Abstract
Introduction
Latent class analysis provides a method for understanding patterns of physical activity and sedentary behavior. This study explored the association of accelerometer-assessed patterns of physical activity/sedentary behavior with all-cause mortality.
Methods
The sample included 4,510 U.S. National Health and Nutrition Examination Survey participants aged ≥ 40 years enrolled in 2003–2006 with mortality follow-up through 2011. Participants wore a hip-worn accelerometer for 1 week that provided minute-by-minute information on physical activity/sedentary behavior. Accelerometry patterns were derived using latent class analysis. Cox proportional hazards models provided adjusted hazard ratios with 95% CIs. Analyses were conducted from 2014 to 2016.
Results
During an average of 6.6 years of follow-up, 513 deaths occurred. For average counts/minute, the more-active classes had a lower risk of mortality compared with the lowest Class 1. Findings were generally similar for percentage of the day in minutes and bouts of moderate to vigorous physical activity, defined two ways. For percentage of the day in sedentary behavior, generally no associations were identified. However, the class with the highest percentage of the day in sedentary bouts (Class 1) had a higher risk of mortality (adjusted hazard ratio, 2.10; 95% CI=1.11, 3.97) versus the class with fewer sedentary bouts (Class 7).
Conclusions
In this national observational study, time spent in more physical activity reduced the risk of all-cause mortality and time spent in more sedentary bouts increased the risk of all-cause mortality, regardless of how both was accumulated. The latent class analysis contributed to understanding the impact of patterning of physical activity/sedentary behavior on mortality.
INTRODUCTION
Accelerometry has emerged as a useful tool to assess detailed information about physical activity and sedentary behavior in epidemiologic studies.1 Adults typically wear accelerometers for 1 week and the device records accelerations in one or multiple planes of movement for each length or epoch of time. From this recording, calibration studies provide translational cut points to interpret the intensity level for each epoch. Typically, epochs are classified into sedentary behavior, and light, moderate, or vigorous activity, and the weekly sum provides number of total minutes in each intensity. Although this grouping of duration is useful, it ignores potential differences in the patterns of accumulated sedentary behavior and physical activity over time.
Latent class analysis (LCA) has emerged as a method, when applied to accelerometry, to understand how physical activity and sedentary behavior are patterned over a week. Patterns could be explored within or across days. LCA assumes participants belong to one of several mutually exclusive classes, derived through statistical modeling. The pattern of conditional probabilities that indicate the chance that a variable takes on certain values comprises the class.
In 2008, an initial application of this method was applied to accelerometry to derive classes for day-to-day moderate to vigorous physical activity (MVPA)2 and the authors subsequently found inverse associations with lower MVPA associated with metabolic syndrome risk factors.3 In this example, participants were grouped based on their observed daily MVPA into different types of patterns or latent classes. Following this work, latent classes for sedentary behavior and MVPA, as well as an indicator of average intensity of physical activity, were developed among a national sample of adults.4 Distinct day-to-day patterns emerged that varied by age, race/ethnicity, gender, and other factors.4,5 For example, the weekend warrior pattern of lower MVPA on the weekdays and higher MVPA on the weekends was more frequent among men, younger ages, and non-Hispanics compared with other race/ethnic groups.
A search of the literature suggests that studies exploring the association of accelerometry on mortality primarily focus on the accumulated time spent in various intensity levels, but not on the day-to-day patterning.6 It may be that the way physical activity/sedentary behavior is accumulated each day impacts mortality that would not be observed by using summary measures of total time in physical activity/sedentary behavior alone. Using data from a national study among adults aged ≥ 40 years, this study explored accelerometry-assessed day-to-day patterns of physical activity and sedentary behavior with all-cause mortality.
METHODS
Data Sources
The study was approved by the University of North Carolina IRB and National Health and Nutrition Examination Survey (NHANES) participants provided written informed consent.7 The data used in this study were collected in 2003–2006, the most recently available accelerometer data, and analyses were conducted from 2014 to 2016. The 2003–2006 NHANES data were linked to the National Death Index by the National Center for Health Statistics. All-cause mortality was defined as any cause of death, except for deaths related to external causes (ICD-10 V01-Y89). Participants who died of external causes were censored on their death day. Follow-up was calculated as the interval between the NHANES examination date and either the death date, censor date, or December 31, 2011, whichever occurred first.
Measures
This section includes a description of the accelerometry measures, with other study measures described in the Appendix. Those who participated in the physical activity monitor examination were asked to wear the ActiGraph accelerometer (AM7164) on their hip for 1 week during waking hours and not during water-based activities. Beginning at midnight on the day following the clinic visit, the accelerometer recorded 1-minute epochs of analog acceleration and were converted to a digital signal.8
For the accelerometer readings, non-wear was defined by an interval of ≥ 90 consecutive minutes of zero counts/minute, with allowance of up to 2 minutes of nonzero counts if no counts were detected during both the 30 minutes upstream and downstream from that interval.9 Any nonzero counts (except the allowed short intervals) were considered wear time. Counts in the non-wear period were set to missing. To be included in the analysis, ≥ 3 adherent days with an adherent day indicating ≥8 hours of accelerometer wear were required.
Average counts/minute were used to explore average physical activity intensity. Cut points originally applied to NHANES, primarily from calibration studies of treadmill walking and running, were also applied to the accelerometry data.10 Vigorous intensity was defined as ≥ 5,999 counts/minute, moderate intensity as 2,020–5,998 counts/minute, and light intensity as 100–2,019 counts/minute. A lower MVPA intensity threshold (MVPA_lifestyle) was calculated based on studies that incorporated more lifestyle activities, defined as ≥ 760 counts/minute,11 with light intensity defined between 100–759 counts/minute. Information on the cut point validity is available elsewhere.12–14 An MVPA bout was defined as ≥ 10 minutes of consecutive MVPA minutes with allowance for interruptions for up to 20% of the time below the threshold and <5 consecutive minutes below the threshold. The MVPA bout had to start and end with MVPA. Sedentary behavior was defined as <100 counts/minute.15 Sedentary bouts were defined as ≥ 30 minutes with at least 80% of the minutes falling below the sedentary threshold, allowing for <5 consecutive minutes above the threshold. The sedentary bout had to start and end with sedentary behavior.
This study used LCA to develop natural groupings of participants who tended to accumulate their accelerometer-assessed physical activity or sedentary behavior similarly.4 The LCA was performed using MPlus, version 7.11, which allowed for the complex survey design in conjunction with the modeling. Mixture modeling was applied to describe the relationship between up to 7 adherent days of accelerometry and the categorical latent variable using a set of linear regression equations. Owing to the large number of participants with zero for percentage of MVPA bouts out of total wear time, a zero-inflated negative binomial model was used for this measure only. Details on the process to make the final selection of classes for each variable are described elsewhere.4 The derived classes were among participants who shared similar means, separately calculated for the following variables:
counts/minute per day;
percentage of MVPA/MVPA_lifestyle out of total wear time/day;
percentage of MVPA/MVPA_lifestyle bouts out of total wear time/day;
percentage of sedentary behavior out of total wear time/day; and
percentage of sedentary bouts out of total wear time/day.
Each participant was assigned to one class for each measure, based on the highest posterior class membership probability. The final classes for MVPA and sedentary behavior were based on relative percentages in order to best account for accelerometer wear time.
Study Sample
The sample was limited to participants aged ≥ 40 years (N=6,355) and excluded those not eligible for mortality linkage due to being unable to match their NHANES record to the National Death Index (n=7). To account for prevalent conditions that might affect physical activity/sedentary behavior, those who died in the first 2 years of follow-up (n=262) were excluded. Those who either did not wear the accelerometer (n=792) or who wore the accelerometer but upon return it was not in calibration (n=251) or was faulty (i.e., recording no counts; n=102) were also excluded. The cohort was further limited by excluding those who did not provide adherent data (≥3 days of accelerometer wear for ≥8 hours/day over the week; n=277). Lastly, those missing self-reported physical activity or any potential confounder (i.e., age, gender, race/ethnicity, education, marital status, smoking, employment, needing special equipment to walk, arthritis, cancer, coronary heart disease, angina, myocardial infarction, stroke, BMI, diabetes, hypertension) in the final models (n=154) were excluded, which left a final sample size of 4,510.
Statistical Analysis
This study used SAS, version 9.3 for all analyses, accessed at a National Center for Health Statistics Research Data Center (www.cdc.gov/rdc/index.htm). Frequencies and means were calculated using the SURVEYFREQ and SURVEYMEAN procedures, respectively, using the 4-year sample weights provided by NHANES. Multivariable Cox proportional hazards models helped assess the association of the accelerometer-derived latent class measures with mortality.
These models were calculated using PHREG and accounted for all variables that comprised the weights in every model (age, race/ethnicity, gender).16 A linear test for trend was calculated by representing the latent class assignments as an ordinal score and obtaining a p-value for that variable. Although the authors had information on the measurement day of the week, the order of these days was not known (e.g., one participant might start the 7-day window on Friday, so that Thursday and Friday data were collected 1 week apart). The latent class models did not make assumptions about proximity of days of the week, but rather controlled for day of the week without the assumption that measures fell on adjacent days. Four model variations were considered with the latent classes included as categorical exposure measures that are described in the Appendix. The proportional hazard assumption was tested using time-dependent covariates.17
RESULTS
Over an average of 6.6 years of follow-up (median, 6.7; interquartile range, 5.6–7.8), 513 deaths occurred (11.4%). Overall, 14 deaths were censored owing to external causes (ICD-10 V01-Y89). The mean age of the sample (≥40 years) was 56.5 years, with 53.7% female, 7.9% Hispanic, 10.1% non-Hispanic black, 77.6% non-Hispanic white, and 4.4% other. Further descriptive characteristics of the sample and the accelerometer summary measures are in Table 1. The weighted means/percentages and median time spent in each intensity for the latent class assignments can be found in Appendix Tables 1 and 2, respectively. A description of the self-reported physical activity and screen time measures by latent class are also reported in the Appendix.
Table 1.
Descriptive Information on Adults ≥ 40 Years (n=4,510), NHANES 2003–2006
| Characteristics | N | Weighted % (SE) | Missing N |
|---|---|---|---|
| Age | 0 | ||
| 40–49 | 1,207 | 34.6 (1.3) | |
| 50–59 | 957 | 29.6 (1.0) | |
| 60–69 | 1,097 | 18.4 (0.7) | |
| 70 and older | 1,249 | 17.4 (1.1) | |
| Gender | 0 | ||
| Male | 2,221 | 46.3 (0.9) | |
| Female | 2,289 | 53.7 (0.9) | |
| Race/Ethnicity | 0 | ||
| Non-Hispanic white | 2,489 | 77.6 (2.2) | |
| Non-Hispanic black | 927 | 10.1 (1.3) | |
| Hispanic | 940 | 7.9 (1.2) | |
| Other | 154 | 4.4 (0.5) | |
| Education | 0 | ||
| Less than high school | 1,342 | 16.9 (1.1) | |
| High school graduate/GED | 1,092 | 26.3 (0.7) | |
| Greater than high school | 2,076 | 56.8 (1.4) | |
| Household income | 254 | ||
| <$15,000 | 671 | 9.4 (0.7) | |
| $15,000–<$34,999 | 1,285 | 23.2 (0.8) | |
| $35,000–<$64,999 | 1,152 | 29.7 (1.4) | |
| >=$65,000 | 1,148 | 37.7 (2.0) | |
| Marital status | |||
| Married | 2,748 | 66.2 (1.2) | 0 |
| BMI (kg/m2) | 0 | ||
| Underweight (<18.5) | 44 | 1.1 (0.2) | |
| Normal (18.5–<25) | 1,156 | 26.5 (1.0) | |
| Overweight (25–<30) | 1,689 | 36.4 (0.9) | |
| Obese class I (30–<35) | 983 | 21.5 (0.7) | |
| Obese class II or III (>=35) | 638 | 14.5 (0.7) | |
| Cigarette smoking | 0 | ||
| Never | 2,112 | 47.3 (1.0) | |
| Former | 1,512 | 32.1 (0.9) | |
| Current | 886 | 20.5 (0.9) | |
| Need special equipment to walk (yes) | 519 | 8.7 (0.5) | 0 |
| Arthritis (yes) | 1,730 | 35.5 (1.1) | 0 |
| >=12 alcoholic drinks/year (yes) | 2,892 | 71.0 (1.7) | 244 |
| Employment | 2,170 | 60.0 (1.5) | |
| C-reactive protein in mg/dL | 145 | ||
| <0.3 | 2,568 | 61.1 (1.0) | |
| >=0.3 | 1,797 | 38.9 (1.0) | |
| Hypertension | 0 | ||
| No | 929 | 24.2 (0.9) | |
| Prehypertension | 962 | 24.0 (1.0) | |
| Yes | 2,619 | 51.8 (1.3) | |
| Diabetes | 0 | ||
| No | 2,752 | 69.2 (1.0) | |
| Prediabetes | 960 | 17.5 (0.8) | |
| Yes | 798 | 13.3 (0.7) | |
| Cancer or malignancy | 0 | ||
| No | 3,935 | 87.5 (0.6) | |
| Non-Melanoma skin cancer | 155 | 3.7 (0.3) | |
| Any other type of cancer | 420 | 8.8 (0.5) | |
| Angina (yes) | 223 | 4.1 (0.4) | 0 |
| Myocardial infarction (yes) | 292 | 5.2 (0.4) | 0 |
| Stroke (yes) | 223 | 3.6 (0.3) | |
| Coronary heart disease (yes) | 276 | 5.0 (0.4) | |
| Congestive heart failure (yes) | 197 | 3.3 (0.3) | |
| Usual daily activities (self-report) | 6 | ||
| Mostly sitting | 1,111 | 23.9 (0.9) | |
| Mostly standing/walking without carrying/lifting | 2,460 | 52.9 (0.9) | |
| Carry/lift light load/heavy work | 933 | 23.2 (1.2) | |
|
| |||
| Characteristics | N | Weighted mean (SE) | Missing N |
|
| |||
| Age | 4,510 | 56.5 (0.4) | 0 |
| BMI | 4,510 | 29.0 (0.1) | 0 |
| Total cholesterol in mg/dL | 4,349 | 206.3 (0.8) | 161 |
| C-reactive protein in mg/dL | 4,365 | 0.4 (0.02) | 145 |
| Accelerometer measures | 4,510 | 0 | |
| Average counts/minute | 282.1 (3.2) | ||
| Sedentary behavior (hours/day) | 8.1 (0.1) | ||
| Sedentary bouts (hours/day) | 6.3 (0.1) | ||
| Light activity (minutes/day) | 305.9 (2.2) | ||
| MVPA (minutes/day) | 17.7 (0.5) | ||
| MVPA bouts (minutes/day) | 5.2 (0.3) | ||
| MVPA_lifestyle (minutes/day) | 91.1 (1.5) | ||
| MVPA_lifestyle bouts (minutes/day) | 32.2 (0.9) | ||
NHANES, National Health and Nutrition Examination Survey; MVPA, moderate to vigorous physical activity
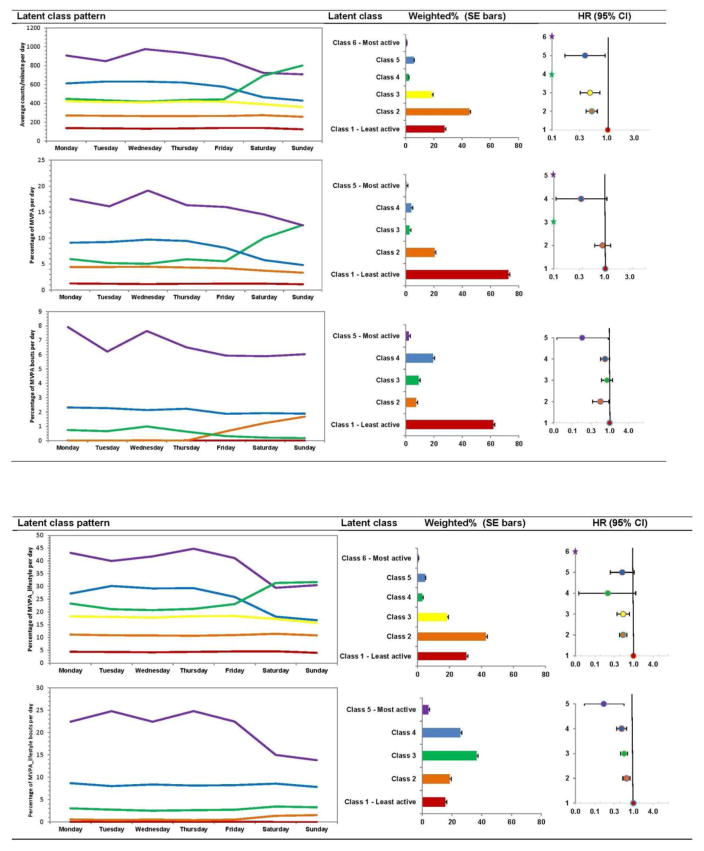
The models for each physical activity class measures are presented in Appendix Table 3, with Model 3 plotted in Figure 1. For average counts/minute, adjustment for accelerometer wear time (Model 1A) and potential mediators (Model 3) did not meaningfully change interpretations compared to Model 1. For average counts/minute, the more-active classes (Class 5: adjusted hazard ratio [AHR]=0.38, 95% CI=0.16, 0.88; Class 3: AHR=0.47, 95% CI=0.31, 0.71; Class 2: AHR=0.52, 95% CI=0.41, 0.65) had a lower risk of mortality compared with the lowest Class 1. No deaths occurred in Class 4 (similar to a “weekend warrior” type pattern) and 6 (highest weekly average intensity).
Figure 1.
Weighted percent of latent class assignments of physical activity and corresponding adjust hazard ratios for all-cause mortality; NHANES 2003–2006 (N=4,510).
Notes: The HRs are plotted on the natural log scale. The numbers corresponding to the plotted weighted percents are in Appendix Table 1 and the HR corresponds to Model 3 in Appendix Table 3. This model controls for age (40–49, 50–59, 60–69, ≥70), gender, race/ethnicity (non-Hispanic white, non-Hispanic black, other), education (<high school, high school or GED, >high school), married (yes, no), cigarette smoking (never, former, current), current employment (yes, no), current employment * follow-up time, need special equipment to walk (yes, no), arthritis (yes, no), cancer (no, non-melanoma skin cancer, any other type of cancer), angina (yes, no), myocardial infarction (yes, no), stroke (yes, no), coronary heart disease (yes, no), congestive heart failure (yes, no), BMI (underweight, normal weight, overweight, obese class 1, obese class II/III), BMI categories * follow-up time, hypertension (no, prehypertension, yes), and diabetes (no, prediabetes, yes). The models on MVPA and MVPA bouts also controls for light activity and sedentary behavior. The latent class variable for average counts/minute did not control for other physical activity/sedentary behavior components.
Star indicates no death observed in this category.
The latent class patterns come from Evenson et al., 2015 (4).
HR, hazard ratio; MVPA, moderate to vigorous physical activity; NHANES, National Health and Nutrition Examination Survey
For all MVPA/MVPA_lifestyle class assignments (using minutes or bouts), adjustment for accelerometer wear time (Model 1A), sedentary behavior and light activity (Model 2), and potential mediators (Model 3) did not meaningfully change interpretations compared to Model 1. For percentage of the day in MVPA, the more-active classes had a lower risk of mortality compared with the class with the lowest average percentage of the day in MVPA (Class 4: AHR=0.33, 95% CI=0.10, 1.03; Class 2: AHR=0.90, 95% CI=0.63, 1.28). No deaths occurred in Class 3 (weekend warrior) and 5 (highest weekly MVPA). When further limiting this exposure to percentage of the day in MVPA bouts, Class 2, 4, and 5 had a reduced risk of mortality. For percentage of the day in either MVPA_lifestyle or MVPA_lifestyle bouts, the more-active classes had a lower risk of mortality compared with the class with the lowest average percentage of the day in MVPA_lifestyle or MVPA_lifestyle bouts.
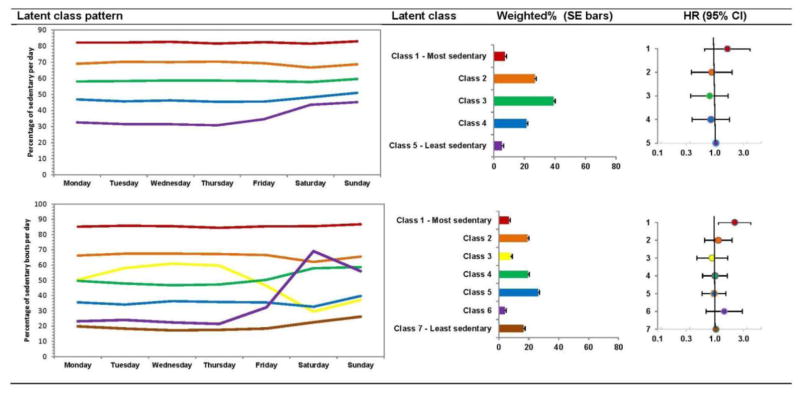
The models for sedentary behavior are presented in Appendix Table 3, with Model 3 plotted in Figure 2. For percentage of the day in sedentary behavior/bouts, adjustment for accelerometer wear time (Model 1A) did not meaningfully change results from Model 1. However, adjustment for light activity and MVPA attenuated the results (Model 2), with not much change with further adjustment for potential mediators (Model 3). For percentage of the day in sedentary behavior, the most sedentary Class 1 was at a higher risk for mortality as compared to the least sedentary Class 5 (Model 1 and 1A), which was attenuated to be non-significant when adjusting for light activity, MVPA, and potential mediators (AHR=1.57, 95% CI=0.64, 3.85; Model 3). When focusing on percentage of the day in sedentary bouts, the most sedentary Class 1 was also at an increased risk for mortality as compared with the least sedentary Class 7 (Model 1 and 1A), which was attenuated when adjusting for light activity, MVPA, and potential mediators but remained significant (AHR=2.10, 95% CI=1.11, 3.97; Model 3).
Figure 2.
Weighted percent of latent class assignments of sedentary behavior and corresponding adjusted hazard ratios (model 3) for all-cause mortality; NHANES 2003–2006 (N=4,510).
Notes: The HR are plotted on the natural log scale. The numbers corresponding to the plotted weighted percents are in Appendix Table 1 and the HR corresponds to Model 3 in Appendix Table 3. This model controls for age (40–49, 50–59, 60–69, ≥70), gender, race/ethnicity (non-Hispanic white, non-Hispanic black, other), education (<high school, high school or GED, >high school), married (yes, no), cigarette smoking (never, former, current), current employment (yes, no), current employment * follow-up time, need special equipment to walk (yes, no), arthritis (yes, no), cancer (no, non-melanoma skin cancer, any other type of cancer), angina (yes, no), myocardial infarction (yes, no), stroke (yes, no), coronary heart disease (yes, no), congestive heart failure (yes, no), BMI (underweight, normal weight, overweight, obese class 1, obese class II/III), BMI categories * follow-up time, hypertension (no, prehypertension, yes), and diabetes (no, prediabetes, yes). The model also controls for light and moderate to vigorous physical activity.
The latent class pattern comes from Evenson et al., 2015 (4).
HR, hazard ratio; NHANES, National Health and Nutrition Examination Survey
DISCUSSION
In a national sample of U.S. adults aged ≥ 40 years, this study found that more-active classes derived from day-to-day accelerometry, indicated by higher levels of average physical activity intensity or percentage of time in MVPA or MVPA bouts, were associated with a lower risk of all-cause mortality compared with the least active class. No deaths occurred in the weekend warrior class (MVPA Class 3). Adults classified in the most sedentary bout class were at a higher risk of all-cause mortality compared with the least sedentary bout class.
Many studies document the inverse association between self-reported physical activity and all-cause mortality.18–24 A rapidly growing literature also supports the association between self-reported sedentary behavior and all-cause mortality.25–28 However, few studies have explored the association of physical activity or sedentary behavior with mortality without relying on self-report. Several of those studies representing unique cohorts are highlighted next.
In a study of 302 adults aged 70–82 years, Manini et al.29 reported a reduction in all-cause mortality for higher levels of total energy expenditure as assessed with doubly labeled water. A limitation of doubly labeled water is that assessment of the contribution of different levels of intensity is not possible. More recently, Ensurd and colleagues30 reported among men aged ≥ 71 years an approximately 1.5-times higher risk of all-cause mortality of the lowest quartile for moderate activity and light activity compared with the most active quartile. Other studies have reported a higher risk of mortality with lower accelerometer-derived physical activity among patients with peripheral arterial disease,31 chronic heart failure,32,33 and pacemaker recipients.34 Using the 2003–2006 NHANES cohort among adults aged ≥ 40 years, higher levels of average physical activity intensity, MVPA, and MVPA bouts as summarized in average duration/day were all associated with a lower risk of all-cause and cardiovascular mortality.6 Other NHANES studies have also reported on these associations, with some examples referenced.35–37
Building on this work, the latent class patterns derived from accelerometry provided additional information on how physical activity was accumulated throughout the week and the associated risk of mortality. For example, no deaths occurred among the group assigned to the weekend warrior pattern (higher amounts of MVPA or average physical activity intensity on the weekends and lower on the weekdays). This supports a prior study in which men classified as weekend warriors from self-reported questionnaires had a lower risk of all-cause mortality when compared with sedentary men, particularly among those without major risk factors.38 Consistently, the highest risk for mortality was found among the group with the lowest levels of MVPA Monday through Sunday. Older age, female sex, history of chronic disease, and higher BMI were consistently associated with lower odds, and having better self-rated health and being employed were consistently associated with higher odds of being assigned into a more active compared with a less active class.5
Previously, using the 2003–2006 NHANES cohort among adults aged ≥ 40 years, sedentary behavior and bouts as summarized in average duration/day were not generally associated with a lower risk of all-cause and cardiovascular mortality.6 This was not in support of a prior study previously mentioned of older men.30 However, in the current study, the class with the highest percentage of time spent in sedentary bouts each day did confer a higher risk for mortality, even after adjustment for light activity and MVPA. The most sedentary class comprised 7.3% of the population under study and averaged 82.0% of their day in sedentary behavior over the week. This class was more likely to be older, have a higher education, need special equipment to walk, and have at least one of several health conditions (e.g., morbid obesity, diabetes, cardiovascular disease, cancer, emphysema).5 Although deaths in the first 2 years of follow-up were excluded, reverse causality may still occur.
Limitations
The strengths of the study include the national sample, the measurement of physical activity/sedentary behavior, and the uniqueness of the research question being addressed. The process to derive latent class assignments from accelerometry are available if others wish to access them.39 Despite the strengths of this study, several limitations should be highlighted. First, the accelerometer was worn for 1 week; it is not known if this time period is too short to reflect long-term patterns. Second, the accelerometer used in this study may undercount some activities (e.g., bicycling) and miss other activities (e.g., swimming) because of the requirement to remove it during water-based activities. Third, the LCA models used to derive the class assignments assumed data were missing at random. This assumption may not always be true, particularly when the accelerometer is removed for water activities. Fourth, in some cases, the statistical power was limited owing to the small class size; longer follow-up time will allow further clarification of these findings. Finally, an assessment of selection bias indicated some differences between those who were included and those not included (i.e., did not wear the accelerometer or returned a faulty accelerometer) in the analysis, as described in the Appendix.
CONCLUSIONS
This study applied LCA to accelerometry and explored day-to-day patterns with mortality. With generalizability among U.S. adults aged ≥ 40 years, the LCA classified adults into groups based on physical activity and sedentary behavior that predicted significantly higher or lower risk for all-cause mortality, even with adjustment for many potential confounders and mediators. The application of the patterns to the accelerometry data provided additional insight beyond the traditional approach of focusing on total duration in various intensity levels over the week. Adults comprising the most sedentary bouts and least physically active classes identified through LCA were at higher risk of all-cause mortality.
Supplementary Material
Acknowledgments
This work was supported by NIH, National Heart, Lung, and Blood Institute #R21 HL115385. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
KRE developed the aims of the study and drafted the paper, and all other authors provided critical feedback on earlier drafts of the paper. AHH and FW provided input on the analysis of the study, and FW wrote all analytic programs. All authors read and approved the final manuscript.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wijndaele K, Westgate K, Stephens SK, et al. Utilization and harmonization of adult accelerometry data: Review and expert consensus. Med Sci Sports Exerc. 2015;47(10):2129–2139. doi: 10.1249/MSS.0000000000000661. http://dx.doi.org/10.1249/MSS.0000000000000661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metzger JS, Catellier DJ, Evenson KR, Treuth MS, Rosamond WD, Siega-Riz AM. Patterns of objectively measured physical activity in the United States. Med Sci Sports Exerc. 2008;40(4):630–638. doi: 10.1249/MSS.0b013e3181620ebc. http://dx.doi.org/10.1249/MSS.0b013e3181620ebc. [DOI] [PubMed] [Google Scholar]
- 3.Metzger J, Catellier D, Evenson K, Treuth M, Rosamond W, Siega-Riz A. Associations between patterns of objectively measured physical activity and risk factors for the metabolic syndrome. Am J Health Promot. 2010;24(3):161–169. doi: 10.4278/ajhp.08051151. http://dx.doi.org/10.4278/ajhp.08051151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evenson KR, Wen F, Metzger JS, Herring AH. Physical activity and sedentary behavior patterns using accelerometry from a national sample of United States adults. Int J Behav Nutr Phys Act. 2015;12:20. doi: 10.1186/s12966-015-0183-7. http://dx.doi.org/10.1186/s12966-015-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones S, Wen F, Herring A, Evenson K. Correlates of U.S. adult physical activity and sedentary behavior patterns. J Sci Med Sport. doi: 10.1016/j.jsams.2016.03.009. In press. Online March 26, 2016. http://dx.doi.org/10.1016/j.jsams.2016.03.009. [DOI] [PMC free article] [PubMed]
- 6.Evenson K, Wen F, Herring A. Association of accelerometry assessed and self-reported physical activity and sedentary behavior with all-cause and cardiovascular mortality among United States’ adults. Am J Epidemiol. doi: 10.1093/aje/kww070. In press. Online October 19, 2016. http://dx.doi.org/10.1093/aje/kww070. [DOI] [PMC free article] [PubMed]
- 7. [Accessed February 1, 2016];IRB Approvals for NHANES. www.cdc.gov/nchs/nhanes/irba98.htm.
- 8.John D, Freedson P. ActiGraph and Actical physical activity monitors: a peek under the hood. Med Sci Sports Exerc. 2012;44(suppl 1):S86–89. doi: 10.1249/MSS.0b013e3182399f5e. http://dx.doi.org/10.1249/MSS.0b013e3182399f5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–364. doi: 10.1249/MSS.0b013e3181ed61a3. http://dx.doi.org/10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Troiano R, Berrigan D, Dodd K, Masse L, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. http://dx.doi.org/10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 11.Matthews C. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(11 suppl):S512–S522. doi: 10.1249/01.mss.0000185659.11982.3d. http://dx.doi.org/10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 12.Welk GJ, McClain JJ, Eisenmann JC, Wickel EE. Field validation of the MTI Actigraph and BodyMedia armband monitor using the IDEEA monitor. Obesity. 2007;15(4):918–928. doi: 10.1038/oby.2007.624. http://dx.doi.org/10.1038/oby.2007.624. [DOI] [PubMed] [Google Scholar]
- 13.Crouter SE, DellaValle DM, Haas JD, Frongillo EA, Bassett DR. Validity of ActiGraph 2-regression model, Matthews cut-points, and NHANES cut-points for assessing free-living physical activity. J Phys Act Health. 2013;10(4):504–514. doi: 10.1123/jpah.10.4.504. http://dx.doi.org/10.1123/jpah.10.4.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matthews CE, Keadle SK, Sampson J, et al. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013;45(8):1629–1638. doi: 10.1249/MSS.0b013e3182897690. http://dx.doi.org/10.1249/MSS.0b013e3182897690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matthews C, Chen K, Freedson P, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. http://dx.doi.org/10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Little R. Weighting and prediction in sample surveys. [Accessed February 1, 2016];University of Michigan Department of Biostatistics Working Paper Series. 2009 :1–30. Paper 81. http://biostats.bepress.com/umichbiostat/paper81/
- 17.Collett D. Modeling Survival Data in Medical Research. London: Chapman and Hall; 1994. http://dx.doi.org/10.1007/978-1-4899-3115-3. [Google Scholar]
- 18.Powell K, Thompson P, Caspersen C, Kendrick J. Physical activity and the incidence of coronary heart disease. Annu Rev Public Health. 1987;9:253–287. doi: 10.1146/annurev.pu.08.050187.001345. http://dx.doi.org/10.1146/annurev.pu.08.050187.001345. [DOI] [PubMed] [Google Scholar]
- 19.Nocon M, Hiemann T, Muller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15(3):239–246. doi: 10.1097/HJR.0b013e3282f55e09. http://dx.doi.org/10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- 20.Boone-Heinonen J, Evenson KR, Taber DR, Gordon-Larsen P. Walking for prevention of cardiovascular disease in men and women: a systematic review of observational studies. Obes Rev. 2009;10(2):204–217. doi: 10.1111/j.1467-789X.2008.00533.x. http://dx.doi.org/10.1111/j.1467-789X.2008.00533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lollgen H, Bockenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med. 2009;30(3):213–224. doi: 10.1055/s-0028-1128150. http://dx.doi.org/10.1055/s-0028-1128150. [DOI] [PubMed] [Google Scholar]
- 22.Lee I. Current issues in examining dose-response relationships between physical activity and health outcomes. In: Lee I, editor. Epidemiologic Methods in Physical Activity Studies. New York City, NY: Oxford University Press; 2009. pp. 56–76. [Google Scholar]
- 23.Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol. 2011;40(5):1382–1400. doi: 10.1093/ije/dyr112. http://dx.doi.org/10.1093/ije/dyr112. [DOI] [PubMed] [Google Scholar]
- 24.Sabia S, Dugravot A, Kivimaki M, Brunner E, Shipley MJ, Singh-Manoux A. Effect of intensity and type of physical activity on mortality: results from the Whitehall II cohort study. Am J Public Health. 2012;102(4):698–704. doi: 10.2105/AJPH.2011.300257. http://dx.doi.org/10.2105/AJPH.2011.300257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41(5):1338–1353. doi: 10.1093/ije/dys078. http://dx.doi.org/10.1093/ije/dys078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matthews CE, Cohen SS, Fowke JH, et al. Physical activity, sedentary behavior, and cause-specific mortality in black and white adults in the Southern Community Cohort Study. Am J Epidemiol. 2014;180(4):394–405. doi: 10.1093/aje/kwu142. http://dx.doi.org/10.1093/aje/kwu142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–132. doi: 10.7326/M14-1651. http://dx.doi.org/10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 28.Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. http://dx.doi.org/10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 29.Manini T, Everhart J, Patel K, et al. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296(2):171–179. doi: 10.1001/jama.296.2.171. http://dx.doi.org/10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- 30.Ensrud KE, Blackwell TL, Cauley JA, et al. Objective measures of activity level and mortality in older men. J Am Geriatr Soc. 2014;62(11):2079–2087. doi: 10.1111/jgs.13101. http://dx.doi.org/10.1111/jgs.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garg PK, Tian L, Criqui MH, et al. Physical activity during daily life and mortality in patients with peripheral arterial disease. Circulation. 2006;114(3):242–248. doi: 10.1161/CIRCULATIONAHA.105.605246. http://dx.doi.org/10.1161/CIRCULATIONAHA.105.605246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Conraads VM, Spruit MA, Braunschweig F, et al. Physical activity measured with implanted devices predicts patient outcome in chronic heart failure. Circ Heart Fail. 2014;7:279–287. doi: 10.1161/CIRCHEARTFAILURE.113.000883. http://dx.doi.org/10.1161/CIRCHEARTFAILURE.113.000883. [DOI] [PubMed] [Google Scholar]
- 33.Shoemaker M, Curtis A, Vangsnes E, Dickinson M, Paul R. Analysis of daily activity data from implanted cardiac defibrillators: The minimum clinically important difference and relationship to mortality / life expectancy. World J Cardiovasc Dis. 2012;2:129–135. http://dx.doi.org/10.4236/wjcd.2012.23021. [Google Scholar]
- 34.Tyagi S, Curley M, Berger M, et al. Pacemaker quantified physical activity predicts all-cause mortality. J Am Coll Cardiol. 2015;66(6):754–755. doi: 10.1016/j.jacc.2015.06.005. http://dx.doi.org/10.1016/j.jacc.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Fishman EI, Steeves JA, Zipunnikov V, et al. Association between objectively measured physical activity and mortality in NHANES. Med Sci Sports Exerc. 2016;48(7):1303–1311. doi: 10.1249/MSS.0000000000000885. http://dx.doi.org/10.1249/MSS.0000000000000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7(6):e37696. doi: 10.1371/journal.pone.0037696. http://dx.doi.org/10.1371/journal.pone.0037696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmid D, Ricci C, Leitzmann MF. Associations of objectively assessed physical activity and sedentary time with all-cause mortality in U.S. adults: the NHANES study. PLoS One. 2015;10(3):e0119591. doi: 10.1371/journal.pone.0119591. http://dx.doi.org/10.1371/journal.pone.0119591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee I-M, Sesso H, Oguma Y, Paffenbarger R., Jr The “weekend warrior” and risk of mortality. Am J Epidemiol. 2004;160(7):636–641. doi: 10.1093/aje/kwh274. http://dx.doi.org/10.1093/aje/kwh274. [DOI] [PubMed] [Google Scholar]
- 39.Evenson K, Wen F, Howard A, Herring A. Applying derived latent class assignments from NHANES 2003–2006 accelerometry to external populations. Data Brief. 2016 doi: 10.1016/j.dib.2016.11.007. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.