Abstract
Urethroplasty is an effective treatment for men with anterior urethral strictures, but is utilized less frequently than ineffective treatments such as internal urethrotomy. We sought to identify provider-level barriers to urethroplasty. An anonymous online survey was emailed to all Mid-Atlantic American Urological Association members. Six scenarios in which urethroplasty was the most appropriate treatment were presented. Primary outcome was recommendation for urethroplasty in ≥ three clinical scenarios. Other factors measured include practice zip code, urethroplasty training, and proximity to a urethroplasty surgeon. Multivariate logistic regression identified factors associated with increased likelihood of urethroplasty recommendation. Of 670 members emailed, 109 (16%) completed the survey. Final analysis included 88 respondents. Mean years in practice was 17.2. Most respondents received formal training in urethroplasty: 43 (49%) in residency, 5 (6%) in fellowship, and 10 (11%) in both; 48 respondents (55%) had a urethroplasty surgeon in their practice, whereas 18 (20%) had a urethroplasty surgeon within 45 minutes of his or her primary practice location. The only covariate that was associated with an increased likelihood of recommending urethroplasty in ≥ three scenarios was formal urethroplasty training. Most members (68%) reported no barriers to referring patients for urethroplasty; the most common barriers cited were long distance to urethroplasty surgeon (n 5 13, 15%) and concern about complications (n 5 8, 9%). Urethroplasty continues to be underutilized in men with anterior urethral strictures, potentially due to lack of knowledge dissemination and access to a urethroplasty surgeon. Appropriate urethroplasty utilization may increase with greater exposure to urethroplasty in training.
Keywords: Urethral stricture, Urethroplasty, Barriers, Physician practice patterns
Urethroplasty is a highly effective treatment for men with anterior urethral strictures, but is utilized less frequently than ineffective endoscopic treatments such as internal urethrotomy.1-6 Although access to a urethroplasty surgeon has historically been a major barrier,7 the number of urethroplasty surgeons in the United States has increased considerably over the past decade.
In a recent analysis of nationwide practice patterns for men with urethral strictures, we identified significant variation in urethroplasty access even in regions with urethroplasty providers.8 This suggests that factors other than access to a urethroplasty surgeon are important determinants of urethroplasty treatment. In an attempt to better understand these barriers, we queried practicing urologists in the Mid-Atlantic region of the American Urological Association (AUA) about management of men with anterior urethral strictures.
Materials and Methods
A link to an online survey website was emailed to all members of the Mid-Atlantic AUA through the association listserve. A single follow- up phone call was made using phone numbers available on the association website. The 2015 roster of the Society of Genitourinary Reconstructive Surgeons (GURS) was used to identify practice location of urologists specializing in reconstructive surgery.
The Mid-Atlantic section of the AUA, which encompasses the states of Delaware, Maryland, Virginia, and West Virginia, the District of Columbia, the eastern portion of Pennsylvania, and the southern portion of New Jersey, was chosen because of its ethnic and geographic diversity. The region consists of several large metropolitan areas, as well as large rural regions, and contains a large number of reconstructive urologists (42/182 United States GURS members, 23%).
A total of 670 Mid-Atlantic AUA members were emailed, and the survey was completed by 109 members (16%). Surveys were completed from December 10, 2014 through March 21, 2015. Members who reported that they no longer practice urology (2) or do not treat male patients with anterior urethral strictures (19) were excluded, yielding a final study cohort of 88.
The survey was composed of six demographic questions, six clinical scenarios, and one question about barriers to referral. All clinical scenarios contained at least one adverse stricture characteristic—length > 1 cm, failure of previous direct vision internal urethrotomy (DVIU), or penile location—such that the expected recurrence rate after minimally invasive treatment would be > 80%.9 In contrast, urethroplasty has consistently shown 75% to 100% lifetime success ranging across a wide spectrum of disease characteristics.4
The primary outcome was recommendation for urethroplasty in ≥ three clinical scenarios. Covariates in the analysis were years in practice, patient volume, urethroplasty training in residency or fellowship, and proximity of the nearest urethroplasty surgeon. Statistical analysis was performed using Stata SE 11.2® (StataCorp LP, College Station, TX).
… urethroplasty has consistently shown 75% to 100% lifetime success ranging across a wide spectrum of disease characteristics.
Results
The final study cohort consisted of 88 respondents. The median number of years in practice was 16 (interquartile range [IQR] 9.5-25). Median number of men with anterior urethral strictures treated in a typical 3-month period was three (IQR 1-6). A total of 58 respondents (66%) reported formal urethroplasty training: 43 (49%) in residency, 5 (6%) in fellowship, and 10 (11%) in residency and fellowship. A total of 48 respondents (55%) reported that there was a urethroplasty surgeon within his or her practice, 18 (20%) reported one less than 45 minutes away, 11 (13%) reported one between 45 minutes and 2 hours away, and 9 (10%) reported one greater than 2 hours away (Table 1).
Table 1.
Demographic Characteristics of Survey Respondents (N = 88)
| Years in practice (median, IQR) | 16 (9.5–25) |
| Stricture volume/3 mo (median, IQR) | 3 (1–6) |
| Urethroplasty training, N | |
| Any (%) | 58 (66) |
| Residency (%) | 43 (49) |
| Fellowship (%) | 5 (6) |
| Both (%) | 10 (11) |
| Nearest urethroplasty surgeon, N | |
| Within practice (%) | 48 (55) |
| < 45 min (%) | 18 (20) |
| 45 min-2 h (%) | 11 (13) |
| > 2 h (%) | 9 (10) |
IQR, interquartile range.
Primary practice location of respondents was in Pennsylvania (24, 27%), New Jersey (19, 22%), Maryland (17, 19%), Virginia (15, 17%), Delaware (4, 5%), Washington, DC (4, 5%), and West Virginia (2, 2%). Primary practice location of survey respondents by county is shown in Figure 1.
Figure 1.

Density of primary practice location of respondents, by county. Blue dots indicate practice locations of Society of Genitourinary Reconstructive Surgeons (GURS).
Across all clinical scenarios, the most common treatment recommendation was DVIU (n 5 172, 33%) followed by referral for urethroplasty (n 5 158, 30%), urethroplasty performed by the respondent (n 5 110, 21%), dilation (n 5 37, 7%), laser urethrotomy (n 5 26, 5%), and self-catheterization/clean intermittent catheterization (n 5 18, 3%). The frequency of urethroplasty recommendation for each clinical scenario is shown in Figure 2. Respondents were least likely to recommend urethroplasty in a 60-year-old man with an untreated 2-cm bulbar urethral stricture and were most likely to recommend urethroplasty in a 60-year-old man with a 2-cm bulbar urethral stricture who had failed two DVIUs. Of 58 respondents with formal training in urethroplasty, 37 (64%) referred at least one patient for urethroplasty.
Figure 2.
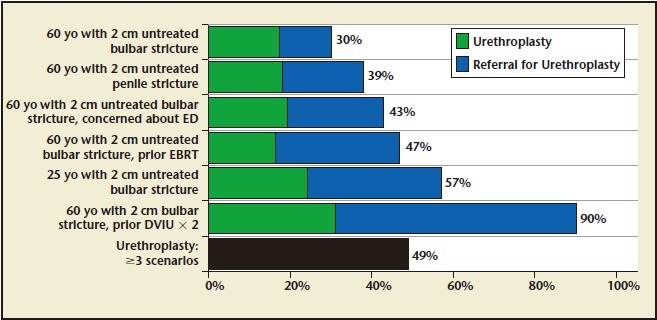
Frequency of urethroplasty recommendation for each clinical scenario. EBRT, external beam radiation therapy; ED, erectile dysfunction; DVIU, direct vision internal urethrotomy.
Formal training in urethroplasty was associated with an increased likelihood of recommending urethroplasty in ≥ three scenarios; however, years in practice, volume of male anterior urethral stricture patients treated in 3 months, and proximity to a urethroplasty surgeon were not (Table 2).
Table 2.
Likelihood of Recommending Urethroplasty in ≥ 3 Clinical Scenarios
| Urethroplasty: < 3 Clinical Scenarios | Urethroplasty: ≥ 3 Clinical Scenarios | OR (95% CI); P Value | |
| Years in practice | 18.4 (8.9) | 16.0 (9.7) | 0.23 |
| Stricture volume/3 mo | 15.8 (74.0) | 12.2 (34.1) | 0.77 |
| Urethroplasty training | |||
| Any (%) | 23 (51) | 35 (81) | 4.2 (1.6–11.0); < .01 |
| Residency (%) | 20 (44) | 23 (53) | 3.2 (1.2–8.7); < .05 |
| Fellowship (%) | 2 (4) | 3 (7) | 4.1 (0.6–29.4); .16 |
| Both (%) | 1 (2) | 9 (21) | 24.8 (2.7–227.6); < .01 |
| Nearest urethroplasty surgeon | |||
| Within practice (%) | 20 (47) | 28 (65) | 1.75 (0.42–7.35); .45 |
| < 45 min (%) | 12 (28) | 6 (14) | 0.63 (0.12–3.22); .57 |
| 45 min-2 h (%) | 6 (14) | 5 (12) | 1.04 (0.18–6.12); .96 |
| > 2 h (%) | 5 (12) | 4 (9) | Ref |
CI, confidence interval; OR, odds ratio.
In multivariate logistic regression, urethral stricture volume was an important covariate (odds ratio [OR] 0.82; 95% confidence interval [CI], 0.33-2.01), but the only covariate that was associated with an increased likelihood of recommending urethroplasty in ≥ three scenarios was urethroplasty training (OR 4.31; 95% CI, 1.62-11.46).
A total of 60 respondents (68%) reported no barriers to referring patients for urethroplasty. Barriers that were identified included reconstructive urologist who was too far away (n 5 13, 15%), concern about postoperative complications (n 5 8, 9%), having no reconstructive urologist in the insurance network (n 5 4, 5%), not knowing a reconstructive urologist (n 5 2; 2%), and concern about losing patients (n 5 1, 1%).
Discussion
Our findings suggest that among self-reported practice patterns for anterior urethral strictures in men, minimally invasive treatments predominate. Although urethroplasty was appropriately recommended when the patient had failed multiple prior DVIUs, patients with long strictures and no prior DVIU continue to be managed endoscopically. The best predictor of urethroplasty recommendation in our study was formal training in urethroplasty, whether in residency or fellowship.
Overutilization of endoscopic management for urethral strictures has been widely demonstrated,4-6 despite evidence that endoscopic management rarely results in long-term patency. In one of the few series with long-term follow-up after DVIU, Pansadoro and Emiliozzi9 reported an overall DVIU success rate of 32% at a median follow-up of 98 months. Stricture length > 1 cm, caliber 15-Fr or less, penile urethral location, and previous failed DVIU were associated with considerably worse outcomes. Among bulbar urethral strictures longer than 1 cm, success rate was 18%. Among patients with penile and penile/ bulbar strictures, success rate was 13%. Among patients who failed a prior DVIU, subsequent DVIU was successful in 0%.
In a randomized trial of dilation versus DVIU, Steenkamp and colleagues10 reported a 60% success rate at 12 months for short (1–2 cm) strictures of the bulbar urethra. Outcomes in this study were considerably worse for longer strictures, with the risk of recurrence more than doubling with each 1-cm increase in stricture length.
Santucci and Eisenberg11 recently reported on 76 men treated with DVIU for urethral strictures, and found a much lower success rate for a single urethrotomy. At a median follow-up of 18 months, the stricture-free rate after a single DVIU was 8%, and median time to recurrence was 7 months.
Largely a result of poor durability, DVIU has been found to be less cost effective than urethroplasty in the majority of cases. Wright12 and associates considered the cost effectiveness of DVIU and urethroplasty from a societal perspective, factoring in lost work and recovery time. They found that DVIU was cost effective when the expected success rate was > 35%. Rourke and Jordan13 conducted a similar analysis but did not factor in lost work and recovery time. They concluded that urethroplasty is economically advantageous in the majority of cases.
Largely a result of poor durability, DVIU has been found to be less cost effective than urethroplasty in the majority of cases.
Although previous studies suggest that the underutilization of urethroplasty is due, at least in part, to limited availability of urethroplasty providers,7,8 we found that most providers did not consider the availability of a urethroplasty surgeon to be a significant barrier; 68% of respondents reported no barriers to referring patients for urethroplasty.
Our findings suggest that the main barrier to urethroplasty is a lack of knowledge about indications for urethroplasty, expected success rates of endoscopic procedures, and the morbidity and side-effect profile of urethroplasty. Respondents who received formal urethroplasty training were significantly more likely to recommend urethroplasty, even if they would not perform the urethroplasty themselves. Of 58 respondents with formal training in urethroplasty, 37 (64%) referred at least one patient for urethroplasty. Based on these findings, we believe that appropriate urethroplasty utilization will continue to increase as the number of residents and fellows exposed to this procedure in training increases.
Our findings suggest that the main barrier to urethroplasty is a lack of knowledge about indications for urethroplasty, expected success rates of endoscopic procedures, and the morbidity and side-effect profile of urethroplasty.
Our survey was designed to elicit individual stricture characteristics that might affect the likelihood of referring a patient for urethroplasty. Although nearly all respondents recognized the failure of two previous DVIUs as a poor prognostic sign and recommended referral for urethroplasty, respondents were unlikely to recommend urethroplasty for a patient with a penile or radiated stricture, despite evidence that these strictures are less likely to respond to endoscopic surgery.9
Our findings are based on a small group of providers who may not be representative of providers nationally. This potential source of bias is increased by a relatively low response rate (16%), which limited our ability to detect differences in treatment patterns according to each of our clinical scenarios. Additional limitations include the lack of a validated instrument and difficulty generalizing our findings to regions of the United States that are demographically, culturally, and economically distinct from the Mid-Atlantic region. Finally, although a number of barriers to urethroplasty exist at the provider level, no studies have assessed patient-reported barriers to urethroplasty. This should be an important aim of future work that seeks to understand underutilization of urethroplasty.
Main Points.
Urethroplasty is an effective treatment for men with anterior urethral strictures, but is utilized less frequently than ineffective treatments such as internal urethrotomy, potentially due to lack of knowledge dissemination and access to a urethroplasty surgeon.
Formal training in urethroplasty was associated with an increased likelihood of recommending urethroplasty in ≥ three scenarios; however, years in practice, volume of male anterior urethral stricture patients treated in 3 months, and proximity to a urethroplasty surgeon were not.
Overutilization of endoscopic management for urethral strictures has been widely demonstrated, despite evidence that endoscopic management rarely results in long-term patency.
Although nearly all respondents to our survey recognized the failure of two previous direct vision internal urethrotomies as a poor prognostic sign and recommended referral for urethroplasty, respondents were unlikely to recommend urethroplasty for a patient with a penile or radiated stricture, despite evidence that these strictures are less likely to respond to endoscopic surgery.
References
- 1.Bullock TL, Brandes SB. Adult anterior urethral strictures: a national practice patterns survey of board certified urologists in the United States. J Urol. 2007;177:685–690. doi: 10.1016/j.juro.2006.09.052. [DOI] [PubMed] [Google Scholar]
- 2.Ferguson GG, Bullock TL, Anderson RE, et al. Minimally invasive methods for bulbar urethral strictures: a survey of members of the American Urological Association. Urology. 2011;78:701–706. doi: 10.1016/j.urology.2011.02.051. [DOI] [PubMed] [Google Scholar]
- 3.Rapp DE, Chanduri K, Infusino G, et al. Internet survey of management trends of urethral strictures. Urol Int. 2008;80:287–290. doi: 10.1159/000127343. [DOI] [PubMed] [Google Scholar]
- 4.Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol. 2007;177:1667–1674. doi: 10.1016/j.juro.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 5.Anger JT, Buckley JC, Santucci RA, et al. Urologic Diseases in America Project. Trends in stricture management among male Medicare beneficiaries: underuse of urethroplasty? Urology. 2011;77:481–485. doi: 10.1016/j.urology.2010.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anger JT, Scott VC, Sevilla C, et al. Patterns of management of urethral stricture disease in the Veterans Affairs system. Urology. 2011;78:454–458. doi: 10.1016/j.urology.2010.12.081. [DOI] [PubMed] [Google Scholar]
- 7.Burks FN, Salmon SA, Smith AC, Santucci RA. Urethroplasty: a geographic disparity in care. J Urol. 2012;187:2124–2127. doi: 10.1016/j.juro.2012.01.078. [DOI] [PubMed] [Google Scholar]
- 8.Figler BD, Gore JL, Holt SK, et al. High regional variation in urethroplasty in the United States. J Urol. 2015;193:179–183. doi: 10.1016/j.juro.2014.07.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: long-term followup. J Urol. 1996;156:73–75. [PubMed] [Google Scholar]
- 10.Steenkamp JW, Heyns CF, Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: a prospective, randomized comparison. J Urol. 1997;157:98–101. [PubMed] [Google Scholar]
- 11.Santucci R, Eisenberg L. Urethrotomy has a much lower success rate than previously reported. J Urol. 2010;183:1859–1862. doi: 10.1016/j.juro.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 12.Wright JL, Wessells H, Nathens AB, Hollingworth W. What is the most cost-effective treatment for 1 to 2-cm bulbar urethral strictures: societal approach using decision analysis. Urology. 2006;67:889–893. doi: 10.1016/j.urology.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Rourke KF, Jordan GH. Primary urethral reconstruction: the cost minimized approach to the bulbous urethral stricture. J Urol. 2005;173:1206–1210. doi: 10.1097/01.ju.0000154971.05286.81. [DOI] [PubMed] [Google Scholar]


