Abstract
Background
Recent trend studies suggest that marijuana use is on the rise among the general population of adults ages 18 and older in the United States. However, little is known about the trends in marijuana use and marijuana-specific risk/protective factors among American adults during the latter part of adulthood.
Method
Findings are based on repeated, cross-sectional data collected from late middle-aged (ages 50–64) and older adults (ages 65 and older) surveyed as part of the National Survey on Drug Use and Health between 2002 and 2014.
Results
The prevalence of past-year marijuana use among late middle-aged adults increased significantly from a low of 2.95% in 2003 to a high of 9.08% in 2014. Similarly, the prevalence of marijuana use increased significantly among older adults from a low of 0.15% in 2003 to a high of 2.04% in 2014. Notably, the upward trends in marijuana use remained significant even when accounting for sociodemographic, substance use, behavioral, and health-related factors. We also found that decreases in marijuana-specific protective factors were associated with the observed trend changes in marijuana use among late middle-aged and older adults, and observed a weakening of the association between late-middle aged marijuana use and risk propensity, other illicit drug use, and criminal justice system involvement over the course of the study.
Conclusions
Findings from the present study provide robust evidence indicating that marijuana use among older Americans has increased markedly in recent years, with the most evident changes observed between 2008 and 2014.
Keywords: marijuana, trends, risk and protective factors, adulthood, older adults
1.0.0 Introduction
The past two decades have been a period of tremendous change with respect to public policy and perception related to the use and distribution of marijuana in the United States (US). Beginning with California's "Compassionate Use Act of 1996", we have witnessed a steady expansion of policies designed to medicalize, decriminalize, and legalize the private use of Cannabis sativa (Lee, 2012). At present, marijuana can be used for medical purposes in 28 states and the District of Columbia, the recreational use of marijuana has been legalized in a handful of states, and more than half (57%) of American adults believe marijuana should be legal (Geiger, 2016). Based on the pattern of results observed for marijuana-related ballot propositions in the November 2016 elections, it seems likely that the expansion and implementation of marijuana liberalization policies will continue to take place across the US.
Cognizant of these changes, scholars have conducted a growing number of epidemiological trend studies designed to examine potential changes in marijuana use and marijuana-specific risk/protective factors (Center for Behavioral Health Statistics and Quality, 2015; Compton, 2016; Fleming et al., 2016; Hasin et al., 2015a, 2015b, 2016; Johnson et al., 2015; Johnston et al. 2015; Johnston et al., 2014; Salas-Wright and Vaughn, 2016a, 2016b; Salas-Wright et al., 2016d; Salas-Wright et al., 2015). By and large, these studies suggest that marijuana use among adults is on the rise. For instance, Hasin and colleagues (2015a), drawing from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), found that past year marijuana use among adults increased from 4.1% in 2001–2002 to 9.5% in 2012–2013. Compton and colleagues (2016) report similar findings from the National Survey on Drug Use and Health (NSDUH) with past year marijuana use among adults increasing from 10.4% in 2002 to 13.3% in 2014. More recent evidence indicates that the prevalence of marijuana use among American adults has continued to increase, nearly doubling from 7% in 2013 to 13% in 2016 (McCarthy, 2016). Taken collectively, these studies provide rather compelling evidence that important changes in adult marijuana use are underway.
While the aforementioned studies provide critical insight into trends among American adults in general, we know less about trends in marijuana use during two particularly salient developmental stages during the latter part of adulthood: late-middle age (ages 50–64) and older adulthood (ages 65 and older). These age groups are important to consider for several reasons. For one, they are large and growing. Indeed, the US Census Bureau projects that both age groups will increase in size in the coming years, with robust growth in the proportion of older adults in the US population (Ortman et al., 2014). Moreover, prior research indicates that a noteworthy proportion of Americans ages 50 and older report recent marijuana use and suggest that older marijuana users report greater levels of psychiatric distress, mental illness, and comorbid substance use (Choi et al., 2016; DiNitto and Choi, 2011; Han et al., 2016).
Several recent studies do provide us some insight into trends in marijuana use during the latter stages of adulthood. For instance, Hasin and colleagues (2015a) report an increase in the prevalence of marijuana use among adults ages 45–64 (2001/2002: 1.6%, 2012/2013: 5.9%) and 65 and older (2001/2002: 0.0%, 2012/2013%: 1.3) between NESARC Wave 1 and the NESARC-III. Similarly, a recent report by Stoner (2016) displays the prevalence of marijuana use among adults ages 50–64 and 65 and older using data from the NSDUH between 2002 and 2014. Importantly, however, neither of the aforementioned studies provide an in-depth assessment of trend data, examine trends in marijuana specific risk factors, nor systematically examine key correlates of marijuana use. Han and colleagues (2016) also recently examined trends in the prevalence of marijuana use among adults ages 50 and older using NSDUH data collected between 2006/2007 and 2012/2013. Regretfully, however, while this study examined a number of important behavioral health correlates, many key risk behaviors and marijuana-specific risk/protective factors were omitted, and the bulk of analyses were conducted with late-middle aged and older adults aggregated into a singular analytic sample.
2.0.0 The Present Study
The present study aims to provide a systematic examination of the trends and correlates of marijuana use among late middle-aged (ages 50–64) and older adults (ages 65 and older) in the US by employing data from a large, population-based study collected between 2002 and 2014 (i.e., the NSDUH [SAHMSA, 2014]). Specifically, we present prevalence estimates for marijuana use and conduct tests of trend while accounting for sociodemographic, substance use, risk behavior, and behavioral health-related factors. We also examine trends in marijuana-specific protective factors and assess the degree to which changes in these marijuana-related factors are related to trends in marijuana use. Finally, we examine the association between marijuana use and comorbid substance use, risk behavior, criminal justice system involvement, and behavioral health outcomes, paying particular attention to changes in the link between marijuana use and these outcomes over time.
3.0.0 Method
3.1.0 Sample
This study examines public-use data collected between 2002 and 2014 as part of the NSDUH. The NSDUH provides population estimates for an array of substance use and health-related behaviors in the US general population. NSDUH participants include household residents; civilians residing on military bases; and residents of shelters and group homes. The design and methods are summarized briefly here, but a detailed description of NSDUH procedures is available elsewhere (SAHMSA, 2014). Since 2002, a total of 723,283 respondents have completed the NSDUH survey; however, the current study restricted analyses to respondents to those corresponding to the oldest two general age categories available in the NSDUH data file (i.e., late-middle aged [ages 50–64, n = 46,600] and older adults [ages 65 and older, n = 29,418]).
3.2.0 Measures
3.2.1 Marijuana Use
We examined self-reports of past 12-month use of marijuana or hashish (0 = no use, 1 = one or more instance of use).
3.2.2 Marijuana-Specific Factors
We examined three variables related to the perception of marijuana use and access to marijuana. Concerning marijuana disapproval, each respondent was asked, "How do you feel about adults trying marijuana or hashish once or twice?" with response options including "neither approve nor disapprove" (1), "somewhat disapprove" (2), and "strongly disapprove" (3). In terms of marijuana access, respondents were asked, "How difficult or easy would it be for you to get some marijuana, if you wanted some?" with response options ranging from "very easy" (1) to "probably impossible" (5). Respondents were also asked about perceptions of risk of marijuana use. They were asked, "How much do people risk harming themselves physically and in other ways when they smoke marijuana once or twice a week?” with response options ranging from "no risk" (1) to "great risk" (4).
3.2.3 Comorbid Substance Use and Risk Behavior
We examined past 12-month use of tobacco and illicit drugs other than marijuana (e.g., cocaine, hallucinogens, opioids, etc.) and binge alcohol use—specifically, five or more drinks on the same occasion—over the past 30 days (the NSDUH does not include a past 12-month binge drinking variable). We also examined several risk behaviors, including: driving under the influence of alcohol or illicit drugs, illicit drug selling, theft of an item worth more than $50, and attacks with the intent to seriously harm others, as well as past year criminal justice system involvement. For each of the aforementioned substance use and risk behavior variables, respondents reporting one or more instances of use/involvement were coded as 1 and all other respondents coded as 0. We also created an index (α = 0.82) based on two variables measuring risk propensity.
3.2.4 Behavioral Health Conditions
We examined four variables measuring behavioral health conditions—anxiety, depression, human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS), and sexual transmitted diseases (STD)—based on respondent reports of past year diagnosis by a doctor/medical professional (0 = no, 1 = yes).
3.2.5 Sociodemographic Factors
Sociodemographic characteristics included age, gender, race/ethnicity, family income, education, marital status, insurance status, and urbanicity. The response categories for each of these variables are listed in Table 1.
Table 1.
Sociodemographic Correlates of Past 12-Month Marijuana Use among Late Middle-Aged and Older Adults in the United States, 2002–2014
| Have you used marijuana or hashish in the past 12 months? | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic Factors |
Late Middle-Aged Adults (Ages 50 to 64) |
Older Adults (Ages 65 and older) |
||||||||||
| No (n = 43,932) |
Yes (n = 2668) |
Odds Ratio | No (n = 29,162) |
Yes (n = 256) |
Odds Ratio | |||||||
| % | 95% CI | % | 95% CI | AOR | (95% CI) | % | 95% CI | % | 95% CI | AOR | (95% CI) | |
| Gender | ||||||||||||
| Female | 52.65 | (52.0–53.3) | 34.54 | (31.2–36.9) | -- | 56.78 | (56.1–57.5) | 30.11 | (23.3–37.9) | -- | ||
| Male | 47.35 | (46.7–48.0) | 65.46 | (63.0–67.8) | 2.26 | (2.03–2.51) | 43.22 | (42.5–43.9) | 69.89 | (62.0–76.7) | 3.12 | (2.09–4.65) |
| Race/Ethnicity | ||||||||||||
| Non-Hispanic White | 73.94 | (73.3–74.5) | 79.24 | (77.3–81.0) | -- | 80.40 | (79.7–81.1) | 72.90 | (64.1–80.2) | -- | ||
| African American | 10.61 | (10.2–11.0) | 12.14 | (10.5–14.0) | 0.81 | (0.68–0.96) | 8.34 | (7.9–8.8) | 15.30 | (10.1–22.6) | 1.92 | (1.07–3.43) |
| Hispanic | 9.65 | (5.5–6.1) | 4.93 | (2.9–4.7) | 0.39 | (0.30–0.50) | 6.78 | (6.4–7.2) | 6.18 | (3.1–9.9) | 0.82 | (0.44–1.56) |
| Other | 5.80 | (9.2–10.1) | 3.69 | (3.9–6.2) | 0.57 | (0.44–0.76) | 4.48 | (4.1–4.9) | 5.61 | (2.5–14.4) | 1.18 | (0.44–3.18) |
| Family Income | ||||||||||||
| Less than $20,000 | 13.62 | (13.2–14.0) | 22.24 | (20.2–24.4) | 1.44 | (1.20–1.73) | 23.80 | (23.1–24.5) | 26.16 | (19.5–34.1) | 1.89 | (0.99–3.62) |
| $20,000–$49,999 | 29.05 | (28.6–29.5) | 30.33 | (27.9–32.8) | 1.12 | 0.96–1.32) | 43.32 | (42.6–44.1) | 38.87 | (31.3–46.9) | 1.47 | (0.86–2.53) |
| $50,000–$74,999 | 19.16 | (18.6–19.7) | 14.90 | (13.4–16.6) | 0.91 | (0.78–1.05) | 15.12 | (14.5–15.7) | 16.77 | (11.2–24.4) | 1.38 | (0.75–2.53) |
| $75,000 or greater | 38.17 | (37.5–38.8) | 32.53 | (30.1–35.0) | -- | 17.76 | (17.1–18.4) | 18.20 | (12.6–25.5) | -- | ||
| Education | ||||||||||||
| Less than High School | 12.46 | (12.0–12.9) | 13.19 | (11.7–14.8) | 1.04 | (0.86–1.25) | 22.85 | (22.1–23.6) | 19.71 | (13.8–27.3) | 0.47 | (0.25–0.88) |
| High School Graduate | 31.04 | (30.4–31.7) | 30.31 | (27.9–32.7) | 0.94 | 0.81–1.09) | 34.26 | (33.5–35.0) | 16.33 | (11.6–22.5) | 0.30 | (0.17–0.54) |
| Some College | 24.77 | (24.3–25.3) | 27.21 | (25.3–29.1) | 1.14 | (1.01–1.27) | 19.57 | (19.0–20.1) | 24.91 | (19.2–31.6) | 0.77 | (0.49–1.20) |
| College Graduate | 31.73 | (31.1–32.4) | 29.29 | (27.1–31.6) | -- | 23.32 | (22.6–24.0) | 39.05 | (30.7–48.1) | -- | ||
| Marital Status | ||||||||||||
| Married | 68.37 | (67.7–69.0) | 48.70 | (46.1–51.3) | -- | 57.51 | (56.7–58.3) | 50.84 | (41.6–60.1) | -- | ||
| Widowed | 4.84 | (4.6–5.1) | 3.55 | (2.7–4.6) | 1.18 | (0.90–1.54) | 27.03 | (26.4–27.7) | 17.19 | (12.3–23.6) | 1.03 | (0.64–1.68) |
| Divorced/Separated | 19.40 | (18.9–20.0) | 34.41 | (32.1–36.8) | 2.33 | (2.05–2.64) | 11.59 | (11.0–12.2) | 25.38 | (18.9–33.2) | 2.27 | (1.37–3.75) |
| Never Married | 7.39 | (7.1–7.7) | 13.34 | (11.8–15.1) | 2.13 | (1.77–2.56) | 3.87 | (3.6–4.1) | 6.59 | (3.1–13.3) | 1.74 | (0.70–4.35) |
| Insurance | ||||||||||||
| Yes | 88.29 | (88.9–89.7) | 83.36 | (81.3–85.2) | -- | 99.42 | (99.3–99.5) | 97.94 | (93.5–99.4) | -- | ||
| No | 10.71 | (10.3–11.1) | 16.64 | (14.8–18.7) | 1.34 | (1.15–1.57) | 0.58 | (0.48–0.70) | 2.06 | (0.63–6.50) | 3.46 | (0.90–13.3) |
| Urbanicity* | ||||||||||||
| Urban | 82.13 | (81.5–82.7) | 83.97 | (81.9–85.8) | -- | 80.79 | (79.9–81.6) | 83.22 | (77.4–87.8) | -- | ||
| Rural | 17.87 | (17.3–18.5) | 16.03 | (14.2–18.0) | 0.77 | (0.66–0.90) | 19.21 | (18.4–20.1) | 16.78 | (12.2–22.6) | 0.90 | (0.61–1.33) |
Note: Odds ratios adjusted for gender, race/ethnicity, family income, education, marital status, insurance, and survey year.
NSDUH data on urbanicity is only available after 2006. As such, while we present estimates and odds ratios for urbanicity, we did not adjust odds ratios for the other demographic factors for urban/rural status. Odds ratios and 95% confidence intervals in bold are statistically significant.
3.3.0 Statistical Analyses
The statistical analyses were conducted in several phases. First, we present survey adjusted prevalence estimates (see Figures 1–2) for past year marijuana use among late middle-aged (ages 50–64) and older adults (ages 65 and older). Figures 1 and 2 also include trend data on marijuana disapproval while prevalence estimates for marijuana access and risk perceptions are reported in the body of the text. For tests of trend, survey year was included—along with gender, race/ethnicity, family income, education, marital status, insurance status—as a continuous independent variable in logistic regression models predicting marijuana use. This approach follows the trend analysis method outlined by the Centers for Disease Control and Prevention (Centers for Disease Control and Prevention, 2016) and is consistent with highly-cited (Flegal et al, 2012) and recent NSDUH-based trend studies (Salas-Wright et al., 2015; Vaughn et al., 2016a; Vaughn et al., 2016b). Lastly, we used logistic regression analyses to examine the associations between marijuana use and comorbid substance use and risk behavior and behavioral health conditions while controlling for sociodemographic characteristics. All statistical analyses were conducted using Stata 14.1 MP (c) and all estimates were weighted to abide by the Substance Abuse and Mental Health Data Archive’s guidelines, accounting for the NSDUH’s stratified cluster sampling design (SAMHSA, 2014).
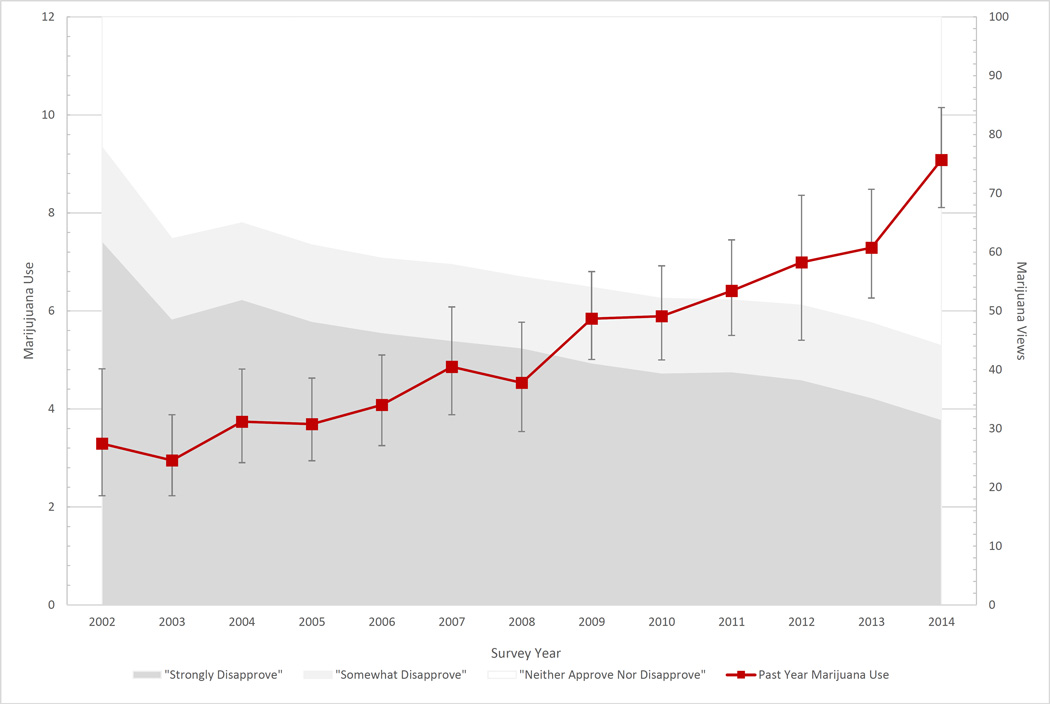
Figure 1.
Prevalence and 95% Confidence Intervals for Past Year Marijuana Use and Disapproval among Adults Ages 50 to 64 in the United States between 2002 and 2014 based on Data from the National Survey on Drug Use and Health
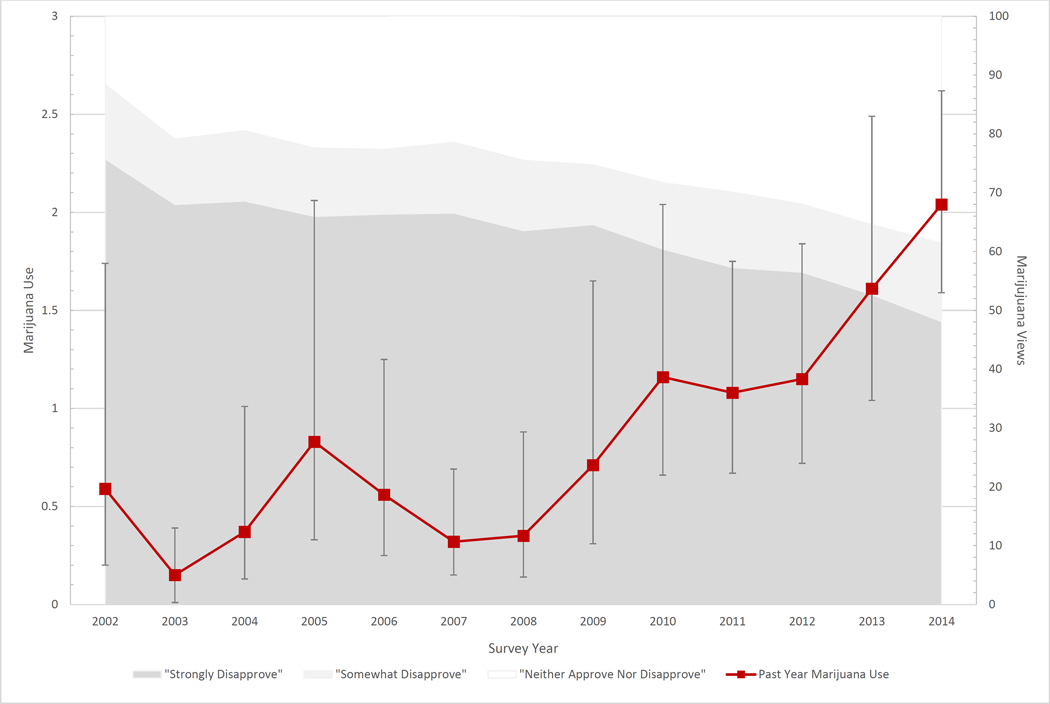
Figure 2.
Prevalence and 95% Confidence Intervals for Past Year Marijuana Use and Disapproval among Adults Ages 65 and Older in the United States between 2002 and 2014 based on Data from the National Survey on Drug Use and Health
4.0.0 Results
4.1.0 Sociodemographic Characteristics of Marijuana Users
Table 1 displays the sociodemographic characteristics of late middle-aged and older adult marijuana users. Compared to non-marijuana users, late middle-aged marijuana users are significantly more likely to be male (AOR = 2.26, 95% CI = 2.03–2.51), have completed some college (AOR = 1.14, 95% CI = 1.01–1.27), be divorced/separated (AOR = 2.33, 95% CI = 2.05–2.64) or have never married (AOR = 2.13, 95% CI = 1.77–2.56), and be uninsured (AOR = 1.34, 95% CI = 1.15–1.57). Older adult marijuana users are significantly more likely to be male (AOR = 3.12, 95% CI = 2.09–4.65), African-American (AOR = 1.92, 95% CI = 1.07–3.43), and be divorced/separated (AOR = 2.27, 95% CI = 1.37–3.75) and significantly less likely—compared with college graduates—to have not completed high school (AOR = 0.47, 95% CI = 0.25–0.88) or have completed only a high school degree (AOR = 0.30, 95% CI = 0.17–0.54).
4.2.0 Trends in Marijuana Use and Marijuana-Specific Factors
Figures 1 and 2 display the prevalence estimates for past year marijuana use—as well as marijuana disapproval—among late middle-aged and older adults between 2002 and 2014. As seen in Table 2, adjusting for sociodemographic and substance use/risk behavioral factors, we observed a significant increase in marijuana use among late middle-aged (AOR = 1.101, 95% CI = 1.082–1.122) and older adults (AOR = 1.153, 95% CI = 1.082–1.228) over the course of the study. The adjusted odds ratios of 1.101 for late-middle aged adults suggests a 10.1% yearly increase in the likelihood of marijuana use among late middle-aged adults (similarly, the odds ratio of 1.153 suggests a 15.3% annual increase in the likelihood of marijuana use among older adults). We also conducted supplementary analyses in which we included a quadratic term for year (year*year) in the multivariate logistic regression. Notably, the quadratic term was not found to be significant among late middle-aged or older adults, lending support to the appropriateness of the use of a linear modeling approach.
Table 2.
Test of Trends in Marijuana Use and Marijuana-Specific Risk Factors among Late Middle-Aged and Older Adults in the United States, 2002–2014
| Late Middle-Aged Adults (Ages 50 to 64) |
Older Adults (Ages 65 and older) |
|||
|---|---|---|---|---|
| Odds Ratio |
(95% CI) | Odds Ratio |
(95% CI) | |
|
Marijuana Use | ||||
| Unadjusted (Bivariable) | 1.097 | (1.080–1.115) | 1.166 | (1.099–1.237) |
| Adjusted for Sociodemographic Factors | 1.095 | (1.077–1.113) | 1.154 | (1.087–1.226) |
| Adjusted for Sociodemographic and Substance Use/Risk Behavior Factors |
1.101 | (1.082–1.122) | 1.153 | (1.082–1.228) |
|
Additional Adjustments for Marijuana-Specific Protective Factors |
||||
| Disapproval | 1.068 | (1.048–1.089) | 1.096 | (1.028–1.117) |
| Limited Access | 1.096 | (1.075–1.116) | 1.131 | (1.062–1.204) |
| Perceptions of Risk | 1.048 | (1.028–1.069) | 1.095 | (1.032–1.162) |
| Full Model | 1.034 | (1.013–1.055) | 1.053 | (0.992–1.117) |
|
Marijuana-Specific Protective Factors | ||||
| Marijuana Disapproval | ||||
| Unadjusted (Bivariable) | 0.925 | (0.920–0.931) | 0.924 | (0.916–0.932) |
| Adjusted for Sociodemographic Factors | 0.926 | (0.920–0.931) | 0.932 | (0.924–0.940) |
| Adjusted for Sociodemographic and Health/Behavioral Factors |
0.919 | (0.913–0.925) | 0.929 | (0.921–0.938) |
| Limited Marijuana Access | ||||
| Unadjusted (Bivariable) | 0.987 | (0.981–0.994) | 0.965 | (0.957–0.973) |
| Adjusted for Sociodemographic Factors | 0.986 | (0.980–0.992) | 0.973 | (0.965–0.982) |
| Adjusted for Sociodemographic and Health/Behavioral Factors |
0.983 | (0.977–0.990) | 0.973 | (0.964–0.981) |
| Marijuana Use Perceived as Great Risk | ||||
| Unadjusted (Bivariable) | 0.922 | (0.916–0.929) | 0.934 | (0.926–0.942) |
| Adjusted for Sociodemographic Factors | 0.920 | (0.913–0.926) | 0.942 | (0.934–0.951) |
| Adjusted for Sociodemographic and Health/Behavioral Factors |
0.916 | (0.909–0.922) | 0.940 | (0.931–0.948) |
Note: The unadjusted model presents results for bivariable analyses without controlling for any covariates. The sociodemographic model adjusts for sociodemographic factors and the health and behavior model adjusts for sociodemographic, behavioral health, substance use, risk behavior, and criminal justice system involvement. The additional adjustments for marijuana specific factors models adjust for sociodemographic, behavioral health, substance use, risk behavior, and criminal justice system involvement, as well as the marijuana-specific risk factors specified in the table. The full model controls for all sociodemographic, behavioral health, behavioral, and marijuana specific risk factors. Odds ratios and 95% confidence intervals in bold are statistically significant. Significant odds ratios with a value of greater than 1.00 reflect an increase in trend. Significant odds ratios with a value of less than 1.00 reflect a decrease in trend.
We also observed a uniform pattern of decreases among late middle-aged and older adults reporting strong marijuana disapproval ("strongly disapprove"), limited marijuana access ("very difficult" or "probably impossible"), and the perception of marijuana use as a "great risk" to one's health and well-being. Specifically, we see that, among the late middle-aged, the proportion reporting limited access to marijuana remained mostly stable between 2002 (32.44%) and 2009 (32.52%) before gradually declining to 27.42% in 2014. A similar pattern was observed among older adults as the proportion reporting limited access was mostly stable between 2002 (56.67%) and 2008 (54.43%) before dropping steadily to 43.30% in 2014. Among late middle-aged adults, the proportion of those perceiving great risk remained steady between 2002 (57.76%) and 2005 (55.07%) before beginning a consistent—and noteworthy—decline to a low of 35.36% in 2014. Among older adults, the perception of great risk remained steady between 2002 (67.15%) and 2008 (67.96%) before decreasing steadily to a low of 50.24% in 2014.
In order to assess the degree to which decreases in marijuana-specific factors may have accounted for the observed increase in marijuana use, we also conducted tests of trend while controlling for marijuana disapproval, limited access, and perceptions of risk (in addition to the same list of sociodemographic and substance use/behavioral risk factors). Among late middle-aged adults, we see that the association between marijuana use and survey year decreases significantly—as observed by the non-overlapping 95% confidence intervals—in the "full model" that accounts for marijuana-specific factors (AOR = 1.034, 95% CI = 1.013–1.055). Among older adults, we do not see a significant change based on the overlap of the 95% confidence intervals; however, the association between survey year and marijuana use reduces to a similar degree and ceases to be significant when accounting for marijuana-specific factors.
It should be noted that the results displayed in Table 2 are not adjusted for past year diagnoses of anxiety, depression, HIV/AIDS, or STDs. This is due to the fact that these particular variables were not measured in the NSDUH prior to 2005. To account for this omission, we conducted sensitivity analyses in which we examined trend data from 2005–2014 while controlling for the aforementioned health conditions. Among adults ages 50 to 64, the results were similar—as evinced by overlapping 95% confidence intervals—while adjusting for sociodemographic, substance use/risk behavioral and health factors (AOR = 1.110, 95% CI = 1.087–1.134) and in the full model which adjusted for marijuana specific factors as well (AOR = 1.041, 95% CI = 1.016–1.066). Among adults ages 65 and older, we saw a similar pattern while adjusting for sociodemographic and substance use/risk behavioral factors, and health conditions (AOR = 1.165, 95% CI = 1.068–1.271) and in the full model (AOR = 1.030, 95% CI = 0.949–1.119). These findings suggest that the exclusion of these specific health conditions did not substantively alter the overall 2002–2014 trend findings.
4.3.0 Behavioral and Behavioral Health Correlates of Marijuana Use
In addition to trend analyses, we also examined the association between marijuana use and a host of behavioral and behavioral health correlates (see Table 3–4). Among late middle-aged adults, we see a consistent pattern in which marijuana users are significantly more likely to report comorbid substance use, and involvement in risky and illegal behaviors and criminal justice system involvement with medium-to-large effects observed (Chen et al., 2010). In terms of behavioral health conditions, we also found that late middle-aged marijuana users are significantly more likely to report diagnoses of anxiety, depression, HIV/AIDS, and STIs. A similar pattern was observed among older adults; however, the link between marijuana use and risky/criminal behavior was not found to be significant for drug selling, theft, or attacks with intent to harm. Additionally, HIV/AIDS was omitted due to the lack of respondents ages 65 and older reporting past year diagnoses of HIV/AIDS. The omission of HIV/AIDS serves to underscore one particular concern in examining associations between marijuana use and behavioral/behavioral health factors among older adults. Namely, of the 29,162 older adults in the sample, only a small minority (n = 256) reported past year marijuana use. Consequently, we are somewhat limited in terms of model stability and the identification of significant associations between marijuana use and comorbid risk behavior, particularly with inclusion of covariates. As such, we conducted sensitivity analyses in which all associations examined in Tables 3–4 were also examined using only survey year as a covariate. For all variables, the results of these supplementary analyses were identical to those presented in Tables 3–4 in terms of the pattern of significance and directionality.
Table 3.
Substance Use and Risk Behavior Correlates of Marijuana Use among Late Middle-Aged and Older Adults in the United States, 2002–2014
| Have you used marijuana or hashish in the past 12 months? | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Late Middle-Aged Adults (Ages 50 to 64) |
Older Adults (Ages 65 and older) |
|||||||||||
| No (n = 43,932) |
Yes (n = 2668) |
Odds Ratio | No (n = 29,162) |
Yes (n = 256) |
Odds Ratio | |||||||
| % | 95% CI | % | 95% CI | AOR | (95% CI) | % | 95% CI | % | 95% CI | AOR | (95% CI) | |
| Substance Use | ||||||||||||
| Tobacco | ||||||||||||
| No | 72.48 | (72.0–72.9) | 39.47 | (36.9–42.1) | 85.57 | (85.1–86.1) | 53.62 | (45.4–61.6) | ||||
| Yes | 27.52 | (27.0–28.0) | 60.53 | (57.9–63.1) | 3.33 | (2.97–3.73) | 14.43 | (13.9–14.9) | 46.38 | (38.4–54.6) | 4.54 | (3.20–6.43) |
| Binge Alcohol | ||||||||||||
| No | 84.22 | (83.8–84.6) | 57.62 | (55.1–60.1) | 91.96 | (91.5–92.4) | 76.79 | (70.1–82.3) | ||||
| Yes | 15.78 | (15.4–16.2) | 42.38 | (39.9–44.8) | 3.26 | (2.91–3.65) | 8.04 | (7.6–8.5) | 23.21 | (17.7–29.9) | 2.73 | (1.90–3.94) |
| Illicit Drugs | ||||||||||||
| No | 97.34 | (97.1–97.5) | 76.95 | (74.7–79.0) | 99.05 | (98.9–99.2) | 87.65 | (80.5–92.4) | ||||
| Yes | 2.66 | (2.5–2.9) | 23.05 | (21.0–25.3) | 9.18 | (7.86–10.7) | 0.95 | (0.82–1.09) | 12.35 | (7.6–19.5) | 11.32 | (6.48–19.8) |
| Risk Behavior | ||||||||||||
| Driving Under Influence | ||||||||||||
| No | 91.55 | (91.2–91.9) | 62.19 | (59.7–64.6) | 97.02 | (96.7–97.3) | 71.00 | (62.0–78.6) | ||||
| Yes | 8.45 | (8.1–8.8) | 37.81 | (35.3–40.3) | 6.25 | (5.53–7.06) | 2.98 | (2.7–3.3) | 29.00 | (21.4–38.0) | 9.97 | (6.26–15.9) |
| Drug Selling | ||||||||||||
| No | 99.68 | (99.6–99.7) | 96.58 | (95.5–97.4) | 99.20 | (99.0–99.3) | 97.96 | (94.2–99.3) | ||||
| Yes | 0.32 | (0.26–0.40) | 3.42 | (2.6–4.5) | 9.68 | (6.54–14.3) | 0.80 | (0.66–0.95) | 2.04 | (0.70–5.75) | 2.86 | (0.91–8.96) |
| Theft | ||||||||||||
| No | 99.64 | (99.6–99.7) | 98.62 | (98.0–99.1) | 99.48 | (99.4–99.6) | 98.66 | (95.8–99.6) | ||||
| Yes | 0.36 | (0.29–0.44) | 1.38 | (0.93–2.04) | 3.12 | (1.87–5.21) | 0.52 | (0.42–0.64) | 1.34 | (0.41–4.2) | 2.44 | (0.72–8.26) |
| Attack to Harm | ||||||||||||
| No | 99.65 | (99.6–99.7) | 98.83 | (99.3–99.2) | 99.49 | (99.4–99.6) | 99.21 | (96.7–99.8) | ||||
| Yes | 0.35 | (0.28–0.42) | 1.17 | (0.79–1.72) | 2.35 | (1.39–4.00) | 0.51 | (0.41–0.64) | 0.79 | (0.19–3.25) | 1.47 | (0.34–6.41) |
| Risk Propensity | 1.02 | (1.00–1.03) | 1.89 | (1.82–1.97) | 1.46 | (1.41–1.52) | 0.75 | (0.74–0.77) | 1.80 | (1.56–2.04) | 1.60 | (1.45–1.78) |
|
Criminal Justice System Involvement |
||||||||||||
| Arrest | ||||||||||||
| No | 99.06 | (98.9–99.2) | 95.01 | (93.8–96.0) | 99.66 | (99.6–99.7) | 96.68 | (93.1–98.4) | ||||
| Yes | 0.94 | (0.84–1.06) | 4.99 | (4.0–6.2) | 3.42 | (2.60–1.52) | 0.34 | (0.26–0.45) | 3.32 | (1.57–6.9) | 4.43 | (1.69–11.6) |
Note: Odds ratios adjusted for gender, race/ethnicity, family income, education, marital status, insurance, and survey year. All variables examined are dichotomously coded, except for risk propensity. Risk propensity is an ordinal variable and therefore values shown under the percent columns reflect mean values rather than percentages. Odds ratios and 95% confidence intervals in bold are statistically significant.
Table 4.
Behavioral Health Correlates of Marijuana Use among Late Middle-Aged and Older Adults in the United States
| Have you used marijuana or hashish in the past 12 months? | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Late Middle-Aged Adults (Ages 50 to 64) |
Older Adults (Ages 65 and older) |
|||||||||||
| No (n = 43,932) |
Yes (n = 2668) |
Odds Ratio | No (n = 29,162) |
Yes (n = 256) |
Odds Ratio | |||||||
| % | 95% CI | % | 95% CI | AOR | (95% CI) | % | 95% CI | % | 95% CI | AOR | (95% CI) | |
|
Past Year Conditions |
||||||||||||
| Anxiety | ||||||||||||
| No | 94.57 | (94.3–94.9) | 90.50 | (89.0–91.8) | 96.87 | (96.6–97.1) | 90.67 | (84.6–94.5) | ||||
| Yes | 5.43 | (5.1–5.7) | 9.50 | (8.2–10.9) | 1.38 | (1.10–1.72) | 3.13 | (2.9–3.4) | 9.33 | (5.5–15.4) | 2.87 | (1.41–5.83) |
| Depression | ||||||||||||
| No | 91.22 | (90.8–91.6) | 85.46 | (83.0–87.6) | 95.25 | (94.9–95.6) | 90.31 | (85.0–93.9) | ||||
| Yes | 8.78 | (8.4–9.2) | 14.54 | (12.4–17.0) | 1.53 | (1.22–1.92) | 4.75 | (4.4–5.1) | 9.69 | (6.1–15.0) | 1.75 | (1.41–5.83) |
| HIV/AIDS | ||||||||||||
| No | 99.87 | (99.8–99.9) | 99.16 | (98.5–99.5) | -- | -- | -- | -- | ||||
| Yes | 0.13 | (0.09–0.19) | 0.84 | (0.48–1.48) | 3.50 | (1.80–6.79) | -- | -- | -- | -- | -- | -- |
| Sexually-Transmitted | ||||||||||||
| Disease | ||||||||||||
| No | 99.55 | (99.4–99.6) | 98.63 | (97.7–99.2) | 2.61 | (1.44–4.73) | 99.90 | (99.8–99.9) | 98.38 | (94.4–99.5) | 8.91 | (2.00–39.7) |
| Yes | 0.45 | (0.36–0.56) | 1.37 | (0.83–2.25) | 0.10 | (0.06–0.17) | 1.62 | (0.46–5.59) | ||||
Note: All odds ratios adjusted for gender, race/ethnicity, family income, education, marital status, insurance, and survey year. Additionally, in the examination of behavioral health conditions, we controlled for comorbid health conditions (i.e., anxiety, depression, HIV, sexually transmitted disease). While self-assessment of overall health has been continuously measured sense 2002, data on health problems reported by health provider were not available prior to 2005 in the NSDUH data. As such, data on health problems reported by health provider are for 2005–2014 only. All variables examined are dichotomously coded, except for self-assessment of overall health. Self-assessment of overall health is an ordinal variable and therefore values shown under the percent columns reflect mean values rather than percentages. Odds ratios and 95% confidence intervals in bold are statistically significant.
Finally, given the potential for changes in the association between marijuana use and health and behavioral factors over time, we created multiplicative terms between the survey year variable and substance use/risk behavioral and behavioral health correlates in order to test for interaction effects (Frazier et al., 2004). While no significant interactions were identified among older adults, we did find several significant and substantively meaningful interactions among late middle-aged adults. Specifically, we found that, among late middle-aged adults, the association between marijuana use and criminal justice system involvement decreased significantly over the course of the study (p < .01). That is, we see a stronger marijuana-arrest link in 2002/2003 (AOR = 5.43, 95% CI = 2.10–14.04) than in 2008/2009 (AOR = 3.37, 95% CI = 1.59–7.17) or 2013/2014 (AOR = 2.04, 95% CI = 1.12–3.74). Notably, supplementary trend analyses also revealed that, while a significant increase in marijuana use was observed among late middle-aged adults reporting no criminal justice system involvement (AOR = 1.106, 9% CI = 1.086–1.126), the prevalence of marijuana use among those reporting criminal justice system involvement remained flat between 2002 and 2014. We observed an analogous pattern with respect to the association between marijuana use and use of illicit drugs other than marijuana (p < .01). Specifically, while the link between marijuana use and the use of other illicit drugs remains robust across the study period, we see a marked attenuation of the magnitude of the association between marijuana use and use of other illicit drugs between 2002/2003 (AOR = 19.92, 95% CI = 11.64–34.08), 2008/2009 (AOR = 10.61, 95% CI = 7.43–15.16), and 2013/2014 (AOR = 7.68, 95% CI = 5.65–10.44). Consistent with criminal justice system involvement, our supplementary trend analyses also found that marijuana use increased significantly among those reporting no illicit drug use (AOR = 1.114, 95% CI = 1.09–1.14), but no significant change in trend was observed among those reporting past year use of other illicit drugs. Although effects appear to be smaller, we also identified an interaction effect between survey year and risk propensity (p < .05) in which the marijuana-risk propensity link gradually weakened over time (2002/2003: AOR = 1.80, 95% CI = 1.51–2.15; 2013/2014: AOR = 1.47, 95% CI = 1.35–1.60). Supplementary trend analyses did not find any significant difference in trend among those reporting lower versus higher levels of risk propensity.
5.0.0 Discussion
Findings from the present study provide compelling evidence that marijuana use is on the rise among the late middle-aged and older adults. Indeed, the prevalence of past year marijuana use among late middle-aged adults increased from a low of 2.95% in 2003 to a high of 9.08% in 2014. Beyond the overall test of trend, we also can observe that the largest increases in prevalence were found between 2008 (4.52%) and 2014 (9.08%). While the prevalence of marijuana use is markedly lower among older adults, we see a similar increase in prevalence, from a low of 0.15% in 2003 to a high of 2.04% in 2014. Notably, the upward trend in marijuana use among late middle-aged and older adults remained significant even when accounting for a host of sociodemographic, substance use, risk behavior, and behavioral health factors.
In addition to examining trends in marijuana use, we also examined trends in marijuana-specific protective factors, including strong disapproval of marijuana use, limited access to marijuana, and perceptions of marijuana use as a great risk to one's health and well-being. Among both late middle-aged and older adults, we observed significant decreases in all three of the aforementioned marijuana-specific protective factors, even when controlling for a wide array of confounding factors. Notably, our analyses also provide compelling evidence that the decreases in these protective factors are associated with observed trend changes in marijuana use among late middle-aged and older adults between 2002 and 2014. Additionally, we found, perhaps somewhat predictably, that late middle-aged and older adult marijuana users are substantially more likely than their abstinent counterparts to use other substances, take part in risk behavior, be involved in the criminal justice system, and experience an array of behavioral health conditions. This is the consistent with prior research on marijuana use among older adults (DiNitto and Choi, 2011; Choi et al., 2016) and is certainly in keeping with a vast body of research that has documented the comorbidity of substance use and risky/antisocial behavior (Salas-Wright et al., 2016c; Vaughn et al., 2016c).
While the drug-risk behavior link is well-established, our examination of the changes in the association between marijuana use and risky behavior over time suggests that this relationship may be changing among late middle-aged marijuana users. That is, we found that—as marijuana use became more prevalent and marijuana perceptions became more tolerant—the relationship between marijuana use and key behavioral outcomes (i.e., risk propensity, other illicit drug use, and criminal justice system involvement) weakened noticeably. Critical as this finding may be, regretfully, the NSDUH data do not allow us to fully disentangle why the observed changes in the marijuana-risk behavior link are observed. We believe that several possibilities exist. First, it may be that, as marijuana use has become more normative and tolerated, it has, in effect, become less of an antisocial or risky behavior; therefore, its association with other risk behaviors may be lessening. Second, a related possibility is that marijuana use may be disproportionately on the rise among late middle-aged adults who, by and large, are not involved in other risky, deviant, or criminal behaviors. This would be in keeping with our finding that increases in marijuana use among late middle-aged adults was driven primarily by those reporting no criminal justice system involvement and no comorbid use of illicit drugs. Finally, the weakened relationship between marijuana use and risky behaviors—including criminal justice system involvement—may be attributable to the fact that marijuana use and possession is more and more decriminalized with passing of medical and recreational marijuana laws and no jail terms in many states.
Findings from the present study should be interpreted in light of several limitations. First, the NSDUH data do not allow us, in our analysis of secular trends, to account for cohort effects. It is, of course, possible that the changes in trend observed are influenced more by cohort effects rather than calendar effects. Third, the publically available NSDUH data file does not allow researchers to examine state-level differences among survey respondents. This is, of course, a noteworthy limitation due to state-level differences in marijuana policy across the US (see Stoner, 2016). Fourth, while we pooled data from 2002 through 2014 in order to examine the correlates of marijuana use, the NSDUH data are cross-sectional and, therefore, we cannot draw any causal conclusions from the observed associations. Finally, despite a very large sample size, relatively few older adults reported past year marijuana use. This can lead to problems with model stability and statistical power, particularly when looking at associations between marijuana use and low prevalence behavioral/health phenomena. As such, while we carried out sensitivity analyses to address this issue, findings for older adults should nevertheless be interpreted with caution.
6.0.0 Conclusions
Findings from the present study provide robust evidence to suggest that marijuana use among late middle-aged and older adults has increased markedly in recent years, with the most evident changes observed between 2008 and 2014. Additionally, we see a corresponding drop in the proportion of late middle-aged and older adults reporting strong disapproval of marijuana use, limited access to marijuana, and the belief that marijuana is of great risk to one's health and well-being. Evidence that marijuana users are more likely to have issues with comorbid substance use, take part in risky behavior and be involved in the criminal justice system, and experience key behavioral health problems underscores the importance of keeping a very close eye on these trends as the nation continues to make policy decisions regarding the medicalization, decriminalization, and legalization of marijuana. Future research should continue to examine trends in marijuana use among late-middle-aged and older adults, including a careful examination of trends in regular marijuana use and cannabis use disorder.
Highlights.
Marijuana use increased among middle-aged and older adults between 2002 and 2014.
We observed a decline in the proportion of adults who disapprove of marijuana use.
Declines in marijuana-specific protective factors are linked with increases in use.
Acknowledgments
Author Disclosures
Role of Funding Source:
This research was supported in part by the National Institute on Drug Abuse at the National Institutes of Health (R25 DA030310; PI: James C. Anthony).
None.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared
Contributors
Dr. Salas-Wright lead all writing and statistical analyses. Dr. Vaughn contributed to the study conceptualization and data analytic plan, as well as the writing and editing of the entire manuscript. Dr. Cummings-Vaughn contributed to the introduction and discussion sections, and the editing of the manuscript. Ms. Holzer and Ms. AbiNader led the review of the literature and provided critical input on the data analysis plan and the presentation of the tables and figures. Dr. Nelson and Mr. Oh provided statistical consultation and contributed the analytic plan, data coding, and data presentation. All authors have read and approve of the submission of this manuscript to Drug and Alcohol Dependence.
References
- Centers for Disease Control and Prevention. Conducting Trend Analyses of YRBS Data. 2016 Retrieved from: http://www.cdc.gov/healthyyouth/data/yrbs/pdf/2015/2015_yrbs_conducting_trend_analyses.pdf.
- Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun. Stat. Simul. Comput. 2010;39(4):860–864. [Google Scholar]
- Choi NG, DiNitto DM, Marti CN. Older Marijuana users: life stressors and perceived social support. Drug Alcohol Depend. 2016 doi: 10.1016/j.drugalcdep.2016.10.012. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry. 2016;3(10):954–964. doi: 10.1016/S2215-0366(16)30208-5. [DOI] [PubMed] [Google Scholar]
- DiNitto DM, Choi NG. Marijuana use among older adults in the USA: user characteristics, patterns of use, and implications for intervention. Int. Psychogeriatr. 2011;23(05):732–741. doi: 10.1017/S1041610210002176. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. Jama. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Guttmannova K, Cambron C, Rhew IC, Oesterle S. Examination of the divergence in trends for adolescent marijuana use and marijuana-specific risk factors in Washington State. J. Adolesc. Health. 2016;0(0):25–63. doi: 10.1016/j.jadohealth.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. J. Couns. Psychol. 2004;51(1):115–134. [Google Scholar]
- Geiger J. One in eight U.S. adults say they smoke marijuana. 2016 Retrieved from http://www.gallup.com/poll/194195/adults-say-smoke-marijuana.aspx.
- Han BH, Sherman S, Mauro PM, Martins SS, Rotenberg J, Palamar JJ. Demographic Trends among Older Cannabis Users in the United States, 2006–2013. Addiction. 2016 doi: 10.1111/add.13670. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H. Prevalence of marijuana use disorders in the united states between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015a;72(12):1235. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O'Malley PM, Feng T. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015b;2(7):601–608. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Grant BF. Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions–III. Am. J. Psychiatry. 2016;173(6):588–599. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RM, Fairman B, Gilreath T, Xuan Z, Rothman EF, Parnham T, Furr-Holden CDM. Past 15-year trends in adolescent marijuana use: Differences by race/ethnicity and sex. Drug Alcohol Depend. 2015;155:8–15. doi: 10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech R, Bachman J, Schulenberg JE. Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2014. Monitoring the Future: National survey results on drug use: 1975–2014. [Google Scholar]
- Johnson LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. College students & adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- Lee MA. Smoke Signals: A Social History Of Marijuana – Medical, Recreational And Scientific. New York: Simon and Schuster; 2012. [Google Scholar]
- McCarthy J. One in eight u.s. adults say they smoke marijuana. 2016 Retrieved from http://www.gallup.com/poll/194195/adults-say-smoke-marijuana.aspx.
- Ortman JM, Velkoff VA, Hogan H. An aging nation: The older population in the United States. Washington, DC: US Census Bureau; 2014. 25-1140. [Google Scholar]
- Substance Abuse and Mental Health Administration (SAMHSA). Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2014. 2014
- Substance Abuse and Mental Health Data Archive. How do I account for complex sampling design when analyzing NSDUH data? 2014 Retrieved March 8, 2016, from http://samhda-faqs.blogspot.com/2014/03/how-do-i-account-complex-sampling.html.
- Salas-Wright CP, Vaughn MG. The changing landscape of adolescent marijuana use risk. J. Adolesc. Health. 2016a;59(3):246–247. doi: 10.1016/j.jadohealth.2016.06.018. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG. Marijuana use among young people in an era of policy change: What does recent evidence tell us? Am. J. Drug Alcohol Abuse. 2016b doi: 10.1080/00952990.2016.1226319. Advanc online publication. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Reingle-Gonzalez JM. Drug Abuse and Antisocial Behavior: A Biosocial Life-Course Approach. New York, NY: Palgrave Macmillan; 2016c. [Google Scholar]
- Salas-Wright CP, Vaughn MG, Perron BE, Gonzalez JMR, Goings TC. Changing perspectives on marijuana use during early adolescence and young adulthood: Evidence from a panel of cross-sectional surveys. Drug Alcohol Depend. 2016d doi: 10.1016/j.drugalcdep.2016.09.026. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Todic J, Córdova D, Perron BE. Trends in the disapproval and use of marijuana among adolescents and young adults in the United States: 2002–2013. Am. J. Drug Alcohol Abuse. 2015;41(5):392–404. doi: 10.3109/00952990.2015.1049493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoner SA. Marijuana use by older adults. Alcohol and Drug Abuse Institute, University of Washington; 2016. Retrieved from: http://learnaboutmarijuanawa.org/factsheets/olderadults.htm. [Google Scholar]
- Vaughn MG, Nelson EJ, Salas-Wright CP, DeLisi M, Qian Z. Handgun carrying among white youth increasing in the United States: New evidence from the National Survey on Drug Use and Health 2002–2013. Prevent. Med. 2016a;88:127–133. doi: 10.1016/j.ypmed.2016.03.024. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Nelson EJ, Salas-Wright CP, Qian Z, Schootman M. Racial and ethnic trends and correlates of non-medical use of prescription opioids among adolescents in the United States 2004–2013. J. Psychiatr. Res. 2016b;73:17–24. doi: 10.1016/j.jpsychires.2015.11.003. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, Reingle-Gonzalez JM. Addiction and crime: The importance of asymmetry in offending and the life-course. J. Addict. Dis. 2016c:1–5. doi: 10.1080/10550887.2016.1189658. http://doi.org/10.1080/10550887.2016.1189658. [DOI] [PubMed] [Google Scholar]