Abstract
Objective
Research has demonstrated high comorbidity between asthma and panic disorder (PD). Less is known about the relationship between asthma and the Latino cultural idiom of distress of ataques de nervios, as well as the role that psychosocial stressors play. The current study tested the hypotheses that Latino asthma patients who experience PD, ataques de nervios, and/or asthma-related death of a loved one endorse greater psychological triggers of asthma, greater perceived impact of asthma triggers, and greater difficulty controlling such triggers than do those without these conditions.
Methods
Data originated from an interview conducted prior to a randomized controlled trial in which 292 Latino adults with self-reported asthma were recruited from outpatient clinics in the Bronx, NY. The PRIME-MD Patient Health Questionnaire (PHQ) was used to screen for PD symptoms, while the Structured Clinical Interview for DSM-IV (SCID-I) was used to confirm diagnosis of PD. Lifetime history of ataques de nervios and asthma-related death of a loved one were based upon self-report. Asthma triggers were examined using the Asthma Trigger Inventory (ATI).
Results
PD, ataques de nervios, and asthma-related death of a loved one each predicted a higher frequency of psychological asthma triggers, controlling for gender and comorbid medical conditions. Participants with PD also reported greater impact of asthma triggers than those without PD, while no significant differences in perceived control were observed.
Conclusion
Providers should screen for PD, ataques de nervios, and asthma-related death of a loved one in Latino asthma patients, given their observed association with emotionally triggered asthma.
Keywords: Asthma, Ataques de Nervios, Death of a Loved One, Latinos, Panic Disorder, Psychological Triggers
Introduction
Managing asthma symptoms requires comprehensive asthma treatment that attends to the interplay between physical and psychological components. Research has found that patients with asthma are more likely to exhibit psychological symptoms than those without asthma [1–3]. In particular, the estimated lifetime prevalence rate of anxiety disorders among adults with asthma is 34% [4]. Further, patients with asthma and comorbid psychological disorders have more impaired emotional and physical functioning than those with one of these conditions alone [1]. Comorbid psychiatric disorders predict poor asthma control and asthma-related quality of life [3, 5]. This comorbidity contributes to greater health care utilization [6], regardless of asthma severity [7].
Psychological asthma triggers are one area in which physiological and mental health factors may be strongly interrelated. Psychological triggers are typically more difficult to avoid than other subcategories of commonly perceived asthma triggers (e.g., animal allergens, pollen, general allergens, physical activity, air pollutants/irritants, and infections) and contribute to compromised asthma management [8]. Empirical evidence suggests that heightened emotional arousal due to increased levels of anxiety, particularly in the context of distressing situations, may alter the subjective interpretation of respiratory impairment and contribute to a learned response of dyspnea in asthma patients [9]. Thus, the current study examined the frequency of psychological asthma triggers, perceived impact of triggers, and perceived ability to control triggers in Latino asthma patients who experience PD, ataques de nervios, and/or asthma-related death of a loved one compared to those without these conditions.
Prevalence Rates of Asthma
Several studies have shown that asthma is more common in Latinos than in other ethnic groups [10, 11]. Among Latinos, Puerto Ricans have the highest prevalence of asthma [12, 13]. In New York City, the lifetime prevalence rate of asthma among adults is 29% higher than the national rate [14]. Further, asthma prevalence, hospitalization, and mortality rates are higher in the Bronx, where the current study was conducted, than in any other NYC borough [14]. Physiologically based genetic differences and environmental factors may explain these higher rates among Puerto Ricans living in the Bronx, NY [15, 16]. The combination of such cultural and geographic patterns in asthma prevalence highlights the importance of investigating this condition among the Bronx Latino population.
Psychological Triggers of Asthma
Ritz, Steptoe [8] found that 28% of asthma patients reported psychological asthma triggers (e.g., being angry, feeling alone, stress at home, feeling tense, depressed mood, arguments with people, being excited, intense worries, feeling unhappy, and feeling weak) as their most frequent triggers. Asthma triggers related to psychosocial stress exert greater negative influence on health-related outcomes such as asthma control and quality of life than do pollen, animal allergens, and other triggers of a pathophysiological nature [8]. Patients with near-fatal asthma attacks are especially likely to report psychological stress as an asthma trigger [17]. Identifying psychological conditions and other negative life events that are associated with psychological triggers of asthma in Latino adults may therefore improve strategies designed to help such patients manage their asthma symptoms.
Asthma and Panic Disorder
Research has repeatedly demonstrated high comorbidity rates of asthma and PD in the general population [18]. In the Bronx, rates of PD are particularly elevated among asthma patients of Puerto Rican descent (21%) [19]. PD significantly contributes to asthma morbidity, including increased use of health care resources and greater use of quick-relief medications for asthma [20]. Illness-specific panic fear, which is anxiety elicited during asthma attacks, has been shown to mediate the relationship between PD and poorer health-related quality of life [21]. When experiencing anxiety and other intense emotions, asthma patients with PD may be more prone to subjectively interpret the accompanying bodily sensations as threatening, potentially even misconstruing them as asthma symptoms. Additionally, stressful episodes may trigger bronchoconstriction via hyperventilation, airway inflammation via production of cytokines, and asthma exacerbations via parasympathetic rebound [22]. Thus, PD warrants examination as a potential predictor of perceived vulnerability to psychological triggers of asthma.
Ataques de Nervios
Another factor that may be associated with psychological triggers of asthma in Latino patients is ataques de nervios, a cultural idiom of distress among Latinos that is characterized by intense emotional reactions of anxiety, anger, or grief [23]. Ataques include physical sensations such as trembling or heat in the chest rising into the head, behavioral responses such as screaming or crying, and cognitive-affective symptoms such as a general sense of losing complete control [23]. Displays of aggression and instances of dissociation may also occur, as do fainting episodes and suicidal gestures on occasion [23]. Among a clinical sample of Dominican and Puerto Rican patients seeking treatment for anxiety and/or depression at a mental health clinic in New York City, nearly 3/4 (72%) of Latinos reported a lifetime history of ataques [24]. The same study found that 36% of such ataques met criteria for panic attacks and 17% for PD [24]. While such data highlight an overlap between ataques de nervios and PD, as well as the somewhat problematic potential for a given experience to receive different diagnostic and cultural labels, the two conditions are considered to be inherently distinct phenomena. For instance, patients who experience ataques commonly endorse panic symptoms such as shortness of breath, palpitations, and sweating, but ataques differentiate themselves from panic attacks in that they are typically experienced for longer durations of time and followed by more of a sense of relief than anticipatory fear [24]. Ataques are also frequently triggered by stressful life events pertaining to the family, such as the death of a close relative, conflicts with a spouse or child, or an accident involving a family member [23].
Puerto Ricans with a lifetime history of ataques are twice as likely to experience asthma and three times as likely in the Bronx [25], particularly in the context of greater exposure to violence and stress among inner-city populations [26]. The work of Hinton and colleagues [27, 28] may offer additional insight into these findings. Noting a strong correlation between the frequency and severity of ataques de nervios in Puerto Rican psychiatric patients and the fear of arousal symptoms known as anxiety sensitivity, the authors theorized that those individuals who experience ataques may be more prone to catastrophically misinterpret their cognitive-affective states and bodily sensations during times of stress [27]. Hyperarousal may then lead to increased psychological and/or somatic symptoms such as difficulty breathing, thereby perpetuating a cycle of further arousal and fear [25]. Subsequent work supports the notion that ataques are associated with fear of negative affect and arousal symptoms, the degree of which is largely determined by the individual’s perceived vulnerability to future episodes [28]. Hence, ataques de nervios may also be implicated in an increased susceptibility to psychological triggers of asthma in Latino adults.
Death of a Loved One due to Asthma
The association between asthma-specific negative life events, such as the death of a loved one due to asthma, and the perception of emotional triggers has received little investigation thus far. Potoczek [29] has noted that the experience of witnessing the suffering or death of a loved one due to a chronic medical condition correlated with the severity of PD symptoms in asthma patients, but did not explore the association with asthma-related deaths per se. Recent research suggests that such negative life events may significantly account for functional impairment in patients with asthma and comorbid psychiatric conditions [30]. In their review of the observed association between negative life events and increased risk of asthma exacerbations, Yii and Koh [31] maintain that psychosocial stressors engender cognitive distortions in asthma patients, including a heightened perception of dyspnea. They explain that such overestimation of perceived threat thereby contributes to increased levels of anxiety during acute attacks, as well as excessive use of bronchodilator medications and greater dependence on medical resources.
Such findings seem especially relevant for the inner-city Latino population, given their aforementioned elevated asthma mortality rates. Data also suggest that Puerto Ricans who live in large U.S. cities such as the Bronx, NY are more likely to suffer emotional distress in response to traumatic situations than those of other ethnic groups [32]. Stressful life events within the family context, such as death of a loved one, are most commonly reported as triggers of ataques de nervios [24]. One study among the Latino population found that patients who suffered from both ataques de nervios and PD reported the greatest asphyxia and fear of dying during their attacks [33]. Hence, illness-specific negative life events such as asthma-related death of a loved one may serve as yet another prognostic indicator of increased vulnerability to psychological triggers of asthma in Latinos.
Specific Aims and Hypotheses
The aim of the current study was to examine the relative importance of psychological asthma triggers in Latino adults who experience PD, ataques de nervios, and death of a loved one due to asthma compared to those who do not. It was hypothesized that patients who experience PD, self-reported ataques de nervios, and self-reported death of a loved one due to asthma would endorse a higher frequency of psychological asthma triggers than those who do not. It was further hypothesized that participants with such conditions would report greater perceived impact of asthma triggers on their daily lives, as well as greater perceived difficulty controlling and/or avoiding their asthma triggers. Covariates were selected based on past studies showing differences in asthma prevalence and morbidity due to age, gender, ethnicity [34], and language [35]. Further, PD is more prevalent in women [36], Puerto Ricans [19], and patients with comorbid medical conditions [37], while ataques are more prevalent in women [38].
Methods
Participants
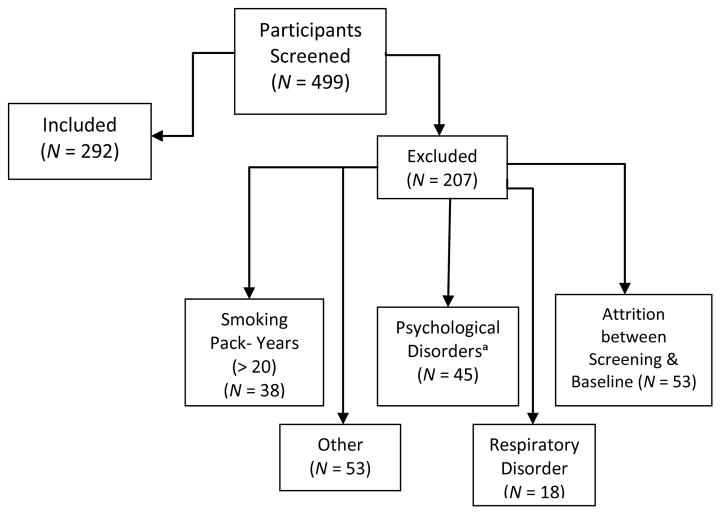
Participants were self-reported asthma patients assessed for eligibility for a larger intervention study of Latinos with asthma and PD[39]. The current study included 292 adults recruited from asthma clinics in the Bronx, NY, 79.5% (n = 235) of whom were female. Their ages ranged from 18 to 86, with a mean age of 43.8. All participants self-identified as Latino, and 25.7% (n = 75) were interviewed in Spanish. Individuals were excluded if their smoking history exceeded 20 pack-years, since they are at a substantially greater risk of having chronic obstructive pulmonary disease (COPD). They were also excluded if they had a respiratory disorder other than asthma, active psychosis, substance dependence or abuse, or bipolar disorder. A total of 1,453 individuals were approached for screening, 954 of whom were not screened due to refusal (n = 452), lack of self-reported asthma (n = 411), lack of self-reported anxiety and/or panic (n = 54), or other reasons (n = 37). The complete breakdown of inclusion and exclusion criteria of screened participants can be seen in Figure 1.
Figure 1.
Inclusion and Exclusion of Participants.
aNote: Psychological disorders that were used as exclusion criteria included active psychosis, bipolar disorder, and substance abuse or dependence.
Procedure
Participants were self-reported asthma patients who completed eligibility screenings and/or baseline assessments for an asthma and PD treatment study prior to randomization. Participants were recruited from asthma, allergy, and chest clinics; primary care clinics; and emergency rooms of multiple inner-city hospitals in the Bronx, NY. Additionally, flyers were posted in the community, advertisements were placed in local newspapers, and mailings were sent from health care providers in order to recruit participants for the study; follow-up phone calls were made to reach out to potential participants.
Eligibility screening questionnaires were administered to patients, either in person or over the telephone. Informed consent was obtained prior to inclusion in the study; consent forms were translated into Spanish using the procedure outlined below. These brief interviews were conducted by clinical psychology graduate students who were trained to differentiate PD from asthma. Participants who passed the eligibility screening process were invited to a baseline session, during which diagnostic interviews were conducted to confirm PD diagnoses. Other self-report measures were also administered at this time. The baseline testing session lasted between 2 and 2 ½ hours on average. Those participants who completed the baseline session were compensated $25 and provided transportation fare. The study protocol was approved by the Albert Einstein College of Medicine Institutional Review Board.
Measures
Translation and adaptation of instruments
For all of the following measures, both English and Spanish versions were utilized. Measures and forms were translated when Spanish versions were not already available, using a conceptual model to guide the process of ensuring cross-cultural equivalence in semantic, content, and technical domains [40–45]. The translations were completed by certified professional translators in the Institute for Clinical and Translational Research at Einstein and Montefiore. The resulting Spanish versions were then back-translated to English in order to ensure that all of the items retained their original meaning, repeating steps if necessary.
Eligibility Screening
Participants were administered a battery of questionnaires that included a demographics questionnaire examining age, gender, ethnicity, psychological conditions, cigarette use, current medical conditions, death of a loved one due to asthma, and ataques de nervios.
PRIME-MD Patient Health Questionnaire: Panic Screening Questions
The PRIME-MD PHQ panic screening questions were used to identify participants exhibiting panic symptoms. Created to facilitate diagnosis of the most common mental disorders seen in primary health care settings [46], the PHQ assesses threshold disorders corresponding to specific DSM-IV diagnoses. The measure consists of 15 yes/no questions regarding the symptoms and overall experience of having a panic attack in the last four weeks. The Spanish version of the PHQ [47], which was originally developed in Spain, was adapted for the present study of Latino (primarily Puerto Rican) participants. The English version of the PHQ has a sensitivity of 81% and a specificity of 99% for diagnosis of PD [46], while the corresponding original Spanish version has a sensitivity of 83% and a specificity of 98% [47]. Both versions have good construct validity, as reflected by impaired functioning, disability days, and use of medical resources [46, 47].
Structured Clinical Interview for the DSM-IV
English and Spanish versions of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) [48–50] were used to confirm diagnosis of PD in those participants who screened positive for PD based on the PHQ. The PD module of the SCID-I assesses PD symptoms during the past month. The SCID-I is a semi-structured interview that is used to evaluate the diagnostic criteria of most of the psychological disorders outlined in the DSM-IV. These psychiatric interviews were conducted by advanced clinical psychology doctoral students and post-doctoral fellows. Licensed clinical psychologists provided supervision, watching videos of all interviews and confirming diagnoses of PD. All interviewers received extensive training on differential diagnosis of PD versus asthma [51]. The SCID-I has been shown to have good inter-rater reliability (K = 0.67) [52].
Panic Disorder Severity Scale
The Panic Disorder Severity Scale (PDSS) [53] is a clinician-rated instrument that assesses the overall severity of PD during the past month (e.g., panic frequency, distress during panic, panic-focused anticipatory anxiety, etc.). The PDSS was used in conjunction with the SCID-I to evaluate the severity of PD as part of the inclusion criteria for the larger study; patients who scored at least an 8 on the PDSS were included in the study.
Self-reported lifetime history of ataques de nervios was based upon responses to the following single-item during screening: “Have you ever had an episode or nervous attack (ataques de nervios) where you felt totally out of control?” This question follows the methodology of the National Latino and Asian American Study (NLAAS) and has repeatedly demonstrated good validity in identifying those with various manifestations of the condition [54].
Self-reported death of a loved one due to asthma was assessed with the following three questions: a) “Have you ever experienced the death of a loved one due to asthma?” b) “How was this person related to you?” and c) “How many years ago did this person die from asthma?”
Self-reported presence of current comorbid medical conditions was assessed based upon the medical history that participants provided during screening.
Asthma Trigger Inventory
The Asthma Trigger Inventory (ATI) is a structured, self-report instrument used to assess commonly perceived asthma triggers [8]. The degree to which 32 different agents trigger a respondent’s asthma is rated on a 5-point scale from 0 (“Never”) to 4 (“Always”). The psychological trigger subscale items include being angry, feeling alone, stress at home, feeling tense, depressed mood, arguments with people, being excited, intense worries, feeling unhappy, and feeling weak. Scores on this subscale were obtained by averaging the ratings across all 10 items. The psychological trigger subscale has shown high internal consistency (Cronbach’s alpha = 0.94), good test-retest reliability (0.73), and construct validity [8].
In order to further clarify trigger patterns, participants were asked to list the top 6 agents that trigger their asthma. Using a 5-point scale ranging from 0 (“Not at all”) to 4 (“Completely”), participants indicated the degree to which each of these 6 agents affected their everyday life and the degree to which they could avoid or control that agent without the use of bronchodilators. Scores for trigger impact and trigger control were obtained by averaging the ratings for these triggers. Trigger impact and trigger control scales exhibited a low to modest intercorrelation (r = 0.37) and acceptable test-retest reliabilities (r = 0.76 and 0.39, respectively) [8].
Statistical Analyses
Independent samples t-tests and Chi-square analyses were used to examine between-group differences (i.e., in participants who experience PD, ataques de nervios, and death of a loved one compared to those who do not) in demographics and psychological asthma triggers. Descriptive statistics characterized the sample, and Pearson correlation analyses tested associations between experimental variables. Chi-square analyses were performed in order to determine the relationships between the predictor variables (i.e., PD, death of a loved one due to asthma, and ataques de nervios). Separate hierarchical linear regression analyses were performed to determine the associations between each predictor variable and psychological asthma triggers, controlling for gender and comorbid medical condition. Hierarchical linear regression analyses were also conducted in order to examine associations between each predictor variable and both trigger impact and trigger control ratings on the ATI, controlling for gender and comorbid medical condition. For all statistical tests, significance was set at p ≤ 0.05. Final dfs for regression analyses differ as a result of missing data.
Results
Descriptive Characteristics
Demographic characteristics of the study sample can be found in Table 1.
Table 1.
Characteristics of the Sample
| Total (N = 292) | |
|---|---|
| Age M (SD) | 43.78 (14.78) |
| Gender n (%) | |
| Male | 57 (19.5) |
| Female | 235 (80.5) |
| Language n (%) | |
| English | 217 (74.3) |
| Spanish | 75 (25.7) |
| Primary Ethnic Origin n (%) | |
| Puerto Rican | 209 (72.1) |
| Dominican | 37 (12.8) |
| Mexican | 8 (2.7) |
| Other (Latin, Central American, and Caribbean) | 38 (12.4) |
| Panic Disorder n (%) | |
| Yes | 73 (25.0) |
| No | 219 (75.0) |
| Recruitment Site n (%) | |
| Mailings | 189 (65.4) |
| Outpatient Hospital Setting | 31 (10.8) |
| Emergency Department | 24 (8.2) |
| Other (Fliers, Ads, etc.) | 45 (15.6) |
| Death of a Loved One due to Asthma n (%) | |
| Yes | 84 (29.7) |
| No | 199 (70.3) |
| History of Ataques de Nervios (Lifetime) n (%) | |
| Yes | 120 (45.1) |
| No | 146 (54.9) |
| Other Medical Condition n (%) | |
| Yes | 158 (54.1) |
| No | 134 (45.9) |
Results indicated that women were more likely to be diagnosed with PD, χ2 (1, N = 289) = 10.22, p ≤ 0.001, as well as to endorse a lifetime history of ataques de nervios, χ2 (1, N = 264) = 11.45, p ≤ 0.001. Participants with comorbid medical conditions were more likely to report psychological asthma triggers, t(272) = 2.13, p = 0.03. Analyses including age, language, and primary ethnic origin were ns. Hence, subsequent regression analyses controlled for gender and the presence of comorbid medical conditions.
Self-reported asthma-related deaths occurred most frequently among aunts or uncles (18.3%) and grandparents (18.3%). On average, asthma-related deaths occurred 14.3 +/− 13.3 years prior to self-report, with data positively skewed such that 84.1% of reported deaths occurred within the past 20 years.
Interrelations between Predictor Variables
Chi-square results indicated that PD was significantly associated with ataques de nervios, χ2 (1, N = 257) = 19.18, p ≤ 0.001. Death of a loved one due to asthma was also significantly associated with ataques de nervios, χ2 (1, N = 251) = 7.60, p = 0.01. PD was not significantly associated with death of a loved one due to asthma, χ2 (1, N = 274) = 2.05, p = 0.15.
Psychological Asthma Triggers
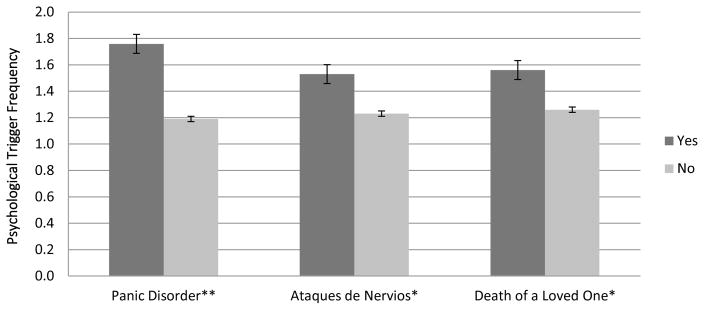
Results from independent samples t-tests revealed that psychological asthma triggers were significantly higher in participants with PD, t(272) = −4.25, p ≤ 0.001, ataques de nervios, t(253) = −2.38, p = 0.02, and death of a loved one due to asthma, t(265) = −2.28, p = 0.02, when compared to those participants who did not experience these conditions (Figure 2).
Figure 2.
Frequency of Psychological Asthma Triggers (ATI)
aNote. *p ≤ .05 level; ** p ≤ .001 level; the standard error of the mean is depicted using error bars.
Results from separate multivariate analyses indicated that PD was significantly associated with psychological asthma triggers, as was death of a loved one due to asthma, and ataques de nervios, after controlling for gender and comorbid medical conditions (Table 2).
Table 2.
Predictors of Psychological Asthma Triggers
| Predictor | Change in R2 | B | T | p |
|---|---|---|---|---|
| Panic Disorder | ||||
| Step 1 | 0.02 | |||
| Gender | 0.06 | 0.96 | 0.34 | |
| Comorbid Medical Condition | 0.12 | 2.05 | 0.04* | |
| Step 2 | 0.06 | |||
| PD | 0.24 | 4.09 | ≤0.001** | |
|
| ||||
| Death of a Loved One | ||||
| Step 1 | 0.02 | |||
| Gender | 0.05 | 0.82 | 0.42 | |
| Comorbid Medical Condition | 0.13 | 2.04 | 0.04* | |
| Step 2 | 0.02 | |||
| Death of a Loved One | 0.13 | 2.18 | 0.03* | |
|
| ||||
| Ataques de Nervios | ||||
| Step 1 | 0.01 | |||
| Gender | 0.06 | 0.91 | 0.36 | |
| Comorbid Medical Condition | 0.10 | 1.55 | 0.12 | |
| Step 2 | 0.02 | |||
| Ataques de Nervios | 0.13 | 2.05 | 0.04* | |
Note.
p ≤ .05 level;
p ≤ .001 level
Trigger Impact and Trigger Control
Results indicated that participants with PD were more likely to report greater impact of asthma triggers, β = 0.20, t(261) = 3.32, p ≤ 0.001, than participants without PD (change in r2 = 4.1%). PD did not predict trigger control, β = −0.04, t(266) = −0.63, p = 0.53. Death of a loved one did not significantly predict either trigger impact, β = 0.08, t(258) = 1.33, p = 0.19, or trigger control, β = −0.10, t(259) = −1.60, p = 0.11. Ataques de nervios did not significantly predict either trigger impact, β = 0.12, t(247) = 1.81, p = 0.07, or trigger control, β = −0.05, t(248) = −0.75, p = 0.46.
Discussion
The current findings highlight the role that PD, ataques de nervios, and death of a loved one due to asthma may play in emotionally induced asthma among Latino patients. As expected, all three conditions significantly predicted the frequency with which patients reported various psychological triggers of their asthma. It should be noted, however, that current PD was assessed by examining symptoms within the last month, while lifetime death of a loved one and ataques de nervios were reported. Thus, smaller observed effect sizes for such factors may also reflect the more protracted time period during which these circumstances were experienced.
The current study suggests that negative life events such as the death of a loved one due to asthma may help explain the degree to which Latino patients with asthma subjectively interpret their illness as stress-induced. Patients who have experienced such losses may exhibit greater learned helplessness with regards to their physical condition, which has been noted to contribute to the comorbidity between asthma and psychiatric disorders [55]. The fact that PD predicted the perceived impact of asthma triggers on participants’ daily lives is also consistent with the literature, as emotional distress due to chronic disease symptoms appears most pronounced among individuals who exhibit the type of rumination and catastrophic thinking characteristic of PD [56]. On the other hand, participants who endorsed a lifetime history of ataques de nervios did not report greater impact of asthma triggers on their daily lives, which suggests the importance of the cultural context in which such symptoms are perceived. These findings are somewhat surprising in light of previous research that found children with a history of ataques de nervios were more likely to have asthma and other somatic complaints [25], but may reflect the fact that adults from the present sample viewed such experiences as less salient.
This study also sought to examine the degree to which PD, ataques de nervios, and death of a loved one due to asthma co-occur. Consistent with the findings of Lewis-Fernandez, Guarnaccia [24] and Salmán, Liebowitz [33], results suggest a significant overlap between ataques de nervios and PD. However, the notion that these two disorders are diagnostically distinct entities is supported by the fact that comorbid ataques de nervios and PD only occurred in 1/5 of the sample. Ataques de nervios and not PD was significantly associated with death of a loved one due to asthma. Such findings seem plausible in light of the fact that ataques de nervios is a more expansive phenomenological construct, with episodes of an anxious and/or depressive nature that are commonly provoked by an upsetting personal event [24]. The fact that ataques de nervios tends to encompass a broader range of experiences also helps explain the much higher prevalence rate of ataques de nervios (45.1%) than of PD (25.0%) in the study, a figure that is actually lower than the 72% rate previously reported for ataques de nervios among a comparable clinical sample [25].
Results may be confounded by the fact that the presence of ataques de nervios was established using a single self-report question, while the presence of PD was assessed using a clinician-administered SCID interview. Thus, it is difficult to determine whether the affective episodes that participants described indeed constituted both conditions without a more comprehensive examination of each event. By improving upon the methodology used to elicit reports of past episodes of ataques and panic, future studies in the field may better differentiate these two conditions and thereby clarify their unique relationships with self-perceived triggers of asthma in Latinos.
The present study had other notable limitations. First, asthma diagnosis was based upon self-report. Since pulmonary function tests were not conducted on all participants during data collection, such asthma diagnoses were not confirmed with more objective measures. Further, given the disproportionate number of women and Puerto Ricans in the current study, conclusions regarding culturally relevant risk factors of emotionally induced asthma in adult Latino patients may be less representative of other gender and ethnic groups. The study also did not assess related factors such as asthma severity, medication use, and other health behaviors. Lastly, the time frame of the factors tested was variable.
In the current study, considerable variability existed with regards to how long ago the self-reported death of a loved one due to asthma had occurred, as well as how close the deceased loved one was to the patient. Future studies should therefore explore whether such variables affect the degree to which Latino patients perceive their asthma to be triggered by psychological factors. Further, individuals who experience asthma-related death of a loved one may presumably have difficulty managing their asthma due to the anticipatory anxiety that such stressful life events instill. Future studies should also investigate whether death of a loved one due to asthma and similar asthma-specific negative life events are predictive of poorer asthma control, asthma morbidity, and health-related quality of life among Latino patients. Finally, longitudinal research is needed to determine whether cognitive-behavioral protocols for asthma and anxiety [39, 57] promote self-efficacy in the specific context of these psychosocial stressors, thereby improving asthma outcomes in Latino patients with ataques de nervios and comorbid psychological conditions such as PD.
Given that perceived psychological triggers have been associated with significantly worse outcomes in health perception and asthma control [8], increased recognition of the role that various mental health conditions and stressful illness-specific experiences play in the frequency of such triggers bears great clinical importance. Results from the current study suggest that providers who work with Latino asthma patients should screen for PD, ataques de nervios, and asthma-related death of a loved one, as they may contribute to emotionally induced asthma. Interventions should include psychoeducation regarding the nature of asthma, as well as cognitive-behavioral techniques that address the maladaptive thoughts related to their symptoms and the resulting emotional distress. Such interventions may decrease health care burden by reducing emergency room visits and other measures of asthma morbidity.
Highlights.
Examined PD, ataques de nervios, and death of a loved in Latino asthma patients
Examined emotional triggers in Latino asthma patients experiencing these conditions
All three conditions predicted a higher frequency of psychological asthma triggers
Asthma patients with PD reported greater impact of triggers on their daily lives
Clinical interventions should address psychosocial stressors in asthma patients
Acknowledgments
We would like to thank Thomas Ritz, Ph.D. for providing us with the Spanish translation of the Asthma Trigger Inventory (ATI).
Conflicts of Interest and Sources of Funding
Funded by National Institute of Mental Health: 1R34MH087679, PI: Jonathan M. Feldman, Ph.D. Measure translations were funded by the Institute for Clinical and Translational Research at Einstein and Montefiore (5UL-1TR001073-02).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lehrer P, Feldman J, Giardino N, Song HS, Schmaling K. Psychological aspects of asthma. Journal of Consulting and Clinical Psychology. 2002;70(3):691–711. doi: 10.1037//0022-006X.70.3.691. [DOI] [PubMed] [Google Scholar]
- 2.Feldman JM, Siddique MI, Morales E, Kaminski B, Lu SE, Lehrer PM. Psychiatric disorders and asthma outcomes among high-risk inner-city patients. Psychosomatic Medicine. 2005;67(6):989–996. doi: 10.1097/01.psy.0000188556.97979.13. [DOI] [PubMed] [Google Scholar]
- 3.Lavoie KL, Bacon SL, Barone S, Cartier A, Ditto B, Labrecque M. What is worse for asthma control and quality of life: Depressive disorders, anxiety disorders, or both? CHEST Journal. 2006;130(4):1039–1047. doi: 10.1378/chest.130.4.1039. [DOI] [PubMed] [Google Scholar]
- 4.Weiser EB. The prevalence of anxiety disorders among adults with asthma: A meta-analytic review. Journal of Clinical Psychology in Medical Settings. 2007;14(4):297–307. doi: 10.1007/s10880-007-9087-2. [DOI] [Google Scholar]
- 5.Lavoie KL, Cartier A, Labrecque M, Bacon SL, Lemière C, Malo JL, … Ditto B. Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respiratory Medicine. 2005;99(10):1249–1257. doi: 10.1016/j.rmed.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 6.ten Brinke A, Ouwerkerk ME, Zwinderman AH, Spinhoven P, Bel EH. Psychopathology in patients with severe asthma is associated with increased health care utilization. American Journal of Respiratory and Critical Care Medicine. 2001;163(5):1093–1096. doi: 10.1164/ajrccm.163.5.2004020. [DOI] [PubMed] [Google Scholar]
- 7.ten Brinke A, Ouwerkerk ME, Bel EH, Spinhoven P. Similar psychological characteristics in mild and severe asthma. Journal of Psychosomatic Research. 2001;50(1):7–10. doi: 10.1016/S0022-3999(00)00203-8. [DOI] [PubMed] [Google Scholar]
- 8.Ritz T, Steptoe A, Bobb C, Harris AH, Edwards M. The asthma trigger inventory: Validation of a questionnaire for perceived triggers of asthma. Psychosomatic Medicine. 2006;68(6):956–965. doi: 10.1097/01.psy.0000248898.59557.74. [DOI] [PubMed] [Google Scholar]
- 9.Rietveld S, Everaerd W, Creer TL. Stress-induced asthma: A review of research and potential mechanisms. Clinical and Experimental Allergy. 2000;30(8):1058–1066. doi: 10.1046/j.1365-2222.2000.00809.x. [DOI] [PubMed] [Google Scholar]
- 10.Dumanovsky T, Matte TD. Variation in adult asthma prevalence in Hispanic subpopulations in New York City. Journal of Asthma. 2007;44(4):297–303. doi: 10.1080/02770900701344140. [DOI] [PubMed] [Google Scholar]
- 11.Rose D, Mannino DM, Leaderer BP. Asthma prevalence among US adults, 1998–2000: Role of Puerto Rican ethnicity and behavioral and geographic factors. American Journal of Public Health. 2006;96(5):880–888. doi: 10.2105/AJPH.2004.050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rhodes L, Moorman J, Redd S, Mannino D. Self-reported asthma prevalence and control among adults–United States, 2001. MMWR. Morbidity and Mortality Weekly Report. 2003;52(17):381–384. doi: 10.1001/jama.289.20.2639. [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum E. Racial/ethnic differences in asthma prevalence: The role of housing and neighborhood environments. Journal of Health and Social Behavior. 2008;49(2):131–145. doi: 10.1177/002214650804900202. [DOI] [PubMed] [Google Scholar]
- 14.Garg R, Karpati A, Leighton J, Perrin M, Shah M. Asthma Facts. 2. New York City Department of Health and Mental Hygiene; 2003. http://www1.nyc.gov/site/doh/health/health-topics/asthma-facts.page. [Google Scholar]
- 15.Burchard E, Avila P, Nazario S. Genetics of Asthma in Latino Americans (GALA) Study. 2005 https://pharm.ucsf.edu/gala/home.
- 16.Warman K, Silver EJ, Wood PR. Modifiable risk factors for asthma morbidity in Bronx versus other inner-city children. Journal of Asthma. 2009;46(10):995–1000. doi: 10.3109/02770900903350481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitchell I, Tough SC, Semple LK, Green FH, Hessel PA. Near-fatal asthma: A population-based study of risk factors. CHEST Journal. 2002;121(5):1407–1413. doi: 10.1378/chest.121.5.1407. [DOI] [PubMed] [Google Scholar]
- 18.Katon WJ, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosomatic Medicine. 2004;66(3):349–355. doi: 10.1097/01.psy.0000126202.89941.ea. [DOI] [PubMed] [Google Scholar]
- 19.Feldman JM, Mayefsky L, Beckmann L, Lehrer PM, Serebrisky D, Shim C. Ethnic differences in asthma–panic disorder comorbidity. Journal of Allergy and Clinical Immunology. 2010;125(3):760–762. doi: 10.1016/j.jaci.2009.11.002. http://dx.doi.org/10.1016/j.jaci.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Feldman JM, Lehrer PM, Borson S, Hallstrand TS, Siddique MI. Health care use and quality of life among patients with asthma and panic disorder. Journal of Asthma. 2005;42(3):179–184. doi: 10.1081/JAS-54633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldman JM, Siddique MI, Thompson NS, Lehrer PM. The role of panic-fear in comorbid asthma and panic disorder. Journal of Anxiety Disorders. 2009;23(2):178–184. doi: 10.1016/j.janxdis.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lehrer PM, Hochron SM, Mayne T, Isenberg S, Lasoski AM, Carlson V, … Porges S. Relationship between changes in EMG and respiratory sinus arrhythmia in a study of relaxation therapy for asthma. Applied Psychophysiology and Biofeedback. 1997;22(3):183–191. doi: 10.1023/A:1026263826106. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [DOI] [Google Scholar]
- 24.Lewis-Fernandez R, Guarnaccia PJ, Martínez IE, Salman E, Schmidt A, Liebowitz M. Comparative phenomenology of ataques de nervios, panic attacks, and panic disorder. Culture, Medicine and Psychiatry. 2002;26(2):199–223. doi: 10.1023/A:1016349624867. [DOI] [PubMed] [Google Scholar]
- 25.Lopez I, Ramirez R, Guarnaccia P, Canino G, Bird H. Ataques de nervios and somatic complaints among Island and Mainland Puerto Rican children. CNS Neuroscience & Therapeutics. 2011;17(3):158–166. doi: 10.1111/j.1755-5949.2010.00137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lopez I, Rivera F, Ramirez R, Guarnaccia PJ, Canino G, Bird HR. Ataques de nervios and their psychiatric correlates in Puerto Rican children from two different contexts. The Journal of Nervous and Mental Disease. 2009;3(12):923–929. doi: 10.1097/NMD.0b013e3181c2997d. [DOI] [PubMed] [Google Scholar]
- 27.Hinton DE, Chong R, Pollack MH, Barlow DH, McNally RJ. Ataque de nervios: Relationship to anxiety sensitivity and dissociation predisposition. Depression and Anxiety. 2008;25(6):489–495. doi: 10.1002/da.20309. [DOI] [PubMed] [Google Scholar]
- 28.Hinton DE, Lewis-Fernandez R, Pollack MH. A model of the generation of ataque de nervios: The role of fear of negative affect and fear of arousal symptoms. CNS Neuroscience & Therapeutics. 2009;15(3):264–275. doi: 10.1111/j.1755-5949.2009.00101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Potoczek A. Gender and presence of profound psychological traumas versus the presence and intensity of panic disorder in difficult and severe asthma and aspirin--induced asthma of different severity. Archives of Psychiatry and Psychotherapy. 2011;2:59–65. http://www.kom-red-wyd-ptp.com.pl/indexen.php. [Google Scholar]
- 30.Lu Y, Feng L, Lim L, Ng TP. Asthma, life events and psychiatric disorders: A population-based study. Social Psychiatry and Psychiatric Epidemiology. 2013;48(8):1273–1282. doi: 10.1007/s00127-013-0655-5. [DOI] [PubMed] [Google Scholar]
- 31.Yii AC, Koh MS. A review of psychological dysfunction in asthma: Affective, behavioral and cognitive factors. Journal of Asthma. 2013;50(9):915–921. doi: 10.3109/02770903.2013.819887. [DOI] [PubMed] [Google Scholar]
- 32.Cohen RT, Canino GJ, Bird HR, Celedón JC. Violence, abuse, and asthma in Puerto Rican children. American Journal of Respiratory and Critical Care Medicine. 2008;178(5):453–459. doi: 10.1164/rccm.200711-1629OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salman E, Liebowitz MR, Guarnaccia PJ, Jusino CM, Garfinkel R, Street L, … Davies SO. Subtypes of ataques de nervios: The influence of coexisting psychiatric diagnosis. Culture, Medicine and Psychiatry. 1998;22(2):231–244. doi: 10.1023/A:1005326426885. [DOI] [PubMed] [Google Scholar]
- 34.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, Liu X. National surveillance of asthma: United States, 2001–2010. Vital & health statistics. Series 3, Analytical and Epidemiological Studies/[US Dept. of Health and Human Services, Public Health Service, National Center for Health Statistics] 2012;(35):1–58. http://www.cdc.gov/nchs/products/pubs/pubd/series/ser.htm. [PubMed]
- 35.Wisnivesky JP, Krauskopf K, Wolf MS, Wilson EA, Sofianou A, Martynenko M, … Federman AD. The association between language proficiency and outcomes of elderly patients with asthma. Annals of Allergy, Asthma & Immunology. 2012;109(3):179–184. doi: 10.1016/j.anai.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 36.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJG, Goodwin RD, Kubzansky L, … Stein MB. Anxiety disorders and comorbid medical illness. General Hospital Psychiatry. 2008;30(3):208–225. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 38.Guarnaccia PJ. Ataques de nervios in Puerto Rico: Culture-bound syndrome or popular illness? Medical Anthropology. 1993;15(2):157–170. doi: 10.1080/01459740.1993.9966087. [DOI] [PubMed] [Google Scholar]
- 39.Feldman JM, Matte L, Interian A, Lehrer PM, Lu SE, Scheckner B, … Shim C. Psychological treatment of comorbid asthma and panic disorder in Latino adults: Results from a randomized controlled trial. Behaviour Research and Therapy. 2016;87:142–154. doi: 10.1016/j.brat.2016.09.007. http://dx.doi.org/10.1016/j.brat.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bravo M. Instrument Development: Cultural Adaptations for Ethnic Minority Research. In: Bernal G, Trimble JE, Burlew AK, Leong FT, editors. Handbook of Racial & Ethnic Minority Psychology. Thousand Oaks, CA: Sage Publications, Inc; 2003. [DOI] [Google Scholar]
- 41.Bravo M, Canino GJ, Rubio-Stipec M, Woodbury-Fariña M. A cross-cultural adaptation of a psychiatric epidemiologic instrument: The diagnostic interview schedule’s adaptation in Puerto Rico. Culture, Medicine and Psychiatry. 1991;15(1):1–18. doi: 10.1007/BF00050825. [DOI] [PubMed] [Google Scholar]
- 42.Canino G, Bravo M. The adaptation and testing of diagnostic and outcome measures for cross-cultural research. International Review of Psychiatry. 1994;6(4):281–286. doi: 10.3109/09540269409023267. [DOI] [Google Scholar]
- 43.Flaherty JA, Gaviria FM, Pathak D, Mitchell T, Wintrob R, Richman JA, Birz S. Developing instruments for cross-cultural psychiatric research. The Journal of Nervous and Mental Disease. 1988;176(5):260–263. http://ovidsp.ovid.com/ [PubMed] [Google Scholar]
- 44.Matias-Carrelo LE, Chávez LM, Negron G, Canino G, Aguilar-Gaxiola S, Hoppe S. The Spanish translation and cultural adaptation of five mental health outcome measures. Culture, Medicine and Psychiatry. 2003;27(3):291–313. doi: 10.1023/a:1025399115023. [DOI] [PubMed] [Google Scholar]
- 45.Alegria M, Vila D, Woo M, Canino G, Takeuchi D, Vera M, … Shrout P. Cultural relevance and equivalence in the NLAAS instrument: Integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. International Journal of Methods in Psychiatric Research. 2004;13(4):270–288. doi: 10.1002/mpr.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spitzer RL, Kroenke K, Williams JB Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Jama. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 47.Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosomatic Medicine. 2001;63(4):679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 48.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition (SCID-I/P; 2002) New York: Biometrics Research, New York State Psychiatric Institute; [Google Scholar]
- 49.First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version. New York: Biometrics Research, New York State Psychiatric Institute; 1996. [Google Scholar]
- 50.First M, Spitzer RL. In: SCID-I Structured Clinical Interview for the DSM-IV Axis I Disorders [Spanish] Blanch J, Andreu I, translators. 1999. [Google Scholar]
- 51.Feldman JM, Giardino ND, Lehrer PM. Asthma and panic disorder. In: Mostofsky DI, Barlow DH, editors. The management of stress and anxiety in medical disorders. Needham Heights, MA: Allyn & Bacon; 2000. pp. 220–239. [Google Scholar]
- 52.Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I disorders (SCID I) and Axis II disorders (SCID II) Clinical Psychology & Psychotherapy. 2011;18(1):75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- 53.Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, … Wang T. Reliability and validity of the Panic Disorder Severity Scale: Replication and extension. Journal of Psychiatric Research. 2001;35(5):293–296. doi: 10.1016/s0022-3956(01)00028-0. [DOI] [PubMed] [Google Scholar]
- 54.Lopez SR, Guarnaccia PJ. Cultural psychopathology: Uncovering the social world of mental illness. Annual Review of Psychology. 2000;51(1):571–598. doi: 10.1146/annurev.psych.51.1.571. [DOI] [PubMed] [Google Scholar]
- 55.Feldman JM, Siddique MI, Morales E, Kaminski B, Lu SE, Lehrer PM. Psychiatric Disorders and Asthma Outcomes Among High-Risk Inner-City Patients. Psychosomatic Medicine. 2005;67(6):989–996. doi: 10.1097/01.psy.0000188556.97979.13. [DOI] [PubMed] [Google Scholar]
- 56.Park DC. Self-regulation and control of rheumatic disorders. In: Maes S, Leventhal H, Johnston M, editors. International Review of Health Psychology. Vol. 3. New York: Wiley; 1994. pp. 189–217. [Google Scholar]
- 57.Lehrer PM, Karavidas MK, Lu SE, Feldman J, Kranitz L, Abraham S, … Reynolds R. Psychological treatment of comorbid asthma and panic disorder: A pilot study. Journal of Anxiety Disorders. 2008;22(4):671–683. doi: 10.1016/j.janxdis.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]