Abstract
Background
Dialysis facility performance measures to improve access to kidney transplantation are being considered. Referral of patients for kidney transplant evaluation by the dialysis facility is one potential indicator, but limited data exist to evaluate whether referral is associated with existing dialysis facility quality indicators.
Study Design
Cross-sectional study.
Setting & Participants
A total of 12,926 incident (7/05–9/11) adult (aged 18-69 years) patients treated at 241 dialysis facilities with complete quality indicator information, from US national registry data linked to transplant referral data from all three Georgia kidney transplant centers.
Factors
Facility performance on dialysis quality indicators (high, intermediate, and low tertiles).
Outcome
Percentages of patients referred within 1 year of dialysis initiation at dialysis facility.
Results
Overall, a median of 25.4% of patients were referred for kidney transplantation within 1 year of dialysis initiation. Higher facility-level referral was associated with better performance with respect to standardized transplantation ratio (high, 28.6%; intermediate, 25.1%; low, 22.9%; P=0.001) and percentage waitlisted (high, 30.7%; intermediate, 26.8%; low, 19.2%; P<0.001). Facility-level referral was not associated with indicators of quality of care associated with dialysis initiation, including percentage of incident patients being informed of transplant options. For most non–transplant-related indicators of high-quality care, including those capturing mortality, morbidity, and anemia management, better performance was not associated with higher facility-level transplant referral.
Limitations
Potential ecologic fallacy and residual confounding.
Conclusions
Transplant referral among patients at dialysis facilities does not appear to be associated with overall quality of dialysis care at the facility. Quality indicators related to kidney transplantation were positively associated with, but not entirely correspondent with, higher percentages of patients referred for kidney transplant evaluation from dialysis facilities. These results suggest that facility-level referral, which is within the control of the dialysis facility, may provide information about the quality of dialysis care beyond current indicators.
Keywords: quality of care, dialysis, kidney transplantation, referral, performance indicator, end-stage renal disease (ESRD), dialysis facility, pay-for-performance, renal replacement therapy (RRT), RRT modality, quality indicator
Although kidney transplantation is generally associated with better patient outcomes and lower costs than dialysis,1, 2 access remains low among dialysis patients, with <3% of end-stage renal disease (ESRD) patients receiving a transplant prior to initiating dialysis and <30% of prevalent ESRD patients having a functioning transplant.2 Despite this, there are currently no transplant-related pay-for-performance indicators in the Centers for Medicare & Medicaid Services (CMS) ESRD Quality Incentive Program (QIP).3 Potential performance measures intended to increase access to transplantation among dialysis patients were recently developed and proposed by a CMS Technical Expert Panel.4 For ESRD patients on dialysis, referral for a kidney transplant evaluation represents a necessary, early step in access to transplantation, over which dialysis providers likely exert tremendous influence5 (see also conceptual model, Figure 1). However, the selected measures, which are not yet endorsed, were limited to placement on the deceased donor waitlist, primarily due to lack of national data on transplant referral.
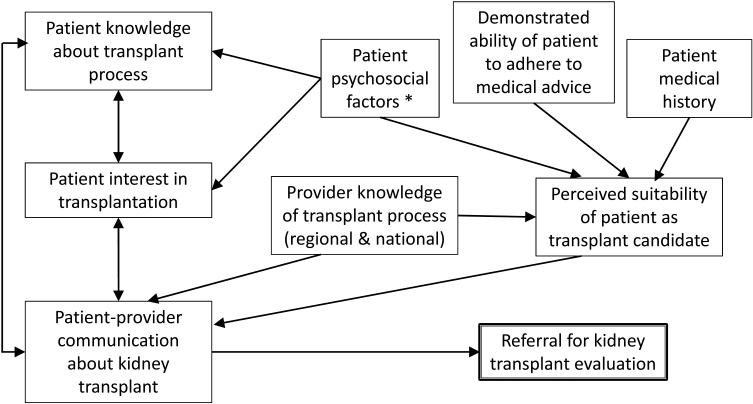
Figure 1.
Conceptual model of factors affecting referral of dialysis patients from dialysis facilities for kidney transplant evaluation. *Can include sociodemographics (e.g., age, sex, race/ethnicity), socioeconomic factors (education, employment, income), living/housing situation, psychological factors (e.g., depression, anxiety, stress), and social support.
We sought to address this gap and provide insight into whether dialysis facility–level transplant referral might provide new, valuable information about dialysis care, beyond that provided by current transplant-related and non–transplant-related indicators of high-quality dialysis care. We leveraged a novel source of data on referral for kidney transplant evaluation among Georgia dialysis patients6 to examine whether the percentage of patients referred from a dialysis facility was associated with other existing indicators of quality of dialysis care at the facility level. Secondarily, to help account for differences in patient characteristics across facilities, we also examined whether individual patient likelihood of being referred was related to quality of care at the treating dialysis facility.
Methods
Data Sources
Georgia Transplant Referral Data
Data were collected on all referrals for evaluation for kidney transplantation to all three adult transplant centers in Georgia in 2005-2012. Each center sent referral data securely to ESRD Network 6, which served as the data coordinating center.
United States Renal Data System
We linked these referral data to US Renal Data System (USRDS) data spanning 1/1/05 through 9/30/12. The USRDS is a national surveillance data system that includes data for all US treated ESRD patients.
Dialysis Facility Report
Dialysis Facility Report (DFR) data include facility-reported data on all publicly reported measures and are available for 2008–2011. Patients treated at transplant-only or Veterans Affairs dialysis facilities and patients who received ESRD therapy for <90 days are excluded from the aggregate measures in the DFR dataset.7
Data Linkage
Georgia referral data and USRDS data were linked using patient identifiers. The DFR data were linked to this merged dataset via unique dialysis facility provider numbers. Data collection and linkage were approved by Institutional Review Boards at Emory University (#56381), Augusta University (#889983), and Piedmont Hospital (#3675008). Referral data collection was retrospective and participant informed consent was waived.
Study Population
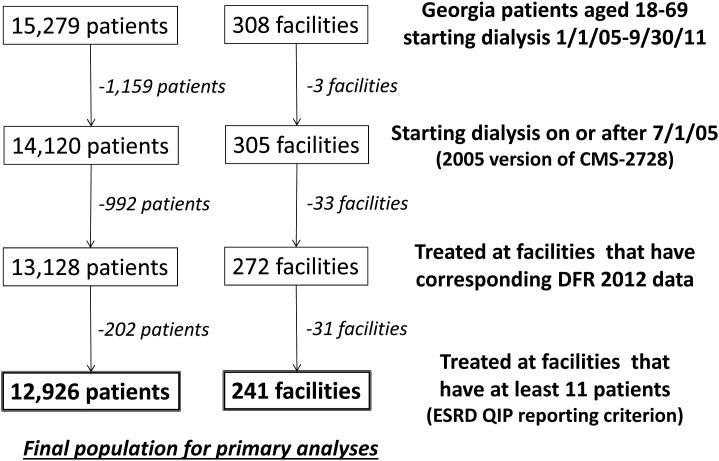
A total of 15,279 Georgia patients aged 18-69 who initiated dialysis at 308 facilities from 1/1/05 through 9/30/11 were identified from merged USRDS and Georgia referral data, as described in detail previously.6 Only patients initiating dialysis through 9/30/11 were included to allow for at least 1 year of potential follow-up for referral (through 9/30/12). From this initial population, the major reasons for excluding patients and facilities included those (n=1,159) who initiated dialysis before 7/1/05, when the 2005 version of the CMS ESRD Medical Evidence Report (CMS Form 2728) was fully adopted; facilities (n=33) that did not have corresponding DFR data; and facilities (n=31) that did not have at least 11 patients, the ESRD QIP criterion for performance reporting.3 After these and other exclusions, there were 12,926 patients and 241 facilities remaining for the primary analyses (Figure 2).
Figure 2.
Study sample selection of Georgia dialysis patients and facilities.
Study Variables
Quality-of-Care Indicators
Existing indicators of quality of care among ESRD patients at the dialysis initiation—including whether patients had pre-ESRD nephrology care, initiated treatment on peritoneal dialysis (PD), had a permanent access (arteriovenous fistula or graft) at the time of first dialysis session, took an erythropoiesis-stimulating agent (ESA) before initiating dialysis, or were informed of transplant options within the first 45 days of dialysis—were taken from aggregate CMS Form 2728 data available in the DFR. Other facility-level indicators of quality of care after dialysis initiation were also taken from the DFR, including the following: standardized transplantation ratio, percentage of prevalent patients waitlisted for transplantation, standardized mortality ratio, standardized hospital admission ratio, percentage readmitted within 30 days after hospital discharge, percentage vaccinated against influenza, percentage with hemoglobin <10 mg/dl, percentage with urea reduction ratio (URR) >65 after 183 days on dialysis, percentage with dialysis dose (Kt/V) <1.2, percentage of prevalent dialysis patients with an arteriovenous fistula in use, and percentage of patients with only a catheter in place at 90 days after dialysis initiation. For variables with annual values, the most recent available values in the period 2008–2011 were assigned to facilities.
Referral
The primary outcome examined was referral for kidney transplant evaluation to one of the three transplant centers in Georgia within 1 year of dialysis initation.6 Referral date was defined as the date on which the transplant center received a referral form. Referrals were assigned to the patient’s initial dialysis facility. At the facility level, the percentage of incident dialysis patients referred within 1 year at the facility served as the outcome; at the patient level, patient referral within 1 year (yes versus no) served as the outcome.
Other Characteristics
Individual patient characteristics (age at dialysis initiation, sex, race/ethnicity, insurance at dialysis initiation, as well as cardiovascular disease, cancer, and smoking within the 10 years prior to dialysis initiation) were obtained from CMS Form 2728. Additional facility-level characteristics included for-profit status and the ratio of ESRD patients to staff within a facility, obtained from the DFR.
Statistical Analyses
Characteristics of facilities and patients were examined overall and by 1-year referral status (high/low [defined by median referral percentage] for facilities; yes/no for patients), using t, chi-square, and equality-of-medians tests, as appropriate. At the facility level, crude associations between percentage of incident dialysis patients referred for transplant evaluation within 1 year and high, intermediate, and low performance on quality indicators (defined by tertiles) were examined using ANOVA. At the patient level, multi-level, mixed-effects logistic regression was used to examine the association between patient referral status and patient- and facility-level quality indicators. A random intercept for facility was included in all patient-level analyses to allow for variation across facilities. We also adjusted for a priori patient-level confounders. Models were sequentially adjusted for patient characteristics and patient-level quality indicators to examine independent effects of facility-level quality indicators. In sensitivity analyses, we included 12,126 patients treated at 198 facilities with at least 25 patients,8 to assess robustness of the results to the variability of measurement in smaller clinics. Stata v. 14.0 (StataCorp LP, College Station, TX) was used for analyses, and α=0.05 was set as the statistical significance threshold.
Results
Characteristics of Georgia Dialysis Facilities
Among the 241 Georgia dialysis facilities included in this study, the median within-facility cumulative percentage of patients aged 18-69 referred for kidney transplantation within 1 year of dialysis initiation was 25.4%. Facilities with high versus low referral were more likely to be for-profit and had higher standardized transplant ratios and percentages of patients waitlisted than lower-referral facilities (Table 1). Additionally, percentages of patients with fistulae were higher, and percentages of dialysis patients with only a catheter for access after 90 days were lower, at higher-referral facilities.
Table 1.
Characteristics of Georgia dialysis facilities (2008-2011), overall and by median percentage of incident patients (2005—2011) referred for kidney transplantation within 1 year of dialysis initiation at the facility
| Referral Rate Category | ||||
|---|---|---|---|---|
|
|
||||
| Referral Rate Facility-level characteristic* |
Overall (N=241) |
Low **
(range: 0.0%- 25.4%; n=121) |
High**
(range: 25.5%-58.3%; n=120) |
P *** |
| Aggregate Patient Characteristics at Facility | ||||
| Average age, y | 61.4 (5.6) | 61.4 (5.5) | 61.4 (5.7) | 0.9 |
| % female | 45.4 (17.1) | 47.2 (17.2) | 43.6 (17.0) | 0.1 |
| % black | 57.5 (28.0) | 60.9 (28.0) | 54.1 (27.8) | 0.06 |
| % without insurance | 9.1 (0.0-20.0) | 10.0 (0.0-20.0) | 8.3 (0.0-20.5) | 0.5 |
| % employed | 33.3 (12.5-50.0) | 25.0 (0.0-42.9) | 33.3 (17.4-50.0) | 0.06 |
| % with diabetes | 60.1 (15.7) | 59.5 (16.3) | 60.8 (15.0) | 0.5 |
| Facility Characteristics | ||||
| For-profit | 88.4% | 81.8% | 95.0% | 0.001 |
| Patient:staff ratio | 4.0 (1.3) | 4.0 (1.2) | 4.0 (1.5) | 0.8 |
| Indicators of Quality Care at Dialysis Initiation | ||||
| % with pre-ESRD nephrology care |
72.1 (22.7) | 72.3 (22.2) | 72.0 (23.3) | 0.9 |
| % initiating dialysis on PD**** | 16.7 (9.1-25.9) | 13.3 (8.3-25.5) | 16.7 (10.0-25.9) | 0.9 |
| % initiating dialysis with a permanent access |
14.3 (8.0-25.0) | 14.3 (8.7-25.0) | 14.3 (7.7-25.0) | 0.9 |
| % on ESA prior to dialysis | 11.1 (0.0-28.6) | 11.8 (0.0-25.0) | 11.1 (0.0-28.6) | 0.07 |
| % informed of Tx options in first 45 d |
91.7 (68.0-100) | 90.0 (65.5-100) | 92.9 (73.0-100) | 0.5 |
| Indicators of Quality of Care After Dialysis Initiation | ||||
| Tx access | ||||
| Std Tx ratio | 0.49 (0.23-0.82) | 0.37 (0.19-0.64) | 0.66 (0.33-0.98) | 0.001 |
| % waitlisted | 17.8 (9.1) | 14.5 (7.9) | 21.1 (9.1) | <0.001 |
| Mortality and morbidity | ||||
| Std mortality ratio | 1.07 (0.79-1.33) | 1.09 (0.84-1.37) | 1.04 (0.74-1.31) | 0.4 |
| Std hospital admission ratio | 0.93 (0.78-1.10) | 0.93 (0.77-1.10) | 0.92 (0.78-1.10) | 0.9 |
| % readmitted | 28.9 (5.0) | 28.7 (4.3) | 29.1 (5.6) | 0.5 |
| Prevention | ||||
| % vaccinated | 70.0 (17.6) | 70.5 (16.9) | 69.6 (18.3) | 0.7 |
| Anemia management | ||||
| % hemoglobin <10 mg/dl | 4.8 (2.6-7.7) | 4.9 (2.9-7.7) | 4.8 (2.1-7.7) | 0.9 |
| Dialysis adequacy | ||||
| % URR ≥65 after 183 d | 98.1 (96.2-100) | 97.7 (96.0-100) | 98.5 (96.5-100) | 0.1 |
| % Kt/V <1.2 | 1.6 (0.1) | 1.6 (0.1) | 1.6 (0.1) | 0.2 |
| Vascular access | ||||
| % with fistula | 54.7 (10.1) | 52.6 (10.1) | 56.8 (9.7) | 0.001 |
| % with catheter only at 90 d | 5.7 (3.8) | 6.4 (4.2) | 5.0 (3.1) | 0.005 |
ESA, erythropoiesis-stimulating agent; ESRD, end stage renal disease; PD peritoneal dialysis; URR, urea reduction ratio; Std, standardized; Tx, transplant(ation)
Note: Unless otherwise indicated, values are given as mean ± standard deviation or median [interquartile range].
Characteristics are from the Dialysis Facility Report and represent 2008-2011 data.
Referral rate is % of patients referred for kidney Tx within 1 y of dialysis initation at facility. Low referral: percentage of patients over the study period who were referred within a year of their dialysis initiation below the median percentage across all facilities in the study; high referral: percentage of patients over the study period who were referred within a year of their dialysis initiation at or above the median percentage across all facilities in the study.
For low- vs. high-referral facilities, by t, equality-of-medians, or χ2 test, as appropriate.
Among 87 clinics offering PD (33 with low referral, 54, with high referral).
Facility-Level Associations of Referral With Quality of Dialysis Care
In crude examination of the association between facility-level referral and high, intermediate, and low facility-level performance on quality indicators (defined by tertiles; Table 2), no pre-dialysis quality-of-care indicators were significantly associated with referral. Percentage of incident patients being informed of transplant options at dialysis initiation was not associated with facility-level referral (Table 2). However, higher facility-level referral was associated with better performance with respect to the standardized transplantation ratio and percentage waitlisted, in a dose-response manner. Higher referral was not associated with better performance on other concurrent facility indicators of quality of care, including those capturing mortality, morbidity, prevention, and anemia management.
Table 2.
Crude facility-level percentage of patients referred for kidney transplantation within 1 year of dialysis initiation among Georgia facilities (2005-2011), by facility level of performance on dialysis quality-of-care indicators (2008–2011)
| Indicator | Level of quality-of-care indicator performance |
P for trend* |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Low | Intermediate | High | ||||||||
|
| ||||||||||
| No. of facilities |
Range of indicator |
Mean ±SD Referral Rate |
No. of facilities |
Range of indicator |
Mean ±SD Referral Rate |
No. of facilities |
Range of indicator |
Mean ±SD Referral Rate |
||
| Indicators of Quality of Care at Dialysis Initiation** | ||||||||||
| pre-ESRD nephrology care |
82 | 0.0%-66.7% | 25.6% (11.0%) | 81 | 66.8%-83.3% | 26.0% (11.7%) | 78 | 83.4%-100% | 25.0% (12.0%) | 0.9 |
| initating dialysis on PD** | 0 | --- | --- | 40 | 0.1%-14.9% | 28.3% (10.4%) | 47 | 15.0%-100% | 28.2% (10.2%) | 0.7 |
| initiating dialysis with permanent access |
80 | 0.0%- 10.4% |
26.2% (12.5%) |
80 | 10.5%-21.4% | 24.4% (10.8%) |
80 | 21.5%-75.0% | 25.9% (11.4%) | 0.9 |
| on ESA prior to dialysis | 82 | 0.0%-5.6% | 26.9% (12.2%) |
81 | 5.7%-23.1% | 25.6% (10.4%) |
78 | 23.2%-91.3% | 23.9% (11.8%) | 0.1 |
| informed of Tx options in first 45 d |
81 | 0.0%- 77.8% |
25.8% (11.3%) |
71 | 77.8%-99.2% | 25.7% (11.1%) |
89 | 100% | 25.1% (12.1%) | 0.9 |
| Indicators of Quality of Care After Dialysis initiation | ||||||||||
| Tx access | ||||||||||
| Std Tx ratio | 73 | 0.00-0.31 | 22.9% (9.5%) | 72 | 0.32-0.71 | 25.1% (11.4%) |
72 | 0.72-1.86 | 28.6% (11.8%) | 0.001 |
| waitlisted | 81 | 0.0%- 12.7% |
19.2% (10.1%) |
81 | 12.8%-20.6% | 26.8% (10.4%) |
79 | 20.7%-50.0% | 30.7% (11.1%) | <0.001 |
| Mortality and morbidity | ||||||||||
| Std mortality ratio | 80 | 1.24-2.41 | 24.8% (11.5%) |
80 | 0.89-1.23 | 25.5% (11.4%) |
80 | 0.0-0.88 | 26.6% (11.4%) | 0.4 |
| Std hospital | 80 | 1.05-1.82 | 26.3% (11.7%) |
80 | 0.83-1.04 | 25.5% (11.1%) |
80 | 0.33-0.82 | 24.8% (11.9%) | 0.4 |
| admission ratio | ||||||||||
| readmitted | 80 | 30.5%- 45.9% |
26.6% (10.9%) |
80 | 27.1%-30.4% | 24.2% (11.0%) |
81 | 15.2%-27.0% | 25.7% (12.6%) | 0.4 |
| Prevention: vaccinated | 84 | 0.0%- 66.7% |
25.3% (10.7%) |
77 | 66.8%-78.2% | 25.0% (11.7%) |
80 | 78.3%-100% | 26.3% (12.2%) | 0.6 |
| Anemia management | ||||||||||
| Hb <10 mg/dl | 77 | 6.8%- 22.2% |
25.8% (11.7%) |
81 | 3.1%-6.7% | 23.6% (10.7%) |
83 | 0.0-3.0 | 27.2% (12.0%) | 0.5 |
| Dialysis adequacy | ||||||||||
| URR ≥65 after 183 d | 81 | 0%-96.9% | 23.2% (10.2%) |
53 | 97.0%-99.9% | 26.3% (10.8%) |
107 | 100%-100% | 26.8% (12.6%) | 0.03 |
| Kt/V <1.2 | 79 | 1.6%-1.8% | 26.3% (12.3%) |
79 | 1.5%-1.6% | 27.3% (11.1%) |
80 | 0.7%-1.4% | 22.9% (10.7%) | 0.07 |
| Vascular access | ||||||||||
| fistula | 81 | 25.8%- 50.1% |
24.4% (11.5%) |
80 | 50.2%-59.1% | 24.3% (11.1%) |
80 | 59.2%-79.2% | 27.8% (11.8%) | 0.03 |
| catheter only at 90 d | 80 | 6.8%- 19.4% |
23.4% (10.8%) |
80 | 3.7%-6.7% | 27.1% (12.7%) |
81 | 0.0%-3.6% | 26.0% (10.8%) | 0.1 |
ESA, erythropoiesis-stimulating agent; ESRD, end stage renal disease; PD peritoneal dialysis; URR, urea reduction ratio; SD, standard deviation; Std, standardized; Tx, transplant(ation); Hb, hemoglobin
P for differences in referral by nonparametric trend test across indicator categories.
Among 87 clinics offering PD.
Patient-Level Associations of Referral With Quality of Dialysis Care
Patient characteristics by referral status are shown in Table S1 (provided as online supplementary material). In fully adjusted multi-level mixed models, those who had pre-ESRD nephrology care or a permanent access used at dialysis initiation had about one-third higher odds of being referred within 1 year of dialysis initiation than those who did not (Table 3). Additionally, patients informed of transplant options within the first 45 days of dialysis initation had 63% higher odds of being referred within 1 year of dialysis initiation than those who were not informed of transplant options. Patients treated at facilities with the highest standardized transplant ratios and highest percentages of prevalent patients waitlisted at the facility had 27% and 47% higher odds of being referred within 1 year of dialysis initiation, respectively, compared to patients at the lowest-performing facilities on these indicators. In sensitivity analyses, associations excluding facilities with fewer than 25 patients were nearly identical to the results in the main analyses in magnitude and statistical significance (Table S2).
Table 3.
Associations of patient referral for kidney transplantation within 1 year of dialysis initiation among Georgia incident dialysis patients (2005–2011) with patient- and facility-level dialysis quality-of-care indicators.
| Quality indicator | Unadjusted | Adjusted* for | ||
|---|---|---|---|---|
|
| ||||
| Demographics | + Clinical | + Predialysis quality |
||
| Patient-level indicator | ||||
| Pre-ESRD nephrology care | 1.13 (1.03-1.24) | 1.32 (1.19-1.45) | 1.32 (1.19-1.46) | 1.32 (1.16-1.49) |
| Initiating dialysis on PD | 0.97 (0.82-1.16) | 0.84 (0.70-1.01) | 0.80 (0.66-0.96) | ---** |
| Initiating dialysis with permanent access |
1.34 (1.22-1.47) | 1.55 (1.41-1.72) | 1.54 (1.39-1.70) | 1.37 (1.22-1.54) |
| ESA prior to dialysis | 0.91 (0.81-1.02) | 1.04 (0.92-1.17) | 1.06 (0.94-1.19) | 0.93 (0.80-1.07) |
| Informed of Tx option | 1.91 (1.68-2.17) | 1.65 (1.44-1.88) | 1.60 (1.39-1.83) | 1.63 (1.40-1.90) |
| Facility-level indicator | ||||
| Std transplant ratio | ||||
| Intermediate vs low | 1.13 (0.92-1.38) | 1.17 (0.96-1.43) | 1.17 (0.95-1.43) | 1.16 (0.93-1.45) |
| High vs low | 1.32 (1.08-1.62) | 1.30 (1.06-1.59) | 1.28 (1.05-1.57) | 1.27 (1.01-1.60) |
| waitlisted | ||||
| Intermediate vs low | 1.39 (1.15-1.68) | 1.39 (1.15-1.68) | 1.38 (1.14-1.67) | 1.37 (1.11-1.70) |
| High vs low | 1.50 (1.23-1.82) | 1.44 (1.18-1.75) | 1.43 (1.18-1.75) | 1.47 (1.18-1.83) |
| Std mortality ratio | ||||
| Intermediate vs low | 0.81 (0.67-0.98) | 0.80 (0.66-0.96) | 0.81 (0.66-0.98) | 0.87 (0.70-1.08) |
| High vs low | 1.00 (0.82-1.22) | 0.98 (0.80-1.19) | 1.01 (0.83-1.23) | 1.07 (0.86-1.33) |
| Std hospital admission ratio | ||||
| Intermediate vs low | 0.84 (0.69-1.02) | 0.83 (0.69-1.01) | 0.85 (0.70-1.04) | 0.87 (0.70-1.09) |
| High vs low | 1.02 (0.84-1.25) | 1.00 (0.82-1.22) | 1.04 (0.85-1.26) | 1.04 (0.84-1.30) |
| readmitted | ||||
| Intermediate vs low | 0.86 (0.70-1.04) | 0.82 (0.68-1.00) | 0.82 (0.67-1.00) | 0.83 (0.67-1.03) |
| High vs low | 0.93 (0.76-1.13) | 0.93 (0.77-1.14) | 0.96 (0.79-1.17) | 0.96 (0.77-1.19) |
| vaccinated | ||||
| Intermediate vs low | 1.05 (0.86-1.27) | 1.09 (0.90-1.32) | 1.11 (0.91-1.35) | 1.19 (0.96-1.48) |
| High vs low | 0.95 (0.77-1.16) | 1.08 (0.88-1.32) | 1.10 (0.90-1.35) | 1.15 (0.92-1.44) |
| hemoglobin <10 mg/dl | ||||
| Intermediate vs low | 0.94 (0.75-1.18) | 0.99 (0.79-1.23) | 1.02 (0.82-1.28) | 1.00 (0.78-1.28) |
| High vs low | 1.12 (0.93-1.34) | 1.21 (1.00-1.45) | 1.22 (1.02-1.47) | 1.24 (1.01-1.51) |
| Kt/V <1.2 | ||||
| Intermediate vs low | 0.90 (0.74-1.11) | 0.91 (0.74-1.11) | 0.92 (0.76-1.13) | 0.90 (0.72-1.12) |
| High vs low | 0.95 (0.78-1.15) | 0.87 (0.72-1.06) | 0.88 (0.73-1.08) | 0.86 (0.69-1.07) |
| URR ≥65 after 183 d | ||||
| Intermediate vs low | 1.22 (1.01-1.48) | 1.22 (1.01-1.48) | 1.21 (0.99-1.47) | 1.14 (0.91-1.41) |
| High vs low | 1.14 (0.94-1.39) | 1.21 (1.00-1.47) | 1.21 (0.99-1.47) | 1.12 (0.90-1.39) |
| with fistula | ||||
| Intermediate vs low | 0.92 (0.76-1.12) | 0.93 (0.76-1.13) | 0.89 (0.73-1.08) | 0.82 (0.66-1.02) |
| High vs low | 1.16 (0.95-1.41) | 1.18 (0.97-1.43) | 1.18 (0.97-1.43) | 1.19 (0.96-1.48) |
| with catheter only at 90 d | ||||
| Intermediate vs low | 1.03 (0.85-1.26) | 0.99 (0.82-1.20) | 0.98 (0.81-1.19) | 0.98 (0.79-1.22) |
| High vs low | 1.24 (1.02-1.51) | 1.30 (1.07-1.58) | 1.32 (1.09-1.61) | 1.31 (1.05-1.62) |
Note: Values are given as odds ratio (95% confidence interval).
ESA, erythropoiesis-stimulating agent; ESRD, end stage renal disease; PD peritoneal dialysis; URR, urea reduction ratio; Std, standardized; Tx, transplant(ation).
All models include a random intercept for dialysis facility. Demographics, for age, race/ethnicity, sex, and insurance; +Clinical, for demographics plus atherosclerotic cardiovascular disease, cancer, body mass index, and smoking; and + Predialysis quality: for demographics and clinical factors plus pre-ESRD care, PD, permanent access, and informed of Tx option (excluding variables for collinearity).
Failure predicted perfectly by variable in at least one facility and no estimate given.
Discussion
In this examination of how dialysis facility performance on quality-of-care indicators relates to referral of patients for kidney transplant evaluation from dialysis facilities, we found that, as expected, higher percentages of patients referred for kidney transplant evaluation within 1 year of dialysis initiation were associated with higher levels of waitlisting and transplantation. However, with the exception of percentage of prevalent patients with a permanent vascular access, referral was not associated with other, non–transplant-related indicators of quality of care at the facility level. At the patient level, those who had pre-ESRD nephrology care, initiated dialysis with a permanent vascular access, and were informed of transplant options were about 30%, 40%, and 60% more likely to be referred within 1 year, respectively, than their counterparts, after adjustment. Also, patients treated at facilities with top-tertile performance with respect to waitlisting and transplantation were about 50% and 30% more likely, respectively, to be referred than patients at facilities with the bottom-tertile performance on these metrics, but patient-level referral was not associated with non-transplant-related indicators of quality of care at the facility.
These results, which show that referral is related to—but not entirely correspondent with—transplantation and waitlisting, emphasize that the measurement of waitlisting, as recommended by the recent Technical Expert Panel on transplant measures,4 may not capture the same information as measurement of referral, which is under the direct control of the dialysis facility. The strength of the observed associations between these outcomes and referral (which is required for waitlisting and transplantation to occur) may be attenuated by unmeasured factors, including dialysis facility staff attitudes toward transplantation,9 which could affect the quality of patient-provider communication about kidney transplantation and, thus, referral (Figure 1).
Similarly, while the association between patients being informed of transplant options and their likelihood of referral is in the expected, positive direction, one might expect that the correlation between transplant education and referral would be of a stronger magnitude, given that education precedes referral in the path to transplantation (Figure 1). At the facility level, there was no association between provider-reported provision of transplant education and referral. These observed patterns may be partially due to inadequate standards for the content, duration, or quality of the information provided10 or due to poor capture of education in available data. In fact, recent literature suggests that patients report receiving information about transplant options far less often than is indicated by provider reports on the CMS-2728.11, 12 The lack of association at the facility level between referral and education underscores the recommendation of the CMS Technical Expert Panel4 that quality indicators related to referral be paired with indicators that would standardize, and increase accountability for, the education provided to dialysis patients.
We hypothesized that the general quality of care provided at a dialysis facility may be related to provider knowledge and patient-provider communication, which are necessary for kidney transplant referral (Figure 1). However, we found that non–transplant-related performance indicators were generally not associated with transplant referral. As Spolter et al.13 inferred in a similar study, which found that performance metrics on dialysis adequacy and anemia management were not aligned, we also infer that different strategies may be needed to improve performance on each new quality indicator. Thus, further studies to examine the optimal ways to increase referral from dialysis facilities are warranted.
Our results cannot address the extent to which adopting transplant referral as a dialysis facility quality measure would increase referral. While it is certainly under the control of dialysis providers, likelihood of referral is nonetheless subject to other factors such as dialysis providers’ perceived suitability of patients as kidney transplant candidates, dialysis facility staff and patient knowledge of the transplantation process, and patient interest in transplantation (Figure 1). Reporting of transplant education, waitlisting, and transplantation is required, but they are not currently pay-for-performance measures. Thus, facilities are less incentivized financially to focus on such measures, given the number of pay-for-performance measures to which the facilities now must adhere and constraints on time and resources. In contrast, we found that there was little variation in pay-for-performance measures that have been in place since the inception of the ESRD QIP (anemia management and dialysis adequacy), suggesting that facilities will quickly adopt best practices related to measures that are pay-for-performance.
The adoption of transplant referral as a dialysis facility quality measure could increase referral of patients from dialysis facilities and, ultimately, lead to higher waitlisting and deceased donor transplantation, more living donor transplantation, and reductions in disparities in access to transplantation. Further, insofar as referral for transplant evaluation reflects patient desires for improved quality of life,14, 15 its adoption as a quality indicator could partially address concerns about limited patient-centeredness in the current pay-for-performance environment.16 But there are also potential disadvantages to including referral as a pay-for-performance indicator. In the face of an ever-increasing number of pay-for-performance benchmarks, dialysis facilities might aggressively increase their levels of referral without regard to appropriateness of referrals, overwhelming transplant centers with referrals and potentially increasing wait times to evaluation for the most suitable candidates. Furthermore, these problems could be differential across regions due to varying concentrations of transplant centers and could potentially worsen existing geographic disparities.17-19 Pay-for-performance in terms of transplant referral might also lead to greater referral of patients who lack the necessary education and support to follow through complex and intimidating processes, such as completing a transplant evaluation and discussing living donation with potential donors. However, the recommendation of the CMS Technical Expert Panel4 to include indicators related to both provider and patient education would at least partially address these concerns. Finally, recent changes to the US kidney transplant allocation policy, which now uses time from ESRD incidence rather than time from waitlisting to assign priority on newly waitlisted patients,20, 21 might serve to make time to referral longer for incident dialysis patients (thus reducing the percentage referred within 1 year of dialysis initiation). For example, under this new policy, providers may think that some patients who are new to dialysis would be better served if referral were delayed and medical and psychosocial factors were addressed first, so that patients have better prospects of being waitlisted and also being transplanted once they are referred for evaluation. Pay-for-performance metrics that limit the time to referral (rather than simply measure percentage of prevalent patients who have been referred) could potentially undercut this type of clinical reasoning.
This study has several additional limitations. First, this is a cross-sectional study with ecological exposures and outcomes; individual target achievement for most of the indicators remains unknown. Furthermore, changes to the US kidney transplant allocation policy, which were not in place during the study period, could have increased levels of referral from dialysis facilities, particularly among prevalent patients with longer dialysis vintage; this may have changed the associations of referral with quality-of-care indicators, if provider knowledge of policy is related to quality of care delivered at the facility. All quality indicators have the potential to change over time, and only anemia management and dialysis adequacy were pay-for-performance indicators for most of the study period. Associations of patient-reported quality indicators such as In-Center Hemodialysis Consumer Assessment of Healthcare Providers and Systems Survey22 scores might be associated with patient referral, but data on this future indicator are not yet being collected. Additionally, while it would be interesting to examine the association of total number of targets achieved with referral, the appropriate benchmarks for each indicator were not entirely clear, since performance is often based on improvement at an individual facility rather than a specific cutoff. Residual confounding by unmeasured facility and patient factors (such as socioeconomic status), as well as unknown local policy or practice patterns during the study period, may have influenced referral. Our inability to capture out-of-state referrals might have led to misclassification, particularly at facilities located near the state border. Also, the DFR reports on quality using the entire patient population, while we only examined referral among those aged 18-69 years, who may differ from the remaining dialysis patient population in terms of some of the quality indicators. Finally, the associations seen are limited to Georgia and might not be generalizable to the United States as a whole. The collection of national transplant referral data is needed to examine associations beyond Georgia.
This study utilized a novel data source on referral for kidney transplant evaluation in Georgia to examine associations of dialysis facility performance on multiple quality indicators with referral. In general, we found that patient-level indicators related to quality of care received by a patient before dialysis initiation were associated with higher patient likelihood of referral, but, with the exception of other measures of access to kidney transplantation, most other facility-level indicators of quality of care were not associated with transplant referral. These results, while preliminary and geographically limited, could generate testable hypotheses about how transplant referral of dialysis patients relates to delivery of quality care at dialysis facilities. Furthermore, the results could inform current efforts underway to develop and adopt quality measures related to access to kidney transplantation.
Supplementary Material
Acknowledgements
We thank the Southeastern Kidney Council and all of the members of the Southeastern Kidney Transplant Coalition.
Some of the data reported here have been supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government. Additionally, this material was prepared with assistance from the Southeastern Kidney Council, contract Number HHSM-500-2013-NW006C, ESRD Network 6, funded by the CMS, an agency of the US Department of Health and Human Services. The ideas presented do not necessarily reflect CMS policies or positions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Support: This work was supported by National Institute on Minority Health and Health Disparities R24MD008077. The funder had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Financial Disclosure: Dr Pastan is a minority shareholder in Fresenius Dialysis, College Park, GA. The other authors declare that they have no other relevant financial interests.
Contributions: Research idea and study design: LCP, SOP, REP; data acquisition: JK, LM, EMG, REP; data analysis/interpretation: LCP, ASW, REP; statistical analysis: LCP; supervision or mentorship: SOP, REP. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. LCP takes responsibility that this study has been reported honestly, accurately, and transparently; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Peer Review: Evaluated by 2 external peer reviewers, a Statistical Editor, a Co-Editor, and the Editor-in-Chief.
Supplementary Material
Table S1: Characteristics of incident dialysis patients overall and by patient referral within 1 y of dialysis initiation.
Table S2: Sensitivity analysis excluding facilities with <25 patients.
Note: The supplementary material accompanying this article (doi:_______) is available at www.ajkd.org
Supplementary Material Descriptive Text for Online Delivery
Supplementary Table S1 (PDF). Characteristics of incident dialysis patients overall and by patient referral within 1 y of dialysis initiation.
Supplementary Table S2 (PDF). Sensitivity analysis excluding facilities with <25 patients.
References
- 1.Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–2109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- 2.United States Renal Data System: USRDS 2015 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda: 2015. [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Medicare program; end-stage renal disease quality incentive program Final rule. Fed Regist. 2011;76(3):627–646. [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services: Technical Expert Panels 2015 Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/TechnicalExpertPanels.html.
- 5.Patzer RE, Gander J, Sauls L, et al. The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol. 2014;15:171. doi: 10.1186/1471-2369-15-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patzer RE, Plantinga LC, Paul S, et al. Variation in dialysis facility referral for kidney transplantation among patients with end-stage renal disease in Georgia. J Am Med Assoc. 2015;314(6):582–594. doi: 10.1001/jama.2015.8897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.University of Michigan Kidney Epidemiology and Cost Center . 2012 Dialysis Facility Report Documentation. University of Michigan Kidney Epidemiology and Cost Center; Ann Arbor, MI: 2012. [Google Scholar]
- 8.Lacson E, Jr., Wang W, Lazarus JM, Hakim RM. Hemodialysis facility-based quality-of-care indicators and facility-specific patient outcomes. Am J Kidney Dis. 2009;54(3):490–497. doi: 10.1053/j.ajkd.2009.01.260. [DOI] [PubMed] [Google Scholar]
- 9.Gander J, Browne T, Plantinga L, et al. Dialysis facility transplant philosophy and access to kidney transplantation in the Southeast. Am J Nephrol. 2015;41(6):504–511. doi: 10.1159/000438463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Medicare & Medicaid Services Medicare and Medicaid programs; conditions for coverage for end-stage renal disease facilities. Final rule. Fed Regist. 2008;73(73):20369–20484. [PubMed] [Google Scholar]
- 11.Waterman AD, Peipert JD, Goalby CJ, Dinkel KM, Xiao H, Lentine KL. Assessing transplant education practices in dialysis centers: comparing educator reported and Medicare data. Clin J Am Soc Nephrol. 2015;10(9):1617–1625. doi: 10.2215/CJN.09851014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salter ML, Orandi B, McAdams-DeMarco MA, et al. Patient- and provider-reported information about transplantation and subsequent waitlisting. J Am Soc Nephrol. 2014;25(12):2871–2877. doi: 10.1681/ASN.2013121298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spolter YS, Seliger SL, Zhan M, Hsu VD, Walker LD, Fink JC. The relationship between dialysis performance measures: adequacy and anemia management. Am J Kidney Dis. 2007;50(5):774–781. doi: 10.1053/j.ajkd.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Evans RW, Manninen DL, Garrison LP, Jr., et al. The quality of life of patients with end-stage renal disease. N Engl J Med. 1985;312(9):553–559. doi: 10.1056/NEJM198502283120905. [DOI] [PubMed] [Google Scholar]
- 15.Fiebiger W, Mitterbauer C, Oberbauer R. Health-related quality of life outcomes after kidney transplantation. Health Qual Life Outcomes. 2004;2:2. doi: 10.1186/1477-7525-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wish JB, Meyer KB. ESRD Networks: past, present, and challenges for the future. Clin J Am Soc Nephrol. 2012;7(11):1907–1914. doi: 10.2215/CJN.01450212. [DOI] [PubMed] [Google Scholar]
- 17.Ashby VB, Kalbfleisch JD, Wolfe RA, Lin MJ, Port FK, Leichtman AB. Geographic variability in access to primary kidney transplantation in the United States, 1996-2005. Am J Transplant. 2007;7(5):1412–1423. doi: 10.1111/j.1600-6143.2007.01785.x. Pt 2. [DOI] [PubMed] [Google Scholar]
- 18.Patzer RE, Plantinga L, Krisher J, Pastan SO. Dialysis facility and network factors associated with low kidney transplantation rates among United States dialysis facilities. Am J Transplant. 2014;14(7):1562–1572. doi: 10.1111/ajt.12749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patzer RE, Pastan SO. Kidney transplant access in the Southeast: view from the bottom. Am J Transplant. 2014;14(7):1499–1505. doi: 10.1111/ajt.12748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ashby VB, Port FK, Wolfe RA, et al. Transplanting kidneys without points for HLA-B matching: consequences of the policy change. Am J Transplant. 2011;11(8):1712–1718. doi: 10.1111/j.1600-6143.2011.03606.x. [DOI] [PubMed] [Google Scholar]
- 21.Organ Procurement and Transplantation Network . Kidney Allocation System. U.S. Department of Health & Human Services; Washington, DC: 2014. Available at: http://optn.transplant.hrsa.gov/learn/professional-education/kidney-allocation-system/ [Google Scholar]
- 22.Centers for Medicare & Medicaid Services: In-Center Hemodialysis CAHPS Survey 2016 Available at: https://ichcahps.org.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.