Abstract
BACKGROUND:
This meta-analysis aimed to determine whether extracorporeal cardiopulmonary resuscitation (ECPR), compared with conventional cardiopulmonary resuscitation (CCPR), improves outcomes in adult patients with cardiac arrest (CA).
DATA RESOURCES:
PubMed, EMBASE, Web of Science, and China Biological Medicine Database were searched for relevant articles. The baseline information and outcome data (survival, good neurological outcome at discharge, at 3–6 months, and at 1 year after CA) were collected and extracted by two authors. Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using Review Manager 5.3.
RESULTS:
In six studies 2 260 patients were enrolled to study the survival rate to discharge and long-term neurological outcome published since 2000. A significant effect of ECPR was observed on survival rate to discharge compared to CCPR in CA patients (RR 2.37, 95%CI 1.63–3.45, P<0.001), and patients who underwent ECPR had a better long-term neurological outcome than those who received CCPR (RR 2.79, 95%CI 1.96–3.97, P<0.001). In subgroup analysis, there was a significant difference in survival to discharge favoring ECPR over CCPR group in OHCA patients (RR 2.69, 95%CI 1.48–4.91, P=0.001). However, no significant difference was found in IHCA patients (RR 1.84, 95%CI 0.91–3.73, P=0.09).
CONCLUSION:
ECPR showed a beneficial effect on survival rate to discharge and long-term neurological outcome over CCPR in adult patients with CA.
Keywords: Extracorporeal cardiopulmonary resuscitation, Cardiac arrest, Adult, Outcome, Meta-analysis
INTRODUCTION
Cardiac arrest (CA) is a major health concern, and the survival rate of such patients remains very low despite early access to emergency medical care and improvement in treatment.[1] Cardiopulmonary resuscitation (CPR) has been the treatment of choice for CA with a better survival.[2] Previous studies revealed a low survival to discharge rate ranging from 7% to 26%, which declines rapidly if the duration of CPR exceeds 10 minutes and dramatically after 30 minutes.[3]
Conventional CPR (CCPR) for patients with CA aims to achieve a neurologically intact survival. However, CCPR provides only 30% to 40% of normal blood flow to the brain even when delivered according to guidelines.[4] In many CA patients, there is a failure to have a return of spontaneous circulation (ROSC) despite advanced cardiac life support and this is often in the setting of severe metabolic acidosis, acute blockage of a coronary artery or massive pulmonary embolism.[5] In refractory CA, extracorporeal membrane oxygenation (ECMO)-assisted CPR is used for both in-hospital CA (IHCA) and out-of-hospital CA (OHCA).[3]
Extracorporeal CPR (ECPR) is a technique to circulate blood outside the body with extracorporeal oxygenation and to support the body’s circulation in the absence of an adequately functioning cardiac pump.[6] Observation studies[7–12] have shown an improved survival rate and better neurological preservation after CA in patients receiving ECPR compared to CCPR. ECPR is a valuable option for CA and that it should be initiated as soon as possible when CA is considered to be refractory to CCPR.[3] On the basis of these findings, the 2015 American Heart Association guidelines for CPR mentioned that ECPR may be considered for selecting patients for whom the suspected etiology of CA was potentially reversible during a limited period of mechanical cardiorespiratory support (Class IIb).[13]
Thus, this meta-analysis collected and reviewed previously reported studies to further evaluate the survival rate and neurological outcome of CA patients receiving ECPR compared with CCPR.
METHODS
This study was performed according to the guidelines of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement (S1 PRISMA Checklist).
Study design
This study encompassed a review of the previous relevant medical literature. The primary end point of this study was the survival rate to discharge of patients receiving ECPR or CCPR. The secondary end point was long-term neurological outcome as determined by the Glasgow-Pittsburgh cerebral-performance categories (CPC) score.
Data source and search strategy
Potentially relevant studies were identified and screened for retrieval by a thesaurus search. PubMed, EMBASE, Web of Science, and China Biological Medicine Database were searched for relevant articles with search terms “(Extracorporeal Membrane Oxygenation or ECMO or Extracorporeal cardiopulmonary resuscitation or ECPR) and (cardiac arrest or CA or cardiopulmonary arrest)”. The “related citations” option in PubMed, as well as reference lists of all retrieved studies, was checked to search for other relevant articles that were not initially identified. The last research updated on December 19, 2015. The entire literature search was performed by two independent researchers.
Study selection
Observational studies examining at least 15 adult patients who received ECPR for CA were included. To keep the search current, only studies published in 2000 or later were included. Furthermore, studies that did not include survival to discharge or CPC status as endpoints were excluded. When institutions published duplicate studies with accumulating sample size or increased length of follow-up, only the most recent complete reports were included. All studies were limited to those with human subjects and published in the English language. Case reports, case series, letters, conference presentations, editorials, and expert opinions were excluded. Review articles also were excluded due to potential publication bias and duplication of studies.
Data extraction
All data were extracted from article texts, tables, and figures. The two of the authors independently reviewed data from each relevant study. Disagreements were reconciled through group discussion and a final consensus was reached on all items. For each study, the following information was collected: the first author’s name, year of publication, region, location of CA, survival rate at discharge, long-term neurological outcome, CPR duration (defined as the interval from initiation of CPR to ROSC or death in CCPR and as the interval from CPR to ECMO in ECPR), etiology, and initial cardiac rhythm. The Newcastle-Ottawa Scale (NOS) was used for assessing the quality of included observational studies in this meta-analysis. A “star system” has been developed in which a study is judged on three broad perspectives: the selection of the study groups; the comparability of the groups; and the ascertainment of the outcome of observational studies. In this system, 9 stars represent the highest level and those studies that get 6 stars are of high quality.
Statistical analysis
Heterogeneity among studies was quantified with the I2 metric, which is independent of the number of studies in a meta-analysis. I2 takes values between 0% and 100%, with higher values denoting a greater degree of heterogeneity, and I2>50% indicates significant heterogeneity between the studies.[14] Based on the test of heterogeneity, along with the 95% confidence interval (CI) to measure the strength of the effect, the pooled risk ratio (RR) was calculated using the fixed-effects model when lacking of heterogeneity while random-effects modeling was adopted when heterogeneity existed. All P values were two tailed and P<0.05 was considered statistically significant. Publication bias was estimated by the visual inspection of funnel plot, Begg’s test and Egger’s regression test (P<0.05 was considered representative of statistically significant publication bias). Data were analyzed and processed using Review Manager software 5.3 (The Cochrane Collaboration, Oxford, United Kingdom) and STATA 12.0 software (StataCorp, College Station, TX, USA).
RESULTS
Eligible studies and characteristics of included studies
A total of 660 relevant articles were identified by the literature search, six of which met the inclusion criteria. Of the 554 excluded studies, 197 were unable to meet predefined research purposes, 212 were studies of pediatric patients, 80 were review articles, 131 were case reports or case series or letters, 24 were animal studies, 4 were lack of detailed description and 6 were duplicate publications. A flow diagram schematized the process of selecting and excluding articles with specific reasons (Figure 1). Finally, 6 studies were included in the meta-analysis comprising 2 260 CA patients, in which 376 and 1 884 patients received ECPR and CCPR respectively.[7–12] Those included were all 7-star or 8-star studies according to the NOS grade, suggesting high literature methodology quality. The detailed characteristics of the included studies were shown in Table 1.
Figure 1.
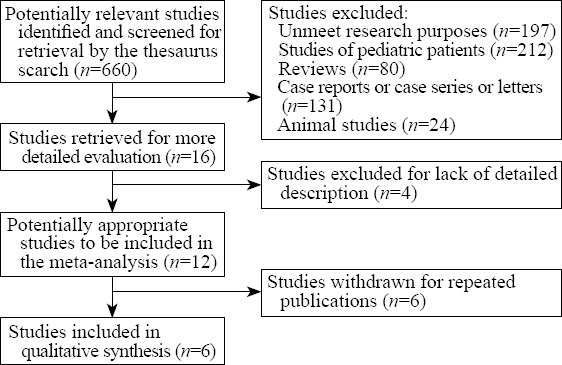
The flow chart of the selected articles.
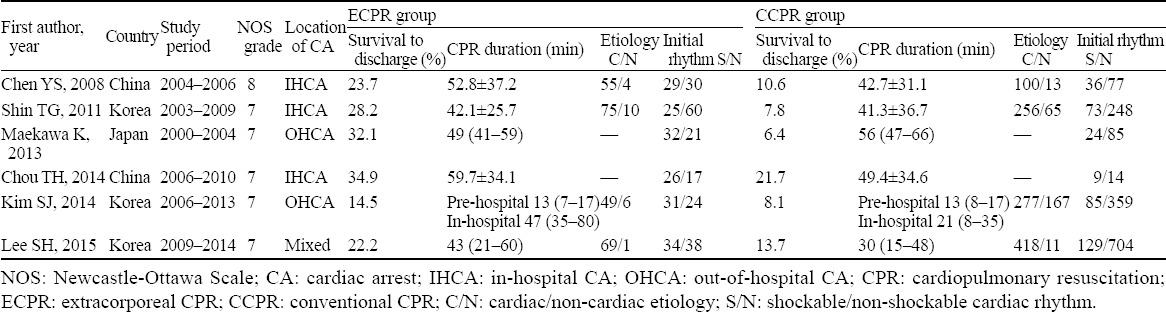
Table 1.
Characteristics of included studies
Survival rate at discharge
Data on survival rate to discharge were available from 6 studies, and the primary end point was used to calculate the overall pooled RR. There was a significant heterogeneity among included studies (I2=51%). Therefore, the random-effects model was used for calculating the pooled RR for survival discharge rate. The results indicated that there was a significant effect of ECPR on survival rate to discharge compared with CCPR in CA patients (RR 2.37, 95%CI 1.63–3.45, P<0.001) (Figure 2).
Figure 2.
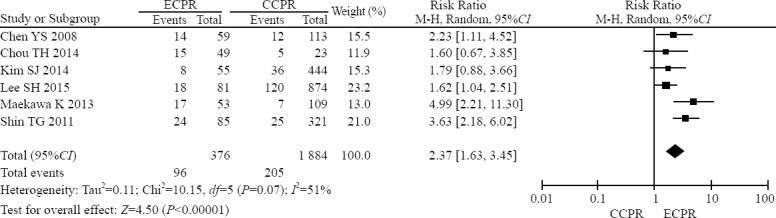
Forest plot of the comparison of ECPR with CCPR in CA patients on the survival rate to discharge.
Long-term neurological outcome
Two studies reported CPC≤2 at 3 months as the long-term neurological outcome,[9,11] and another two studies reported CPC≤2 at 6 months[8] and 1 year[7] respectively. All four studies included were used to calculate the effect of ECPR on long-term neurological outcome in CA patients. As shown in Figure 3, there was a lack of significant heterogeneity (I2=41%), and the fixed-effects model was used. It was found that patients who underwent ECPR had a significant better long-term neurological outcome than those who received CCPR (RR 2.79, 95%CI 1.96–3.97, P<0.001).
Figure 3.
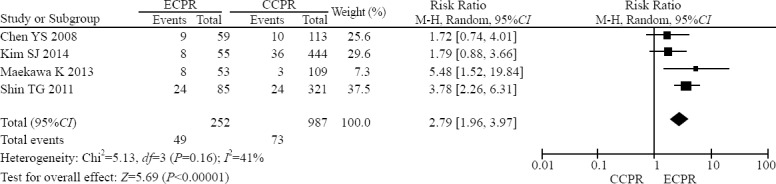
Forest plot of the comparison of ECPR with CCPR in CA patients on the long-term neurological outcome.
Subgroup and sensitivity analysis
In consideration of the significant heterogeneity observed, the sensitivity analysis was performed to investigate the influence of a single study on the overall meta-analysis estimate. Under the sensitivity analysis, the influence of each study on the pooled RR was examined by repeating the meta-analysis while omitting each study, one at a time. This procedure demonstrated that our results were reliable and robust (data not shown). A predefined subgroup analysis was performed according to the location of CA (IHCA or OHCA). Four studies were selected from the subgroup of IHCA[7,8,10,12] and three studies from the subgroup of OHCA.[9, 11, 12] There was a significant difference in survival to discharge favoring ECPR over CCPR group in OHCA patients (RR 2.69, 95%CI 1.48–4.91, P=0.001) (Figure 4). However, no significant difference was found in IHCA patients (RR 1.84, 95%CI 0.91–3.73, P=0.09).
Figure 4.
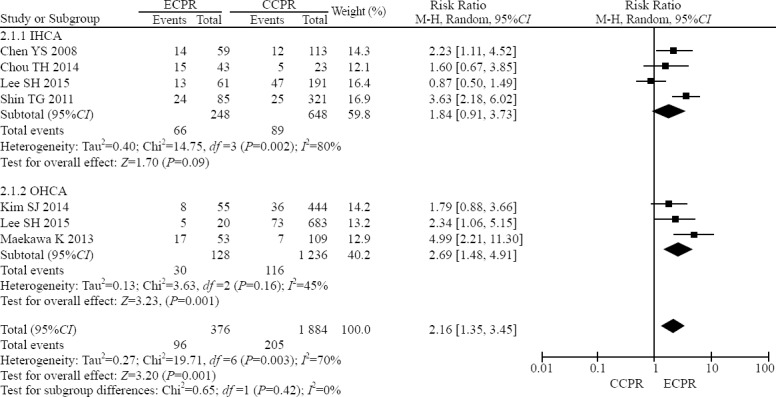
Forest plot of subgroup analysis of the comparison of ECPR with CCPR in CA patients on the survival rate to discharge.
Publication bias
Funnel plot for studies of the comparison of ECPR with CCPR in CA patients on the survival rate to discharge and the long-term neurological outcome failed to denote significant bias (Figure 5). Begg’s test revealed that there was no statistical evidence of publication bias among studies (P=0.851 for survival discharge rate and P=1.000 for long-term neurological outcome, respectively). Egger’s regression test showed that there was no publication bias in the statistical results either (P=0.725 and 0.880, respectively).
Figure 5.
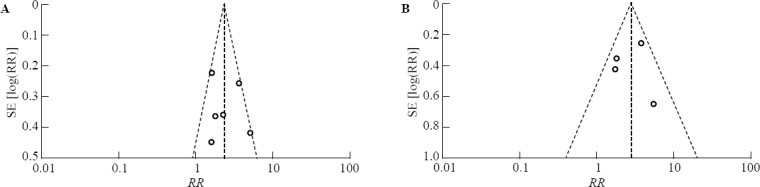
Funnel plot for studies of the comparison of ECPR with CCPR in CA patients on the survival rate to discharge (A), and the long-term neurological outcome (B). The horizontal and vertical axes correspond to the RR and confidence limits. RR: risk ratio; SE: standard error.
DISCUSSION
Despite advances in management, outcomes for both IHCA and OHCA remain poor. IHCA treated with CCPR typically has a survival rate of 15%–17% and OHCA survival is even lower than 8%–10%.[15] The worst outcomes are in patients with prolonged time to ROSC. Several factors are related to the outcomes, including immediate recognition of CA, early CPR, rapid defibrillation, initial rhythm, underlying cause of CA, duration of CPR and initial resuscitation effort as well as integrated post-CA care.[16] Because cerebral blood flow is insufficient during CPR, there is the possibility of ECPR using a cardiopulmonary support device for the recovery of neurological function. ECPR was introduced in the 1960s to improve neurological outcomes.[17] Recently, observational studies have reported an association between ECPR and improved survival. The present study provides a current review of survival to discharge and long-term neurological outcome for CA patients who have received ECPR compared with CCPR.
In this study, there were significant effects of ECPR on survival rate to discharge and long-term neurological outcome compared with CCPR in CA patients, and the survival rate to discharge overall was 25.5%. This finding is comparable to previous studies. According to the Extracorporeal Life Support Organization (ELSO) registry, the survival rate of adult patients receiving ECPR for CA was 27% between 1990 and 2012.[18] And a recent meta-analysis in 135 patients from 1990 to 2007 showed a hospital survival rate to discharge with ECPR of 40%.[19]
In our study, ECPR represents a treatment option in CA adults rescuing 19.4% of patients with good long-term neurological outcome. The field of CPR-assisted with more invasive strategies is currently investigated regarding different aspects, including ECMO, hypothermia, mechanical CPR with chest compression systems and also early reperfusion in the catheterization laboratory.[20] Stub et al[5] presented the CHEER-trial (mechanical CPR, hypothermia, ECMO and early reperfusion) showing the feasibility of such an invasive protocol in a single center with high survival rates (54%). Also the SAVE-J study revealed an improved neurological outcome in patients with OHCA with shockable rhythm treated by a treatment bundle including ECPR, therapeutic hypothermia and intra-aortic balloon pump.[17] Further large studies implementing such strategies are warranted.
The present study demonstrated a better survival to discharge outcome using ECPR for OHCA compared with CCPR. However, beneficial effects were not found in IHCA patients receiving ECPR. Survival rates for ECPR for IHCA were higher than OHCA (26.6% vs. 23.4%). This finding is in line with several recent retrospective studies presenting survival rates of 26%–39% for IHCA. Expectedly, survival for OHCA is inferior with a reported rate of 4%–39%.[20] Distinct differences between the subgroup analyses were evident: patients following IHCA were older and had more comorbidities but patients with OHCA had more initial shockable rhythm indicating that the comparability of these groups is limited. Also patients post-surgery or post-interventional were characterized by a worse prognosis.[20] Furthermore, this difference is probably related to the duration of CA, which seems to be more important than the location of CA. IHCA patients are much more likely to have witnessed CA with a shorter duration to achieve advanced cardiac life support, and with a shorter time until start of ECPR and that comorbidities are known to the treating physician implicating a bias in decision for ECMO implantation.[15]
Several observational studies have found variable improvements in mortality with the use of ECPR. Haneya et al[21] compared ECPR initiated in the ED for OHCA with ECPR initiated for IHCA, and found a survival rate of 42% for IHCA patients versus only 15% for OHCA patients. While an optimistic estimate of survival from OHCA with the use of ECPR may be in the 15%–20% range, the critical factor that determines success appears to be the duration from the onset of arrest to achieving ECMO flow.[15] This may be why IHCA studies have generally reported better outcomes.[22] When ECPR can be initiated rapidly, the outcomes for OHCA may be similar to those seen with IHCA patients.[23] Moreover, the present study demonstrated survival with a favorable CPC score in 19.4% of those with ECPR versus 7.4% with CCPR. ECPR may provide a tool to improve survival with good neurologic outcomes when initiated early in selected patients.
The present meta-analysis should be interpreted within the context of its limitations. Firstly, we present data of comparably cohorts with different long-term outcomes but with retrospective data collection. However, some data regarding CPR circumstances such as exact etiology of CA are incomplete. Secondly, although there were clear in- and exclusion criteria regarding patient selection, these criteria were ignored in several patients on an individual basis. Data collection following ECPR initiation was heterogeneous. Further meta-regression will be required to explore the source of heterogeneity. Thirdly, although no publication bias was found in Begg’s test and Egger’s regression test from the present meta-analysis, we cannot exclude this probability because some null and unexpected results may not be published. As any other meta-analysis of published results, the quality of the present meta-analysis depends on that of individual studies.
CONCLUSION
The present meta-analysis suggested that ECPR showed a survival benefit both on survival rate to discharge and on long-term neurological outcome over CCPR in patients with CA. Future randomized studies need to determine the role of ECPR in different settings and multicenter registries need to explore long-term neurological prognosis and risk prediction possibilities.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: There is no conflict of interest related to this study.
Contributors: Wang GN proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Zhao Y, Xing J, Du Z, Liu F, Jia M, Hou X. Extracorporeal cardiopulmonary resuscitation for adult patients who underwent post-cardiac surgery. Eur J Med Res. 2015;20:83. doi: 10.1186/s40001-015-0179-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blewer AL, Buckler DG, Li J, Leary M, Becker LB, Shea JA, et al. Impact of the 2010 resuscitation guidelines training on layperson chest compressions. World J Emerg Med. 2015;6(4):270–6. doi: 10.5847/wjem.j.1920-8642.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fagnoul D, Combes A, De Backer D. Extracorporeal cardiopulmonary resuscitation. Curr Opin Crit Care. 2014;20(3):259–65. doi: 10.1097/MCC.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 4.Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality:improving cardiac resuscitation outcomes both inside and outside the hospital:a consensus statement from the American Heart Association. Circulation. 2013;128(4):417–35. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 5.Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial) Resuscitation. 2015;86:88–94. doi: 10.1016/j.resuscitation.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Mochizuki K, Imamura H, Iwashita T, Okamoto K. Neurological outcomes after extracorporeal cardiopulmonary resuscitation in patients with out-of-hospital cardiac arrest:a retrospective observational study in a rural tertiary care center. J Intensive Care. 2014;2(1):33. doi: 10.1186/2052-0492-2-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest:an observational study and propensity analysis. Lancet. 2008;372(9638):554–61. doi: 10.1016/S0140-6736(08)60958-7. [DOI] [PubMed] [Google Scholar]
- 8.Shin TG, Choi JH, Jo IJ, Sim MS, Song HG, Jeong YK, et al. Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest:A comparison with conventional cardiopulmonary resuscitation. Crit Care Med. 2011;39(1):1–7. doi: 10.1097/CCM.0b013e3181feb339. [DOI] [PubMed] [Google Scholar]
- 9.Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin:a propensity-matched study and predictor analysis. Crit Care Med. 2013;41(5):1186–96. doi: 10.1097/CCM.0b013e31827ca4c8. [DOI] [PubMed] [Google Scholar]
- 10.Chou TH, Fang CC, Yen ZS, Lee CC, Chen YS, Ko WJ, et al. An observational study of extracorporeal CPR for in-hospital cardiac arrest secondary to myocardial infarction. Emerg Med J. 2014;31(6):441–7. doi: 10.1136/emermed-2012-202173. [DOI] [PubMed] [Google Scholar]
- 11.Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest:a propensity-matched study. Crit Care. 2014;18(5):535. doi: 10.1186/s13054-014-0535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SH, Jung JS, Lee KH, Kim HJ, Son HS, Sun K. Comparison of Extracorporeal Cardiopulmonary Resuscitation with Conventional Cardiopulmonary Resuscitation:Is Extracorporeal Cardiopulmonary Resuscitation Beneficial? Korean J Thorac Cardiovasc Surg. 2015;48(5):318–27. doi: 10.5090/kjtcs.2015.48.5.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks SC, Anderson ML, Bruder E, Daya MR, Gaffney A, Otto CW, et al. Part 6:Alternative Techniques and Ancillary Devices for Cardiopulmonary Resuscitation:2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S436–43. doi: 10.1161/CIR.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mosier JM, Kelsey M, Raz Y, Gunnerson KJ, Meyer R, Hypes CD, et al. Extracorporeal membrane oxygenation (ECMO) for critically ill adults in the emergency department:history, current applications, and future directions. Crit Care. 2015;19:431. doi: 10.1186/s13054-015-1155-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blumenstein J, Leick J, Liebetrau C, Kempfert J, Gaede L, Groß S, et al. Extracorporeal life support in cardiovascular patients with observed refractory in-hospital cardiac arrest is associated with favourable short and long-term outcomes:A propensity-matched analysis. Eur Heart J Acute Cardiovasc Care. 2015 Oct 26;:2048872615612454. doi: 10.1177/2048872615612454. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Zhuo CN, Zhang L, Gong YS, Yin CL, Li YQ. Performance of cardiopulmonary resuscitation during prolonged basic life support in military medical university students:A manikin study. World J Emerg Med. 2015;6(3):179–85. doi: 10.5847/wjem.j.1920-8642.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paden ML, Conrad SA, Rycus PT, Thiagarajan RR. Extracorporeal Life Support Organization Registry Report 2012. ASAIO J. 2013;59(3):202–10. doi: 10.1097/MAT.0b013e3182904a52. [DOI] [PubMed] [Google Scholar]
- 19.Cardarelli MG, Young AJ, Griffith B. Use of extracorporeal membrane oxygenation for adults in cardiac arrest (E-CPR):a meta-analysis of observational studies. ASAIO J. 2009;55(6):581–6. doi: 10.1097/MAT.0b013e3181bad907. [DOI] [PubMed] [Google Scholar]
- 20.Jung C, Janssen K, Kaluza M, Fuernau G, Poerner TC, Fritzenwanger M, et al. Outcome predictors in cardiopulmonary resuscitation facilitated by extracorporeal membrane oxygenation. Clin Res Cardiol. 2016;105(3):196–205. doi: 10.1007/s00392-015-0906-4. [DOI] [PubMed] [Google Scholar]
- 21.Haneya A, Philipp A, Diez C, Schopka S, Bein T, Zimmermann M, et al. A 5-year experience with cardiopulmonary resuscitation using extracorporeal life support in non-postcardiotomy patients with cardiac arrest. Resuscitation. 2012;83(11):1331–7. doi: 10.1016/j.resuscitation.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Ryu JA, Cho YH, Sung K, Choi SH, Yang JH, Choi JH, et al. Predictors of neurological outcomes after successful extracorporeal cardiopulmonary resuscitation. BMC Anesthesiol. 2015;15:26. doi: 10.1186/s12871-015-0002-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang CH, Chou NK, Becker LB, Lin JW, Yu HY, Chi NH, et al. Improved outcome of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest—a comparison with that for extracorporeal rescue for in-hospital cardiac arrest. Resuscitation. 2014;85(9):1219–24. doi: 10.1016/j.resuscitation.2014.06.022. [DOI] [PubMed] [Google Scholar]


