Abstract
IMPORTANCE
Exposure to violence continues to be a growing epidemic, particularly among children. An enhanced understanding of the biological effect of exposure to violence is critical.
OBJECTIVE
To examine the association between neighborhood violence and cellular and biological stress in children.
DESIGN, SETTING, AND PARTICIPANTS
A matched, cross-sectional study of 85 black children aged 5 to 16 years from 52 neighborhoods took place in the greater New Orleans, Louisiana, area between January 1, 2012, and July 31, 2013.
EXPOSURES
Density of businesses where individuals can purchase alcohol as measured by rates per capita of liquor or convenience stores, and violence as measured by reports of violent crime and reports of domestic violence, operationalized as reports per capita of crime and domestic violence. Rates of exposure within a 500-, 1000-, and 2000-m radius from the child’s home were calculated.
MAIN OUTCOMES AND MEASURES
Primary biological outcomes were telomere length and cortisol functioning.
RESULTS
Among the 85 children in the study, (mean [SD] age, 9.8 [3.1] years; 50 girls and 35 boys) significant variation in telomere length and cortisol functioning was observed at the neighborhood level, with intraclass correlation coefficients of 6% for telomere length, 3.4% for waking cortisol levels, and 5.5% for peak cortisol levels following a stressor. Density of liquor or convenience stores within a 500-m radius of a child’s home was associated with a decrease in mean telomere length by 0.004 for each additional liquor store or convenience store (β [SE], −0.004 [0.002]; P = .02). The rate of domestic violence was significantly and inversely associated with a decrease in mean telomere length by 0.007 for each additional report of domestic violence in a 500-m radius of a child’s home (β [SE], −0.007 [0.001]; P < .001). The rate of violent crime was significantly associated with a decrease in mean telomere length by 0.006 for each additional report of violent crime in a 500-m radius of a child’s home (β [SE], −0.006 [0.002]; P < .001). Children exposed to more liquor and convenience stores within 500 m of their home were significantly less likely to reduce cortisol levels after a reactivity test (β, 0.029; P = .047), as were children exposed to high rates of domestic violence (β, 0.088; P = .12) and violent crime (β. 0.029; P = .006). Children exposed to more liquor and convenience stores within 500 m of their home had a steeper diurnal decline in cortisol levels during the day (β [SE], −0.002 [0.001]; P = .04), as did children exposed to more violent crime within 500 m of their home (β [SE] −0.032 [0.014]; P = .02).
CONCLUSIONS AND RELEVANCE
Neighborhoods are important targets for interventions to reduce the effect of exposure to violence in the lives of children. These findings provide the first evidence that objective exposures to neighborhood-level violence influence both physiological and cellular markers of stress, even in children.
Before the age of 18 years, approximately two-thirds of children are exposed to multiple types of violence.1 A greater understanding of the effect on children’s health owing to exposure to violence across socioecological contexts is critical, as differential exposure to social environmental conditions likely contributes mechanistically to health disparities.2,3 Socioeconomically disadvantaged communities have higher exposure to violence, suggesting that the effects of such exposure also may be accentuated.1,4 Exposure to violence may create persistent biological effects across multiple stress response systems (SRS), resulting in lasting physiological and psychological vulnerability.5,6 There has been limited information on racial and socioeconomic differences in biological stress and antecedent factors among children,7 and few studies have examined within-race or socioeconomic differences in biological stress.
Violence may play a key role in mechanisms that lead to shorter-term biological changes and long-term health outcomes; this finding helped motivate the inclusion of exposure to violence in the self-reported Adverse Childhood Experiences scale.8 Children’s exposure to violence has been linked to altered biological responses across many SRS, suggesting mechanistic roles in negative health effects.9 In adults and youths, exposure to violence has been associated with lower telomere length (TL) and greater attrition of TL.10–12 As one of the most frequently investigated biomarkers and a primary allostatic mediator,13,14 the hypothalamic-pituitary-adrenal (HPA) axis is shaped by the individual’s social context, with both low and high cortisol levels as biological alterations resulting from early adversity.15 These alterations may be adaptations to the individual’s circumstances, but may not be desirable or may come at a high cost to long-term health.16
To separate perceived exposure to violence from objective exposure, the assessment of cross-contextual violence requires the use of objective measures.17 We examined the links between cortisol levels and TL in children and the rate of violent crime, an established objective marker of neighborhood violence, as well as 2 closely linked unique neighborhood-level exposures: density of locations where individuals can purchase alcohol and the rate of reports of domestic violence (DV) at the neighborhood level. Density of businesses where individuals can purchase alcohol, particularly those where alcohol is purchased and consumed off-site (ie, liquor or convenience stores), is associated with neighborhood crime and assaults,18,19 and has been associated with many health and social outcomes as well as neighborhood DV.20,21 Therefore, we tested the direct association between cortisol response and TL in children and neighborhood density of businesses where individuals can purchase alcohol, neighborhood rates of DV reports, and neighborhood rates of violent crime, as well as indirect pathways of witnessing violence in the neighborhood and DV and fighting in the home.
Methods
Participants
Children aged 5 to 16 years and their families from New Orleans, Louisiana, were recruited using street outreach techniques between January 1, 2012, and July 31, 2013. Participants were geographically linked to their census tract and located in 51 of 177 census tracts.
Mothers provided data about multiple levels of their children’s social ecology using an interviewer-assisted computer survey (Nova Research) administered face-to-face at the research site. Written informed consent was obtained from caregivers and assent obtained from children older than 8 years. This study was approved by the Tulane University Health Sciences Center Institutional Review Board.
Given the outcomes examined, potential structural confounding, and the importance of age, children were matched 3:1 (with replacement) on age within 1 year, exposure to Hurricane Katrina in 2005, and the propensity (with a caliber of 0.05) of living in a neighborhood with a high level of violence. The final matched sample included 85 black children.
Measures
Both primary and secondary data were included and a multilevel data system was created of children nested within their household and neighborhoods. Neighborhood was defined as geographic buffers around the child’s home as well as a US census tract.
The primary outcomes of interest were TL and salivary acute and diurnal cortisol levels. The mean relative TL, as represented by the telomere to single copy gene ratio, was determined by monochromic multiplex quantitative polymerase chain reaction from extracted DNA. Measures were performed in triplicate and duplicated on a second plate. The mean of the 6 replicates was used to calculate TL. Two samples with high coefficients of variation (10% intra-assay and 6% interassay) were removed.
Each participant provided 11 saliva samples. Cortisol reactivity was assessed using the Trier Social Stressor Test for Children (TSST-C), a validated test of psychosocial stressors for youth.22 The TSST-C was administered in the early afternoon (mean 2:03 PM) to minimize diurnal influences.23 Saliva was collected a mean of 39 minutes after arrival,24 and then twice after the TSST-C was performed (mean, 23 and 85 minutes after the TSST-C) to capture the peak level of cortisol after the TSST-C, as well as cortisol reactivity and recovery. Participants also provided diurnal saliva samples on 2 separate days: on awakening, 30 minutes later to capture the cortisol awakening response, in the early afternoon, and at bedtime. Cortisol was measured in saliva via passive drool and stored in freezers. Samples were assayed using a commercially available validated enzyme immunoassay (Salimetrics). Samples were assayed in duplicate; those varying more than 7% were reassayed. Cortisol levels were log-transformed.
The primary exposures of interest were density of liquor and convenience stores, neighborhood rate of reports of DV, and neighborhood rate of violent crime. Density of liquor and convenience stores was measured within a 500-, 1000-, and 2000-m radius of each child’s residence. The density per census tract and distance to the nearest liquor store or convenience store from the child’s home were also calculated and compared for consistency. Counts of alcohol licenses were obtained from the Louisiana Department Alcohol and Tobacco Control.
The rate of reports of DV per meter radius and per capita within a census tract was calculated by analyzing 911 call data from the city of New Orleans, via the method used by Capowich and Kondkar,25 whereby calls are analyzed for DV events. Each call was linked to an address so that calls could be geographically linked and measured as calls within the same 500-, 1000-, and 2000-m radius around the child’s home.
The rate of neighborhood violent crime was calculated with data from the police department with address information for each type of substantiated crime, calculated as the number of homicide and assault (including rape) crimes within the same meter radius of each child’s residence.
Potential mediators included witnessing DV, fighting, and neighborhood violence. Witnessing violence in the neighborhood and home was measured by items adapted from the minor and major life events from the Preschool Age Psychiatric Assessment,26 including witnessing physical or verbal fighting at home, DV, and violence in the community. Key covariates or potential confounders included the following sociodemographics: child sex, maternal age, maternal educational level, prenatal maternal smoking, exposure to smoking in the home, exposure to alcohol in the home, and immediate neighborhood.
Statistical Analysis
Univariate, bivariate, and multivariable analyses were performed using SAS, version 9.2 (SAS Institute Inc), including PROC MIXED, to take into account neighborhood clustering, multiple children per household, and conditioning on matched stratum. Thirteen enrolled families (15%) had more than 1 child participate (range, 1–5). Mixed models were used for partitioning variance estimates at all levels, expressed as the intraclass correlation coefficient. Modeling was performed in the following steps: (1) examination of empty models to determine the extent of clustering of TL and cortisol values by neighborhood, (2) testing the unadjusted associations between the neighborhood violence environments and stress markers, (3) testing the adjusted association after accounting for potential confounders, and (4) testing potential mediation. Mixed models for repeated measures of cortisol over time accounted for within-individual correlation within the levels of child, matched stratum, and neighborhood. All models compared use of alcohol and rates of violence at different radii around the child’s home, as well as with distance and tract-level exposures. Potential mediation by reported witnessing of violence at home and in the neighborhood was calculated separately, using the SAS MEDIATE macro.27
Results
Characteristics of the sample are presented in Table 1. Thirty children (35%) had witnessed DV in the home and 31 (37%) had witnessed violence in the neighborhood. Children living in neighborhoods were more likely to witness DV and neighborhood violence.
Table 1.
Characteristics of Matched Sample by Neighborhood Alcohol Environment
| Characteristic | Valuea | ||
|---|---|---|---|
| Total (N = 85) | High Liquor and Convenience Stores (≥75th Percentile) (n = 22) | Lower Liquor and Convenience Stores (<75th Percentile) (n = 63) | |
| Sex of child | |||
| Male | 35 (41.2) | 11 (50.0) | 24 (38.1) |
| Female | 50 (58.8) | 11 (50.0) | 39 (61.9) |
| Age of child, y | |||
| ≤6 | 13 (15.3) | 3 (13.6) | 10 (15.9) |
| 7–9 | 37 (43.5) | 10 (45.5) | 27 (42.8) |
| ≥10 | 35 (41.2) | 9 (40.9) | 26 (41.3) |
| Age of caregiver, yb | |||
| 18–29 | 17 (20.2) | 4 (19.1) | 13 (20.6) |
| 30–39 | 52 (61.9) | 9 (47.6) | 42 (66.7) |
| ≥40 | 15 (17.8) | 7 (33.3) | 8 (12.7) |
| Mother’s educational level | |||
| Less than high school | 20 (23.5) | 9 (40.9) | 11 (17.5) |
| High school degree or GED | 24 (28.2) | 6 (27.3) | 18 (28.6) |
| Some college or more | 41 (48.3) | 7 (31.8) | 34 (53.9) |
| Smoking during pregnancyb | 10 (11.8) | 5 (22.7) | 5 (7.9) |
| Smoke exposure in the homec | 18 (21.2) | 8 (36.4) | 10 (15.9) |
| Caregiver drank alcohol in the last monthb | 31 (36.5) | 9 (40.0) | 20 (31.8) |
| Alcohol use in the homec | 37 (43.5) | 12 (54.6) | 25 (39.7) |
| Seen neighbors drinking outside | 44 (51.7) | 12 (54.6) | 32 (50.6) |
| Caregiver drinks in the last month, mean (SD), No. | 3.0 (2.79) | 2.62 (1.60) | 2.27 (3.41) |
| Drinking frequency of individuals in the child’s home in the last 12 mo, mean (SD)b,d | 1.9 (2.4) | 2.4 (2.7) | 1.7 (2.3) |
| Children witnessed domestic violence in homec | 30 (34.8) | 9 (42.3) | 20 (31.7) |
| Children witnessed violence in the neighborhood | 31 (36.7) | 9 (40.7) | 22 (34.9) |
| Telomere length, mean (SD), T/S ratioc | 1.5 (0.1) | 1.1 (0.2) | 1.6 (0.5) |
| Diurnal cortisol, mean (SD), μg/dL | 2.9 (1.1) | 3.0 (1.0) | 2.9 (1.1) |
| Acute cortisol, mean (SD), μg/dL | 2.8 (0.6) | 2.8 (0.6) | 2.7 (0.5) |
| Liquor or convenience stores per 500 m, mean (SD), No.c | 2.4 (2.7) | 6.1 (1.5) | 1.1 (1.2) |
| Reports of domestic violence per 500 m, mean (SD), No.c | 77.8 (51.2) | 112.5 (95.0) | 65.7 (49.5) |
| Assault rate per 500 m, mean (SD), No.c | 8.3 (7.9) | 16.3 (7.6) | 4.9 (5.3) |
| Homicide rate per 500 m, mean (SD), No.c | 1.1 (1.5) | 2.2 (1.7) | 0.6 (1.0) |
Abbreviations: GED, General Educational Development certificate; T/S, telomere to single copy gene.
SI conversion factor: To convert contisol to nanomoles per liter, multiply by 27.588.
Data are presented as number (percentage) of patients unless otherwise indicated. Percentages and estimates based on nonmissing data (<5% were missing across all variables).
P < .10.
P < .05.
Response choices were on a scale of 0 to 7, as follows: 0, at least once per day; 1, nearly every day; 2, three or four times per week; 3, once or twice per week; 4, two or three times per month; 5, about once per month; 6, less than once per month but at least once per year; 7, none in the last 12 months.
Telomere Length
In empty models, not considering any covariates, we observed substantial clustering of TL, with 10% of the variance in TL explained at the household level (intraclass correlation coefficient, 10%) and 6% of the variance in TL explained at the census tract or neighborhood level. Table 2 shows results of multivariable analysis depicting the direct effect of neighborhood liquor and convenience stores, rates of DV, and rates of violent crime on TL, separately. Even after adjusting for potential confounders, the number of liquor and convenience stores within a 500-m radius of a child’s home remained associated with TL, with a decrease in mean TL by 0.004 for each additional liquor store or convenience store (β [SE], −0.004 [0.002]; P = .02) (Table 2). Considering only bivariate association, the number of liquor and convenience stores explained 3.5% of the variance (R2 = 3.5%) in TL and a further 4.7% was explained by additional covariates (R2 = 8.2%). Results were nearly identical for alcohol exposure within a 500-m radius.
Table 2.
Effect of Neighborhood Violence on Telomere Lengtha
| Characteristic | β (SE) | P Value |
|---|---|---|
| Direct effect of liquor or convenience storesb | ||
| Intercept | 1.45 (0.013) | <.001 |
| Liquor or convenience stores within 500 m | −0.004 (0.002) | .02 |
| Child sex, female vs male | 0.080 (0.004) | <.001 |
| Maternal age, y | 0.0003 (0.0004) | .56 |
| Maternal educational level, ordinal | −0.002 (0.002) | .29 |
| Prenatal smoke exposure | −0.004 (0.006) | .56 |
| Current smoking in child’s home | −0.006 (0.006) | .32 |
| Child witnessed neighborhood violence | −0.003 (0.004) | .42 |
| R2, % | 8.2 | |
| Direct effect of neighborhood domestic violence | ||
| Intercept | 1.46 (0.014) | <.001 |
| Domestic violence reports within 500 m | −0.007 (0.001) | <.001 |
| Child sex, female vs male | 0.081 (0.004) | <.001 |
| Maternal age, years | 0.0003 (0.001) | .50 |
| Maternal educational level, ordinal | −0.002 (0.002) | .37 |
| Prenatal smoke exposure | −0.005 (0.006) | .36 |
| Current smoking in child’s home | −0.007 (0.006) | .26 |
| Child witnessed neighborhood violence | −0.025 (0.004) | .53 |
| R2, % | 6.7 | |
| Direct effect of neighborhood violent crime | ||
| Intercept | 1.45 (0.014) | <.001 |
| Violent crimes within 500 m | −0.006 (0.002) | <.001 |
| Child sex, female vs male | 0.082 (0.003) | <.001 |
| Maternal age, years | 0.0004 (0.001) | .43 |
| Maternal educational level, ordinal | −0.002 (0.002) | .48 |
| Prenatal smoke exposure | −0.002 (0.005) | .73 |
| Current smoking in child’s home | −0.006 (0.005) | .28 |
| Child witnessed neighborhood violence | −0.003 (0.002) | .42 |
| R2, % | 5.9 | |
Telomere length reported as telomere to single copy gene ratio.
Natural indirect effect, −0.099 (95% CI, −0.037 to −0.217): the proportion of the effect of liquor or convenience stores on telomere length that acts through witnessing domestic violence.
The rate of reports of DV remained significantly and inversely associated with TL after adjusting for several potential confounders, with a decrease in mean TL by 0.007 for each additional report in a 500-m radius (β [SE], −0.007 [0.001]; P < .001) (Table 2). Considering only the bivariate association, the rate of reports of DV explained 2.8% of the variance (R2 = 2.8%) in TL and a further 3.9% was explained by including additional covariates (R2 = 6.7%). Results were nearly identical for reports of DV within a 1000- and 2000-m radius.
The rate of violent crime remained significantly associated with TL after adjusting for several potential confounders, with a decrease in mean TL by 0.006 for each additional report in a 500-m radius (β [SE], −0.006 [0.002]; P < .001) (Table 2). Considering only the bivariate association, violent crime rate explained 2.8% of the variance (R2 = 1.6%) in TL and an additional 4.3% was explained by additional covariates (R2 = 5.9%). Findings were similar for violent crime exposure within a 1000- and 2000-m radius.
Subjective report of the child witnessing violence in the neighborhood was controlled for. Models run with witnessing DV in the home returned similar results. Mediation between the neighborhood exposures and caregiver report of the child’s witnessing DV and community violence were examined, but a significant indirect effect emerged only for the association between number of liquor and convenience stores and TL with mediation by witnessing DV (natural indirect effect, −0.099; 95% CI, −0.037 to −0.217) (Table 2).
Acute Cortisol Reactivity
Approximately 5.5% of the variance in mean acute cortisol level was explained at the neighborhood level, illustrating a substantial amount of clustering at this level. Empty models captured 3 cortisol measures simultaneously within the same model. Peak individual cortisol level was the intercept (β, 2.808; P = .001). Cortisol reactivity was captured as the time (in minutes) leading to the peak cortisol level (β, 0.030; P = .05), with higher values indicating a steeper rise from before the TSST-C to the peak level. Cortisol recovery was the time (in minutes) from after the peak cortisol level until the end of the study visit (β, −0.037; P = .35), with more negative values indicating a steeper decline in the cortisol level after the stressor. Table 3 depicts the direct effect of neighborhood liquor and convenience stores, rates of DV, and rates of violent crime on acute cortisol levels.39
Table 3.
Effect of Neighborhood Violence on Acute Cortisol Level
| Characteristic | β (SE) | P Value |
|---|---|---|
| Direct effect of liquor or convenience stores | ||
| Intercept | 2.941 (0.241) | .001 |
| Time before peak cortisol level | 0.052 (0.026) | .049 |
| Liquor or convenience stores within 500 m | −0.022 (0.019) | .26 |
| Time before peak cortisol level × liquor or convenience stores | −0.005 (0.005) | .30 |
| Time after peak cortisol level | −0.121 (0.056) | .03 |
| Time after peak cortisol level × liquor or convenience stores | 0.029 (0.014) | .047 |
| Child sex, female vs male | −0.076 (0.099) | .44 |
| Puberty stage, 0–4a | 0.095 (0.042) | .03 |
| Maternal educational level, ordinal | −0.128 (0.066) | .054 |
| Child witnessed neighborhood violence | −0.117 (0.113) | .31 |
| R2, % | 7.0 | |
| Direct effect of neighborhood domestic violence | ||
| Intercept | 3.366 (0.276) | .001 |
| Time before peak cortisol level | −0.092 (0.084) | .28 |
| Domestic violence reports within 500 m | −0.144 (0.078) | .07 |
| Time before peak cortisol level × domestic violence reports | 0.052 (0.037) | .16 |
| Time after peak cortisol level | −0.214 (0.122) | .08 |
| Time after peak cortisol level × domestic violence reports | 0.088 (0.056) | .12 |
| Child sex, female vs male | −0.129 (0.106) | .22 |
| Puberty stage, 0–4a | 0.090 (0.042) | .03 |
| Maternal educational level, ordinal | −0.119 (0.065) | .07 |
| Child witnessed neighborhood violence | −0.092 (0.112) | .40 |
| R2, % | 9.5 | |
| Direct effect of neighborhood violent crime | ||
| Intercept | 3.613 (0.285) | .001 |
| Time before peak cortisol level | 0.093 (0.078) | .24 |
| Violent crimes within 500 m | −0.225 (0.074) | .003 |
| Time before peak cortisol level × violent crimes | −0.031 (0.034) | .36 |
| Time after peak cortisol level | −0.333 (0.056) | .03 |
| Time after peak cortisol level × violent crimes | 0.029 (0.119) | .006 |
| Child sex, female vs male | −0.149 (0.104) | .15 |
| Puberty stage, 0–4a | 0.084 (0.041) | .04 |
| Maternal educational level, ordinal | −0.138 (0.063) | .03 |
| Child witnessed neighborhood violence | −0.099 (0.108) | .36 |
| R2, % | 10.8 | |
Puberty status categorized by maternal-reported Pubertal Development Scale and converted to Tanner stage 1–4.39
We observed a significant effect of density of liquor and convenience stores on cortisol recovery, with children exposed to more liquor and convenience stores within 500 m of their home being significantly less likely to reduce cortisol levels after the TSST-C (β, 0.029; P = .047) (Figure). Neighborhood rate of reports of DV and rate of violent crime also affected children’s response to the TSST-C, with overall blunted cortisol levels and shallow recovery, as noted by interaction between time and exposure, among children living in areas with high rates of DV (β, 0.088; P = .12) and violent crime (β, 0.029; P = .006) (Figure). Results were similar for neighborhood exposures within a 1000-m radius and marginally significant within a 2000-m radius. We did not observe an indirect effect for cortisol recovery by the child’s witnessing DV and community violence.
Figure. Predicted Acute Cortisol Response to the Trier Social Stressor Test for Children (TSST-C) by Neighborhood Exposures.
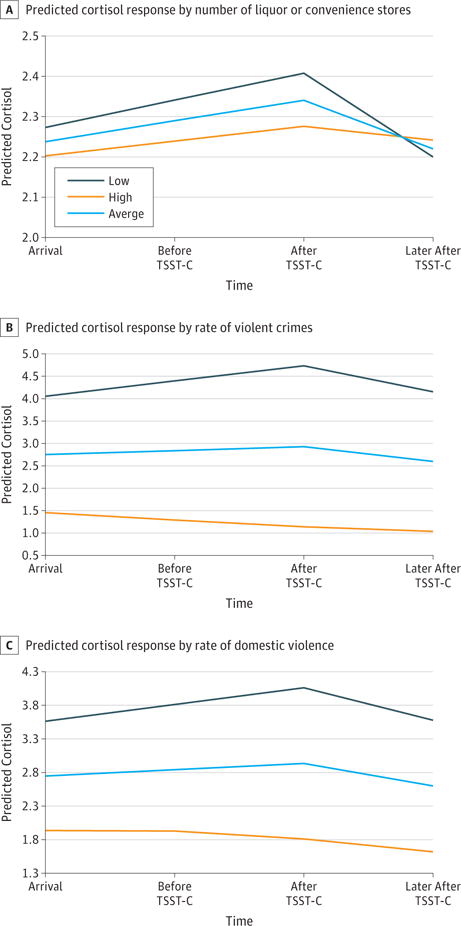
A, Predicted cortisol response by number of liquor and convenience stores. B, Predicted cortisol response by rate of violent crimes. C, Predicted cortisol response by rate of domestic violence. Neighborhood exposures measured within a 500-m radius from child’s home.
Diurnal Rhythm of Cortisol
We also observed moderate clustering of cortisol at the neighborhood level, with approximately 3.4% of the variance in mean diurnal cortisol levels explained at the neighborhood level. Empty models captured waking basal cortisol levels as the intercept (β, 3.1174; P = .001), a cortisol awakening response rise in cortisol within 30 minutes of awakening (β, 0.6752; P = .001), and a diurnal decline in cortisol across the day until bedtime (β, −0.08419; P < .001), which was marginally steeper in the morning than afternoon hours (β, 0.003; P = .14). Multivariable results depicting the direct effect of neighborhood liquor and convenience stores, rates of DV, and rates of violent crime on diurnal cortisol levels, separately, are presented in Table 4.39 We observed a significant effect of density of liquor and convenience stores on mean daily cortisol levels, with children exposed to more liquor and convenience stores within 500 m of their home having a steeper diurnal decline in cortisol levels during the day (β [SE], −0.002 [0.001]; P = .04) (Table 4). Children exposed to more violent crime within 500 m of their home also had a steeper decline in cortisol levels (β [SE] −0.032 [0.014]; P = .02). Results were similar for exposures to neighborhood violence within a 1000-m radius and similar but only marginally significant within a 2000-m radius. We did not observe a significant indirect effect for average cortisol recovery by the child’s witnessing DV and community violence.
Table 4.
Effect of Neighborhood Violence on Diurnal Cortisol Levels
| Characteristic | β (SE) | P Value |
|---|---|---|
| Direct effect of liquor or convenience stores | ||
| Intercept | 3.135 (0.354) | <.001 |
| Time since awakening | −0.075 (0.029) | .01 |
| Time since awakening, squared | 0.004 (0.002) | .06 |
| Cortisol awakening response | 0.621 (0.200) | .06 |
| Liquor or convenience stores within 500 m | 0.010 (0.011) | .36 |
| Time × liquor or convenience stores | −0.002 (0.001) | .04 |
| Child sex, female vs male | −0.114 (0.138) | .41 |
| Puberty stage, 0–4a | 0.064 (0.054) | .24 |
| Maternal educational level, ordinal | −0.064 (0.098) | .51 |
| Child witnessed neighborhood violence | 0.077 (0.167) | .64 |
| Liquor or convenience stores × cortisol awakening response | 0.0005 (0.013) | .97 |
| R2, % | 16.9 | |
| Direct effect of neighborhood domestic violence | ||
| Intercept | 3.150 (0.4337) | <.001 |
| Time since awakening | −0.086 (0.036) | .02 |
| Time since awakening, squared | 0.004 (0.002) | .048 |
| Cortisol awakening response | 0.734 (0.387) | .06 |
| Domestic violence reports within 500 m | 0.044 (0.133) | .74 |
| Time × domestic violence reports | −0.004 (0.011) | .68 |
| Child sex, female vs male | −0.112 (0.137) | .42 |
| Puberty stage, 0–4a | 0.065 (0.054) | .23 |
| Maternal educational level, ordinal | −0.067 (0.097) | .49 |
| Child witnessed neighborhood violence | 0.078 (0.165) | .64 |
| R2, % | 15.5 | |
| Direct effect of neighborhood violent crime | ||
| Intercept | 3.0181 (0.415) | <.001 |
| Time since awakening | −0.045 (0.034) | .19 |
| Time since awakening, squared | 0.004 (0.002) | .05 |
| Cortisol awakening response | 0.573 (0.393) | .15 |
| Violent crimes within 500 m | 0.169 (0.171) | .32 |
| Time × violent crimes | −0.032 (0.014) | .02 |
| Child sex, female vs male | −0.137 (0.150) | .36 |
| Puberty stage, 0–4a | 0.057 (0.057) | .32 |
| Maternal educational level, ordinal | −0.061 (0.086) | .48 |
| Child witnessed neighborhood violence | 0.119 (0.153) | .44 |
| Violent crimes × cortisol awakening response | 0.032 (0.231) | .89 |
| R2, % | 16.9 | |
Puberty status categorized by maternal-reported Pubertal Development Scale and converted to Tanner stage 1–4.39
Discussion
Results indicate that the effect of adverse neighborhood- level factors is measurable at the biological level, even in children. Previous studies have linked violence with other indices of the SRS in children, yet our results are the first, to our knowledge, to examine the role of objective neighborhood environments, including neighborhood liquor and convenience stores, DV, and violent crime across biological stress markers. We observed substantial clustering at the neighborhood level for SRS markers, with significant association between these neighborhood environments and shorter TL, blunted recovery of cortisol levels, and steeper diurnal rhythms. This finding suggests a powerful effect of neighborhood adversity, of which children may not be aware, but which nonetheless has a physiological consequence.
Results are consistent with previous findings that link family violence and shorter TL,10 as well as the findings by Shalev and colleagues.12 Our study extends previous studies by showing that the effects of neighborhood violence operate beyond family-level adversity. The findings on cortisol levels and reactivity help clarify the limited literature on exposure to violence, which found that greater exposure to violence is associated with both heightened reactivity4 and blunted cortisol levels and reactivity.28 In a community sample of children with relatively protracted exposure to violence,4 heightened cortisol functioning is thought to reflect vigilance to potential threats.16 As in other urban populations,28 however, children in our study experienced a wide range of adversity that together culminates in a blunted HPA axis profile. Extant theory does not suggest that this blunted arousal is maladaptive but rather may reflect a biological shielding from chronic danger signals.29
It may seem counterintuitive that we found steeper diurnal rhythms with greater exposure to violence, as early adversity is often linked with flattened diurnal rhythms.30,31 Nonetheless, steeper rhythms have been shown previously within populations exposed to violence,32 particularly within the most at-risk youth. We speculate on 2 possible mechanisms built from the observation that the rhythm was altered in the evening hours when psychosocial effects predominate over genetically mediated influences on the HPA axis.33 First, steep rhythms may exist because youth with more neighborhood violence stay awake later at night in relatively chaotic environments. The evening sample might be provided later when a cortisol level would naturally be closer to its nadir. Second, it may be adaptive for these youth to have blunted cortisol levels across the evening hours, as stressors and unstructured events typically occur at these times. Although speculative, these findings illustrate a blunted HPA axis precisely when youth might need to be physiologically shielded from the stressors occurring in their ecological context.
Exposure to violence has been found to influence the underlying neurobiological pathways associated with threat perception, potentially altering an individual’s response to threat not only when exposed to violence but also on a day-to-day basis.34 In the case of exposure to neighborhood violence, the perpetrator is not necessarily known to the witness nor is the perpetrator the same person in all violent events, triggering an adaptive constant vigilance response leading to a greater biological toll. Furthermore, violence often manifests both inside and outside the home, making it difficult to have a safe haven where one feels buffered from stress. The effect of the neighborhood risk may also minimize any protective effect of neighborhood support.
Contrary to our hypothesis, witnessing violence did not universally mediate the objective association between neighborhood violence and biological stress. This finding is critical for community-based intervention and prevention efforts, as it suggests that the neighborhood may not necessarily operate through the home but rather exerts its own biological effect. The one exception to a direct effect of neighborhood violence was that we did observe an indirect effect wherein liquor and convenience stores operated through witnessing DV in the home in association with TL. Other untested family-level dynamics, such as family structure and parenting behavior, may be present in the lives of these children to affect biological stress.35,36
Limitations
Limitations to our study include the cross-sectional nature and lack of applicability to other demographic groups. We had no information on relevant transgenerational, preconception, prenatal, or early life exposures that may shape the SRS.37 Our neighborhood definitions are based on administrative boundaries and may not truly represent a child’s neighborhood; however, we used a variety of neighborhood exposure metrics for comparison. Furthermore, while some may argue that TL is not a SRS marker, we argue that TL reflects the cellular SRS given its sensitivity to oxidative stress, cellular metabolism, and environmental exposures in addition to correlates of poor health outcomes (2 critical features of an SRS biomarker). It is not a critical feature that the SRS links with cortisol level.38
Conclusions
With persistent exposure to violence in the United States and elsewhere, it is pertinent that we gain a deeper understanding of the role that violence plays in both early development and later health outcomes. As observed in our study, neighborhood violence may play a significant role in the SRS, even above and beyond secondary experiences or witnessing violence within the home and neighborhood. This complex association points to the larger structural forces that shape child development, including neighborhoods as critical arenas influencing child health trajectories, with specific neighborhood conditions that can be successfully targeted for even greater effect on public health.
Key Points.
Question
Could neighborhood violence and associated conditions lead to biological stress in children?
Findings
A matched, cross-sectional study of 85 children examined whether the rate of violent crime in a neighborhood, rate of reports of domestic violence, and density of liquor or convenience stores were associated with telomere length and cortisol functioning. Each neighborhood stressor was significantly associated with biological stress, with greater exposure associated with shorter telomere length, lower acute cortisol levels and blunted recovery, and steeper diurnal cortisol declines.
Meaning
Neighborhoods may be important targets for interventions to reduce the effect of exposure to violence in the lives of children.
Acknowledgments
Funding/Support: This study was supported by grants 1R01ES020447 and P60AA009803-RC5 (Dr Theall) and R21MH094688 and R01MH101533 (Dr Drury) from the National Institutes of Health.
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Theall had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Theall, Shirtcliff, Drury. Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Theall, Shirtcliff, Drury.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Theall, Shirtcliff, Dismukes, Drury.
Obtained funding: Theall, Shirtcliff, Drury.
Administrative, technical, or material support: Theall, Wallace, Drury.
Study supervision: Theall, Drury.
Conflict of Interest Disclosures: None reported.
Additional Contributions: We thank all the participants who agreed to take part in this study.
References
- 1.Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl. 2007;31(1):7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Lee C. Environmental justice: building a unified vision of health and the environment. Environ Health Perspect. 2002;110(suppl 2):141–144. doi: 10.1289/ehp.02110s2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yen IH, Syme SL. The social environment and health. Annu Rev Public Health. 1999;20(1):287–308. doi: 10.1146/annurev.publhealth.20.1.287. [DOI] [PubMed] [Google Scholar]
- 4.Peckins MK, Dockray S, Eckenrode JL, Heaton J, Susman EJ. The longitudinal impact of exposure to violence on cortisol reactivity in adolescents. J Adolesc Health. 2012;51(4):366–372. doi: 10.1016/j.jadohealth.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gunnar MR, Talge NM, Herrera A. Stressor paradigms in developmental studies. Psychoneuroendocrinology. 2009;34(7):953–96. doi: 10.1016/j.psyneuen.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnston-Brooks CH, Lewis MA, Evans GW, Whalen CK. Chronic stress and illness in children. Psychosom Med. 1998;60(5):597–603. doi: 10.1097/00006842-199809000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Needham BL, Fernandez JR, Lin J, Epel ES, Blackburn EH. Socioeconomic status and cell aging in children. Soc Sci Med. 2012;74(12):1948–1951. doi: 10.1016/j.socscimed.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 8.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moffitt TE. Klaus-Grawe 2012 Think Tank. Childhood exposure to violence and lifelong health. Dev Psychopathol. 2013;25(4, pt 2):1619–1634. doi: 10.1017/S0954579413000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drury SS, Mabile E, Brett ZH, et al. The association of telomere length with family violence and disruption. Pediatrics. 2014;134(1):e128–e137. doi: 10.1542/peds.2013-3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tyrka AR, Price LH, Kao H-T, Porton B, Marsella SA, Carpenter LL. Childhood maltreatment and telomere shortening: preliminary support for an effect of early stress on cellular aging. Biol Psychiatry. 2010;67(6):531–534. doi: 10.1016/j.biopsych.2009.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shalev I, Moffitt TE, Sugden K, et al. Exposure to violence during childhood is associated with telomere erosion from 5 to 10 years of age. Mol Psychiatry. 2013;18(5):576–581. doi: 10.1038/mp.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lupien SJ, Ouellet-Morin I, Hupbach A, et al. Beyond the stress concept: allostatic load—a developmental biological and cognitive perspective. In: Cicchetti D, Cohen D, editors. Developmental Psychopathology. 2nd. Hoboken, NJ: John Wiley & Sons; 2006. pp. 578–628. [Google Scholar]
- 14.Skinner ML, Shirtcliff EA, Haggerty KP, Coe CL, Catalano RF. Allostasis model facilitates understanding race differences in the diurnal cortisol rhythm. Dev Psychopathol. 2011;23(4):1167–1186. doi: 10.1017/S095457941100054X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koss KJ, Hostinar CE, Donzella B, Gunnar MR. Social deprivation and the HPA axis in early development. Psychoneuroendocrinology. 2014;50:1–13. doi: 10.1016/j.psyneuen.2014.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Del Giudice M, Ellis BJ, Shirtcliff EA. Making sense of stress: an evolutionary-developmental framework. In: Laviola G, Macri S, editors. Adaptive and Maladaptive Aspects of Developmental Stress. New York, NY: Springer; 2013. pp. 23–44. [Google Scholar]
- 17.Rutter M. Achievements and challenges in the biology of environmental effects. Proc Natl Acad Sci USA. 2012;109(suppl 2):17149–17153. doi: 10.1073/pnas.1121258109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorman DM, Speer PW, Gruenewald PJ, Labouvie EW. Spatial dynamics of alcohol availability, neighborhood structure and violent crime. J Stud Alcohol. 2001;62(5):628–636. doi: 10.15288/jsa.2001.62.628. [DOI] [PubMed] [Google Scholar]
- 19.Scribner R, Cohen D, Kaplan S, Allen SH. Alcohol availability and homicide in New Orleans. J Stud Alcohol. 1999;60(3):310–316. doi: 10.15288/jsa.1999.60.310. [DOI] [PubMed] [Google Scholar]
- 20.Livingston M. Alcohol outlet density and harm: comparing the impacts on violence and chronic harms. Drug Alcohol Rev. 2011;30(5):515–523. doi: 10.1111/j.1465-3362.2010.00251.x. [DOI] [PubMed] [Google Scholar]
- 21.Theall KP, Scribner R, Cohen D, et al. The neighborhood alcohol environment and alcohol-related morbidity. Alcohol Alcohol. 2009;44(5):491–499. doi: 10.1093/alcalc/agp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buske-Kirschbaum A, Jobst S, Wustmans A, Kirschbaum C, Rauh W, Hellhammer D. Attenuated free cortisol response to psychosocial stress in children with atopic dermatitis. Psychosom Med. 1997;59(4):419–426. doi: 10.1097/00006842-199707000-00012. [DOI] [PubMed] [Google Scholar]
- 23.van Eekelen AP, Kerkhof GA, van Amsterdam JG. Circadian variation in cortisol reactivity to an acute stressor. Chronobiol Int. 2003;20(5):863–878. doi: 10.1081/cbi-120024212. [DOI] [PubMed] [Google Scholar]
- 24.Balodis IM, Wynne-Edwards KE, Olmstead MC. The other side of the curve: examining the relationship between pre-stressor physiological responses and stress reactivity. Psychoneuroendocrinology. 2010;35(9):1363–1373. doi: 10.1016/j.psyneuen.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 25.Capowich GE, Kondkar MM. Rebuilding New Orleans neighborhoods after Hurricane Katrina: toward a theory of social structure and cultural creativity. In: Brunsma DL, Overfelt D, Picou JS, editors. The Sociology of Katrina: Perspectives on a Modern Catastrophe. Lanham, MD: Rowman & Littlefield; 2007. pp. 173–190. [Google Scholar]
- 26.Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) J Am Acad Child Adolesc Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 27.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–150. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kliewer W. Violence exposure and cortisol responses in urban youth. Int J Behav Med. 2006;13(2):109–120. doi: 10.1207/s15327558ijbm1302_2. [DOI] [PubMed] [Google Scholar]
- 29.Del Giudice M, Ellis BJ, Shirtcliff EA. The adaptive calibration model of stress responsivity. Neurosci Biobehav Rev. 2011;35(7):1562–1592. doi: 10.1016/j.neubiorev.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dozier M, Manni M, Gordon MK, et al. Foster children’s diurnal production of cortisol. Child Maltreat. 2006;11(2):189–19. doi: 10.1177/1077559505285779. [DOI] [PubMed] [Google Scholar]
- 31.Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology. 2007;32(8–10):892–905. doi: 10.1016/j.psyneuen.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gostisha AJ, Vitacco MJ, Dismukes AR, Brieman C, Merz J, Shirtcliff EA. Beyond physiological hypoarousal: the role of life stress and callous-unemotional traits in incarcerated adolescent males. Horm Behav. 2014;65(5):469–479. doi: 10.1016/j.yhbeh.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Hulle CA, Shirtcliff EA, Lemery-Chalfant K, Goldsmith HH. Genetic and environmental influences on individual differences in cortisol level and circadian rhythm in middle childhood. Horm Behav. 2012;62(1):36–42. doi: 10.1016/j.yhbeh.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LeDoux J. Rethinking the emotional brain. Neuron. 2012;73(4):653–676. doi: 10.1016/j.neuron.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caughy MOB, O’Campo PJ. Neighborhood poverty, social capital, and the cognitive development of African American preschoolers. Am J Community Psychol. 2006;37(1–2):141–154. doi: 10.1007/s10464-005-9001-8. [DOI] [PubMed] [Google Scholar]
- 36.Pachter LM, Auinger P, Palmer R, Weitzman M. Do parenting and the home environment, maternal depression, neighborhood, and chronic poverty affect child behavioral problems differently in different racial-ethnic groups? Pediatrics. 2006;117(4):1329–1338. doi: 10.1542/peds.2005-1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matthews SG, Phillips DI. Mini review: transgenerational inheritance of the stress response: a new frontier in stress research. Endocrinology. 2010;151(1):7–13. doi: 10.1210/en.2009-0916. [DOI] [PubMed] [Google Scholar]
- 38.Shirtcliff EA, Peres JC, Dismukes AR, Lee Y, Phan JM. Hormones: commentary: riding the physiological roller coaster: adaptive significance of cortisol stress reactivity to social contexts. J Pers Disord. 2014;28(1):40–51. doi: 10.1521/pedi.2014.28.1.40. [DOI] [PubMed] [Google Scholar]
- 39.Child Growth Foundation. Puberty and the Tanner stages—developed by Professor James M Tanner. http://www.childgrowthfoundation.org/CMS/FILES/Puberty_and_the_Tanner_Stages.pdf. Accessed October 6, 2016.


