Abstract
Aim
This study was designed to investigate the predictive and prognostic values of serum vascular endothelial growth factor (VEGF) level in non-small cell lung cancer (NSCLC) patients treated with platinum-based chemotherapy.
Methods
Patients’ peripheral blood samples were collected prior to chemotherapy and after 1 week of the third cycle of combination chemotherapy. Serum VEGF levels were evaluated through Luminex multiplex technique. Between September 2011 and August 2015, a total of 135 consecutive advanced or recurrent histologically verified NSCLC patients were enrolled in the study. Moreover, all the patients received platinum-based combination chemotherapy as a first-line treatment.
Results
No significant associations were found between pretreatment serum VEGF levels and clinical characteristics, such as sex (P=0.0975), age (P=0.2522), stage (P=0.1407), lymph node metastasis (P=0.6409), tumor location (P=0.3520), differentiated degree (P=0.5608), pathological (histological) type (P=0.4885), and response to treatment (P=0.9859). The VEGF load per platelet (VEGFPLT) levels were not correlated with sex, age, primary tumor site, and pathological type in NSCLC patients (all P>0.05). The median survival time of progression-free survival (PFS) was 6.407 and 5.29 months in the low and high groups, respectively, when using 280 pg/mL VEGF level as the cutoff point (P=0.024).
Conclusion
In conclusion, the serum VEGF levels were found to be a poor prognostic biomarker for the efficacy of platinum-based chemotherapy in terms of PFS, but it was not shown to be a suitable predictive marker for clinical response to platinum-based chemotherapy.
Keywords: non-small cell lung cancer, VEGF, progression-free survival, platinum, chemotherapy, Luminex multiplex, prognosis
Video abstract
Introduction
Lung cancer is the leading cause of cancer-related death worldwide. Moreover, non-small cell lung cancer (NSCLC) accounts for 80% of lung cancer.1 The majority of the NSCLC patients are in advanced stage when diagnosed. Patients with a good performance status (PS) in this stage can benefit from platinum-based chemotherapy, particularly those without epidermal growth factor receptor mutation or anaplastic lymphoma kinase translocation.2 However, NSCLC patients still show poor response to chemotherapy because of the relatively short duration and rarity of complete remissions. The median survival of advanced NSCLC patients treated with chemotherapy alone is ~10 months.3 While selecting patients who may benefit from chemotherapeutic modalities, identifying validated biomarkers associated with chemotherapeutic response and prognosis of NSCLC is essential. Moreover, stratifying NSCLC patients as well as monitoring tumor progression and therapeutic response may be useful. Being noninvasive and convenient, blood-based markers have significant advantages over tissue biomarkers.
Neoangiogenesis is critical in tumor growth and systemic dissemination of cancer cells and may be related to the poor survival in NSCLC patients. Vascular endothelial growth factor (VEGF) is largely responsible for neoangiogenesis.4 VEGF signal pathways regulate endothelial cell migration, proliferation, survival, and expression of downstream genes.5 Kondo et al first recognized the potential of VEGF as a serum diagnostic marker for malignant diseases. They found that the VEGF levels in the sera from cancer patients were significantly higher than those without signs of cancer.6 Since then, studies have focused on the predictive and prognostic implications of circulating VEGF in NSCLC and other cancer types. The predictive role of circulating VEGF for chemotherapy response was studied, and some results revealed that VEGF was not associated with chemotherapy response in NSCLC patients.7,8 However, Lissoni et al reported that the chemotherapy response was worse in patients of NSCLC and colorectal carcinoma with higher levels of pretreatment VEGF.9 Similarly, investigations on the prognostic impact of VEGF in chemotherapy revealed conflicting results. The discrepancy between the studies might be explained by the different methodologies used in assessing VEGF concentrations and the different histological types, sample sizes, or treatment regimens used in the study populations. Therefore, improving detection techniques and classification criteria may help identify the predictive and prognostic values.
Serum marker detection was done traditionally using the enzyme-linked immunosorbent assay (ELISA), which requires a large sample volume and is expensive. Recently, the FLEXMAP 3D™ system, which is based on lipid assay technology, has been widely used for its multiplexed function and enhanced sensitivity.10
We previously measured serum VEGF levels in NSCLC patients using the Luminex® xMAP® and found that serum VEGF levels were closely correlated with NSCLC progression and metastasis.11 However, we did not explore the relationship between VEGF concentrations and treatment response. Following the abovementioned investigations, we hypothesized that serum VEGF levels may be an independent predictive and prognostic markers for NSCLC patients. In this study, we estimated the predictive and prognostic values of serum VEGF level in platinum-based chemotherapy patients.
Materials and methods
Ethical statement
The study was approved by the Institutional Review Board and the Research and Ethical Committee of Nanjing Medical University Affiliated Cancer Hospital. Written informed consents were obtained from all participants.
Patient population
Between September 2011 and August 2015, a total of 135 consecutive advanced or recurrent NSCLC patients with histologically verified were enrolled in the study. The 135 NSCLC patients included 91 males and 44 females, with a mean age of 58.5 years (range, 28–78 years). To be eligible for first-line combination chemotherapy, the patients were required to meet the following criteria: cytologically or histologically proven lung cancer; measureable unresectable stage III–IV disease or recurrence after surgery; an Eastern Cooperative Oncology Group PS of 0 or 1; normal hepatic, renal and hematological functions; and no concomitant or serious comorbidities. Stage classification was based on the Union for International Cancer Control–Tumor Node Metastasis classification. Patients with other malignant neoplasms were ruled out. Written informed consent was obtained from each patient prior to the start of the study. Patient follow-ups were obtained through the hospital records and direct patient contact.
Treatment planning
All of the patients who received platinum-based combination chemotherapy as a first-line treatment were enrolled from September 2011 to August 2015. The chemotherapy regimens were as follows: pemetrexed 0.5 g/m2 iv drip d1; cisplatin 75 mg/m2 iv drip d1; q21d (PC regimen), gemcitabine 1.25 g/m2 iv drip d1, 8; cisplatin 75 mg/m2 iv drip d1, q21d (GP regimen), and docetaxel 75 mg/m2 iv drip d1; cisplatin 75 mg/m2 iv drip d1, q21d (TP regimen), and the GP regimen was continued for 4 cycles. PC or TP regimen was administrated for 6 cycles. Pemetrexed or docetaxel was maintained until disease progressed.
Collection and preservation of blood samples
Patients’ peripheral blood samples were collected before chemotherapy and after 1 week of the third cycle of conventional chemotherapy. A total of 3 mL venous blood was extracted from the fasting patients. The blood samples were immediately collected in the endotoxin- and pyrogen-free test tubes. The whole blood specimens were then shaken three times and left to coagulate for 30 min at room temperature. The blood samples were centrifuged at 1,000× g for 10 min at 4°C, and the serum was transferred to Eppendorf tubes and stored at −80°C until analysis. The sera of the participants were obtained following the approval from the Ethics Committee of Nanjing Medical University Affiliated Cancer Hospital (Nanjing, People’s Republic of China). Written informed consent was obtained from each patient.
Detection of serum VEGF
The assay used a Luminex multiplex technique. The FLEXMAP 3D system was supplied by Luminex Corporation (Austin, TX, USA). Serum VEGF levels were examined through human cytokine/chemokine panels (cat no MPXHCYTO-60K). Assays were performed according to the manufacturer’s instructions. All reagents were acclimatized to room temperature before the main immunoassay procedure. The placement of standards for VEGF was 0 (background), 3.2, 16, 80, 400, 2,000, and 10,000 pg/mL, control and test specimens were then added to the plate (25 µL per well). The specimens were shaken at room temperature for 16 h, avoiding light. After washing twice, a 25-µL detection antibody was added and the plates were shaken for 1 h at room temperature. After incubating with agitation on a plate shaker for 1 h at room temperature (20°C–25°C), 2-µL streptavidin–phycoerythrin was added to each well. The plate was then further incubated for 30 min and washed twice with 200 µL/well wash buffer, and 150-µL sheath fluid was added to each well. The plate was run on the FLEXMAP 3D system, and the median fluorescence intensity results were saved and analyzed using a weighted five-parameter logistic method to calculate the sample concentrations. The concentration of VEGF load per platelet (VEGFPLT) (pg/mL) was calculated as serum VEGF (pg/mL)/platelet count ×106, correcting for the variations in platelet counts between patients.12
Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) 18.0. Numeric values were expressed as mean ± standard deviation (SD). The independent sample t-test/Mann–Whitney U and chi-square tests/Fisher’s exact test were used to compare values among different groups for continuous variables and categorical variables, respectively. Cox regression analysis was performed to assess potential prognostic factors. We utilized Pearson’s/Spearman’s correlation coefficient to evaluate the correlations between VEGF concentration and clinical parameters. In all statistical analyses, a P-value <0.05 was considered significant.
Results
General features of the patients
This study was conducted in 135 inoperable NSCLC patients. The baseline characteristics of all the patients are summarized in Table 1. Among the 135 patients, 91 were males and 44 were females. A total of 28 patients were pathologically diagnosed with squamous cell carcinoma, 105 patients with adenocarcinoma, and 2 were missing. Moreover, 61 patients (45.19%) were aged >60 years, 74 patients (54.81%) were aged ≤60 years, and the median age was 59.5 years (range, 28–78). During initial blood sample collection, 35.56% of the patients had stage III (48/135) and 64.44% had stage IV cancers (87/135). On the basis of the tumor location, 25.19% of the patients (34/135) had central pulmonary tumors, 69.63% (94/135) exhibited peripheral pulmonary tumors, and 5.18% were missing (7/135). Furthermore, 37 patients (27.41%) were histopathologically confirmed to have poorly differentiated carcinomas, 10 (7.41%) had moderately differentiated carcinomas, 2 (1.48%) had well-differentiated carcinomas, and 86 (63.7%) were missing. A total of 35.56% (48/135) cases had no distant metastases and 64.44% (87/135) cases had distant metastases.
Table 1.
Patient characteristics
| Clinicopathological characteristics | Patients, n (%) |
|---|---|
| Sex | |
| Male | 91 (67.41) |
| Female | 44 (32.59) |
| Age, years | |
| >60 | 61 (45.19) |
| ≤60 | 74 (54.81) |
| TNM stage | |
| III | 48 (35.56) |
| IV | 87 (64.44) |
| Location | |
| Central | 34 (25.18) |
| Peripheral | 94 (69.63) |
| Missing | 7 (5.19) |
| Histological grade | |
| Grade 1 | 2 (1.48) |
| Grade 2 | 10 (7.41) |
| Grade 3 | 37 (27.41) |
| Grade data missing | 86 (63.70) |
Abbreviation: TNM, tumor node metastasis.
Correlation between serum VEGF levels and clinical pathological parameters
The relationship between serum VEGF and clinical pathological parameters is shown in Table 2. The median serum VEGF concentration in all patients was 134 pg/mL (range, 9.0–15,998 pg/mL). No significant associations were found between pretreatment serum VEGF levels and clinical characteristics, such as sex (P=0.0975), age (P=0.2522), stage (P=0.1407), lymph node metastasis (P=0.6409), tumor location (P=0.3520), differentiated degree (P=0.5608), pathological (histological) type (P=0.4885), and response to treatment (P=0.9859).
Table 2.
Clinicopathological features associated with VEGF in non-small cell lung cancer patients
| Variables | VEGF (pg/mL)
|
|
|---|---|---|
| Median (IQR) | P-value | |
| Sex | 0.0975 | |
| Male | 141.00 (80.00, 250.00) | |
| Female | 98.50 (32.00, 234.00) | |
| Age (years) | 0.2522 | |
| >60 | 149.00 (66.00, 151.00) | |
| ≤60 | 115.50 (10.00, 227.00) | |
| TNM stage | 0.1407 | |
| IV | 112.00 (40.00, 227.00) | |
| III | 153.50 (87.50, 257.50) | |
| Lymph node metastasis | 0.6409 | |
| N1 | 121.50 (32.00, 284.00) | |
| N2 | 135.00 (64.00, 253.00) | |
| N3 | 183.00 (90.00, 285.00) | |
| Location | 0.3520 | |
| Central | 156.00 (75.00, 259.00) | |
| Peripheral | 127.00 (48.00, 241.00) | |
| Histology | 0.4885 | |
| SCC | 153.50 (63.50, 271.50) | |
| ADC | 122.00 (50.00, 225.00) | |
| Histological grade | 0.5608 | |
| Grade 1 | 220.50 (200.00, 241.00) | |
| Grade 2 | 102.50 (62.00, 225.00) | |
| Grade 3 | 122.00 (50.00, 250.00) | |
| Response* | 0.9859 | |
| CR + PR | 138.00 (41.00, 241.00) | |
| SD + PD | 119.50 (62.00, 243.00) | |
Note:
Tumor response was evaluated according to the response evaluation criteria for solid tumors.33
Abbreviations: ADC, adenocarcinomas; CR, complete response; IQR, interquartile range; PD, progressive disease; PR, partial response; SCC, squamous cell carcinomas; SD, stable disease; TNM, tumor node metastasis; VEGF, vascular endothelial growth factor.
A significant amount of VEGF is stored within platelet membranes, thus platelets may be a major source of serum VEGF.13 Therefore, we examined VEGFPLT with an expectation to minimize the variations due to the differences in platelet counts among NSCLC patients, and this may be a reliable method to examine the clinical effects of VEGF inpatients. However, we failed to associate pretreatment serum VEGFPLT and patients’ clinical characteristics. The VEGFPLT levels showed no correlations with sex, age, primary tumor site, and pathological type in NSCLC patients (all P>0.05).
Predictive and prognostic values of VEGF in NSCLC patients
In this study, a total of 65 patients (48.15%) had complete or partial response and 70 patients (51.85%) had stable or progressive disease (PD) (Table 2). Moreover, pretreatment concentrations of VEGF and first-line platinum-based combination chemotherapy effects were not correlated (P=0.9859).
The median follow-up time was 7.0 months. During the follow-up periods, disease progression was detected in 120 (88.89%) patients, 5 (3.70%) patients had died, 6 (4.44%) patients had not progressed, and 4 (2.96%) patients were missing. After 1 year, 100 (74.07%) patients were found to have PD, 28 (20.74%) had not progressed, 3 (2.22%) had died, and 4 (2.96%) were missing. One-year progression-free survival (PFS) rate was 19.26%. Moreover, age, sex, stage, treatment modality, response to treatment, and VEGF level were evaluated for survival using univariate analysis. Among the variables evaluated, VEGF >280 pg/mL was determined as an independent factor for PFS. Results of multivariate analysis are summarized in Table 3. After adjusting for age and sex, high VEGF levels tended to be associated with a poor prognosis (P=0.024). Patients with higher VEGF levels (≥280 pg/mL) had shorter PFS (median, 5.29 months; 95% CI, 2.293–8.186 months) versus lower VEGF levels (median 6.407 months; 95% CI, 5.068–7.745 months; Figure 1).
Table 3.
Univariate analysis for prognosis of patients with NSCLC
| Variables | Univariate
|
Multivariate*
|
||
|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Sex | 0.2770 | |||
| Male | 1.237 (0.843, 1.816) | |||
| Female | ||||
| Age (years) | 0.1956 | |||
| >60 | 1.268 (0.885, 1.816) | |||
| ≤ 60 | ||||
| TNM stage | 0.932 | |||
| IV | 1.016 (0.700, 1.475) | |||
| III | ||||
| Location | 0.941 | |||
| Peripheral | 0.941 (0.619, 1.430) | |||
| Central | ||||
| VEGF (pg/mL) | 0.0494 | 0.024 | ||
| >280 | 1.539 (1.001, 2.365) | 1.600 (1.063, 2.408) | ||
| ≤280 | ||||
| PLT (×109/L) | 0.4046 | |||
| >300 | 0.815 (0.503, 1.319) | |||
| ≤300 | ||||
| VEGFPLT (×10−6 pg) | 0.1288 | |||
| >0.55 | 1.326 (0.921, 1.909) | |||
| ≤ 0.55 | ||||
| ΔVEGFPLT | 0.7380 | |||
| >0.005 | 1.064 (0.738, 1.534) | |||
| ≤ 0.005 | ||||
| CR + PR (pg/mL) | 0.7390 | |||
| VEGF >280 | 1.112 (0.596, 2.074) | |||
| VEGF ≤280 | ||||
| SD + PD (pg/mL) | 0.0310 | 0.0224 | ||
| VEGF >280 | 1.935 (1.062, 3.527) | 2.087 (1.110, 3.926) | ||
| VEGF ≤280 | ||||
Note:
Adjusted for age and sex.
Abbreviations: ΔVEGFPLT, the minus value of VEGFPLT before the first cycle minus the value after the chemotherapy; CI, confidence interval; CR, complete response; HR, hazard ratio; NSCLC, non-small cell lung cancer; PD, progressive disease; PLT, platelets; PR, partial response; SD, stable disease; TNM, tumor node metastasis; VEGF, vascular endothelial growth factor; VEGFPLT, VEGF load per platelet.
Figure 1.
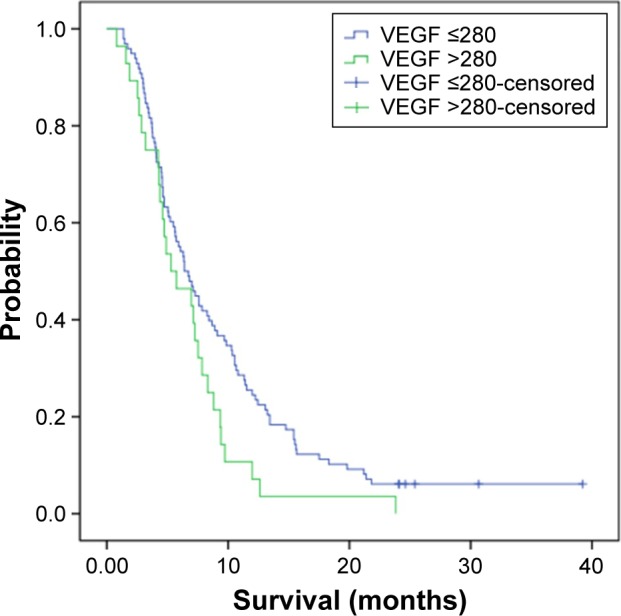
Progression-free survival with high (≥280 pg/mL) and low (<280 pg/mL) pretreatment serum VEGF levels, respectively.
Note: Hazard ratio (high versus low) =1.60 (95% CI, 1.063–2.408), P=0.024.
Abbreviations: CI, confidence interval; VEGF, vascular endothelial growth factor.
Discussion
Neoangiogenesis is critical in tumor growth and systemic dissemination of cancer cells14 and may be related to poor survival among NSCLC patients.15 Studies showed that the presence of neoangiogenesis is a significantly negative prognostic factor for both overall and disease-free survival in lung cancer.9,16–18 Compared with the immunohistochemical evaluation of angiogenic factors in tumor tissues, assessing these angiogenic factors in blood has theoretical advantages: more available, cheaper, faster, more readily performed preoperatively, easier to serially repeat, and less biased.19
Angiogenic factors secreted by tumor cells stimulate endothelial cells to proliferate and form new blood vessels. Among these factors, VEGF is the most important mediator20 because it regulates endothelial sprouting, increases vessel permeability, and contributes to the mobilization and recruitment of bone marrow-derived hematopoietic and endothelial progenitor cells to tumors.21 Being a good reflector of tumor angiogenic activity, circulating VEGF levels have been related to patient tumor burden.22
Although VEGF in the serum may originate from the tumor itself, it could come from peripheral blood cells as well, especially platelets. A significant positive correlation between serum VEGF and platelet counts was reported in several types of malignancies, including NSCLC.23 However, in this study, we failed to detect an association. Research showed that besides platelets, serum VEGF may come from malignant cells, leukocytes, and other cell types, and this may have contributed to the inconsistent results regarding the relationship between the serum VEGF level and the platelet count.24 Moreover, different sample processing methods may have led to the inconsistencies.
The predictive role of VEGF for chemotherapeutic response in NSCLC was investigated with conflicting results.
Regarding platinum-based chemotherapy, Fu et al reported that VEGFPLT levels in the gemcitabine plus cisplatin-sensitive group decreased sharply after chemotherapy, but showed opposite results in the gemcitabine plus cisplatin-resistant group, indicating that VEGFPLT levels can be used as surrogate biomarkers to determine chemotherapeutic response in NSCLC.12 By contrast, Yazar et al concluded that VEGF is not useful as a predictive and prognostic markers in advanced NSCLC patients treated with cisplatin-containing chemotherapy.7,8 Similarly, Ludovini et al concluded that VEGF expression in cancerous tissues is not associated with chemotherapeutic response and overall survival (OS) in advanced NSCLC patients.25 Moreover, we found no significant correlation between the baseline serum VEGF levels and the efficacy of cisplatin-based combination chemotherapy. Furthermore, serum VEGF levels between pre- and post-treatment groups were not significantly different. The decrease in VEGF levels in responders may be due to the effect of cytotoxic drugs on tumor cells by killing them, thereby decreasing the number of cells that synthesize and secrete various angiogenic proteins, including VEGF.26 However, certain chemotherapeutic agents may exert antiangiogenic effects by affecting endothelial cells, thereby increasing the mobilization of circulating endothelial progenitor cells, again promoting tumor angiogenesis. Furthermore, as a response to chemotherapy, VEGF produced by tumor cells can increase. All of these may increase VEGF concentrations, even in patients with response effects.27 However, inconsistencies of the results prompt further study. Furthermore, different histological types, stages, treatment strategies, and sample processes may account for the disparities.
VEGF overexpression in NSCLC is correlated with neoangiogenesis and poor prognosis,28 and increased VEGF levels upon NSCLC diagnosis may predict poor survival.29 Herein lay the controversial reports concerning the VEGF impact on NSCLC patient prognosis. Jantus-Lewintre et al observed that time to tumor progression (TTP) and OS were not significantly associated with plasma VEGF-A concentrations in NSCLC patients treated with cisplatin plus docetaxel, although patients with higher pretreatment VEGF-A levels tend to have shorter TTP and OS.30 Chakra et al also studied 451 NSCLC patients receiving conventional treatments and found that the prognostic information from the high circulating VEGF serum level is not an independent determinant of survival in NSCLC.31 In contrast, Brattström et al concluded that in NSCLC patients with normal platelet counts, VEGF levels after radiotherapy significantly correlated to good prognosis (P=0.023); however, VEGF levels during radiotherapy indicated the same correlation (P=0.085), indicating that serum VEGF is of clinical interest as a prognostic factor.32 Moreover, Lissoni et al reported that the chemotherapeutic response was worse in patients with higher levels of pretreatment VEGF in patients of NSCLC and colorectal carcinoma.9 In this study, patients with higher VEGF levels (≥280 pg/mL) had shorter PFS (median, 5.29 months; 95% CI, 2.293–8.186 months) compared with those with lower VEGF levels (median, 6.407 months; 95% CI, 5.068–7.745 months). The discrepancy between our study results and those of previous studies regarding survival might be partially due to the differences among the assay methods, heterogeneity of study populations, different chemotherapy regimens, and sample size. Different from most of the previous studies using a traditional ELISA as a testing measure, we performed our examination using the Luminex multiplex assay through which we previously found that VEGF levels in NSCLC patients at stages III and IV were higher than those with at stages I and II.11 Limitations of this study should be considered including its retrospective feature. Moreover, the PC regimen was administrated only among patients with pathological type of adenocarcinoma and may have resulted in statistical bias. Therefore, a large-scale prospective validation study is needed to testify the value of VEGF as a biomarker in platinum-based chemotherapy.
Conclusion
The findings of this study imply that pretreatment serum VEGF levels may be a potential prognostic biomarker for the anti-tumor efficacy of platinum-based chemotherapy in terms of PFS. However, VEGF was not a useful marker to anticipate the response to chemotherapy in patients with advanced NSCLC. It needs further investigation to verify the prognostic implications of serum VEGF in NSCLC patients.
Acknowledgments
The authors thank all the enrolled patients who contributed to the study and Fei Deng, Haixia Cao, and Rong Ma for data acquisition and technical support for this research. This work was supported, in part, by the National Nature Science Foundation of China (number 81372396).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Azzoli CG, Baker S, Jr, Temin S, et al. American Society of Clinical Oncology Clinical Practice Guideline update on chemotherapy for stage IV non-small-cell lung cancer. J Clin Oncol. 2009;27(36):6251–6266. doi: 10.1200/JCO.2009.23.5622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–2550. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 4.Ferrara N. Role of vascular endothelial growth factor in the regulation of angiogenesis. Kidney Int. 1999;56(3):794–814. doi: 10.1046/j.1523-1755.1999.00610.x. [DOI] [PubMed] [Google Scholar]
- 5.Thurston G, Kitajewski J. VEGF and Delta-Notch: interacting signalling pathways in tumour angiogenesis. Br J Cancer. 2008;99(8):1204–1209. doi: 10.1038/sj.bjc.6604484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kondo S, Asano M, Matsuo K, Ohmori I, Suzuki H. Vascular endothelial growth factor/vascular permeability factor is detectable in the sera of tumor-bearing mice and cancer patients. Biochim Biophys Acta. 1994;1221(2):211–214. doi: 10.1016/0167-4889(94)90016-7. [DOI] [PubMed] [Google Scholar]
- 7.Tas F, Duranyildiz D, Oguz H, Camlica H, Yasasever V, Topuz E. Serum vascular endothelial growth factor (VEGF) and bcl-2 levels in advanced stage non-small cell lung cancer. Cancer Invest. 2006;24(6):576–580. doi: 10.1080/07357900600894781. [DOI] [PubMed] [Google Scholar]
- 8.Yazar A, Soydinc H, Ertan E, Yasasever V, Tas F. The role of serum vascular endothelial growth factor and matrix metalloproteinase-9 in predicting response to chemotherapy in patients with advanced nonsmall cell lung cancer. South Med J. 2008;101(3):327–328. doi: 10.1097/SMJ.0b013e318164e432. [DOI] [PubMed] [Google Scholar]
- 9.Lissoni P, Rovelli F, Malugani F, Brivio F, Fumagalli L, Gardani GS. Changes in circulating VEGF levels in relation to clinical response during chemotherapy for metastatic cancer. Int J Biol Markers. 2003;18(2):152–155. doi: 10.1177/172460080301800209. [DOI] [PubMed] [Google Scholar]
- 10.Hsu HY, Joos TO, Koga H. Multiplex microsphere-based flow cytometric platforms for protein analysis and their application in clinical proteomics – from assays to results. Electrophoresis. 2009;30(23):4008–4019. doi: 10.1002/elps.200900211. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Y, Wu JZ, Zhang JY, et al. Detection of circulating vascular endothelial growth factor and matrix metalloproteinase-9 in non-small cell lung cancer using Luminex multiplex technology. Oncol Lett. 2014;7(2):499–506. doi: 10.3892/ol.2013.1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fu BH, Fu ZZ, Meng W, Gu T, Sun XD, Zhang Z. Platelet VEGF and serum TGF-beta1 levels predict chemotherapy response in non-small cell lung cancer patients. Tumour Biol. 2015;36(8):6477–6483. doi: 10.1007/s13277-015-3338-x. [DOI] [PubMed] [Google Scholar]
- 13.Bambace NM, Levis JE, Holmes CE. The effect of P2Y-mediated platelet activation on the release of VEGF and endostatin from platelets. Platelets. 2010;21(2):85–93. doi: 10.3109/09537100903470298. [DOI] [PubMed] [Google Scholar]
- 14.Foekens JA, Peters HA, Grebenchtchikov N, et al. High tumor levels of vascular endothelial growth factor predict poor response to systemic therapy in advanced breast cancer. Cancer Res. 2001;61(14):5407–5414. [PubMed] [Google Scholar]
- 15.Han H, Silverman JF, Santucci TS, et al. Vascular endothelial growth factor expression in stage I non-small cell lung cancer correlates with neoangiogenesis and a poor prognosis. Ann Surg Oncol. 2001;8(1):72–79. doi: 10.1007/s10434-001-0072-y. [DOI] [PubMed] [Google Scholar]
- 16.Yano T, Tanikawa S, Fujie T, Masutani M, Horie T. Vascular endothelial growth factor expression and neovascularisation in non-small cell lung cancer. Eur J Cancer. 2000;36(5):601–609. doi: 10.1016/s0959-8049(99)00327-5. [DOI] [PubMed] [Google Scholar]
- 17.Offersen BV, Pfeiffer P, Hamilton-Dutoit S, Overgaard J. Patterns of angiogenesis in nonsmall-cell lung carcinoma. Cancer. 2001;91(8):1500–1509. [PubMed] [Google Scholar]
- 18.Fontanini G, Vignati S, Lucchi M, et al. Neoangiogenesis and p53 protein in lung cancer: their prognostic role and their relation with vascular endothelial growth factor (VEGF) expression. Br J Cancer. 1997;75(9):1295–1301. doi: 10.1038/bjc.1997.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bremnes RM, Camps C, Sirera R. Angiogenesis in non-small cell lung cancer: the prognostic impact of neoangiogenesis and the cytokines VEGF and bFGF in tumours and blood. Lung Cancer. 2006;51(2):143–158. doi: 10.1016/j.lungcan.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Roskoski R., Jr Vascular endothelial growth factor (VEGF) signaling in tumor progression. Crit Rev Oncol Hematol. 2007;62(3):179–213. doi: 10.1016/j.critrevonc.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Grunewald M, Avraham I, Dor Y, et al. VEGF-induced adult neovascularization: recruitment, retention, and role of accessory cells. Cell. 2006;124(1):175–189. doi: 10.1016/j.cell.2005.10.036. [DOI] [PubMed] [Google Scholar]
- 22.Brattstrom D, Bergqvist M, Hesselius P, et al. Elevated preoperative serum levels of angiogenic cytokines correlate to larger primary tumours and poorer survival in non-small cell lung cancer patients. Lung Cancer. 2002;37(1):57–63. doi: 10.1016/s0169-5002(02)00027-2. [DOI] [PubMed] [Google Scholar]
- 23.Choi JH, Kim HC, Lim HY, et al. Vascular endothelial growth factor in the serum of patients with non-small cell lung cancer: correlation with platelet and leukocyte counts. Lung Cancer. 2001;33(2–3):171–179. doi: 10.1016/s0169-5002(01)00200-8. [DOI] [PubMed] [Google Scholar]
- 24.Salgado R, Vermeulen PB, Benoy I, et al. Platelet number and interleukin-6 correlate with VEGF but not with bFGF serum levels of advanced cancer patients. Br J Cancer. 1999;80(5–6):892–897. doi: 10.1038/sj.bjc.6690437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ludovini V, Gregorc V, Pistola L, et al. Vascular endothelial growth factor, p53, Rb, Bcl-2 expression and response to chemotherapy in advanced non-small cell lung cancer. Lung Cancer. 2004;46(1):77–85. doi: 10.1016/j.lungcan.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 26.Kumar S, Guleria R, Singh V, Bharti AC, Mohan A, Das BC. Efficacy of plasma vascular endothelial growth factor in monitoring first-line chemotherapy in patients with advanced non-small cell lung cancer. BMC Cancer. 2009;9:421. doi: 10.1186/1471-2407-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arjaans M, Schroder CP, Oosting SF, Dafni U, Kleibeuker JE, de Vries EG. VEGF pathway targeting agents, vessel normalization and tumor drug uptake: from bench to bedside. Oncotarget. 2016;7(16):21247–21258. doi: 10.18632/oncotarget.6918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Delmotte P, Martin B, Paesmans M, et al. VEGF and survival of patients with lung cancer: a systematic literature review and meta-analysis. Rev Mal Respir. 2002;19(5 Pt 1):577–584. French. [PubMed] [Google Scholar]
- 29.Dudek AZ, Mahaseth H. Circulating angiogenic cytokines in patients with advanced non-small cell lung cancer: correlation with treatment response and survival. Cancer Invest. 2005;23(3):193–200. doi: 10.1081/cnv-200055949. [DOI] [PubMed] [Google Scholar]
- 30.Jantus-Lewintre E, Sanmartin E, Sirera R, et al. Combined VEGF-A and VEGFR-2 concentrations in plasma: diagnostic and prognostic implications in patients with advanced NSCLC. Lung Cancer. 2011;74(2):326–331. doi: 10.1016/j.lungcan.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 31.Chakra M, Pujol JL, Lamy PJ, et al. Circulating serum vascular endothelial growth factor is not a prognostic factor of non-small cell lung cancer. J Thorac Oncol. 2008;3(10):1119–1126. doi: 10.1097/JTO.0b013e318187464e. [DOI] [PubMed] [Google Scholar]
- 32.Brattström D, Bergqvist M, Hesselius P, Larsson A, Wagenius G, Brodin O. Serum VEGF and bFGF adds prognostic information in patients with normal platelet counts when sampled before, during and after treatment for locally advanced non-small cell lung cancer. Lung Cancer. 2004;43(1):55–62. doi: 10.1016/j.lungcan.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]


