1.79) | 2.32 (1.77–3.03)* | 2.24 (1.37–3.64)* |
| Categories | ||||
| Household Dysfunction | 2.30 (1.75–3.01)* | 1.11 (0.95–1.30) | 1.46 (1.20–1.78)* | 1.70 (1.22–2.37)* |
| Physical Abuse | 2.62 (1.98–3.47)* | 0.98 (0.77–1.24) | 1.67 (1.33–2.11)* | 1.25 (0.83–1.90) |
| Verbal Abuse | 1.98 (1.53–2.56)* | 1.14 (0.97–1.36) | 1.46 (1.18–1.79)* | 1.57 (1.13–2.19)* |
| Sexual Abuse | 1.47 (1.08–1.99)* | 1.16 (0.93–1.45) | 1.69 (1.34–2.13)* | 1.37 (0.94–2.01) |
| Model 2: Adjusteda | ||||
| Count | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 1.40 (0.94–2.08) | 1.22 (1.003–1.48)* | 1.00 (0.76–1.31) | 1.32 (0.86–2.02) |
| 2 | 1.56 (1.03–2.37)* | 0.98 (0.76–1.27) | 1.21 (0.91–1.60) | 0.85 (0.52–1.39) |
| 3 | 1.72 (1.04–2.83)* | 1.35 (1.03–1.76)* | 1.38 (0.99–1.94) | 1.34 (0.76–2.37) |
| 4 | 2.40 (1.56–3.69)* | 1.25 (0.89–1.74) | 1.70 (1.23–2.36)* | 0.81 (0.44–1.51) |
| 5+ | 2.55 (1.74–3.74)* | 1.31 (0.96–1.79) | 1.85 (1.42–2.43)* | 1.03 (0.64–1.66) |
| Categories | ||||
| Household Dysfunction | 1.67 (1.26–2.22)* | 1.09 (0.93–1.28) | 1.22 (1.01–1.48)* | 1.03 (0.74–1.44) |
| Physical Abuse | 2.04 (1.50–2.78)* | 0.92 (0.71–1.19) | 1.36 (1.10–1.70)* | 0.83 (0.54–1.28) |
| Verbal Abuse | 1.62 (1.25–2.10)* | 1.16 (0.97–1.38) | 1.35 (1.11–1.64)* | 0.99 (0.71–1.39) |
| Sexual Abuse | 1.19 (0.88–1.61) | 1.13 (0.91–1.40) | 1.53 (1.25–1.88)* | 1.06 (0.72–1.55) |
ACEs, Adverse Childhood Events; BRFSS, Behavioral Risk Factor Surveillance System; CI, 95% Confidence Interval; PR, Prevalence Ratio
Adjusted for age, race/ethnicity, education, emotional support, healthcare coverage
In adjusted models, BMI and binge drinking status were included.
Normal weight (n=1,753); overweight (n=949); obese (n=652)
In adjusted models, current smoking status and binge drinking status were included.
In adjusted models, current smoking and BMI were included.
Significant upward trend for smoking and obesity in fully-adjusted models (both p-value < 0.05).
Significant p-value < 0.05.
The number of ACE was positively related to both overweight and obesity in adjusted models with generally greater magnitude of association and significance for obesity. In addition, there was a significant upward trend between ACE count and obesity (p-trend<0.001). No ACE type was associated with overweight; however, women who experienced household dysfunction, and physical, verbal and sexual abuse during childhood had significantly higher prevalence of being obese in adulthood, fully-adjusted. The relationship between ACE and overweight/obesity was not found to significantly differ by race/ethnicity.
ACE count and categories were not associated with binge drinking in the overall population after adjustment for covariates. However, among the Asian cohort, sexual abuse was significantly associated with lower prevalence of binge drinking in adulthood (PR=0.26, CI=0.07–0.93), which was significantly different (interaction p=0.02) from the positive, though non-significant, association found among Whites (PR=1.39, CI=0.89–2.19) (see Table 4).
Table 4.
Prevalence ratios (PR) of sexual abuse with binge drinking by race/ethnicity
| Race/ethnicity
|
||||
|---|---|---|---|---|
| White | Asian | Native Hawaiian or Pacific Islander | Other | |
|
| ||||
| PR (95% CI) | 1.39 (0.89–2.19) | 0.26 (0.07–0.93)* | 0.94 (0.46–1.94) | 0.96 (0.15–6.26) |
| Interaction p-value | Reference | 0.016* | 0.365 | 0.707 |
Significant at a p-value <0.05
DISCUSSION
Study results found that as the number of ACEs increased, there was an increased prevalence of current smoking and obesity. These relationships did not differ by race/ethnicity. Household dysfunction, physical abuse and verbal abuse in childhood were also associated with higher odds of smoking, and all ACE categories were positively associated with adulthood obesity; however, no significant interaction by race/ethnicity was found in these relationships. Although ACE categories were not significantly related with binge drinking in the overall population, sexual abuse was found associated with lower binge drinking among Asians, which was different from the positive, though non-significant, association among Whites.
Although it has been established that ACEs are related to adverse health factors such as smoking and obesity, differences by race/ethnicity is unclear and generalizability to Asians and NHOPI populations are limited. Studies in Hawaii have shown Native Hawaiians to account for the largest number of cases of child abuse and neglect as well as a higher rate of domestic violence compared to Caucasians [11]. For Asians, reports of domestic violence are lower compared to other race groups in the state; however, underreporting due to cultural beliefs may call for needed culturally-tailored interventions.
ACEs and Current Smoking
Previous studies have found ACEs associated with smoking in adulthood [1–3]. In an assessment of a large HMO clinical database, the presence of 4+ ACEs was linked to over twice the likelihood of smoking in adulthood [1]. Further, using the same data, individuals who reported 5+ categories of ACEs were more likely to engage in early smoking initiation [2]. In a study of individuals with no significant psychopathology, a 4-fold magnitude of association was found between early childhood trauma and cigarette smoking in adulthood [26]. These overall results have also been demonstrated in studies nationwide using the BRFSS data [3–6]
ACEs have been shown to motivate the persistence of smoking, such as when ACEs lead to increased depressive symptoms [27]. Nicotine has been shown effective in regulating mood among individuals exposed to ACEs and may be especially craved during times of chronic distress including depressive episodes previously found in the current population borne from ACEs [28]. Evaluations for the presence of ACE and addressing these issues may be an essential component for smoking interventions, particularly for long-term effects.
ACEs and Obesity
Women exposed to ACEs may become obese due to increased depressive symptomatology as a consequence of experiencing a hostile childhood environment. In a previous study, ACEs were associated with elevated depressive symptoms in adulthood, particularly verbal abuse, independent of age, race/ethnicity, education, smoking, binge drinking, and meeting emotional needs [25]. Elevated depressive symptoms may promote high caloric intake and physical inactivity both of which can contribute to increased adiposity [29]. Altered patterning of diurnal rhythm due to ACEs may also contribute to obesity in adulthood. Among those with early maltreatment, the initial spike in cortisol level after awakening has been shown to remain abnormally elevated throughout the day [30–32]. This flatter diurnal slope may translate to higher than normal cortisol levels, which can potentially increase visceral adiposity leading to obesity [33].
Weight reduction interventions may benefit from assessment of ACEs and inclusion of components that address potentially existing psychological trauma, which may interfere with achieving weight loss or maintaining this reduction overtime [34, 35].
ACEs and Binge Drinking
ACEs have been associated with alcohol initiation during early- and mid-adolescence [36]. In an adult HMO, alcoholism was related to an increasing number of ACEs, independent of other variables including parental alcohol abuse [1, 37]. Previous studies assessed personal alcoholism defined by heavy drinking (i.e. 14+ drinks/week consumed during any 10-year period of adulthood); or by an affirmative answer to the questions: “Have you ever had a problem with your use of alcohol?” or “Have you ever considered yourself to be an alcoholic?” [1, 37]. In the current study we assessed binge drinking which had a more restrictive definition that was limited to a reporting of 4+ drinks in one sitting in the past 30 days. This may result in lower estimates of drinking than the other measures due to the quantity or the time frame, and potentially contribute to the lack of a statistical significance when evaluating the overall population for most of our ACE-health factor relationships. A study in California demonstrated that those living with individuals with substance abuse or mental illness were more likely to binge drink in adulthood [9] which was not supported by our findings. More so, we surprisingly found a relationship between sexual abuse during childhood and a lower prevalence of binge drinking in adulthood among Asians. It is probable that Asians who experience sexual abuse during childhood are still at an increased risk for binge drinking soon after the exposure; however, the negative effects of excessive alcohol consumption that disproportionately affect this cohort (i.e. alcohol flushing reaction) [38] may likely reinforce the non-use of alcohol, and thus more strongly dissuade use into adulthood among those exposed. The preponderance of adverse biological reaction to alcohol consumption seen among Asians may perhaps explain differences between study results. It is also plausible that stigmatization against reporting sexual abuse, particularly among Asians as demonstrated in our study, may misclassify individuals as not being exposed, although binge drinking is accounted. Participants who report sexual abuse may less likely be affected by stigma and may more likely have received treatment to address psychological issues stemming from such experience. This, in turn, may have attenuated the risk for binge drinking in adulthood. Thus, although results show an inverse relationship between sexual abuse and binge drinking, it may likely reflect the effects of stigmatization of reporting sexual abuse. Further investigation is needed to assess changes in the association between sexual abuse and binge drinking throughout the life course, and to delineate the mechanism of this relationship, particularly among Asians.
Quitting attempts to smoke or maintaining a healthy weight among women becomes particularly important during preconception and pregnancy for the health of the mother and baby. During pregnancy smoking can lead to preterm labor, ectopic pregnancy, vaginal bleeding, placental abruption and placenta previa [39], while obesity is associated with low birthweight, high blood pressure, preeclampsia, blood clotting and, in a recent study, autism in the presence of diabetes [40, 41]. Further, smoking and obesity may worsen progression of existing chronic conditions such as heart disease. Thus, it is also important that factors that maintain smoking or obesity such as ACEs be identified and intervened upon to reduce poor health outcomes. Assessment for ACEs may be beneficial in primary care environments, as well as promotion of support groups or specialists to address issues borne from ACEs. These approaches may benefit in considering cultural differences in how ACEs are perceived and tailor interventions accordingly.
Evidence that supports primary and secondary prevention of ACEs may set a foundation to start community discussions to better identify and address ACEs, and help develop resources available for those affected. In addition to better detection, an accurate account of ACEs and their association with health factors in adulthood involves the collection of appropriate data to develop indicators for maternal and child well-being. This can essentially inform intervention and surveillance of any needed modification. Prevention strategies can include community education for families on ACEs, as well as the development of services or support groups that can alleviate stressors that may promote ACEs (e.g. home visitation programs which can assist in optimizing parenting practices and household environment, ‘Big Brother/Sister’ programs). Further, partnership with child advocacy centers whose purpose is to serve children who have been neglected and/or abused may be a means to develop strategies and prevention efforts of ACEs. It could also serve as a data source to monitor the trend of ACEs overtime in particular areas, which may dictate where funding is most needed.
Strengths and Limitations
This study allows for the evaluation of a diverse multi-racial/ethnic cohort of women, including a large population of Asians and NHOPIs typically not represented in studies. It also possess noteworthy limitations. First, the cross-sectional design of the study cannot rule out reverse causality. For example, discipline against smoking during childhood may involve physical or verbal abuse. Similarly, children who are obese may also be victims of physical and verbal abuse. Longitudinal studies are necessary to better assess the causal relationship between ACEs and poor health factors. Second, recall bias may have occurred while reporting ACEs; however, no specific outcome was tied to ACEs in the survey, which may lead to non-differential misclassification, deeming our estimates to be more conservative. Third, the BRFSS data excluded institutionalized or hospitalized individuals, who may be more likely than others to have had ACE exposure and suffer from chronic disease. Inclusion of these individuals, therefore, could strengthen the estimates in this study. Fourth, landlines were the only mode used to reach participants. There might be differences between those who use cell phones as their primary contact versus those who use landlines. Updated BRFSS methods now include cell phone users, which will enable better estimates for future analyses. Fifth, the duration, frequency and gravity of ACE exposure were not assessed and may be necessary to better account for their effect on health as an adult.
Conclusion
The positive relationship of ACEs with smoking and obesity was found generalizable to a population of Asians and NHOPIs; however, a significant association between sexual abuse and binge drinking was only found among Asians. Further studies that consider cultural differences in the reporting of ACEs and how that may influence risk for adverse health factors may help inform interventions.
SIGNIFICANCE.
What is already known on this subject?
Adverse childhood events (ACEs) have been linked to smoking, obesity and alcohol use, but little is known about whether these relationships differ by race/ethnicity, or whether these findings are generalizable to understudied populations including Asians, Native Hawaiians or Pacific Islanders (NHOPIs).
What this study adds?
The current study found the association of ACEs with smoking and obesity generalizable to Asians and NHOPIs typically underrepresented in previous literature; however, it also revealed a significant association between sexual abuse and binge drinking among Asians that was different from Whites. This finding has important implications for interventions as there are variations across cultural groups with regards to prevention of ACEs and health factors such as smoking, overweight, obesity and binge drinking.
Acknowledgments
We would like to acknowledge the contribution of participants in the Hawaii BRFSS survey, particularly the women from whom the data was gathered and used for this study. The authors also appreciate the assistance from Dave Goodman and Charlan Kroelinger in the Division of Reproductive Health at the Centers for Disease Control and Prevention Maternal and Child Health Epidemiology Team who assisted in oversight and general review of the analysis. The Hawaii BRFSS survey is supported by grant from the Centers for Disease Control and Prevention (1U58/DP001962-01W1 Revision 2) and the Association of State and Territorial Chronic Disease Program Directors supported the ACE module. Additionally, this work was supported by a training grant by the National Institute of Diabetes, Digestive, and Kidney Diseases (No: T32 DK062707) and by the National Heart, Lung, and Blood Institute (No: T32 HL079891).
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the University of California-San Diego, the Hawaii Department of Health, the National Institute of Health or the Centers for Disease Control and Prevention.
The authors declare that they have no conflict of interest.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 3.Yeoman K, Safranek T, Buss B, et al. Adverse childhood experiences and adult smoking, Nebraska, 2011. Preventing Chronic Disease. 2013;10:E159. doi: 10.5888/pcd10.130009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anda RF, Brown DW. Washington State Family Policy Council, editor. Adverse childhood experiences and population health in Wasthington: The face of a chronic public health disaster. Results from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) Washington: 2010. [Google Scholar]
- 5.Gudmuson CG, Ryherd LM, Bougher K, et al. Central Iowa ACEs Steering Committee, editor. Adverse childhood experiences in Iowa: A new way of understanding lifelong health. Iowa: 2013. [Google Scholar]
- 6.Oreskovich J, Ballew C. Montana Factors, editor. The prevalence of adverse childhood experiences (ACEs) and their association with current health, Montana Behavioral Risk Factor Surveillance System (BRFSS), 2011. Helena: 2013. [Google Scholar]
- 7.Pretty C, O’Leary DD, Cairney J, et al. Adverse childhood experiences and the cardiovascular health of children: A cross-sectional study. BMC Pediatrics. 2013;13:208–213. doi: 10.1186/1471-2431-13-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye D, Reyes-Salvail F. Adverse childhood experiences among Hawai’i adults: Findings from the 2010 Behavioral Risk Factor Survey. Hawai’i Journal of Medicine & Public Health. 2014;73(6):181–190. [PMC free article] [PubMed] [Google Scholar]
- 9.Timko C, Sutkowi A, Pavao J, et al. Women’s childhood and adult adverse experiences, mental health, and binge drinking: The California Women’s Health Survey. Substance Abuse Treatment, Prevention, and Policy. 2008;3:15. doi: 10.1186/1747-597X-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kauia Committee on the Status of Women. Women’s Needs Assessment Survey. Lihue HI: 1992. [Google Scholar]
- 11.Chemtob CM, Carlson JG, Perrone P. State of Hawaii Department of of the Attorney General, editor. Domestic Violence in Hawaii: impact on mothers and their children. Honolulu, HI: 2000. [Google Scholar]
- 12.Yoshihama M. Reinterpreting strength and safety in socio-cultural context: Dynamics of domestic violence and experiencdes of women of Japanese descent. Children and Youth Services Review. 2000;22:207–227. [Google Scholar]
- 13.Shibusawa T, Yick AG. Experiences and perceptions of intimate partner violence among older Chinese immigrants. Journal of Elder Abuse & Neglect. 2007;19:1–17. doi: 10.1300/J084v19n03_01. [DOI] [PubMed] [Google Scholar]
- 14.Yoshioka M, Dang Q. Violence., A. T. F. A. D, editor. Asian family violence report: a study of the Cambodian, Chinese, Korean, South Asians, and Vietnamese Communities in Massachusetts. Boston, MA: 2000. [Google Scholar]
- 15.Yick AG. Predictors of physical spousal/intimate violence in Chinese American families. Journal of Family Violence. 2000;15:249–267. [Google Scholar]
- 16.McDonnell KA, Abdulla SE. Asian/Pacific Islander Domestic Violence Resource Project, editor. Project AWARE: Research Project. Washington, DC: 2001. [Google Scholar]
- 17.Yoshihama M. Battered women’s coping strategies and psychological distress: differences by immigration status. American Journal of Community Psychology. 2002;30:429–459. doi: 10.1023/A:1015393204820. [DOI] [PubMed] [Google Scholar]
- 18.Hawaii Health Data Warehouse. Youth Tobacco Survey Reports: Current tobacco use prevalence tables. Hawaii Youth Tobacco Survey; 2011. [Accessed November 10 2014]. http://www.hhdw.org. [Google Scholar]
- 19.Pobutsky A, Lowery St John T. Hawaii State Department of Health, editor. Smoking and tobacco use in Hawai’i: Facts, figures and trends. Honolulu: 2010. [Google Scholar]
- 20.Center for Disease Control. [Accessed June 6 2014];Overweight and Obesity. 2012 http://www.cdc.gov/obesity/stateprograms/fundedstates/hawaii.html.
- 21.Center for Disease Control; Center for Disease Control, editor. Vital and Health Statistics. Atlanta: Center for Disease Control; 2012. Summary Health Statistics for US Adults: National Health Interview Survey, 2010. [Google Scholar]
- 22.HMSA Foundation. [Accessed Dec 12 2012];Health Status - Alcohol Use. 2008 http://www.healthtrends.org/status_behave_alcohol.aspx.
- 23.White A. American Statistical Association, editor. Response rate calculation in RDD telephone health surveys: Current practices. Washington (DC): National Center for Health Statistics; 1984. [Google Scholar]
- 24.Center for Disease Control and Prevention. Adverse childhood experiences reported by adults. Five states, 2009. [Report] Morbidity and Mortality Weekly Report (MMWR) 2010;59(49):1609–1613. [PubMed] [Google Scholar]
- 25.Remigio-Baker RA, Hayes DK, Reyes-Salvail F. Adverse childhood events and current depressive symptoms among women in Hawaii: 2010 BRFSS, Hawaii. Matern Child Health J. 2014;18(10):2300–2308. doi: 10.1007/s10995-013-1374-y. [DOI] [PubMed] [Google Scholar]
- 26.Spratt EG, Back SE, Yeatts SD, et al. Relationship between child abuse and adult smoking. Int J Psychiatry Med. 2009;39(4):417–426. doi: 10.2190/PM.39.4.f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Edwards VJ, Anda RF, Gu D, et al. Adverse childhood experiences and smoking persistence in adults with smoking-related symptoms and illness. The Permanente Journal. 2007;11(2):5–13. doi: 10.7812/tpp/06-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pomerleau OF, Pomerlaeu CS. Neuroregulators and the reinforcement of smoking: Towards a biobehavioral explanation. Neurosci biobehav Rev. 1984;8:503–513. doi: 10.1016/0149-7634(84)90007-1. [DOI] [PubMed] [Google Scholar]
- 29.Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299(23):2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dozier M, Manni M, Gordon MK, et al. Foster children’s diurnal production of cortisol: An exploratory study. Child Maltreatment. 2006;11(2):189–197. doi: 10.1177/1077559505285779. [DOI] [PubMed] [Google Scholar]
- 31.Weissbecker I, Floyd A, Dedert E, et al. Adverse early events: Childhood trauma and diurnal cortisol disruption in fibromyalgia. Psychoneuroendocrinology. 2006;31(3):312–324. doi: 10.1016/j.psyneuen.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 32.Nicolson NA, Davis MC, Kruszewski D, et al. Childhood maltreatment and diurnal cortisol patterns in women with chronic pain. Psychosom Med. 2010;72(5):471–480. doi: 10.1097/PSY.0b013e3181d9a104. [DOI] [PubMed] [Google Scholar]
- 33.Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2(2):73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 34.Chrousos GP. The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: Neuro-endocrine and target tissue-related causes. International Journal of Obesity and Related Metabolic Disorders. 2000;24(Suppl 2):S50–S55. doi: 10.1038/sj.ijo.0801278. [DOI] [PubMed] [Google Scholar]
- 35.Nemeroff CB. Neurobiological consequences of childhood trauma. J Clin Psychiatry. 2004;65(Suppl 1):18–28. [PubMed] [Google Scholar]
- 36.Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38(4):444e441–444.e410. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 37.Anda RF, Whitfield CL, Felitti VJ, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr Serv. 2002;53(8):1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- 38.Tu GC, Israel Y. Alcohol consumption by orientals in North America is predicted largely by a single gene. Behav Genet. 1995;25(1):59–65. doi: 10.1007/BF02197242. [DOI] [PubMed] [Google Scholar]
- 39.March of Dimes Foundation. [Accessed Apr 22 2016];Smoking during pregnancy. 2016 http://www.marchofdimes.org/pregnancy/smoking-during-pregnancy.aspx.
- 40.March of Dimes Foundation. [Accessed Apr 22 2016];Being overweight during pregnancy. 2016 http://www.marchofdimes.org/pregnancy/being-overweight-during-pregnancy.aspx.
- 41.Li M, Fallin MD, Landa AR, et al. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics. 2016;137(2):e20152206. doi: 10.1542/peds.2015-2206. [DOI] [PMC free article] [PubMed] [Google Scholar]