Abstract
Introduction
Cigarette smoking is the single greatest preventable cause of disease and death. Our literature review highlights the increased risk of cigarette smoking and kidney cancer, bladder cancer and prostate cancer.
Material and methods
Smoking cessation improves outcomes at all stages of these disease processes, where patients who quit for 10–20 years appear to obtain a similar risk as those who have never smoked, even after diagnosis of disease.
Results
Urologists, however, very seldom provide smoking cessation assistance. By applying brief smoking cessation intervention techniques, physicians’ posses an effective means of providing quitting advice.
Conclusions
Patients who receive smoking cessation advice from their urologist are 2.3 times more likely to attempt to quit. Urologists are well-positioned to screen, counsel, and promote cessation at regular intervals, which may improve quit rates, and ultimately improve our patients’ outcomes.
Keywords: bladder, kidney, prostate, erectile dysfunction, smoking cessation
Cigarette smoking is the single greatest preventable cause of disease and death, being responsible for 1 in every 5 deaths each year [1]. The World Health Organization estimates that cigarette use kills nearly 6 million people worldwide every year. More than 5 million of those deaths are the result of direct tobacco use while more than 600,000 are the result of non-smokers being exposed to second-hand smoke, making smoking one of the largest threats to public health. Smoking is a leading cause of cancer and death from cancer. It causes cancers of the lungs, esophagus, larynx, mouth, throat, liver, pancreas, stomach, cervix, colon, and rectum, as well as acute myeloid leukemia. Furthermore, cigarette smoking is linked to several genitourinary malignancies including kidney, bladder, and prostate cancer as well as infertility and erectile dysfunction.
The adverse health consequences of tobacco use are well documented, widely acknowledged, and smoking demands the use of primary prophylaxis along with continued smoking cessation counselling. As many urologic malignancies are associated with smoking, we as urologists, are in the unique role to encourage our patients not to begin smoking, as this decreases tobacco-related disease morbidity, and counsel those who smoke to stop, as this improves therapeutic results of their diseases.
Kidney cancer
Smoking is a well-established risk factor for renal cell carcinoma (RCC) [2]. A meta-analysis with pooled data from 19 controlled cases and 5 cohort studies confirmed that smoking increases the risk of RCC (RR 1.38, 95% Cl 1.27–1.50) [2]. Smoking has also been found to be an independent risk factor for advanced RCC, leading to a 1.5-fold increase in the odds of advanced disease compared to non-smokers [3]. Patients who quit smoking for 20 years reduce their risk for advanced RCC to that of patients who never smoked [3]. These results reinforce the importance of smoking prevention and cessation in this disease [4].
Bladder cancer
Although bladder cancer (BCa) is a substantial public health burden, it is also highly preventable as cigarette smoking is the number one environmental cause of this malignancy [5]. The risk of BCa correlates with smoking quantity (the number of cigarettes smoked daily) and smoking duration as well as age at smoking initiation, and type of tobacco smoked. Secondhand smoke exposure is also associated with a significant increase in BCa risk [4]. Cumulative smoking exposure (combined duration and quantity) has been associated with BCa recurrence, progression, and overall survival in both non-muscle-invasive and muscle-invasive BCa [6].
Smoking cessation substantially prolongs life at every stage. Smoking cessation for 1 to 4 years results in a 30% decrease in the risk of BCa [7]. Even after the diagnosis of BCa, smoking cessation of over 10 years reverts the risks of cancer progression and death to that of non-smokers. Actual smoking at the time of diagnosis has been associated with worse disease associated outcomes compared to former smokers, while those who quit substantially reduce the risk of recurrent BCa [5]. Given the need for frequent follow-up office visits in addition to surveillance cystoscopies, urologists are in a unique position to promote patient awareness of this topic and offer smoking cessation counselling and intervention [4, 8]. Given the high socioeconomic burden of BCa, prevention and cessation interventions are likely to be cost-effective for the society.
Prostate cancer
Cigarette use is the leading cause of death from cancer but the relationship between smoking and prostate cancer (PCa) remains controversial. Considerable evidence has, however, linked cigarette smoking to a more aggressive disease at diagnosis, biochemical recurrence, and PCa mortality [9]. Of 5366 men diagnosed with prostate cancer in the Health Professionals Follow-Up Study, current smokers had a 61% greater risk of PCa mortality and biochemical recurrence compared to those who never smoked [10]. Men who have quit smoking for at least 10 years demonstrated PCa specific mortality risks similar to those who have never smoked.
Several observation PCa studies have shown that smoking is associated with a worse outcome in patients treated with radiotherapy, medical, or surgical treatment. In patients undergoing radical prostatectomy, smoking was associated with adverse pathologic features (greater volumes and high grade cancer) and a higher risk of biochemical recurrence in men undergoing radical prostatectomy [11, 12]. A similar scenario is evident for patients treated with radiotherapy or androgen deprivation therapy [13]. Smoking at PCa diagnosis negatively impacts PCa-specific, long-term survival, regardless of Gleason score [14]. The influence of smoking on PCa screening and PSA evaluation has been also investigated, providing a great opportunity for smoking counselling [9].
Role of urologists in smoking cessation
Smoking remains a leading contributor to urological health problems and premature death. Even though smoking impacts nearly every aspect of urological health ranging from the development and prognosis of prostate, bladder, and renal cell carcinoma, to erectile dysfunction, lower urinary tract symptoms including benign prostate hyperplasia, chronic prostatitis, and chronic pelvic pain syndrome, there exists a paucity of research on how we, as urologists, can impact our patients through smoking cessation counselling [16, 17]. The urological and scientific community has, however, begun to address this lack of research through several different avenues. First, the inaugural issue of ‘European Urology Focus’ was dedicated entirely to the effects of smoking on urological health, highlighting how we must accept the responsibility and better counsel our patients about the detrimental effects of smoking and assist them in cessation efforts to improve their health and lives. Second, the American College of Surgeons (ACS) recently published a policy statement entitled “The effects of tobacco use on surgical complications and the utility of smoking cessation counselling” underscoring how the perioperative time is a critical window of opportunity to help patients realize the importance of their role in their own surgical outcomes and how smoking cessation can influence the success of their operation. The ACS emphasizes that surgeons should play an active role in smoking cessation counselling with their patients and promotes educational programs on effective smoking cessation strategies. Third, number of PubMed indexed articles on the topic of smoking and urology has grown exponentially; there have been 905 references in the last 10 years with 619 (68%) of these published in the last 5 years. Strides such as these have promoted a better understanding and implementation of smoking cessation in our patient care.
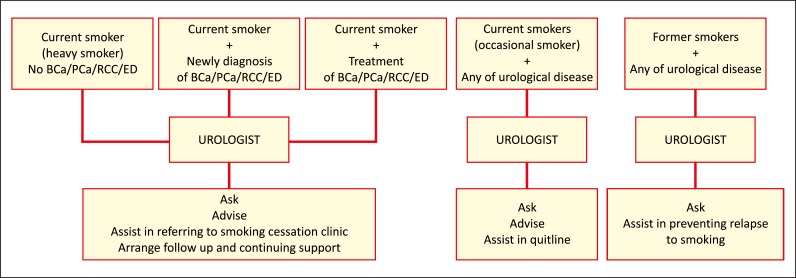
Given the wide variety of genitourinary diseases affected by cigarette smoking, along with patients’ varying degrees of tobacco dependence, urologists appear well positioned to influence patient tobacco use (Figure 1) [17]. Studies have shown that patients who receive smoking cessation advice from their urologist are 2.3 times more likely to attempt to quit [8]. The diagnosis of cancer may represent a window of opportunity during which patients are particularly motivated to quit smoking and are receptive to advice. This teachable moment has been shown to result in successful smoking cessation in 48% of BCa patients and was the most often cited reason for quitting [18]. Smokers with a new diagnosis of BCa are at least five times more likely to quit smoking than those in the general population (48% vs. 10%, respectively; p <0.001). With this in mind, physicians should give advice that clearly connects the patient’s illness or potential illness with smoking.
Figure 1.
The role of urologists in the smoking cessation process. BCa – bladder cancer; PCa – prostate cancer; RCC – kidney cancer, ED – erectile dysfunction.
Contrary to common perceptions, active anti-smoking actions in the form of a 5-minute brief smoking cessation intervention are not time prohibitive and are easily incorporated into daily clinical practice [8]. Brief interventions along with straightforward smoking cessation advice such as “As your urologist, I must advise you that smoking is risky for your health, and it would be important for you to stop“ has been shown to increase smoking cessation [18]. Indeed, failure to address smoking is interpreted as a sign of acceptance by the patient. Optimal smoking cessation counselling can be further individualized and in some cases rely on the strict collaboration with specialized institutions [18]. Continuing to assist the patient in abstaining from smoking by a referral to a smoking cessation clinic, telephone quite line, psychologist support, and/or a patient support group is often a necessary element in order to achieve permanent smoking cessation. Furthermore, providing pharmacological smoking cessation therapy such as nicotine replacement therapy, Varenicline, or bupropion, has proven efficient in cessation rates.
The health awareness of smoking associated urological diseases remains low. Therefore, it is crucial for urologists to engage in primary prevention, social campaigns and multidisciplinary health-promoting actions. While such an approach will undoubtedly improve overall health, it may also improve overall kidney, prostate, bladder cancer and erectile dysfunction outcomes.
Although data is accruing to support the importance of smoking cessation in urological health along with the role of the urologist in providing advice on quitting, there remains obstacles to the universal adoption of smoking cessation counselling. First, to date there are no European or American urological guidelines or consensus statements directing urologists on appropriate strategies for providing smoking cessation counselling. Second, urologists frequently do not feel qualified to provide smoking cessation counselling, while only a fraction of urologists have had formal smoking cessation training themselves (Bjurlin American urologist survey reference). This in turn may lead to a limited use of pharmacological smoking cessation therapy which has been shown to clearly be beneficial in increasing quit rates. Third, pharmacological smoking cessation therapy is not fully reimbursed by health insurance in most European countries despite its proven efficacy and cost-effectiveness, which may ultimately deter its use and subsequently the number of successful quitters (Reda AA, Kotz D, Evers SM, van Schayck CP. Healthcare financing systems for increasing the use of tobacco dependence treatment. Cochrane Database Syst Rev 2012;6:CD004305). In order to address these hurdles in providing smoking cessation, knowledge of tobacco cessation and control actions should be considered for inclusion in the core curriculum of urological training. Moreover, establishment of practice pattern guidelines for smoking cessation counselling by the European Urology Association and the American Urological Association may provide a framework for which urologists can offer quit advice. As advocates for our patients, we must accept the responsibility and better counsel our patients about the detrimental effects of smoking and assist them in cessation efforts to improve their health and lives.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunt JD, van der Hel OL, McMillan GP, Boffetta P, Brennan P. Renal cell carcinoma in relation to cigarette smoking: meta-analysis of 24 studies. Int J Cancer. 2005;114:101–108. doi: 10.1002/ijc.20618. [DOI] [PubMed] [Google Scholar]
- 3.Tsivian M, Moreira DM, Caso JR, Mouraviev V, Polascik TJ. Cigarette smoking is associated with advanced renal cell carcinoma. J Clin Oncol. 2011;29:2027–2031. doi: 10.1200/JCO.2010.30.9484. [DOI] [PubMed] [Google Scholar]
- 4.Cumberbatch MG, Rota M, Catto JW, La Vecchia C. The Role of Tobacco Smoke in Bladder and Kidney Carcinogenesis: A Comparison of Exposures and Meta-analysis of Incidence and Mortality Risks. Eur Urol. 2016;70:458–466. doi: 10.1016/j.eururo.2015.06.042. [DOI] [PubMed] [Google Scholar]
- 5.Burger M, Catto JW, Dalbagni G, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63:234–241. doi: 10.1016/j.eururo.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 6.Crivelli JJ, Xylinas E, Kluth LA, Rieken M, Rink M, Shariat SF. Effect of smoking on outcomes of urothelial carcinoma: a systematic review of the literature. Eur Urol. 2014;65:742–754. doi: 10.1016/j.eururo.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 7.Brennan P, Bogillot O, Cordier S, et al. Cigarette smoking and bladder cancer in men: a pooled analysis of 11 case-control studies. Int J Cancer. 2000;86:289–294. doi: 10.1002/(sici)1097-0215(20000415)86:2<289::aid-ijc21>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 8.Bjurlin MA, Cohn MR, Kim DY, et al. Brief smoking cessation intervention: a prospective trial in the urology setting. J Urol. 2013;189:1843–1849. doi: 10.1016/j.juro.2012.11.075. [DOI] [PubMed] [Google Scholar]
- 9.Islami F, Moreira DM, Boffetta P, Freedland SJ. A systematic review and meta-analysis of tobacco use and prostate cancer mortality and incidence in prospective cohort studies. Eur Urol. 2014;66:1054–1064. doi: 10.1016/j.eururo.2014.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kenfield SA, Stampfer MJ, Chan JM, Giovannucci E. Smoking and prostate cancer survival and recurrence. JAMA. 2011;305:2548–2555. doi: 10.1001/jama.2011.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ngo TC, Lee JJ, Brooks JD, Nolley R, Ferrari M, Presti JC., Jr Smoking and adverse outcomes at radical prostatectomy. Urol Oncol. 2013;31:749–754. doi: 10.1016/j.urolonc.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 12.Rieken M, Shariat SF, Kluth LA, et al. Association of Cigarette Smoking and Smoking Cessation with Biochemical Recurrence of Prostate Cancer in Patients Treated with Radical Prostatectomy. Eur Urol. 2015;68:949–956. doi: 10.1016/j.eururo.2015.05.038. [DOI] [PubMed] [Google Scholar]
- 13.Moreira DM, Aronson WJ, Terris MK, et al. Cigarette smoking is associated with an increased risk of biochemical disease recurrence, metastasis, castration-resistant prostate cancer, and mortality after radical prostatectomy: results from the SEARCH database. Cancer. 2014;120:197–204. doi: 10.1002/cncr.28423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polesel J, Gini A, Dal Maso L, et al. The negative impact of tobacco smoking on survival after prostate cancer diagnosis. Cancer Causes Control. 2015;26:1299–1305. doi: 10.1007/s10552-015-0624-2. [DOI] [PubMed] [Google Scholar]
- 15.Cao S, Gan Y, Dong X, Liu J, Lu Z. Association of quantity and duration of smoking with erectile dysfunction: a dose-response meta-analysis. J Sex Med. 2014;11:2376–2384. doi: 10.1111/jsm.12641. [DOI] [PubMed] [Google Scholar]
- 16.Harte CB, Meston CM. Association between smoking cessation and sexual health in men. BJU Int. 2012;109:888–896. doi: 10.1111/j.1464-410X.2011.10503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sosnowski R, Verze P, Nunzio C, Bjurlin MA. Re: Marcus G. Cumberbatch, Matteo Rota, James W.F. Catto, Carlo La Vecchia. The Role of Tobacco Smoke in Bladder and Kidney Carcinogenesis: A Comparison of Exposures and Meta-analysis of Incidence and Mortality Risks. Eur Urol. In press. http: Smoking Cessation and Urology: A New Domain for Prevention and Treatment. Eur Urol. 2015 doi: 10.1016/j.eururo.2015.09.035. [In press] [DOI] [Google Scholar]
- 18.Sosnowski R, Przewozniak K. The role of the urologist in smoking cessation: why is it important? Urol Oncol. 2015;33:30–39. doi: 10.1016/j.urolonc.2014.07.011. [DOI] [PubMed] [Google Scholar]