Abstract
HIV infection induces a wide range of effects in B cells, including skewed memory cell differentiation, compromised B cell function and hypergammaglobulinaemia. However, data on the extent to which these B cell abnormalities can be reversed by antiretroviral therapy (ART) are limited.
To investigate the effect of ART on B cells, the activation (CD86) and differentiation (IgD, CD27 and CD38) profiles of B cells were measured longitudinally in 19 HIV-infected individuals before (median, 2 months) and after ART initiation (median, 12 months) and compared to 19 age-matched HIV-uninfected individuals, using flow cytometry.
Twelve months of ART restored the typical distribution of B cell subsets, increasing the proportion of naive B cells (CD27−IgD+CD38−) and concomitantly decreasing the immature transitional (CD27−IgD+CD38+), unswitched memory (CD27+IgD+CD38−), switched memory (CD27+IgD−CD38− or CD27−IgD−CD38−) and plasmablast (CD27+IgD−CD38high) subsets. However, B cell activation was only partially normalized post-ART, with the frequency of activated B cells (CD86+CD40+) reduced compared to pre-ART levels (p=0.0001), but remaining significantly higher compared to HIV-uninfected individuals (p=0.0001). Interestingly, unlike for T cell activation profiles, the extent of B cell activation prior to ART did not correlate with HIV plasma viral load, but positively associated with plasma sCD14 levels (p=0.01, r=0.58).
Overall, ART partially normalizes the skewed B cell profiles induced by HIV, with some activation persisting. Understanding the effect of HIV on B cell dysfunction and restoration following ART may provide important insights into mechanisms of HIV pathogenesis.
INTRODUCTION
Systemic immune hyperactivation is a hallmark of HIV infection, affecting a range of immune cells, including both T cells and B cells (1). Multiple B cell defects have been reported in HIV-infected individuals, including alteration in the distribution of B cell memory subsets, with the accumulation of differentiated B cells (2–5), excessive B cell activation (6, 7) and increased cell turnover (8). These B cell perturbations lead to functional abnormalities, as demonstrated by hypergammaglobulinemia, decreased B cell responsiveness to both T cell-dependent and T cell-independent antigens (9–11) and compromised responses to vaccination (9, 12, 13).
The specific mechanisms contributing to B cell abnormalities are only partially known, and multiple factors may account for their dysfunction. HIV-driven alteration of the cytokine and chemokine environment has been described as a source of B cell dysfunction (5, 14–16); and it has also been proposed that specific HIV proteins may have a direct effect on B cells (17, 18). Several studies, performed mostly in cross-sectional Caucasian cohorts, have investigated the effect of antiretroviral therapy (ART) on B cells, reporting that suppressive ART can partially or completely normalize B cell phenotypic defects, as shown by the replenishment of naive B cells (19–22), contraction of activated B cells (21–25) and increase in B cell survival potential (26). It is still uncertain, however, whether normalization of B cell memory subsets results in improved B cell immune responses to antigens, including influenza, measles, pneumococcus and hepatitis B (10, 11, 27–29).
There is a paucity of published studies on female and African populations with regard to B cell activation and restoration of B cell immunity following successful treatment of HIV (30, 31). There are cogent reasons to believe there may be differences in Africans compared to Caucasian cohorts. African cohorts have demonstrated higher baseline levels of T cell activation, significantly different T cell memory differentiation profiles (32, 33), and consistently weaker cellular and humoral reactivity to some vaccines (34, 35). A variety of factors may influence immune activation and therefore normalization of immune profiles after ART, such as genetic, gender and environmental differences, the latter including higher antigenic exposure, diet and gut microbiota. Furthermore, a variety of sex-specific differences in the response to infections have been described. Women have higher levels of immune activation and faster progression of HIV disease than men with the same viral load (36). These effects have been attributed to oestrogen receptor signaling and/or differences in expression of key X-chromosome-expressed immune regulators, such as toll-like receptors and CD40L (37). Additional factors such as HIV strains, treatment regimens and delayed access to HIV treatment could result in distinct outcomes with respect to immunity after ART.
Thus, in this study, to define the extent to which ART restores B cell phenotype, we measured the memory differentiation and activation profiles of B cells longitudinally in chronically HIV-infected African women before and 12 months after ART initiation, and compared these profiles to age- and sex-matched HIV-uninfected individuals.
MATERIAL AND METHODS
Description of study participants
Study participants consisted of 19 women from the Centre for the AIDS Programme of Research in South Africa (CAPRISA) 002 HIV acute infection cohort in KwaZulu-Natal, previously described (38, 39). Peripheral blood samples were obtained at two time-points, during chronic infection pre-ART initiation, and post-ART initiation. With respect to ART regimens, 15 of the 19 participants were taking current standard first-line therapy (TDF/3TC/EFV or TDF/FTC/EFV), and 1 each were taking D4T/3TC/EFV, D4T/3TC/NVP, AZT/3TC/NVP and AZT/3TC/LPV/r. One participant (CAP255) switched ART regimens during the study period (D4T/3TC/EFV to AZT/3TC/EFV at month 10). No participants had active TB during the study period, or exhibited any immune reconstitution inflammatory syndrome upon HIV treatment. An additional 19 HIV-uninfected women who were matched for age and ethnicity were studied, from the CAPRISA 004 1% tenofovir microbicide gel trial (40). These women were either in the pre-intervention or in the placebo arms of the trial. For HIV-infected individuals, either a prospective RNA positive/antibody negative reading or the midpoint between the last antibody negative test and the first antibody positive enzyme-linked immunosorbent assay test were used to determine the time after infection. HAART was given according to the South African national HIV treatment guidelines (at a CD4 count of <200 cells/mm3 prior to October 2012; <350 cells/mm3 until March 2015). Ethical approval for the study was obtained from the Research Ethics Committees at the University of KwaZulu-Natal and University of Cape Town. All participants provided written informed consent prior to participating in the study.
Measurements of HIV plasma viral load and CD4 counts
Plasma HIV viral load and CD4 count were assessed at each study visit. Over the course of the study, the viral load PCR assay switched from Roche AMPLICOR HIV-1 monitor test version 1.5 (lower detection limit (LDL) of 400 RNA copies/ml) to Roche Taqman version 1.0 in June 2010 (LDL 40 RNA copies/ml), and then to Roche Taqman version 2.0 in January 2012 (LDL 20 RNA copies/ml). The FACSCalibur TruCOUNT method (BD Biosciences) was used to measure blood absolute CD4+ and CD8+ T cell counts.
Sample processing
Peripheral blood mononuclear cells (PBMC) were isolated by Ficoll-Hypaque (Amersham Pharmacia) density gradient centrifugation and cryopreserved in freezing media (heat-inactivated fetal calf serum (FCS; Invitrogen) containing 10% dimethylsulfoxide (Sigma-Aldrich). Cells were stored in liquid nitrogen until use. Cryopreserved PBMC were thawed and rested in R10 (RPMI 1640 plus 10% heat-inactivated FCS and 50 U/ml of penicillin-streptomycin) at 37°C with 5% CO2 for 3 hours before staining.
Antibodies, Surface and Intracellular staining (ICS)
The following antibodies were used in three different staining panels: CD19 ECD (J3-119), CD27 PE-Cy5 (1A4CD27; both Beckman Coulter), IgD APC-Cy7 (IA6-2), CD10 BV605 (HI10a), CD21 PE-Cy7 (Bu32), CD40 PerCP-Cy5.5 (5C3; all Biolegend), CD38 APC (HIT2), CD86 PE (IT2.2), CD3 PE-Cy7 (SK7), HLA-DR APC-Cy7 (L243; all BD Biosciences), CD4 PE-Cy5.5 (S3.5), CD8 Qdot-705 (3B5), CD19 Pacific Blue (SJ25-CI), CD14 Pacific Blue (Tük4), CD3 Pacific Blue (UCHT1), Ki67 FITC (7B11; all Invitrogen) and a violet viability reactive dye (“Vivid”; Molecular Probes). All antibodies were titrated prior to use to obtain optimal titers for staining. Briefly, PBMC were stained with Vivid, then labeled with antibodies against surface markers, fixed, permeabilized and subsequently stained intracellularly with Ki67. Cells were then re-suspended in 1X CellFix (BD Biosciences) and kept at 40C until acquisition. Samples were acquired on a BD Fortessa using FACSDiva software and analyzed using FlowJo (version 9.9.3; TreeStar). The gating strategy to identify B cell subsets is shown in Supplemental Figure S1.
Enzyme-linked immunosorbent assays (ELISA)
Plasma samples were used to measure soluble CD14 (sCD14, a marker of monocyte/macrophage activation) from the same women pre- and post-ART. One participant was not included in this analysis due to the sample being unavailable. Plasma (n=18) was tested in duplicate using commercially available ELISA kits according to the manufacturers’ protocol (R&D Systems). In addition, 30 plasma samples from HIV-uninfected women from the same cohort were included. Samples were diluted 1:200, data were collected using a SpectraMax Plus reader (Molecular Devices) and point-to-point curve fits were used to calculate sCD14 concentrations from the standard curves. Data were analyzed using SoftMax Pro software (Version 3.2.1; Molecular Devices).
Statistical analyses
Statistical analyses were performed using GraphPad Prism (version 5.0). The Mann-Whitney U test and the Wilcoxon Signed Rank test were used for unmatched and paired samples, respectively. Correlations between the different groups were determined by the non-parametric Spearman Rank test. A p-value of <0.05 was considered statistically significant.
RESULTS
Effect of antiretroviral therapy (ART) on the memory differentiation and activation of B cells
To define the extent to which ART normalizes HIV-induced alteration of B cells, we first determined the distribution of B cell subsets in 19 HIV-infected individuals before and one year after ART initiation, and compared it to 19 HIV-uninfected matched controls. Pre-ART samples were obtained during chronic infection at a median of 4.9 years [Interquartile range (IQR): 2.8–5.8 years] after the estimated date of HIV infection, and a median of 1.5 months (IQR: 0.05–2.7) prior to starting ART. The median plasma viral load at this time was 34,325 HIV RNA copies/ml (IQR: 7,997–78,573), and the median CD4 count was 314 cells/mm3 (IQR: 260–369) (Table I). After a median of 12 months of treatment (IQR: 12–13 months), all individuals exhibited viral suppression (p=0.0001), the majority to <40 copies/ml, and an increase in both absolute CD4 count and CD4/CD8 ratio (both p=0.0001) (Table I and data not shown).
Table 1.
Clinical parameters of study participants
| HIV-infected (pre-ART) | HIV-infected (post-ART) | P-value | |
|---|---|---|---|
| Sample size | 19 | 19 (paired) | |
| CD4 count (cells/mm3) * | 314 [260–369] | 629 [514–696] | p=0.0001 |
| CD4/CD8 ratio * | 0.23 [0.18–0.33] | 0.61 [0.48–0.74] | p=0.0001 |
| Viral load (RNA copies/ml) * | 34,325 [7,997–78,573] | <20 [<20–39] | p=0.0001 |
| Duration of ART (months) * | NA | 12 [12–13] |
Median and Interquartile range
NA: Not Applicable
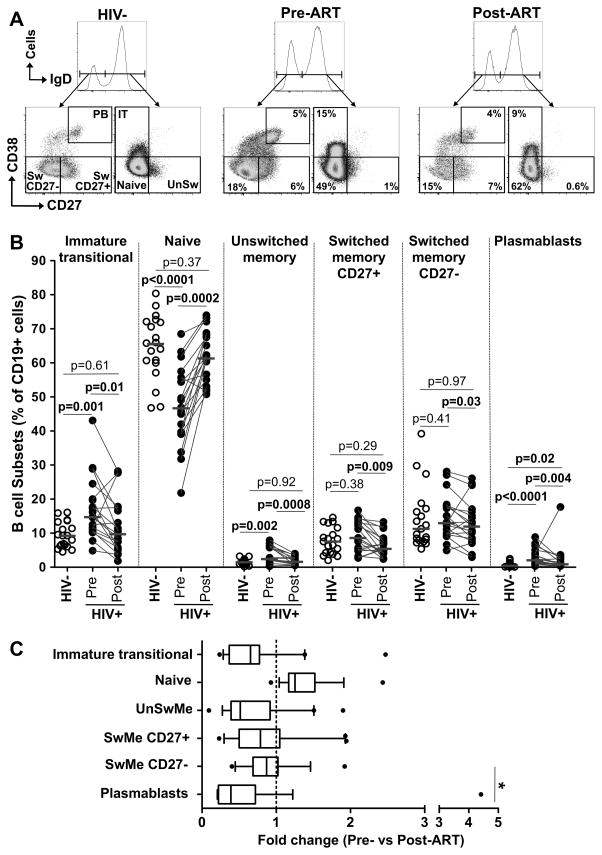
Figure 1A shows representative flow plots of each B cell subset from one HIV-uninfected and one HIV-infected individual pre- and post-ART. Based on the expression of CD27, IgD and CD38, six B cell subsets were identified, namely immature transitional B cells (CD27−IgD+CD38+), naive B cells (CD27−IgD+CD38−), unswitched memory (CD27+IgD+CD38−), CD27+ switched memory B cells (IgD−CD38−), CD27− switched memory B cells (IgD−CD38−) and plasmablasts (CD27+IgD−CD38high). There was a marked skewing of B cell subsets in chronic HIV infection prior to ART (Figure 1B). When compared to HIV-uninfected participants, HIV-infected individuals were characterized by significantly higher frequencies of immature transitional B cells, unswitched memory B cells and plasmablasts (median: 9.3% [IQR: 6.3–13.3] vs 14.8% [IQR: 10.6–20]; 1.5% [IQR: 1.2–1.7] vs 2.3% [IQR: 2–5.8] and 0.44% [IQR: 0.3–1] vs 2.1% [IQR: 1.4–4], respectively), and significantly lower proportions of naive B cells (median: 65.8% [IQR: 60–72.1] vs 46.9% IQR: 39.7–55.7) (Figure 1B). Additionally, the frequencies of switched memory B cells, expressing CD27 or not were comparable in HIV-uninfected and ART naive HIV-infected individuals (~8% and ~12%, respectively). It is worth mentioning that the frequency of un-switched memory B cells in our healthy study population was about 7 times lower when compared to a previous study reporting that the proportion of unswitched memory was comparable to switched memory (representing about 15% of total B cells) in a predominantly male cohort from London (11). Following 12 months of ART, the frequency of immature transitional, naive and unswitched memory B cells were normalized, returning to levels comparable to those observed in HIV-uninfected individuals (Figure 1B). The frequency of plasmablasts was also reduced in response to ART (p=0.004), but remained significantly elevated compared to the HIV-uninfected group. To further define the restoration dynamics of B cell subsets upon ART, we compared the fold change in their frequencies pre- and post-ART. After one year of ART, only naive B cells displayed an overall expansion (median 1.3 fold [IQR: 1.2–1.5]); amongst the subsets decreasing upon ART, plasmablasts exhibited the largest contraction, with a median fold change of 0.38 [IQR: 0.22–0.72]. The contraction of other B cells subsets was more moderate with a median fold change of 0.51 [IQR: 0.39–0.92] for unswitched memory B cells, 0.65 [IQR: 0.37–0.77] for immature transitional B cells, 0.79 [IQR: 0.5–1] for CD27+ switched memory B cells and 0.87 [IQR: 0.69–1] CD27− switched memory B cells (Figure 1C). Although ART had a predominant effect on reducing the frequency of plasmablasts (~60% reduction), this was not sufficient for their normalization with respect to HIV-uninfected individuals.
Figure 1. Effect of ART on the memory differentiation profile of B cells.
(A) Representative flow plots of CD27, IgD and CD38 expression in B cells from one HIV-uninfected and one HIV-infected (pre- and post-ART) individual. Numbers represent the frequencies of each B cell subset, namely immature transitional (CD27−IgD+CD38+), naive (CD27−IgD+CD38−), Unswitched memory (CD27+IgD+CD38−), switched CD27+ memory (IgD−CD38−), switched CD27- memory (IgD−CD38−) and plasmablasts (CD27+IgD−CD38high). (B) Frequencies of B cell subsets in HIV-uninfected (n=19; open circles) and HIV-infected pre- and post ART (n=19; closed circles) individuals. Horizontal lines indicate the median. Statistical significance was calculated using a Mann-Whitney U test and Wilcoxon Signed Rank for unpaired and paired samples, respectively. (C) Fold change in the frequency of B cell subsets over 12 months of ART. Data are shown as box and whisker (interquartile range) plots. The vertical dotted line indicates no change from the time point prior to ART. Statistical comparisons were calculated using a one-way ANOVA test. *p < 0.05, **p < 0.01, ***p < 0.001.
Alternative B cell markers such as CD27, CD10 and CD21 have been used to delineate B cell memory subsets (41), allowing for the identification of three additional B cell memory subsets, namely tissue-like memory (CD10−CD21−CD27−), resting memory (CD21+CD27dim) and activated memory (CD10−CD21−CD27dim) B cells (Supplemental Figure S1B). The expression of CD10 and CD21 on B cell subsets is shown in Supplemental Figure S2. Thus, to validate our data, we defined the evolution of B cell memory subpopulations pre- and post-ART using this set of markers in 10 of the HIV-infected individuals from our study (Supplemental Figure S3). ART led to a significant reduction in the frequencies of tissue-like memory, activated memory B cells and plasmablasts, and an increase in the frequencies of naive and resting memory B cells. These observations confirm the data described above, and are in line with published data (21). Of note, using this alternative gating strategy, we found no significant difference in the frequencies of immature transitional B cells between the two timepoints. This may be due to the small sample size (a subset of n=10) used for this set of markers, since further analysis of the same individuals using IgD, CD38 and CD27 also showed no significant difference in immature transitional B cells (data not shown).
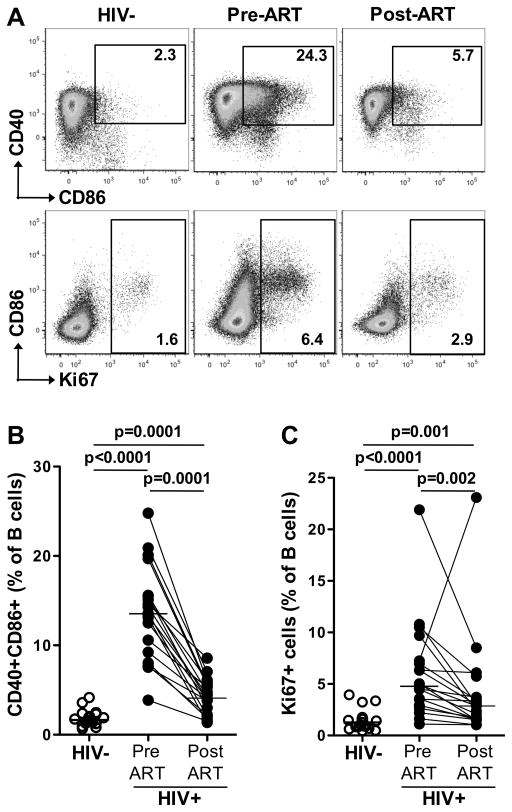
The effect of ART on B cell activation and proliferation were also evaluated. Figure 2A shows representative flow plots of B cell activation, measured as the frequency of B cells co-expressing CD86 and CD40, and proliferation (Ki67 expression) from one HIV-uninfected and one HIV-infected individual pre- and post-ART. The frequency of activated B cells (CD86+CD40+) was significantly higher in HIV-infected subjects prior to ART compared to HIV-uninfected participants (median: 14% [IQR: 9.2–15.6] vs 1.7% [IQR: 1.3–2.3]; Figure 2B). In response to ART, the frequency of activated B cells was substantially reduced but remained significantly higher than HIV-uninfected participants (Figure 2B). It is important to mention that during HIV infection, activated B cells were mostly confined to switched memory cells (i.e. IgD- B cells), with a median of 25% (IQR: 19.6–32) of switched cells co-expressing CD40 and CD86. On the contrary, the activation level of un-switched B cells (i.e. IgD+ B cells) was only marginal, with less that 5% of these cells positive for CD40 and CD86 (median: 4.5% [IQR: 2.4–5]; data not shown).
Figure 2. Effect of ART on B cell activation and proliferation.
(A) Representative flow plots of CD40, CD86 and Ki67 expression in B cells from one HIV-uninfected and one HIV-infected (pre- and post-ART) individual. Numbers represent the frequencies of activated (CD86+CD40+) and proliferating (Ki67+) B cells. (B) Frequencies of CD86+CD40+ B cells in HIV-uninfected (n=19; open circles) and HIV-infected pre- and post-ART (n=19; closed circles) individuals. (C) Frequencies of proliferating B cells as measured by Ki67 expression. Horizontal lines represent the median. Statistical significance was calculated using a Mann-Whitney U test and Wilcoxon Signed Rank for unpaired and paired samples, respectively.
Similar to activated B cells, there were significantly more Ki67+ B cells in ART-naive HIV-infected individuals compared to HIV-uninfected controls (median: 5% [IQR: 2.9–7.2] vs 1.3% [IQR: 0.9–1.6]); and while ART led to a significant decline in proliferating B cells, they remained elevated compared to the HIV-uninfected group (p=0.001, Figure 2C). Of note, the frequencies of proliferating (Ki67+) and activated (CD86+CD40+) B cells were positively associated with the frequency of plasmablasts following ART (p=0.004, r=0.62 and p=0.003, r=0.63, respectively, data not shown), suggesting that residual B cell activation and proliferation upon ART may be explained by the persistence of an elevated frequency of plasmablasts, consistent with our findings presented in Figure 1B.
Overall, our data show that HIV infection skews the B cell memory differentiation profile and causes abnormal B cell activation and proliferation. Defects in B cell memory phenotype were largely normalized within one year of ART, while B cell activation and proliferative capacities were only partially reduced and longer periods of suppressive therapy may be required for normalization.
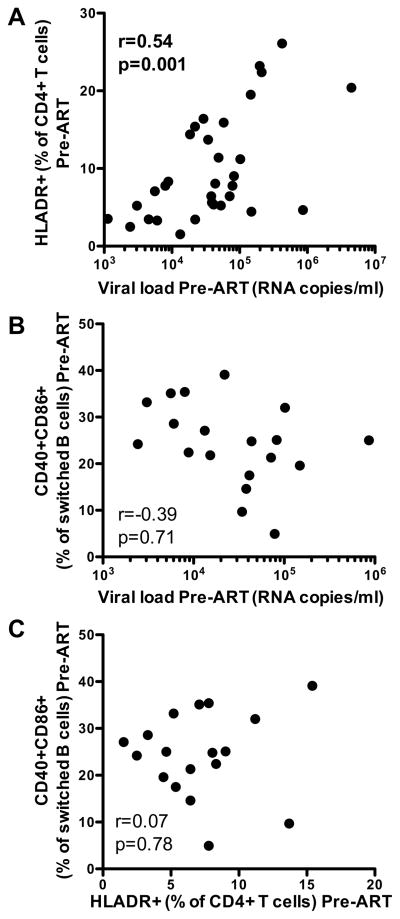
B cell defects during HIV infection do not directly associate with HIV viral load
It has been clearly established that hyper-immune activation of T cells during HIV infection is related to viral replication (42) and is partially normalized upon ART (43). This was confirmed in our experimental setting, where we had T cell activation data for 18 of the participants in the current study, as well as 14 additional subjects from the same cohort. The proportion of activated CD4+ T cells (measured by the expression of HLA-DR) was positively associated with plasma viral load (p=0.001, r=0.54; Figure 3A) in HIV-infected subjects pre-ART. While 12 months of ART led to a substantial reduction in the frequency of HLA-DR expression by T cells, T cell activation levels remained significantly higher than HIV-uninfected subjects (Supplemental Figure S4). Thus, in order to determine whether HIV load was also the driving factor for B cell activation, we examined the relationship between B cell phenotype and HIV plasma viral load before ART initiation. As previously stated, switched memory B cells (i.e IgD- B cells) are highly activated during HIV infection, thus we focused our analyses on this particular subset. Surprisingly, unlike for T cells, we found no association between the frequency of activated (CD86+CD40+) switched memory B cells and HIV viral load (p=0.71, r=0.39; Figure 3B). Moreover, none of the B cell memory subset frequencies were found to be associated with viral load (data not shown). Finally, the extent of CD4+ or CD8+ T cell activation did not correlate with the level of switched B cell activation (p=0.78, r=0.07; Figure 3C and data not shown). Together, these results show that HIV differentially affects the T cell and B cell compartments, where B cell activation does not mirror T cell activation and is not directly associated with the levels of HIV. This suggests that additional factors besides HIV replication may contribute to B cell activation.
Figure 3. Relationship between CD4+ T cell and B cell activation and plasma viral load pre-ART.
Correlation of (A) the frequency of HLA-DR expressing CD4+ T cells (n=32) and (B) the frequency of CD40+CD86+ switched memory B cells (n=18) and plasma viral load in HIV-infected individuals prior to ART initiation. (C) Correlation between B cell activation (CD86+CD40+) and CD4+ T cell activation (HLA-DR+) in 18 HIV-infected participants before ART. Statistical significance was calculated using a non-parametric Spearman Rank test.
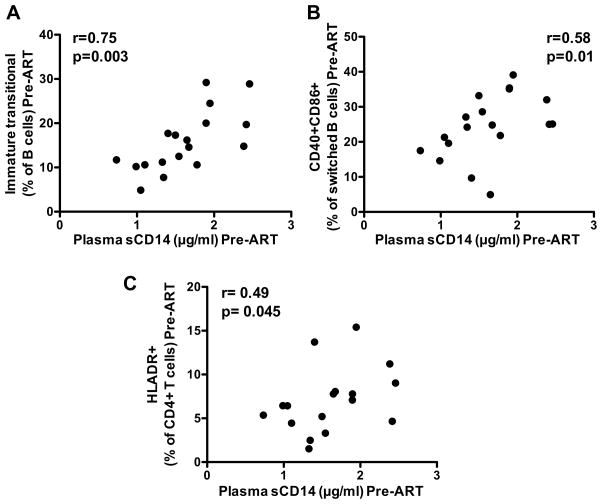
Additional contributors of B cell defects during HIV infection
The translocation of bacterial products, resulting from HIV-induced damage to the gastrointestinal tract, is an important contributor of systemic immune activation (44). Therefore, we investigated the relationship between the activation and skewed differentiation profile of B cells and the level of plasma sCD14, a marker of monocyte/macrophage activation, that may be an indicator, in the absence of other infections, of microbial translocation. Prior to ART, plasma sCD14 levels associated negatively with the frequency of naive B cells (p=0.036, r=−0.50; data not shown) and positively with the frequency of immature transitional B cells (p=0.003, r=0.75; Figure 4A) and the frequency of activated (CD86+CD40+) switched memory B cells (p=0.01, r=0.58; Figure 4B). Moreover, a positive correlation was also observed between sCD14 levels and the frequency of activated HLA−DR+CD4+ T cells (p=0.045, r=0.49; Figure 4C). It is worth noting that the levels of plasma sCD14 were not significantly changed after 12 months of ART (Supplemental Figure S5), and there were no associations with residual B cell activation post-ART (data not shown).
Figure 4. Relationship plasma sCD14 levels and B cell phenotype and CD4+ T cell activation pre-ART.
Correlation of (A) the frequency of immature transitional B cells, (B) the frequency of CD86+CD40+ switched memory B cells and (C) and the frequency of HLA-DR+ CD4+ T cells with plasma sCD14 levels in HIV-infected individuals (n=18 and n=17, respectively). Statistical significance was calculated using a non-parametric Spearman Rank test.
Overall, these data suggest a possible impact of microbial translocation on B cell dysfunction, as suggested by sCD14 levels correlating with HIV-induced B cell skewing and hyperactivation in untreated chronic HIV infection. However, their influence may be relatively minor, since there are consistently elevated levels of sCD14 after ART, when B cell defects are largely reversed. It is clear that a variety of factors may directly or indirectly influence B cell defects during HIV infection.
DISCUSSION
Despite the fact that HIV does not directly infect B cells, the virus causes several B cell abnormalities that contribute to HIV pathogenesis (45). Whilst these B cell defects may be reverted upon antiretroviral therapy (ART), this effect has mostly been studied in cross-sectional Caucasian cohorts. Thus, in this study, we assessed longitudinally the impact of ART on the memory and activation profile of B cells in South African adult women (n=19); and compared these profiles to age-matched HIV-uninfected women from the same community (n=19). Our data show that 1) HIV-induced alterations of B cells did not associate with viral burden but rather correlated with plasma sCD14 concentration and 2) 12 months of ART largely normalized the distribution of B cell memory subsets whilst activation of B cells was only partially reduced.
HIV induces multiple defects in B cells, altering their memory and activation profiles and function (3, 5, 41, 46). In our experimental setting, we showed that, in HIV-infected African women, B cells were skewed towards a more differentiated memory phenotype (with the accumulation of plasmablasts and the reduction of naive B cells) and were hyperactivated (as measured by CD86 expression) when compared to HIV-uninfected persons. These observations are in accordance with previous studies performed primarily in male Caucasian populations (3, 20, 21, 28, 46, 47), highlighting that similar abnormalities occur in African women. To date, the drivers of B cell alterations during HIV infection have not been fully elucidated. Even though HIV does not directly target B cells for infection, the interaction between HIV and B cells has been previously described, where HIV glycoprotein gp120 can bind to B cell receptors (such as CD21, DC-SIGN and variable heavy chain 3 (VH3) immunoglobulin (Ig), resulting in polyclonal B cell activation and Ig production (48). Furthermore, HIV Nef can interact directly with B cells, resulting in suppression of Ig class switching (49, 50). How each of these mechanism contribute to B cell dysfunction is unknown (41).
It has also been proposed that excessive B cell activation may be driven by pro-inflammatory cytokines, such as IFN-α, TNF-α, IL-6 and IL-10, molecules commonly up-regulated during HIV-induced systemic inflammation (51). HIV infection also leads to increased production of B cell-specific growth factors such as BLyS/BAFF from macrophages, dendritic cells and granulocytes (52–54), promoting B cell dysregulation right from the early stages of infection. Additionally, HIV pathogenesis has also been linked to extensive damage to the gastrointestinal tract, leading to the release of bacterial products into the circulation (44). These products may induce aberrant B cell activation via TLR signaling (55), by both direct and indirect means. Stimulation of monocytes by bacterial LPS leads to the release of cytokines that contribute to the inflammatory environment. Additionally, human B cells express a range of TLRs, including high levels of TLR9 (56), and abundant bacterial DNA as a result of HIV-induced microbial translocation (57) may stimulate B cells directly. In fact, TLR9 stimulation of human B cells promotes their activation, proliferation and the generation of plasmablasts (58, 59). The potential role of microbial products as direct factors fueling B cell hyperactivation is further inferred by the fact that in other chronic diseases leading to gut damage (such as inflammatory bowel disease), B cells exhibit aberrant activation profiles (60).
We found an association pre-ART of B cell activation and differentiation profile with the concentration of plasma sCD14, secreted upon monocyte/macrophage activation by LPS, which may be a surrogate marker of microbial translocation. Interestingly, whilst there was a relative normalization of B cells post-ART, plasma sCD14 concentration did not decrease overall upon treatment. This phenomenon has been observed in several studies, where sCD14 levels remain elevated even after several years on ART (61–63), and unreversed damage to the gastrointestinal tract has been proposed to account for this. These data confirm that in African women, inflammation persists after ART even while there is a substantial decrease in cellular activation. The absence of any decrease in sCD14 after ART, despite a substantial normalization of B cells profiles, suggests that sCD14 plays only a partial role in contributing to B cell activation. Alternatively, we could speculate that microbial translocation and viral-induced factors might act synergistically to drive B cell activation and skewing, and ART uncouples this effect by suppressing viral replication even in the face of ongoing inflammation. Whilst we did not find an association of HIV viral load with B cell dysfunction pre-ART, this relationship may not be linear, with a multitude of viral-induced factors influencing B cell activation and differentiation directly and indirectly (64). Overall, this suggests that a combination of inflammatory mediators such as cytokines, B cell growth factors and microbial products may directly and indirectly stimulate B cell differentiation and proliferation, favoring their functional impairment and exhaustion.
Several studies have shown that ART leads to a near normalization of peripheral B cell memory subsets (19, 20, 22, 65); and the extent of restoration was linked to the timing of ART initiation (21, 66), the duration of treatment or related to the age of the patients (22, 67). Very limited data are available on the effect of ART on B cells in African cohorts. To our knowledge, only one cross-sectional study has investigated how ART influences the restoration of B cell numbers in an African adult population (31). It is of importance to define, in countries disproportionately affected by the HIV pandemic and where access to ART is limited and often started during advanced lymphopenia, whether HIV treatment can restore B cell profiles to similar levels observed in HIV-uninfected individuals (of note, the CD4 count pre-treatment in the participants included in this study was <350 cells/mm3). Our data showed that while 12 months of ART largely normalized the distribution of memory subsets, B cell activation remained significantly elevated compared to HIV-uninfected individuals. The persistence of these cycling, activated B cells composed mainly of plasmablasts could reflect residual systemic inflammation, despite viral suppression. Indeed, it has been shown that even upon successful ART, inflammation, microbial translocation and germinal center destruction still persist (44, 68–70). These observations are in line with results reported in Caucasian cohorts (20, 21, 71), showing that the normalization of B cell subsets can be achieved even when treatment is initiated at a late stage of chronic HIV infection.
The limitations of this study include a cohort exclusively composed of women; further studies could test the generalizability of our findings in men. Additionally, we only analyzed B cells from peripheral blood and this may not be representative of B cell profile within the tissues; it is plausible that B cell residing in germinal center are differentially affected during HIV infection and that the extent and/or kinetics of their restoration during treatment may differ. For future studies, use of additional phenotypic markers such as CD10 and CD24 could improve the definition of B cell subsets, in particular immature transitional B cells. Furthermore, we did not examine the relationship of relative normalization of B cell activation and differentiation with restoration of functional B cell immunity, which may not always return (72). Further studies of humoral immunity after ART, by investigation of both memory B cell responses and long-lived plasma cells to a variety of vaccines and infections, are warranted in larger African cohorts. This is particularly important if functional B cell immunity is not fully restored and revaccination to certain pathogens may be required. In this respect, early ART initiation, compared to those treated during chronic HIV infection, has demonstrated a benefit for restoration of B cell functionality (21).
In conclusion, our study has shown that the B cell compartment is highly disturbed in chronically HIV-infected African women, an understudied group disproportionately affected by the HIV pandemic, as it is for Caucasian cohorts. Differences in methodology limit our ability to directly compare our results in African women to published studies in western cohorts, but we observed a substantial reduction in B cell activation and a relative normalization of skewed B cell subsets as observed in Caucasian cohorts, despite the commencement of ART in chronic HIV infection. Identifying the drivers of B cell activation and defective differentiation may provide a better understanding of the mechanisms associated with B cell dysfunction. This can potentially lead to the development of intervention strategies to improve B cell function during HIV infection, for both HIV-specific humoral immunity and responses to vaccines targeting other pathogens.
Supplementary Material
Acknowledgments
We thank all of the CAPRISA 002 and 004 study participants who are continuing to make an important personal contribution to HIV research. The scientific and supportive role of the whole CAPRISA 002 and CAPRISA 004 study and protocol team is gratefully acknowledged. Thank you to Lindi Masson for contributing T cell data, and to Mrs Kathryn Norman for administrative assistance.
This work was funded by the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH), the Office of the Director (OD) and the Department of Health and Human Services Grant R01 AI084387 (to W.A.B.), U19 A151794 (to S.A.K.), R21 AI115977 (to C.R.) and the South African Medical Research Council. The clinical trial from which some of the participants were drawn (CAPRISA 004) was supported by the United States Agency for International Development (USAID), FHI360 [USAID co-operative agreement #GPO-A-00-05-00022-00, contract #132119]. W.A.B. is supported by a Wellcome Trust Intermediate Fellowship in Public Health and Tropical Medicine (089832/Z/09/Z).
Footnotes
CONTRIBUTION:
Conceived and designed the experiments: A.P.S., N.J.G., Q.A.K., S.A.K. C.R and W.A.B. Performed the experiments: R.F.T., T.L.M. and A.P.S. Analyzed the data R.F.T, C.R. and W.B. Contributed reagents/materials/analysis tools: N.S., N.J.G., Q.A.K. and S.A.K. Wrote the paper: R.F.T., C.R. and W.A.B. All authors approved the final manuscript.
Disclosure:
The authors have no conflict of interest.
References
- 1.Appay V, Sauce D. Immune activation and inflammation in HIV-1 infection: causes and consequences. J Pathol. 2008;214:231–241. doi: 10.1002/path.2276. [DOI] [PubMed] [Google Scholar]
- 2.Moir S, Malaspina A, Ogwaro KM, Donoghue ET, Hallahan CW, Ehler LA, Liu S, Adelsberger J, Lapointe R, Hwu P, Baseler M, Orenstein JM, Chun TW, Mican JAM, Fauci AS. HIV-1 induces phenotypic and functional perturbations of B cells in chronically infected individuals. Proc Natl Acad Sci. 2001;98:10362–10367. doi: 10.1073/pnas.181347898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moir S, Ogwaro KM, Malaspina A, Vasquez J, Donoghue ET, Hallahan CW, Liu S, Ehler LA, Planta MA, Kottilil S, Chun TW, Fauci AS. Perturbations in B cell responsiveness to CD4+ T cell help in HIV-infected individuals. Proc Natl Acad Sci. 2003;100:6057–6062. doi: 10.1073/pnas.0730819100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moir S, Ho J, Malaspina A, Wang W, DiPoto AC, O’Shea MA, Roby G, Kottilil S, Arthos J, Proschan MA, Chun T, Fauci AS. Evidence for HIV-associated B cell exhaustion in a dysfunctional memory B cell compartment in HIV-infected viremic individuals. J Exp Med. 2008;205:1797–1805. doi: 10.1084/jem.20072683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malaspina A, Moir S, Ho J, Wang W, Howell ML, O’Shea MA, Roby GA, Rehm CA, Mican JM, Chun TW, Fauci AS. Appearance of immature/transitional B cells in HIV-infected individuals with advanced disease: Correlation with increased IL-7. Proc Natl Acad Sci. 2006;103:2262–2267. doi: 10.1073/pnas.0511094103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malaspina A, Moir S, Kottilil S, Hallahan CW, Ehler LA, Liu S, Planta MA, Chun TW, Fauci AS. Deleterious Effect of HIV-1 Plasma Viremia on B Cell Costimulatory Function. J Immunol. 2003;170:5965–5972. doi: 10.4049/jimmunol.170.12.5965. [DOI] [PubMed] [Google Scholar]
- 7.De Milito A, Nilsson A, Titanji K, Thorstensson R, Reizenstein E, Narita M, Grutzmeier S, Sönnerborg A, Chiodi F. Mechanisms of hypergammaglobulinemia and impaired antigen-specific humoral immunity in HIV-1 infection. Blood. 2004;103:2180–2186. doi: 10.1182/blood-2003-07-2375. [DOI] [PubMed] [Google Scholar]
- 8.Kovacs JA, Lempicki RA, Sidorov IA, Adelsberger JW, Herpin B, Metcalf JA, Sereti I, Polis MA, Davey RT, Tavel J, Falloon J, Stevens R, Lambert L, Dewar R, Schwartzentruber DJ, Anver MR, Baseler MW, Masur H, Dimitrov DS, Lane HC. Identification of dynamically distinct subpopulations of T lymphocytes that are differentially affected by HIV. J Exp Med. 2001;194:1731–41. doi: 10.1084/jem.194.12.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malaspina A, Moir S, Orsega SM, Vasquez J, Miller NJ, Donoghue ET, Kottilil S, Gezmu M, Follmann D, Vodeiko GM, Levandowski RA, Mican JM, Fauci AS. Compromised B Cell Responses to Influenza Vaccination in HIV-Infected Individuals. J Infect Dis. 2005;191:1442–1450. doi: 10.1086/429298. [DOI] [PubMed] [Google Scholar]
- 10.Titanji K, De Milito A, Cagigi A, Thorstensson R, Grützmeier S, Atlas A, Hejdeman B, Kroon FP, Lopalco L, Nilsson A, Chiodi F. Loss of memory B cells impairs maintenance of long-term serologic memory during HIV-1 infection. Blood. 2006;108:1580–1587. doi: 10.1182/blood-2005-11-013383. [DOI] [PubMed] [Google Scholar]
- 11.Hart M, Steel A, Clark SA, Moyle G, Nelson M, Henderson DC, Wilson R, Gotch F, Gazzard B, Kelleher P. Loss of Discrete Memory B Cell Subsets Is Associated with Impaired Immunization Responses in HIV-1 Infection and May Be a Risk Factor for Invasive Pneumococcal Disease. J Immunol. 2007;178:8212–8220. doi: 10.4049/jimmunol.178.12.8212. [DOI] [PubMed] [Google Scholar]
- 12.French N, Gilks CF, Mujugira A, Fasching C, O’Brien J, Janoff EN. Pneumococcal vaccination in HIV-1-infected adults in Uganda. AIDS. 1998;12:1683–1689. doi: 10.1097/00002030-199813000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Pasricha N, Datta U, Chawla Y, Singh S, Arora SK, Sud A, Minz RW, Saikia B, Singh H, James I, Sehgal S. Immune responses in patients with HIV infection after vaccination with recombinant Hepatitis B virus vaccine. BMC Infect Dis. 2006;6:65. doi: 10.1186/1471-2334-6-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müller F, Aukrust P, Nordoy I, Froland SS. Possible role of interleukin-10 (IL-10) and CD40 ligand expression in the pathogenesis of hypergammaglobulinemia in human immunodeficiency virus infection: modulation of IL-10 and Ig production after intravenous Ig infusion. Blood. 1998;92:3721–9. [PubMed] [Google Scholar]
- 15.Swingler S, Zhou J, Swingler C, Dauphin A, Greenough T, Jolicoeur P, Stevenson M. Evidence for a Pathogenic Determinant in HIV-1 Nef Involved in B Cell Dysfunction in HIV/AIDS. Cell Host Microbe. 2008;4:63–76. doi: 10.1016/j.chom.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lantto R, Nasi A, Sammicheli S, Amu S, Fievez V, Moutschen M, Pensieroso S, Hejdeman B, Chiodi F, Rethi B. Increased extrafollicular expression of the B-cell stimulatory molecule CD70 in HIV-1-infected individuals. AIDS. 2015;29:1757–1766. doi: 10.1097/QAD.0000000000000779. [DOI] [PubMed] [Google Scholar]
- 17.Schnittman SM, Lane HC, Higgins SE, Folks T, Fauci AS. Direct polyclonal activation of human B lymphocytes by the acquired immune deficiency syndrome virus. Science. 1986;233:1084–6. doi: 10.1126/science.3016902. [DOI] [PubMed] [Google Scholar]
- 18.Swingler S, Brichacek B, Jacque J, Ulich C, Zhou J, Stevenson M. HIV-1 Nef intersects the macrophage CD40L signalling pathway to promote resting-cell infection. Nature. 2003;424:213–219. doi: 10.1038/nature01749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Orsogna LJ, Krueger RG, McKinnon EJ, French MA. Circulating memory B-cell subpopulations are affected differently by HIV infection and antiretroviral therapy. AIDS. 2007;21:1747–52. doi: 10.1097/QAD.0b013e32828642c7. [DOI] [PubMed] [Google Scholar]
- 20.Moir S, Malaspina A, Ho J, Wang W, DiPoto AC, O’Shea MA, Roby G, Mican JM, Kottilil S, Chun TW, Proschan MA, Fauci AS. Normalization of B Cell Counts and Subpopulations after Antiretroviral Therapy in Chronic HIV Disease. J Infect Dis. 2008;197:572–579. doi: 10.1086/526789. [DOI] [PubMed] [Google Scholar]
- 21.Moir S, Buckner CM, Ho J, Wang W, Chen J, Waldner AJ, Posada JG, Kardava L, O’Shea MA, Kottilil S, Chun TW, Proschan MA, Fauci AS. B cells in early and chronic HIV infection: evidence for preservation of immune function associated with early initiation of antiretroviral therapy. Blood. 2010;116:5571–5579. doi: 10.1182/blood-2010-05-285528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amu S, Lavy-Shahaf G, Cagigi A, Hejdeman B, Nozza S, Lopalco L, Mehr R, Chiodi F. Frequency and phenotype of B cell subpopulations in young and aged HIV-1 infected patients receiving ART. Retrovirology. 2014;11:76. doi: 10.1186/s12977-014-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pensieroso S, Galli L, Nozza S, Ruffin N, Castagna A, Tambussi G, Hejdeman B, Misciagna D, Riva A, Malnati M, Chiodi F, Scarlatti G. B-cell subset alterations and correlated factors in HIV-1 infection. AIDS. 2013;27:1209–1217. doi: 10.1097/QAD.0b013e32835edc47. [DOI] [PubMed] [Google Scholar]
- 24.Rethi B, Sammicheli S, Amu S, Pensieroso S, Hejdeman B, Schepis D, Thang PH, Chiodi F. Concerted effect of lymphopenia, viraemia and T-cell activation on Fas expression of peripheral B cells in HIV-1-infected patients. AIDS. 2013;27:155–162. doi: 10.1097/QAD.0b013e32835b8c5e. [DOI] [PubMed] [Google Scholar]
- 25.Abudulai LN, Fernandez S, Corscadden K, Hunter M, Kirkham LS, Post JJ, French MA. Chronic HIV-1 Infection Induces B-Cell Dysfunction That Is Incompletely Resolved by Long-Term Antiretroviral Therapy. J Acquir Immune Defic Syndr. 2016;71:381–389. doi: 10.1097/QAI.0000000000000869. [DOI] [PubMed] [Google Scholar]
- 26.Van Grevenynghe J, Cubas RA, Noto A, Dafonseca S, He Z, Peretz Y, Filali-mouhim A, Dupuy FP, Procopio FA, Chomont N, Balderas RS, Said EA, Boulassel M, Tremblay CL, Routy J. Loss of memory B cells during chronic HIV infection is driven by Foxo3a- and TRAIL-mediated apoptosis. 2011;121:3877–3888. doi: 10.1172/JCI59211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroon FP, Rimmelzwaan GF, Roos MTL, AD, Osterhaus ME, Hamann D, Miedema F, Van Dissel JT. Restored humoral immune response to influenza vaccination in HIV-infected adults treated with highly active antiretroviral therapy. AIDS. 1998;12:217–223. doi: 10.1097/00002030-199817000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Malaspina A, Moir S, Kottilil S, Hallahan CW, Ehler LA, Liu S, Planta MA, Chun TW, Fauci AS. Deleterious effect of HIV-1 plasma viremia on B cell costimulatory function. J Immunol. 2003;170:5965–5972. doi: 10.4049/jimmunol.170.12.5965. [DOI] [PubMed] [Google Scholar]
- 29.Whitaker JA, Rouphael NG, Edupuganti S, Lai L, Mulligan MJ. Strategies to increase responsiveness to hepatitis B vaccination in adults with HIV-1. Lancet Infect Dis. 2012;12:966–976. doi: 10.1016/S1473-3099(12)70243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Béniguel L, Bégaud E, Cognasse F, Gabrié P, Mbolidi CD, Sabido O, Marovich MA, DeFontaine C, Frésard A, Lucht F, Genin C, Garraud O. Identification of Germinal Center B Cells in Blood from HIV-infected Drug-naive Individuals in Central Africa. Clin Dev Immunol. 2004;11:23–27. doi: 10.1080/10446670410001670454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Longwe H, Gordon S, Malamba R, French N. Characterising B cell numbers and memory B cells in HIV infected and uninfected Malawian adults. BMC Infect Dis. 2010;10:280. doi: 10.1186/1471-2334-10-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eggena MP, Barugahare B, Okello M, Mutyala S, Jones N, Ma Y, Kityo C, Mugyenyi P, Cao H. T Cell Activation in HIV-Seropositive Ugandans: Differential Associations with Viral Load, CD4 + T Cell Depletion, and Coinfection. J Infect Dis. 2005;191:694–701. doi: 10.1086/427516. [DOI] [PubMed] [Google Scholar]
- 33.Roetynck S, Olotu A, Simam J, Marsh K, Stockinger B, Urban B, Langhorne J. Phenotypic and Functional Profiling of CD4 T Cell Compartment in Distinct Populations of Healthy Adults with Different Antigenic Exposure. PLoS One. 2013;8:e55195. doi: 10.1371/journal.pone.0055195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monath TP, Nichols R, Archambault WT, Moore L, Marchesani R, Tian J, Shope RE, Thomas N, Schrader R, Furby D, Bedford P. Comparative safety and immunogenicity of two yellow fever 17D vaccines (ARILVAX and YF-VAX) in a phase III multicenter, double-blind clinical trial. Am J Trop Med Hyg. 2002;66:533–41. doi: 10.4269/ajtmh.2002.66.533. [DOI] [PubMed] [Google Scholar]
- 35.Muyanja E, Ssemaganda A, Ngauv P, Cubas R, Perrin H, Srinivasan D, Canderan G, Lawson B, Kopycinski J, Graham AS, Rowe DK, Smith MJ, Isern S, Michael S, Silvestri G, Vanderford TH, Castro E, Pantaleo G, Singer J, Gillmour J, Kiwanuka N, Nanvubya A, Schmidt C, Birungi J, Cox J, Haddad EK, Kaleebu P, Fast P, Sekaly RP, Trautmann L. Immune activation alters cellular and humoral responses to yellow fever 17D vaccine. J Clin Invest. 2014;124:3147–3158. doi: 10.1172/JCI75429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meier A, Chang JJ, Chan ES, Pollard RB, Sidhu HK, Kulkarni S, Wen TF, Lindsay RJ, Orellana L, Mildvan D, Bazner S, Streeck H, Alter G, Lifson JD, Carrington M, Bosch RJ, Robbins GK, Altfeld M. Sex differences in the Toll-like receptor–mediated response of plasmacytoid dendritic cells to HIV-1. Nat Med. 2009;15:955–959. doi: 10.1038/nm.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hagen S, Altfeld M. The X awakens: multifactorial ramifications of sex-specific differences in HIV-1 infection. J virus Erad. 2016;2:78–81. [PMC free article] [PubMed] [Google Scholar]
- 38.van Loggerenberg F, Mlisana K, Williamson C, Auld SC, Morris L, Gray CM, Karim QA, Grobler A, Barnabas N, Iriogbe I, Abdool Karim SS. Establishing a cohort at high risk of HIV infection in South Africa: Challenges and experiences of the CAPRISA 002 acute infection study. PLoS One. 2008;3:1–8. doi: 10.1371/journal.pone.0001954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mlisana K, Werner L, Garrett NJ, McKinnon LR, Van Loggerenberg F, Passmore JAS, Gray CM, Morris L, Williamson C, AbdoolKarim SS. Rapid disease progression in HIV-1 subtype c-infected South African women. Clin Infect Dis. 2014;59:1322–1331. doi: 10.1093/cid/ciu573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abdool KQ, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, Kharsany AB, Sibeko S, Mlisana KP, Omar Z, Gengiah TN, Maarschalk S, Arulappan N, Mlotshwa M, Morris L, Taylor D on behalf of the CAPRISA 004 Trial Group. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moir S, Fauci AS. B cells in HIV infection and disease. Nat Rev Immunol. 2009;9:235–245. doi: 10.1038/nri2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deeks SG, Kitchen CMR, Liu L, Guo H, Gascon R, Narváez AB, Hunt P, Martin JN, Kahn JO, Levy J, McGrath MS, Hecht FM. Immune activation set point during early HIV infection predicts subsequent CD4+ T-cell changes independent of viral load. Blood. 2004;104:942–7. doi: 10.1182/blood-2003-09-3333. [DOI] [PubMed] [Google Scholar]
- 43.Hunt PW, Martin JN, Sinclair E, Bredt B, Hagos E, Lampiris H, Deeks SG. T cell activation is associated with lower CD4+ T cell gains in human immunodeficiency virus-infected patients with sustained viral suppression during antiretroviral therapy. J Infect Dis. 2003;187:1534–43. doi: 10.1086/374786. [DOI] [PubMed] [Google Scholar]
- 44.Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, Blazar BR, Rodriguez B, Teixeira-Johnson L, Landay A, Martin JN, Hecht FM, Picker LJ, Lederman MM, Deeks SG, Douek DC. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2007;12:1365–1371. doi: 10.1038/nm1511. [DOI] [PubMed] [Google Scholar]
- 45.Moir S, Fauci AS. Insights into B cells and HIV-specific B-cell responses in HIV-infected individuals. Immunol Rev. 2013;254:207–224. doi: 10.1111/imr.12067. [DOI] [PubMed] [Google Scholar]
- 46.Ho J, Moir S, Malaspina A, Howell ML, Wang W, DiPoto AC, O’Shea MA, Roby GA, Kwan R, Mican JM, Chun TW, Fauci AS. Two overrepresented B cell populations in HIV-infected individuals undergo apoptosis by different mechanisms. Proc Natl Acad Sci. 2006;103:19436–19441. doi: 10.1073/pnas.0609515103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Titanji K, Chiodi F, Bellocco R, Schepis D, Osorio L, Tassandin C, Tambussi G, Grutzmeier S, Lopalco L, De Milito A. Primary HIV-1 infection sets the stage for important B lymphocyte dysfunctions. AIDS. 2005;19:1947–1955. doi: 10.1097/01.aids.0000191231.54170.89. [DOI] [PubMed] [Google Scholar]
- 48.Moir S, Malaspina A, Li Y, Chun TW, Lowe T, Adelsberger J, Baseler M, Ehler LA, Liu S, Davey RT, Mican JA, Fauci AS. B cells of HIV-1-infected patients bind virions through CD21-complement interactions and transmit infectious virus to activated T cells. J Exp Med. 2000;192:637–46. doi: 10.1084/jem.192.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qiao X, He B, Chiu A, Knowles DM, Chadburn A, Cerutti A. Human immunodeficiency virus 1 Nef suppresses CD40-dependent immunoglobulin class switching in bystander B cells. Nat Immunol. 2006;7:302–310. doi: 10.1038/ni1302. [DOI] [PubMed] [Google Scholar]
- 50.Xu W, Santini PA, Sullivan JS, He B, Shan M, Ball SC, Dyer WB, Ketas TJ, Chadburn A, Cohen-Gould L, Knowles DM, Chiu A, Sanders RW, Chen K, Cerutti A. HIV-1 evades virus-specific IgG2 and IgA responses by targeting systemic and intestinal B cells via long-range intercellular conduits. Nat Immunol. 2009;10:1008–1017. doi: 10.1038/ni.1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruffin N, HongThang P, Rethi B, Nilsson A, Chiodi F. The impact of inflammation and immune activation on B cell differentiation during HIV-1 infection. Front Immunol. 2012;2:1–7. doi: 10.3389/fimmu.2011.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fontaine J, Chagnon-Choquet J, Valcke HS, Poudrier J, Roger M. High expression levels of B lymphocyte stimulator (BLyS) by dendritic cells correlate with HIV-related B-cell disease progression in humans. Blood. 2011;117:145–155. doi: 10.1182/blood-2010-08-301887. [DOI] [PubMed] [Google Scholar]
- 53.Poudrier J, Soulas C, Chagnon-Choquet J, Burdo T, Autissier P, Oskar K, Williams KC, Roger M. High Expression Levels of BLyS/BAFF by Blood Dendritic Cells and Granulocytes Are Associated with B-cell dysregulation in SIV-Infected Rhesus Macaques. PLoS One. 2015;10:e0131513. doi: 10.1371/journal.pone.0131513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gomez AM, Ouellet M, Deshiere A, Breton Y, Tremblay MJ. HIV-1-Mediated BAFF Secretion in Macrophages Does Not Require Endosomal TLRs, Type-I IFN, and Nef, but Depends on the Cellular Phenotype Status. J Immunol. 2016;196:3806–3817. doi: 10.4049/jimmunol.1501249. [DOI] [PubMed] [Google Scholar]
- 55.Jiang W. Microbial Translocation and B Cell Dysfunction in Human Immunodeficiency Virus Disease. Am J Immunol. 2012;8:44–51. doi: 10.3844/ajisp.2012.44.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hornung V, Rothenfusser S, Britsch S, Krug A, Jahrsdorfer B, Giese T, Endres S, Hartmann G. Quantitative Expression of Toll-Like Receptor 1–10 mRNA in Cellular Subsets of Human Peripheral Blood Mononuclear Cells and Sensitivity to CpG Oligodeoxynucleotides. J Immunol. 2002;168:4531–4537. doi: 10.4049/jimmunol.168.9.4531. [DOI] [PubMed] [Google Scholar]
- 57.Jiang W, Lederman MM, Hunt P, Sieg SF, Haley K, Rodriguez B, Landay A, Martin J, Sinclair E, Asher AI, Deeks SG, Douek DC, Brenchley JM. Plasma levels of bacterial DNA correlate with immune activation and the magnitude of immune restoration in persons with antiretroviral-treated HIV infection. J Infect Dis. 2009;199:1177–85. doi: 10.1086/597476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.He B, Qiao X, Cerutti A. CpG DNA induces IgG class switch DNA recombination by activating human B cells through an innate pathway that requires TLR9 and cooperates with IL-10. J Immunol. 2004;173:4479–4491. doi: 10.4049/jimmunol.173.7.4479. [DOI] [PubMed] [Google Scholar]
- 59.Jiang W, Lederman MM, Harding CV, Rodriguez B, Mohner RJ, Sieg SF. TLR9 stimulation drives naive B cells to proliferate and to attain enhanced antigen presenting function. Eur J Immunol. 2007;37:2205–2213. doi: 10.1002/eji.200636984. [DOI] [PubMed] [Google Scholar]
- 60.Noronha AM, Liang Y, Hetzel JT, Hasturk H, Kantarci A, Stucchi A, Zhang Y, Nikolajczyk BS, Farraye FA, Ganley-Leal LM. Hyperactivated B cells in human inflammatory bowel disease. J Leukoc Biol. 2009;86:1007–1016. doi: 10.1189/jlb.0309203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.d’Ettorre G, Baroncelli S, Micci L, Ceccarelli G, Andreotti M, Sharma P, Fanello G, Fiocca F, Cavallari EN, Giustini N, Mallano A, Galluzzo CM, Vella S, Mastroianni CM, Silvestri G, Paiardini M, Vullo V. Reconstitution of Intestinal CD4 and Th17 T Cells in Antiretroviral Therapy Suppressed HIV-Infected Subjects: Implication for Residual Immune Activation from the Results of a Clinical Trial. PLoS One. 2014;9:e109791. doi: 10.1371/journal.pone.0109791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hattab S, Guihot A, Guiguet M, Fourati S, Carcelain G, Caby F, Marcelin A, Autran B, Costagliola D, Katlama C. Comparative impact of antiretroviral drugs on markers of inflammation and immune activation during the first two years of effective therapy for HIV-1 infection: an observational study. BMC Infect Dis. 2014;14:122. doi: 10.1186/1471-2334-14-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rudy BJ, Kapogiannis BG, Worrell C, Squires K, Bethel J, Li S, Wilson CM, Agwu A, Emmanuel P, Price G, Hudey S, Goodenow MM, Sleasman JW. Immune Reconstitution but Persistent Activation After 48 Weeks of Antiretroviral Therapy in Youth With Pre-Therapy CD4 >350 in ATN 061. J Acquir Immune Defic Syndr. 2015;69:52–60. doi: 10.1097/QAI.0000000000000549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Haas A, Zimmermann K, Oxenius A. Antigen-Dependent and -Independent Mechanisms of T and B Cell Hyperactivation during Chronic HIV-1 Infection. J Virol. 2011;85:12102–12113. doi: 10.1128/JVI.05607-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Amu S, Fievez V, Nozza S, Lopalco L, Chiodi F. Dysfunctions in the migratory phenotype and properties of circulating immature transitional B cells during HIV-1 infection. AIDS. 2016;30:2169–2177. doi: 10.1097/QAD.0000000000001182. [DOI] [PubMed] [Google Scholar]
- 66.Pensieroso S, Cagigi A, Palma P, Nilsson A, Capponi C, Freda E, Bernardi S, Thorstensson R, Chiodi F, Rossi P. Timing of HAART defines the integrity of memory B cells and the longevity of humoral responses in HIV-1 vertically-infected children. Proc Natl Acad Sci. 2009;106:7939–7944. doi: 10.1073/pnas.0901702106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Van Epps P, Matining RM, Tassiopoulos K, Anthony DD, Landay A, Kalayjian RC, Canaday DH. Older Age Is Associated with Peripheral Blood Expansion of Naïve B Cells in HIV-Infected Subjects on Antiretroviral Therapy. PLoS One. 2014;9:e107064. doi: 10.1371/journal.pone.0107064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Levesque MC, Moody MA, Hwang KK, Marshall DJ, Whitesides JF, Amos JD, Gurley TC, Allgood S, Haynes BB, Vandergrift NA, Plonk S, Parker DC, Cohen MS, Tomaras GD, Goepfert PA, Shaw GM, Schmitz JE, Eron JJ, Shaheen NJ, Hicks CB, Liao HX, Markowitz M, Kelsoe G, Margolis DM, Haynes BF. Polyclonal B Cell Differentiation and Loss of Gastrointestinal Tract Germinal Centers in the Earliest Stages of HIV-1 Infection. PLoS Med. 2009;6:e1000107. doi: 10.1371/journal.pmed.1000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Klatt NR, Funderburg NT, Brenchley JM. Microbial translocation, immune activation, and HIV disease. Trends Microbiol. 2013;21:6–13. doi: 10.1016/j.tim.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ghislain M, Bastard J, Meyer L, Capeau J, Fellahi S, Gérard L, May T, Simon A, Vigouroux C, Goujard C. Late Antiretroviral Therapy (ART) Initiation Is Associated with Long-Term Persistence of Systemic Inflammation and Metabolic Abnormalities. PLoS One. 2015;10:e0144317. doi: 10.1371/journal.pone.0144317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fogli M, Torti C, Malacarne F, Fiorentini S, Albani M, Izzo I, Giagulli C, Maggi F, Carosi G, Caruso A. Emergence of Exhausted B Cells in Asymptomatic HIV-1-Infected Patients Naïve for HAART is Related to Reduced Immune Surveillance. Clin Dev Immunol. 2012;2012:1–10. doi: 10.1155/2012/829584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wheatley AK, Kristensen AB, Lay WN, Kent SJ. HIV-dependent depletion of influenza-specific memory B cells impacts B cell responsiveness to seasonal influenza immunisation. Sci Rep. 2016;6:26478. doi: 10.1038/srep26478. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.