Short abstract
The potential benefits of linking tuberculosis control programmes with interventions to reduce smoking and indoor air pollution make research to improve our understanding of their relation a high priority
Tuberculosis, smoking, and indoor air pollution from solid fuels are among the leading global causes of death and burden of disease.1,2 Several studies have observed an increased risk of tuberculosis disease or mortality among smokers and those exposed to indoor air pollution, but our understanding of the strength and causal pathways of the risk remains uncertain Tuberculosis and exposure to respirable pollutants are often highest in the poorest socioeconomic groups, who are also those with the least access to interventions and health care. Thus, integrating interventions to reduce smoking and indoor air pollution with tuberculosis control programmes could in principle increase coverage and effectiveness. We discuss the arguments for linking the two public health measures and the scientific uncertainties that currently limit the potential for integration.
Current evidence and its limitations
Tuberculosis, indoor air pollution from solid fuels, and smoking each accounted for substantial mortality and disease burden in 2000, with a high proportion in developing countries (table). Epidemiological studies have found an increased risk of tuberculosis disease or mortality among smokers and those exposed to indoor air pollution, with relative risks or odds ratios varying between > 1 and nearly 5.4-10 Most published studies have used a retrospective, case-control design, generally with limited control for covariates (such as socioeconomic status, nutrition, alcohol consumption, housing, and crowding) or assessment of heterogeneity of risk. All studies have used self reported exposure for smoking and solid fuel use, and few have examined a dose-response relation.5 A few studies on smoking have considered increased risk of death from tuberculosis.4,6,8 All other studies have examined increased risk of tuberculosis disease in patients with confirmed tuberculosis in medical facilities and community disease surveillance or self reported cases in household surveys. More studies have examined smoking as a risk factor for tuberculosis than indoor air pollution, generally with more systematic identification of tuberculosis cases.
Table 1.
Mortality and burden of disease from tuberculosis, exposure to indoor air pollution from solid fuels, and smoking in the year 2000. Numbers in brackets show the proportion of deaths in developing countries1,2
| No of deaths (millions) | Burden of disease (% of total global burden of disease)* | |
|---|---|---|
| Tuberculosis† | 1.6(>90%) | 2.5(>90%) |
| Indoor air pollution | 1.6(>95%) | 2.6(>95%) |
| Smoking | 4.8 (50%) | 4.1(>50%) |
Burden of disease is measured in disability adjusted life years (DALY).
Deaths from tuberculosis exclude those among people with HIV according to the tenth revision of the International Classification of Disease system (ICD-10). When people with HIV are included, the total number of deaths is about 2 million.3
The relatively small number of epidemiological studies and limitations in their design mean that our knowledge of the presence, strength, and operative mechanisms of any relation between respirable pollutants and tuberculosis is uncertain. Given the central role of the infecting bacillus in tuberculosis microbiology and epidemiology, the observed association could be thought of as spurious, especially because solid fuels and smoking may both be correlated with socioeconomic and behavioural factors (poverty, poor housing and nutrition, risky behaviours, etc) that are also determinants of tuberculosis infection, progression to disease, or mortality. However, the consistency of association in increasingly well-designed studies, with more systematic measurement of exposure and outcome and control for covariates, would reduce the likelihood of an entirely spurious association. Potential mechanisms for reduced pulmonary resistance to infection as a result of exposure to respirable pollutants11—including increased airway resistance, increased permeability of the pulmonary epithelia, disruption of ciliary action, and reduced macrophage response—provide some biological plausibility for a causal association.
Linked or separate intervention programmes?
The existence of a causal association alone, even if confirmed in subsequent studies, would have limited implications for public health interventions and policies. Even excluding tuberculosis, mortality and disease burden attributable to both smoking and indoor air pollution places them among leading global health concerns, persistently and increasingly affecting the poor.1,2 Therefore, establishing a causal link with tuberculosis will add little to the already strong arguments for reducing these two risk factors.
Neither can interventions for smoking and indoor air pollution be used as key elements of tuberculosis control, because tuberculosis control cannot rely on any single risk factor whose role in disease aetiology and transmission dynamics is highly dependent on multiple other factors, with heterogeneity across populations or over time. This is in contrast to diseases like chronic obstructive pulmonary disease, for which a reduction in exposure to airborne pollutants would reduce disease in nearly all circumstances. The core of national or regional tuberculosis control programmes therefore has unequivocally been, and should remain, interventions that can reduce and eventually interrupt transmission under relatively generalisable circumstances—that is, the directly observed treatment, short-course (DOTS) strategy.12,13
The effectiveness and coverage of DOTS, however, has been constrained by obstacles such as cost, physical and human infrastructure, and compliance of users or providers, which have limited case detection and completion of treatment.3,12-14 Hence, it is widely acknowledged that achieving higher case detection rates under DOTS requires participation outside health systems,12-14 but the nature of this participation needs to be better defined in different populations. A causal relation with respirable pollutants might provide a possible mechanism for such participation. Before attempting to link the two public health interventions, however, we need a better understanding of the aetiological relation between respirable pollutants and tuberculosis.
Implications of different possible mechanisms of association
We currently have insufficient evidence about the mechanisms of the association between respirable pollutants from smoking or indoor air pollution and tuberculosis. Respirable pollutants may increase the probability of initial infection after exposure to Mycobacterium tuberculosis or progression to active tuberculosis.4 Alternatively, the acute and chronic damage to the respiratory system caused by respirable pollutants may increase the risk of mortality among people with active tuberculosis.
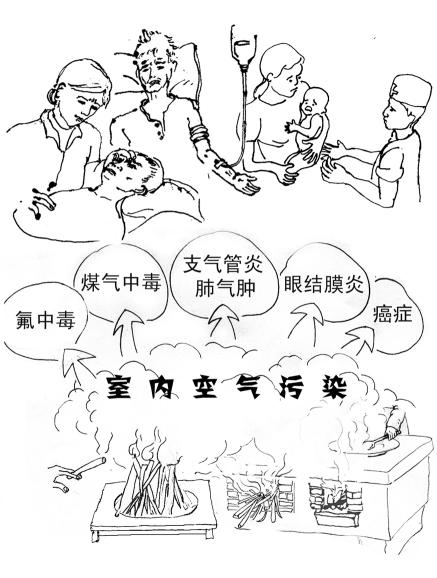
Figure 2.
Poster used to educate people in rural China about dangers of indoor air pollution
Credit: HUAXI SCHOOL OF PUBLIC HEALTH, CHINA CENTRE FOR DISEASE CONTROL AND PREVENTION
If respirable pollutants increase the risk of mortality among those with the disease, interventions against smoking or indoor air pollution will not reduce or interrupt transmission of tuberculosis (one of the central aims of tuberculosis control) but can increase the survival of patients with tuberculosis. Some interventions, such as subsidised provision of cleaner fuels and stoves to people who are tested for tuberculosis and complete treatment, may even encourage people in low income households to report to tuberculosis dispensaries (increased case detection) and enhance compliance with treatment, both important current hurdles to expansion of DOTS.
If those exposed to respirable pollutants are at an increased risk of initial infection or progression to active tuberculosis, but not necessarily of death once active tuberculosis is developed, integrating smoking and indoor air pollution interventions with DOTS cannot provide survival benefits. Because these risks, especially solid fuel use, affect the poor, who also have less access to tuberculosis case detection and treatment, the combination of socioeconomic correlation and aetiological association might be used to tackle the growing concern about limited DOTS coverage.
Many countries and aid agencies are planning and implementing rural energy and health education programmes to reduce exposure to indoor air pollution, which is directly or indirectly related to multiple millennium development goals, such as environmental sustainability, reducing child mortality, and gender equity. Successful implementation of these programmes requires the presence of trained staff in communities and follow up for several months to monitor adoption and maintenance of technology. Indoor air pollution projects are increasingly implemented by agencies whose primary focus is health. If indoor air pollution is a risk factor for tuberculosis infection, energy-health projects could be a low cost approach to increase case detection in households using solid fuel. Project workers could at least ask about symptoms and refer potential cases to a health provider. Sputum collection and testing could also be included when training and organisational circumstances allow.
A remaining question would be whether the energy-health programme workers could supervise treatment for tuberculosis patients who have minimal contact with other health services. Given the need for strict adherence to a standard regimen, workers would require enhanced technical and managerial training that is currently not a part of any indoor air pollution programme. However, other efforts to train community members and health workers for therapeutic interventions could be used as a model for this linkage of services.15
China: an illustrative example
China had an estimated 1.4 million new cases of tuberculosis in 2000, more than any country except India.16 China made substantial progress in expanding DOTS in the 1990s in 13 provinces, municipalities, and autonomous regions.16 Nevertheless, case detection and completion of treatment remain important challenges in poor rural areas.17
Nearly 80% of China's population relies on biomass (wood, crop residues, and animal dung) and coal for cooking and heating.18 China also has one of the highest levels of tobacco consumption in the world, with more than 60% of men smoking.8 The two risk factors, both increasingly concentrated in rural populations, magnify one another's effects, resulting in high levels of respiratory diseases among Chinese adults.1,2,8 The Chinese improved (high efficiency and low emissions) stove programme has primarily targeted exposure during cooking (figure).19 Home heating remains an important route of exposure, as does the absence of improved stove programmes in the poorest provinces and communities.
Figure 1.
Biomass burning stove in rural China
Credit: HUAXI SCHOOL OF PUBLIC HEALTH, SICHUAN UNIVERSITY
Two important characteristics of new indoor air pollution programmes in poor communities are targeting solid fuel use and cigarettes as sources of airborne pollutants and combining clean fuels and stoves with health education among adults and children. Linking tuberculosis control to rural energy and health programmes as described above could in principle increase case detection and ultimately the coverage and community effectiveness of DOTS.
Research needs
A persisting challenge of public health in resource poor settings is scaling-up efficacious technical innovations (such as DOTS or clean energy technologies) into programmes with high community effectiveness. An important step in meeting this challenge is to integrate interventions whose targets are linked, socially and aetiologically. This allows increased coverage and effectiveness compared with individual programmes, as shown by the programme on integrated management of childhood illness. If the observed association between respirable pollutants and tuberculosis is confirmed as aetiological and accompanied by a better understanding of the operative mechanisms, a programme on “integrated management of respiratory health” may provide an opportunity to design intervention clusters for respiratory diseases and risk factors. Further integration could be considered through national or subnational policies such as using tobacco taxation to subsidise DOTS, clean energy technology, and nutrition for poor households that take part in integrated programmes.
Summary points
Risk of tuberculosis disease or mortality is increased among smokers and those exposed to indoor air pollution from solid fuels
The social and potential aetiological links between respirable pollutants and tuberculosis could provide an opportunity for integrated intervention
Before attempting integrated programmes three important research and surveillance issues must be tackled
Scientific research must establish whether respirable pollutants increase susceptibility to new infections, facilitate progress to active tuberculosis, or increase tuberculosis mortality risk
Tuberculosis surveillance should incorporate data on smoking and fuel use to quantify the correlation between tuberculosis and these risk factors
Effectiveness of joint interventions needs to be assessed to avoid compromising existing tuberculosis programmes and to select the most effective combination of interventions
Previous attempts to integrate tuberculosis control with other interventions have been abandoned because of demanding managerial needs.13,20 Most of these other interventions were not directly related to tuberculosis control—for example, vaccination. Interventions against smoking and indoor air pollution, however, could strengthen measures to combat tuberculosis and require little extra effort.
Before linked programmes can be designed, further research is needed to establish whether respirable pollutants increase susceptibility to tuberculosis, facilitate progress to active tuberculosis, or increase mortality. In addition, tuberculosis control programmes should collect data on exposure to tobacco and indoor air pollutants in order to quantify the correlation between tuberculosis and these risk factors. Finally, intervention studies are needed to determine whether linking DOTS with measures to reduce smoking and exposure to indoor air pollution is more effective than single interventions. This information would allow the benefits of various intervention packages to be modelled in terms of their potential to reduce tuberculosis transmission or mortality.
We thank Marc Mitchell, Megan Murray, and Joshua Salomon for valuable comments and references. The findings, interpretations, and conclusions expressed here are those of the authors and do not necessarily reflect the views of the board of executive directors of the World Bank or the governments they represent.
Contributors and sources: EB and ME conduct research on and implement health interventions in developing countries, with focus on cross sectoral programmes and policies. This paper originated from their field experiences in poor rural areas.
Funding: ME was supported by a grant from National Institute on Aging (PO1-AG17625).
Competing interests: None declared.
References
- 1.World Health Organization. World health report 2002: reducing risks, promoting healthy life. Geneva: WHO, 2002. [DOI] [PubMed]
- 2.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJL, Comparative Risk Assessment Collaborative Group. Selected major risk factors and global and regional burden of disease. Lancet 2002;360: 1347-60. [DOI] [PubMed] [Google Scholar]
- 3.Frieden TR, Sterling TR, Munsiff SS, Watt CJ, Dye C. Tuberculosis. Lancet 2003;362: 887-99. [DOI] [PubMed] [Google Scholar]
- 4.Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43 000 adult male deaths and 35 000 controls. Lancet 2003;362: 507-15. [DOI] [PubMed] [Google Scholar]
- 5.Kolappan C, Gopi PG. Tobacco smoking and pulmonary tuberculosis. Thorax 2002;57: 964-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lam TH, Ho SY, Hedley AJ, Mak KH, Peto R. Mortality and smoking in Hong Kong: case-control study of all adult deaths in 1998. BMJ 2001;323: 361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung CC, Yew WW, Chan CK, Tam CM, Lam CW, Chang KC, et al. Smoking and tuberculosis in Hong Kong. Int J Tuberc Lung Dis 2003;7: 980-6. [PubMed] [Google Scholar]
- 8.Liu BQ, Peto R, Chen ZM, Boreham J, Wu YP, Li JY, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ 1998;317: 1411-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mishra VK, Retherford RD, Smith KR. Biomass cooking fuels and prevalence of tuberculosis in India. Int J Infect Dis 1999;3: 119-29. [DOI] [PubMed] [Google Scholar]
- 10.Perez-Padilla R, Perez-Guzman C, Baez-Saldana R, Torres-Cruz A. Cooking with biomass stoves and tuberculosis: a case control study. Int J Tuberc Lung Dis 2001;5: 1-7. [PubMed] [Google Scholar]
- 11.Thomas P, Zelikoff J. Air pollutants: moderators of pulmonary host resistance against infection. In: Holgate ST, Samet JM, Koren HS, Maynard RL, eds. Air pollution and health. San Diego, CA: Academic Press, 1999.
- 12.Dye C, Watt CJ, Bleed DM. Low access to a highly effective therapy: a challenge for international tuberculosis control. Bull World Health Organ 2002;80: 437-44. [PMC free article] [PubMed] [Google Scholar]
- 13.Raviglione MC, Pio A. Evolution of WHO policies for tuberculosis control, 1948-2001. Lancet 2002;359: 775-80. [DOI] [PubMed] [Google Scholar]
- 14.Dye C, Watt CJ, Bleed DM, Williams BG. What is the limit to case detection under the DOTS strategy for tuberculosis control? Tuberculosis 2003;83: 35-43. [DOI] [PubMed] [Google Scholar]
- 15.Squire SB, Wilkinson D. Strengthening “DOTS” through community care for tuberculosis. BMJ 1997;315: 1395-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.China Tuberculosis Control Collaboration. The effect of tuberculosis control in China. Lancet 2004;364: 417-22. [DOI] [PubMed] [Google Scholar]
- 17.Squire SB, Tang S. How much of China's success in tuberculosis control is really due to DOTS? Lancet 2004;364: 391-2. [DOI] [PubMed] [Google Scholar]
- 18.Florig HK. China's air pollution risks. Environ Sci Tech 1997;31: 274-9A. [DOI] [PubMed] [Google Scholar]
- 19.Smith KR, Shuhua G, Kun H, Daxiong Q. One hundred million improved cookstoves in China: how was it done? World Development 1993;21: 941-61. [Google Scholar]
- 20.Raviglione MC, Dye C, Schmidt S, Kochi A. Assessment of worldwide tuberculosis control. WHO global surveillance and monitoring project. Lancet 1997;350: 624-9. [DOI] [PubMed] [Google Scholar]