Abstract
Femoroacetabular impingement (FAI) is an increasingly recognized cause of hip pain. This pathology often involves abnormal femoral neck shape (cam-type FAI), acetabular over coverage (pincer-type FAI), or mixed pathology. Surgical treatment of this entity includes labral repair and femoral head-neck osteochondroplasty. A mindful arthroscopic technique is of paramount importance, because maintaining the integrity of the labrum and a corresponding neck volume has been reported to be vital in maintaining the hip suction seal. Arthroscopic resection of the cam deformity must be performed with care to ensure appropriate femoral offset and maintenance of appropriate femoroacetabular contact. Although the most common cause of failure after hip arthroscopy is incomplete resection of a cam lesion, a previously unrecognized complication is excessive cam resection that can also lead to excessive femoral offset and loss of the suction seal. The purpose of this technical note is to describe the technique for arthroscopic recognition of excessive cam decompression leading to loss of the suction seal and a surgical treatment approach using the “remplissage” technique.
Femoroacetabular impingement is a well-known cause of hip pain, chondrolabral damage, and an osteoarthritis precursor in the hip joint.1, 2, 3 It is defined as an abnormality of the femoral head-neck junction or by acetabular overcoverage causing impingement and soft tissue failure.4 In cases of an abnormal femoral head-neck junction, the preferred treatment is to partially resect the bony overgrowth in the femoral neck (cam lesion), thereby restoring the normal femoral head-neck offset, and alleviating mechanical impingement.
In general, the cam lesion is located anterolaterally in the femoral neck and requires a resection that begins 1 cm lateral from the labral margin, is less than 1 cm deep, 8 mm in length from proximal to distal, and 15 mm in width from medial to lateral.5 Although not previously reported as a potential complication, over-resection is a concern. In such cases, patients can become symptomatic because of the loss of the suction seal5 and the consequent development of microinstability.6, 7
In our tertiary referral practice, we have seen rare complications such as over-resection of the femoral neck. This has necessitated the development of techniques to restore near-normal anatomy and recreate native hip biomechanics when possible. The purpose of this technical note is to describe a technique to correct the over-resection of the femoral head-neck junction after a hip arthroscopy that resulted in loss of the fluid suction seal using an iliotibial band (ITB) allograft to fill the bone defect (hip “remplissage”).
Preoperative Evaluation
A thorough history, physical examination, and radiographic evaluation are paramount for an accurate diagnosis. Patients will often report a period of improvement after their index surgery but then note a rapid return of pain that is characteristically in the groin or anterior hip. Because over-resection results in loss of the suction seal, signs and symptoms will be very similar to that for a labral tear, or consistent with microinstability.8
Findings on imaging can be subtle and may only be apparent on advanced imaging studies. Conventional radiography may show a small lucency at the anterolateral femoral head-neck junction in the area of expected cam resection. Magnetic resonance imaging may reveal an area of impression at the head-neck junction instead of a smooth contour that is suggestive of over-resection and loss of appropriate labral contact (Figs 1 and 2). Because of the subtlety of the diagnosis, a combination of the above should be performed, and the surgeon should maintain a high index of suspicion in patients with such findings. After a period of nonsurgical management, patients with such findings may be candidates for revision surgical intervention to restore the native suction seal and stability of the hip.
Fig 1.
(A) An axial T1-weighted magnetic resonance (MR) image of the right hip showing an area of excessive resection at the femoral head-neck junction that resulted in the loss of labral contact and suction seal (red arrow). (B) A sagittal T2-weighted MR image of the same hip further showing excessive resection of the femoral head-neck junction with loss of the normal femoral head-neck contour (white arrow). (FH, femoral head.)
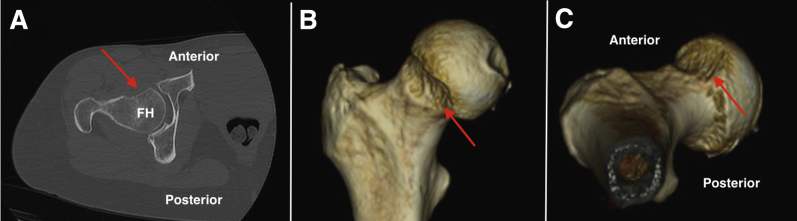
Fig 2.
(A) An axial computed tomography (CT) image of a right hip that has undergone an over-resection of a previous cam lesion. Three-dimensional coronal (B) and axial (C) CT reconstruction of the proximal femur further showing areas of cam excessive resection of the femoral head-neck junction. Areas of excessive resection are noted with red arrows. (FH, femoral head.)
Surgical Technique
Anesthesia and Patient Positioning
The patient is placed in a modified supine position on a traction table (Steris/Amsco, Mentor, OH). A combined epidural with a lumbar plexus sciatic regional block is our preferred anesthetic modality. After induction, a bilateral hip examination is performed to assess for the hip range of motion. To prevent neurologic complications an extra-wide perineal post is used to minimize pressure on the pudendal nerve and to force the femoral head laterally, shifting the vector of forces. The feet are placed in padded boots and secured. Traction is applied to the operative limb between 10 and 25 kg of force, with gentle countertraction applied to the contralateral limb (confirmed with a “vacuum sign” and 1 cm of joint distraction). The leg is positioned with 15° of internal rotation, 10° of lateral tilt, 10° of flexion, and neutral abduction. The time of traction application is noted, and continuous traction time should be limited to less than 2 hours.
Diagnostic Arthroscopy and Intraoperative Examination
Anterolateral and midanterior portals are established in the modified supine position. A 70° arthroscope (Smith & Nephew, Andover, MA) is used to perform a diagnostic arthroscopy, evaluating the articular surfaces, labrum, and other associated pathologies9 (Video 1). After the labrum and other central compartment pathologies have been appropriately addressed, traction is released and the femoral neck in the peripheral compartment is visualized.
A dynamic examination is then performed, ranging the hip in various degrees of flexion/extension and internal/external rotation. The presence of a cam over-resection can be noted as a space between the labrum and femoral head-neck junction in mid-ranges of flexion, which represents a loss of the suction seal (Fig 3). The size of the defect can be measured using a standard arthroscopic probe, noting the depth, width, and length. The defect is then debrided with a mechanical shaver and arthroscopic burr to expose a healthy bone bed that promotes healing and graft incorporation.
Fig 3.
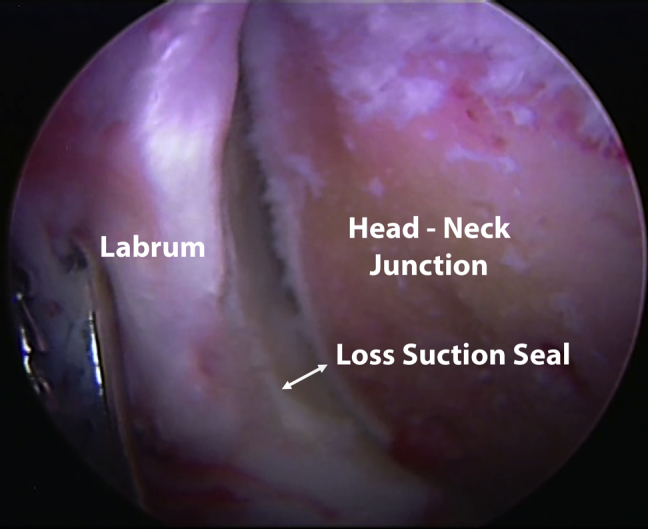
Arthroscopic image of a right hip showing loss of contact between the labrum and femoral head-neck junction as the hip is flexed seen through the anterolateral portal.
Graft Preparation
An ITB allograft (Allosource, Centennial, CO) is used and shaped based on the defect size. Hanging stitches are created on the ends of the graft to help with fashioning the graft (Fig 4). Preparation of the graft is accomplished with a baseball stitch performed in a longitudinal fashion in one direction and nonlocked continuous suture in the reverse direction, using 2-0 Vicryl (Ethicon, Somerville, NJ). Additional sutures can be placed at both ends to avoid graft tearing that can occur with suture passage.
Fig 4.
Intraoperative photograph of the iliotibial band allograft is used to create a graft appropriate to the dimensions of the defect.
Graft Insertion and Fixation
From the anterolateral portal a 2.9-mm Osteoraptor (Smith & Nephew, Memphis, TN) suture anchor preloaded with a No. 2 Vicryl is placed in the center of the defect (Fig 5). A large cannula is placed in the anterolateral portal and the sutures brought though the cannula (Fig 6). One limb of the suture is passed through the middle of the graft and the graft is then delivered through the cannula into the joint with the aid of an arthroscopic knot pusher. The graft is positioned in the defect and then an arthroscopic knot is tied to secure the graft.
Fig 5.

Arthroscopic image as viewed through the midanterior portal of a right hip. A 2.9-mm Osteoraptor suture anchor preloaded with a No. 2 Vicryl is placed in the center of the defect for later passage and securing the iliotibial band allograft.
Fig 6.

Intraoperative photograph of a right hip with an arthroscopic cannula placed in the anterolateral portal (ALP). One limb from the 2.9-mm Osteoraptor suture anchor is passed through the center of the iliotibial band allograft (ITB graft) and used to shuttle the graft into the joint through a large cannula in the ALP. The arthroscope is positioned in the midanterior portal (MAP).
In addition, 1.5-mm JuggerKnot suture anchors (Biomet, Warsaw, IN) are placed along the length of the defect and suture limbs are passed in a pierced fashion using a pointed suture passer (Arthropierce, Smith & Nephew) through the graft to firmly affix it to the underlying bony bed. It is important to ensure that the graft is fully affixed to the area of the defect (Fig 7).
Fig 7.

Arthroscopic image of a right hip as viewed through the midanterior portal. With the graft in place to fill in the cam over-resection defect, the suction seal is restored.
The remplissage is evaluated dynamically in all planes of motion to assess the fixation, position of the graft, and re-creation of the suction seal on the femoral head and neck. There should be appropriate frictionless contact between the graft and the labrum throughout full range of motion.
Rehabilitation
The postoperative protocol is the same as used in a regular labral repair or reconstruction.10, 11 To promote early motion and avoid the formation of scar tissue, the authors prefer that patients begin gentle cyclic motion with the use of a stationary bicycle with no resistance within 4 hours after surgery, and to use a continuous passive motion machine until 2 to 3 weeks after surgery. Circumduction exercises are performed 4 times a day for the first 2 weeks. Patients are kept at 10 kg of flatfoot weight bearing for 2 to 3 weeks. Patients are advised to wear an antirotational bolster and a hip brace to prevent stress of the repaired capsule. To prevent flexor contracture, patients are asked to lie prone for 2 hours per day.
Discussion
This surgical technique describes our preferred method to address a femoral neck deficiency as a result of a previous over-resection of a cam-type impingement using a folded ITB allograft in the femoral defect to reestablish the fluid suction seal.
Remplissage has been described and validated in the shoulder literature to address posterosuperior bony defects of the humeral head.12, 13 The bony defect is addressed with a capsulotenodesis using the capsule and infraspinatus muscle. One of the mechanisms of success is the filling in of the defect due to healing of the soft tissue to the underlying bony impression.12 In a similar fashion, the ITB allograft should incorporate into the head-neck junction defect.
Disruption of the fluid seal can cause imbalances within the hip joint such as impaired lubrication and nutrition of the cartilage and thereby an accelerated degenerative process of the joint.14, 15 Labral pathologies are being increasingly recognized as a possible cause for fluid seal disruption. Similarly, a disruption due to bony loss at the head-neck junction will affect the status of the fluid seal. Addressing this pathology should restore the fluid seal.
This technique provides a solution to an under-reported problem (Tables 1 and 2). However, surgeons should be careful not to place a graft that is too large, thereby recreating a cam-type impingement. Conversely, inadequately sizing the graft can result in incomplete filling of the defect and thus a failure in restoring the fluid seal. Although this technique may be challenging, it provides a less technically demanding and less invasive solution compared with a bone grafting technique.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Inadequate cam resection is the leading cause of failure of arthroscopy for femoroacetabular impingement (FAI). | Excessive cam resection is an under-recognized cause of failure in arthroscopic FAI surgery. |
| Iliotibial band allograft is a useful method of filling a femoral head-neck junction defect. | Do not make the graft too thick as it may reproduce the effects of a cam lesion. |
| Place the first suture anchor in the center of the defect and suture limbs through the center of the graft to center it appropriately. | Incomplete filling of the defect may not reconstitute the suction seal. |
Table 2.
Advantages and Limitations of This Technique
| Advantages | Limitations |
|---|---|
| Iliotibial (IT) band allograft is a readily available graft option. | The graft does not reconstitute bony architecture. |
| The IT band is well suited for filling in of smaller defects (<5 mm depth). | Larger defects may require a bone grafting technique. |
| The suction seal is reestablished with appropriate contact between the labrum and femoral head-neck junction. | There are no biomechanical or long-term studies to prove efficacy and durability. |
In conclusion, remplissage with an ITB allograft is a technique for addressing an unrecognized complication of hip arthroscopy for addressing femoroacetabular impingement. Despite being technically demanding, this technique reestablishes anatomic contact between the labrum and femoral head-neck junction, reconstituting the labral seal and therefore allows for improved hip stability. We recommend this technique to address femoral neck cam over-resection; however, further studies are required to evaluate the efficacy and durability of the procedure.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.J.P. receives support from Arthrex, Ossur, Siemens, Smith & Nephew, Vail Valley Surgery Center, Steadman Philippon Research Institute, Vail Health Services, ISHA, ASIAM, ConMed Linvatec, Bledsoe, Slack, Elsevier, Donjoy, Arthrosurface, HIPCO, and MIS.
Supplementary Data
Standard anterolateral and midanterior portals are established in the modified supine position in a right hip. A 70° arthroscope is used to perform a diagnostic arthroscopy. After the labrum and other central compartment pathologies have been appropriately addressed, traction is released and the femoral neck in the peripheral compartment is visualized. A dynamic examination is then performed to assess for the presence of a cam over-resection (loss of suction seal). Next, the size of the defect is measured using a standard arthroscopic probe, noting the depth, width, and length. The bony bed is then prepared with a mechanical shaver and arthroscopic burr to expose a healthy bone bed that promotes healing and graft incorporation. An iliotibial band allograft is used as the graft. Hanging stitches are created on the ends of the graft to help with fashioning the graft. Preparation of the graft is accomplished with a baseball stitch performed in a longitudinal fashion in one direction and a nonlocked continuous suture in the reverse direction. From the anterolateral portal a suture anchor preloaded with a No. 2 Vicryl is placed in the center of the defect. A large cannula is placed in the anterolateral portal and the sutures brought though the cannula. One limb of the suture is passed through the middle of the graft and the graft is then delivered through the cannula into the joint with the aid of an arthroscopic knot pusher. The graft is positioned in the defect and then an arthroscopic knot is tied to secure the graft. Additional anchors are placed along the length of the defect and suture limbs are passed in a pierced fashion using a pointed suture passer through the graft to firmly affix it to the underlying bony bed. It is important to ensure that the graft is fully affixed to the area of the defect. Finally, the remplissage is evaluated dynamically in all planes of motion.
References
- 1.Beck M., Kalhor M., Leunig M., Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 2.Ganz R., Parvizi J., Beck M., Leunig M., Nötzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R., Leunig M., Leunig-Ganz K., Harris W.H. The etiology of osteoarthritis of the hip: An integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Philippon M.J., Stubbs A.J., Schenker M.L., Maxwell R.B., Ganz R., Leunig M. Arthroscopic management of femoroacetabular impingement: Osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571–1580. doi: 10.1177/0363546507300258. [DOI] [PubMed] [Google Scholar]
- 5.Vaughn Z.D., Safran M.R. Arthroscopic femoral osteoplasty/chielectomy for cam-type femoroacetabular impingement in the athlete. Sports Med Arthrosc. 2010;18:90–99. doi: 10.1097/JSA.0b013e3181dfce63. [DOI] [PubMed] [Google Scholar]
- 6.Kalisvaart M.M., Safran M.R. Microinstability of the hip-it does exist: Etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2:123–135. doi: 10.1093/jhps/hnv017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Safran M.R. The acetabular labrum: Anatomic and functional characteristics and rationale for surgical intervention. J Am Acad Orthop Surg. 2010;18:338–345. doi: 10.5435/00124635-201006000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Groh M.M., Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2:105–117. doi: 10.1007/s12178-009-9052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Philippon M.J., Faucet S.C., Briggs K.K. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2:e73–e76. doi: 10.1016/j.eats.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ejnisman L., Philippon M.J., Lertwanich P. Acetabular labral tears: Diagnosis, repair, and a method for labral reconstruction. Clin Sports Med. 2011;30:317–329. doi: 10.1016/j.csm.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 12.Boileau P., O'Shea K., Vargas P., Pinedo M., Old J., Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012;94:618–626. doi: 10.2106/JBJS.K.00101. [DOI] [PubMed] [Google Scholar]
- 13.Purchase R.J., Wolf E.M., Hobgood E.R., Pollock M.E., Smalley C.C. Hill-sachs “remplissage”: An arthroscopic solution for the engaging hill-sachs lesion. Arthroscopy. 2008;24:723–726. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Philippon M.J., Nepple J.J., Campbell K.J. The hip fluid seal—Part I: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22:722–729. doi: 10.1007/s00167-014-2874-z. [DOI] [PubMed] [Google Scholar]
- 15.McCarthy J.C., Noble P.C., Schuck M.R., Wright J., Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;(393):25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Standard anterolateral and midanterior portals are established in the modified supine position in a right hip. A 70° arthroscope is used to perform a diagnostic arthroscopy. After the labrum and other central compartment pathologies have been appropriately addressed, traction is released and the femoral neck in the peripheral compartment is visualized. A dynamic examination is then performed to assess for the presence of a cam over-resection (loss of suction seal). Next, the size of the defect is measured using a standard arthroscopic probe, noting the depth, width, and length. The bony bed is then prepared with a mechanical shaver and arthroscopic burr to expose a healthy bone bed that promotes healing and graft incorporation. An iliotibial band allograft is used as the graft. Hanging stitches are created on the ends of the graft to help with fashioning the graft. Preparation of the graft is accomplished with a baseball stitch performed in a longitudinal fashion in one direction and a nonlocked continuous suture in the reverse direction. From the anterolateral portal a suture anchor preloaded with a No. 2 Vicryl is placed in the center of the defect. A large cannula is placed in the anterolateral portal and the sutures brought though the cannula. One limb of the suture is passed through the middle of the graft and the graft is then delivered through the cannula into the joint with the aid of an arthroscopic knot pusher. The graft is positioned in the defect and then an arthroscopic knot is tied to secure the graft. Additional anchors are placed along the length of the defect and suture limbs are passed in a pierced fashion using a pointed suture passer through the graft to firmly affix it to the underlying bony bed. It is important to ensure that the graft is fully affixed to the area of the defect. Finally, the remplissage is evaluated dynamically in all planes of motion.