Abstract
Study Objectives:
Sleep disturbances are well documented in relation to trauma exposure and posttraumatic stress disorder (PTSD), but correlates of such disturbances remain understudied in veteran populations. We conducted a preliminary study of sleep disturbances in Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn veterans (n = 133; mean [standard deviation] age = 29.8 [4.7] y).
Methods:
Veterans were assigned to one of three groups based on responses to the Clinician Administered PTSD Scale: control (no trauma-exposure [TE] or PTSD), TE, and PTSD. Sleep disturbance was assessed using the Pittsburgh Sleep Quality Index (PSQI). Measures of resilience, trauma load, personality, coping, alcohol use, and mild traumatic brain injury were also assessed via self-report.
Results:
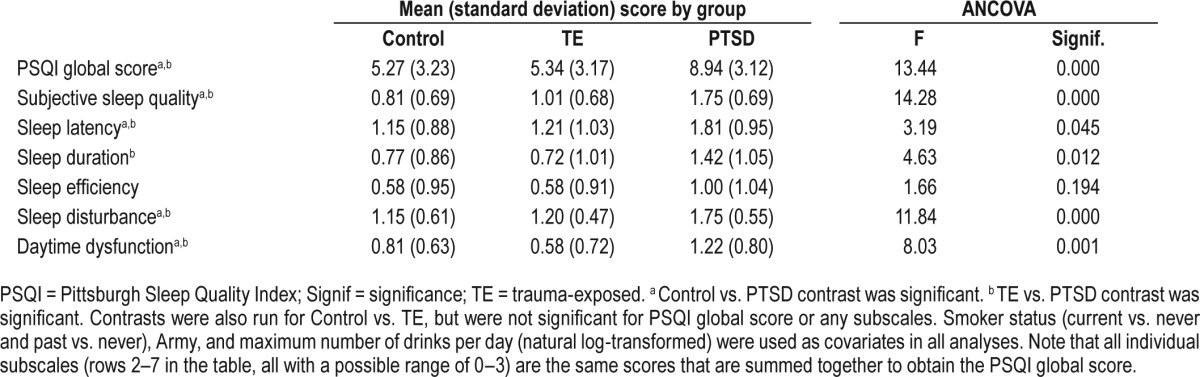
The PTSD group had significantly more disturbed sleep (PSQI global score mean = 8.94, standard deviation = 3.12) than control (mean = 5.27, standard deviation = 3.23) and TE (mean = 5.34, standard deviation = 3.17) groups, but there were no differences between TE and control. The same pattern emerged across most PSQI subscales. Results of linear regression analyses indicated that current smoking, Army (versus other military branches), neuroticism, and using substances to cope were all significant correlates of higher sleep disturbance, whereas post-deployment social support was associated with less sleep disturbance. However, when combined together into a model with PTSD status, only neuroticism and substance use coping remained significant as predictors of more disturbed sleep.
Conclusions:
These initial findings suggest that TE itself may not be an independent risk factor for disturbed sleep in veterans, and that neurotic personality and a tendency to cope by using substances may partially explain sleep disturbance, above and beyond a diagnosis of PTSD.
Citation:
Lind MJ, Brown E, Farrell-Carnahan L, Brown RC, Hawn S, Berenz E, McDonald S, Pickett T, Danielson CK, Thomas S, Amstadter AB. Sleep disturbances in OEF/OIF/OND veterans: associations with PTSD, personality and coping. J Clin Sleep Med 2017;13(2):291–299.
Keywords: combat, coping, personality, PTSD, sleep, trauma, veterans
INTRODUCTION
Exposure to combat trauma is prevalent among veterans of Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND),1 with 95% of returning veterans reporting at least one combat trauma experience.2 This includes events such as combat patrols or other dangerous duty, witnessing violence, taking direct fire, and exposure to severe human suffering.1,2 Trauma exposure is associated with a range of negative sequelae, such as posttraumatic stress disorder (PTSD),3 which affects approximately 23% of OIF/ OEF veterans.4 PTSD is a costly disorder to the individual and society, as it affects overall quality of life, interpersonal relationships, job performance, and mental and emotional well-being.1,3,5
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although it is well established that veterans (particularly those with PTSD) have poor sleep and many studies have examined this, few studies have investigated how sleep may differ in a three-group model (controls without trauma exposure, trauma-exposed individuals, and individuals with PTSD). Further, there is a need for more studies that examine correlates of disturbed sleep in veterans, beyond demographics and psychiatric comorbidities.
Study Impact: We have shown that trauma exposure itself may not be an independent risk factor for disturbed sleep in veterans, further emphasizing the importance of targeting sleep in this population. Additionally, neuroticism and substance use coping may also be areas to focus on when addressing disturbed sleep in veterans.
Another debilitating condition that has been associated with both PTSD and trauma exposure itself is difficulty sleeping. Sleep disturbances are reported following a wide variety of traumatic events and are also commonly endorsed by those individuals in whom PTSD develops.5–8 Moreover, such disturbance is a key component of PTSD diagnostic criteria.9 It is well documented that sleep complaints are common among OEF/OIF veterans,5,10,11 particularly those returning from combat zones.8 However, most studies of sleep in veteran populations have focused on comparisons across individuals with and without PTSD,5,8,11 neglecting examination of the specific effects that trauma exposure itself may have on sleep in this population. Civilian samples have occasionally been included for comparison,12 but more research is needed to determine the effects of trauma exposure itself on sleep in veterans.
The consequences of chronic sleep disturbance can also be devastating to the individual, ultimately affecting job performance, quality of life, and both mental and physical health status.13 Further, recent evidence suggests that sleep disturbances may influence the development and course of subsequent psychopathology (e.g., depression, PTSD).14,15 Fragmentation in rapid eye movement sleep specifically is predictive of PTSD.16–18 Numerous studies have been conducted to identify correlates of sleep disturbance in veteran samples,5,7 yet few have incorporated a three-group design that separates “true” controls from trauma-exposed controls and individuals with PTSD. In one of the first studies that examined factors beyond demographics and psychopathology in OEF/OIF veterans, positive cognitive coping strategies (such as cognitive distraction) and unit support demonstrated negative associations with sleep problems in individuals with PTSD.5 Further investigation of other potential protective influences on sleep in OEF/ OIF veterans with and without combat exposure and PTSD is warranted.
Thus, this study aimed to address the outlined gaps in the existing sleep literature of OEF/OIF veterans, using preliminary data from an ongoing study of this population. We used a three-group design; such that individuals were separated into control (no lifetime trauma exposure [TE] or PTSD), combat TE, and current (past 30-day) combat-related PTSD groups. The first aim was to evaluate group differences in sleep disturbance scores. It was hypothesized that TE and PTSD would be incrementally associated with greater sleep disturbance (i.e., PTSD > TE > control). The second aim was to identify psychosocial correlates of sleep disturbance, above and beyond the influence of TE and PTSD. It was hypothesized that greater trauma load, lower scores on resilience-related measures, negative personality traits, and less adaptive coping methods would be significantly associated with greater sleep disturbances.
METHODS
Sample
The sample included 133 OEF/OIF/OND veterans who participated in an ongoing study designed to examine the effects of combat trauma and stress reactivity on drinking behaviors in veterans. Participants were recruited through the community, as well as the university and Veterans Affairs hospitals, by advertising (e.g., flyers, Internet), and through collaborations with other researchers. All study activities were approved by the Institutional Review Board.
Eligible participants were between 21–40 y old, able to provide informed consent, and regular drinkers (drank alcohol at least 4 days in the month prior to the study screener) who did not meet Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria for alcohol dependence (those meeting criteria for alcohol abuse were not excluded) or current major depressive disorder as assessed by the Mini-International Psychiatric Interview (MINI).19 Other exclusion criteria included abuse or dependence on other illicit drugs (other than cannabis); women who were pregnant or nursing, or who suspected they might be pregnant; history of a moderate or severe traumatic brain injury (TBI); the presence of a blood-clotting disorder; and presence of a medical condition or medication affecting hypothalamic-pituitary-adrenal axis functioning (e.g., antidepressants). Further, participants could not be taking sleep medications at the time of their second session, and thus were not likely regular users.
Group assignments
Group assignments were based on diagnostic interviews from the Clinician Administered PTSD Scale (CAPS) DSM-IV version,20 which ascertains current and lifetime PTSD (see end-note A). The CAPS demonstrates high interrater reliability (i.e., at or above 0.90) and internal consistency on each of the three PTSD symptom clusters (range 0.8 to 0.9), and correlates strongly (i.e., above 0.7) with other measures of PTSD.21
To be eligible for the Control group, participants could not have had a history of a DSM-IV Criterion A traumatic event (combat or otherwise; DSM-IV Criterion A requires that the person has experienced, witnessed, or been confronted with an event or events that involve actual or threatened death or serious injury, or a threat to the physical integrity of oneself or others, and that the person's response involved intense fear, helplessness, or horror).22 To be eligible for the Combat Trauma Exposed group (TE), participants must have had a history of a Criterion A combat traumatic event during OIF/OEF/OND deployment but not meet the DSM-IV criteria for PTSD (Current or Lifetime), as defined by CAPS score ≤ 25. To be eligible for the PTSD group, participants must have had a history of combat trauma meeting Criterion A and have met current criteria for PTSD, as defined by DSM-IV (exposure to a Criterion A event, endorsement of at least one cluster B symptom, three or more cluster C symptoms, at least two cluster D symptoms, and functional impairment) and a CAPS severity score ≥ 40. The described analyses used only individuals with group assignments. Note that participants in both the TE and PTSD groups may have experienced non-combat “lifetime” traumatic events meeting Criterion A before or after combat exposure. Participants in all groups were required to be regular drinkers.
Measures
Demographic variables
Standard demographic variables, including sex, race, ethnicity, age, marital status, education, income, and employment status, were asked of all participants via questionnaire at initial visit. Veteran-specific items, including military branch (collapsed into Army versus other for analysis), rank, current status, number of deployments, and mild traumatic brain injury (TBI) were also assessed. Additionally, participants were asked about smoking status within the demographic questions, and then assessed for at-risk drinking behavior as defined by National Institute on Alcohol Abuse and Alcoholism published criteria (more than 4 standard drinks a day OR more than 14 drinks per week for men; more than 3 standard drinks a day OR 7 or more drinks per week for women).23 Further, additional information on the quantity and frequency of alcohol consumption within the past month was assessed via the alcohol Timeline Follow Back (TLFB).24
Sleep
Sleep disturbances were assessed using the Pittsburgh Sleep Quality Index (PSQI).25 The PSQI is a self-report instrument containing 9 questions (19 total items) that measure sleep quality and disturbance over a 1-mo period. All scores are combined to derive a global PSQI score. There are seven subscales: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime functioning. The PSQI also has an item that queries nightmares. For our analyses, we created a modified global PSQI score that did not use the sleep medication sub-scale, given our study's exclusion criteria. Cronbach's alpha for this modified global PSQI score (using the six component sub-scales), was 0.765. Throughout this article, we will continue to refer to this measure as “PSQI global score.”
Trauma exposure
Trauma exposure history was assessed with the Life Events Checklist (LEC),26 which includes a list of 17 potentially traumatic events (e.g., sexual assault, physical assault). Participants indicate whether they have experienced each event, have witnessed the event happening to someone else, or have learned about the event happening to someone close to them. In the following analyses, we have created and used a sum score of all events endorsed as “self.” The sum score was created if a participant answered at least 15 of 17 LEC self items.
Deployment-related measures
The Deployment Risk and Resiliency Inventory (DRRI)27 is a series of scales assessing 14 key deployment-related risk and resilience factors with demonstrated implications for veterans' long-term health including the veteran's exposure to various combat-related experiences, level of social support prior to and following deployment, and the effect of deployment on family life. Estimates of reliability were 0.80 or higher for most DRRI subscales (with prior stressors and post-deployment stressors being the exceptions) across several veteran samples.28 Scales used in the current analyses include the following:
POST-DEPLOYMENT SUPPORT (DRRI SECTION L): This section includes 15 items related to post-deployment social support that are rated on a five-point Likert scale, ranging from strongly disagree (SD) to strongly agree (SA). The items were summed to create a total score, with appropriate items reverse coded. Cronbach's alpha was 0.863 in our sample.
UNIT SUPPORT (DRRI SECTION F): This measure is from Section F of the DRRI: Unit Support, and includes 12 questions pertaining to relationships with other individuals in the military during deployment. These items were also asked on a five-point Likert scale, ranging from SD to SA and summed for a composite score. Cronbach's alpha was 0.912 in our sample.
COMBAT EXPERIENCES (DRRI SECTION I): Combat Experiences, from section I of the DRRI, includes 15 yes/no questions about combat experiences that occurred during deployment. Responses across all items were summed to create a total score, with higher scores indicating more experiences endorsed. Cronbach's alpha was 0.875 in our sample. This measure will be referred to as the Combat Experiences Scale (CES) throughout the manuscript.
POST-BATTLE EXPERIENCES (DRRI SECTION J): Post-Battle Experiences asks 15 yes/no questions about experiences that occurred after battle. Responses across all items were summed to create a total score, with higher scores indicating more experiences endorsed. Cronbach's alpha was 0.911 in our sample.
Personality
The NEO Five-Factor Inventory (NEO-FFI),29 a shortened version of the NEO Personality Inventory (NEO-PI), was used to measure personality traits. The NEO-FFI asks 60 questions that include the 12 strongest items from each factor on the NEO-PI. This scale is a comprehensive personality inventory based on the Big Five personality trait model.30 The NEO-FFI measures neuroticism, openness to experience, extraversion, conscientiousness, and agreeableness. Respondents are instructed to rate each item on a five-point Likert scale, from SD to SA. Cronbach's alphas in our sample were 0.851 (neuroticism), 0.821 (extraversion), 0.739 (openness), 0.749 (agreeableness), and 0.850 (conscientiousness) within this sample.
Coping
The COPE Questionnaire31 is a 60-item self-report measure of an individual's coping style across 15 different dimensions (e.g., active, denial, substance use). The measure possesses adequate internal consistency (most subscales above 0.60) and test-retest reliability (above 0.40 across 2 samples), and correlates with predicted aspects of personality (e.g., anxiety).31 In our sample, Cronbach's alpha ranged from 0.519 to 0.943 across all 15 subscales.
Self-reported resilience
Resilience was measured using the shortened 10-item version of the Connor-Davidson Resilience Scale (CD-RISC).32 Respondents are instructed to respond to each item on a five-point Likert scale ranging from 0 (not true at all) to 4 (true nearly all the time). Cronbach's alpha in this sample was 0.861.
Data Analytic Plan
Descriptive statistics were conducted using SPSS version 23. Variables were assessed for violations of normality prior to initial analyses and variables with skewness and/or kurtosis > 1 were natural log-transformed and significant outliers (> 3 standard deviation from the mean) were removed. Correlations were run between demographic variables and PSQI global score, COPE subscales and PSQI global score, and additional alcohol variables and PSQI global score to determine which subscales to use in regression analyses, given the modest sample size. Note that military branch was dichotomized as Army (1; most endorsed category) versus other branches (0) for use in all analyses. To examine mean group differences on the PSQI while taking into account demographic covariates (e.g., smoker status, Army), one-way analyses of covariance (ANCOVAs) were conducted across PSQI scores. This was done for the PSQI global score as well as the subscales (see endnote B). Next, five linear regressions were run with PSQI global score as the dependent variable. The five categories of predictor variables, chosen based on the literature, included demographics (as indicated by significant correlations), personality (NEO-FFI; all five scales), coping (COPE; as indicated by significant correlations), resilience (CD-RISC, social support, unit support), and trauma load (LEC self, CES, and post-battle experiences). Significant variables from individual models were then incorporated in a final combined regression model along with group status to determine if these correlates accounted for independent variance beyond that of trauma/ PTSD status.
RESULTS
Sample demographic characteristics are presented in Table 1. The 133 participants who met eligibility criteria based on group assignment were used in subsequent analyses. The group breakdown included 26 control, 69 TE, and 38 PTSD. To determine which variables to use as covariates, correlations were run between these demographic variables and PSQI global score. Smoker status (current or past versus never; Spearman's rho = 0.255, p = 0.004) and Army (versus other branches; Spearman's rho = 0.228, p = 0.010) were the only demographic variables significantly correlated with PSQI global score. Correlations were also conducted with all 15 of the coping subscales to determine which subscales should be included in regression analyses, and two coping subscales were significantly correlated with PSQI global score: denial (log) (R = 0.176, p = 0.046 and substance use (log) (R = 0.317, p < 0.001). We also conducted exploratory correlations on alternate alcohol variables (see endnote C) but only maximum number of drinks per day (with a natural log transformation) was significantly correlated with PSQI global score (R = 0.199, p = 0.025).
Table 1.
Demographic information.

Analyses of Covariance
Table 2 presents group means for PSQI global score and six subscales and ANCOVA results. Smoker status (dummy coded), Army (versus other branches), and maximum number of drinks per day (natural log-transformed) were included as covariates. ANCOVA results revealed a significant effect of PTSD group status for the PSQI global score, as well as all subscales except for sleep efficiency. Follow-up contrasts were conducted to identify specific group differences among significant PSQI subscales. There were significant differences between control and PTSD and TE and PTSD groups across all PSQI variables where contrasts were run, with the exception of sleep duration, which only significantly differed between TE and PTSD groups. There were no signifi-cant differences between control and TE groups on any PSQI measures.
Table 2.
Pittsburgh Quality Sleep Index scores by group status, analyses of covariance.
Regressions
Results of both individual and combined regressions are shown in Table 3. The mean (standard deviation) or n (%) for each independent variable is also presented in this table. Smoker status (current vs. never, std. β = 0.228, p = 0.024) and Army (vs. other branches, std. β = 0.176, p = 0.044) were significantly associated with higher sleep disturbance. For personality, only neuroticism was significantly related to the global sleep score (std. β = 0.409, p < 0.001). For the coping subscales included, only substance use coping (log) (std. β = 0.271, p = 0.003) was significantly associated with higher disturbance. In the resilience regression, DRRI social support (std. β = −0.236, p = 0.021) was inversely associated with sleep disturbances. Finally, none of the trauma load variables were significant. Based on these results, smoker status (current versus never), Army (versus other military branches), neuroticism, substance use coping (log), and DRRI social support were included the combined regression, along with group status (collapsed into no PTSD and PTSD). In this final model, group status significantly predicted higher global sleep scores (std. β = 0.272, p = 0.004). Neuroticism (std. β = 0.246, p = 0.009) and substance use coping (log) (std. β = 0.176, p = 0.034) remained significant in this model. None of the other variables accounted for unique variance in the final model.
Table 3.
Predictors of Pittsburgh Sleep Quality Index global score via linear regression.

DISCUSSION
Overall, this veteran sample experienced disturbed sleep. As hypothesized, the PTSD group reported significantly more disturbed sleep including higher PSQI global scores, as well as worse scores on all PSQI subscales except for sleep duration and efficiency, when compared to both the control and TE groups. The TE group did not differ from control on any sleep measures, which is a novel result. Our findings are consistent with the extant literature suggesting that OEF/OIF veterans, in general, have poor sleep.5,10–12 Although there is a large body of work outlining disturbed sleep and insomnia in veterans, our study contributes uniquely in that it used a three-group design to investigate an issue that has been unclear: Does PTSD, TE, and/or simply being a veteran drive sleep disturbance, particularly in OEF/OIF/OND veterans? Given that disturbed sleep is part of the diagnostic criteria for PTSD9 and that to our knowledge, most studies of sleep and PTSD have not examined this (the majority have used the PTSD Checklist to obtain PTSD symptom scores but do not specifically assess traumatic event exposure5,8,11), it remains an important question to answer and one that we were specifically suited to examine within our sample. Results from our ANCOVAs indicated that the PTSD group differed from both control and TE groups on global sleep disturbances, as well as all PSQI subscales except efficiency and duration.
There are two main conclusions to be drawn from these results. First, all groups of veterans (even non-TE controls) experienced poor sleep, as defined by PSQI global scores > 5.25 Mean (standard deviation) PSQI global scores for the control group were higher than what is reported by normal sleepers (5.27 ± 3.23 versus 2.67 ± 1.70).25 This is striking, given our use of a modified PSQI global score, which did not include the sleep medication item and thus had a smaller possible range. Second, individuals with PTSD experienced worse sleep than the other groups. Note that overall, we had lower mean PSQI global scores (including in the PTSD group), when compared to other OEF/OIF veteran samples.5,11,12 This is likely due to the non-treatment seeking nature of our sample and exclusion criteria, combined with use of a modified PSQI global scale. Note that the sleep medication component has been removed from prior factor analyses of the PSQI in both veteran33 and other populations.34 Babson and colleagues,33 in their sample of veterans with PTSD, found that the sleep medication component had the lowest correlation with PSQI global score (out of all other subscales). Additionally, our finding of no group differences on sleep efficiency is consistent with several prior papers,12,33 supporting the contention that sleep quality, not efficiency or duration, is the important component of disturbed sleep for veterans with PTSD.33
Our second set of findings relate to the identification of correlates of disturbed sleep. Although current smoking (versus never), Army (versus other branches), neuroticism, substance use coping, and DRRI social support were significantly associated with PSQI global scale scores individually, only neuroticism and substance use coping remained significant predictors of sleep when combined and controlled for group status. Note that although approximately 40% of our sample endorsed a mild TBI, mild TBI was not correlated with PSQI global score. The significance of neuroticism (a personality trait characterized by fear, anxiety, moodiness, worry, envy, frustration, jealousy, and loneliness35) as a predictor of disturbed sleep (see Table 3), even after controlling for other significant correlates and group status, is not surprising given literature on the personality trait. Research indicates that sleep and psychiatric disorders that include anxiety as a symptom may share a common diathesis.36 Neuroticism is associated with greater likelihood of psychiatric comorbidities (e.g., depression, anxiety),37 and there is evidence for shared genetic contributions between neuroticism and anxiety disorders.38 Further, several studies indicate that higher neuroticism significantly predicted poor sleep in non-veteran populations,39,40 which supports our results.
In addition to neuroticism, substance use coping remained significantly associated with disturbed sleep in the final model. Using substances to cope is a maladaptive coping method akin to “self medication” and this is particularly common among individuals with PTSD and sleep disturbance (see Vandrey et al.41 for a thorough review of interactions between sleep, PTSD, and substance use disorders). Substance use itself, particularly alcohol use, can have detrimental effects on sleep.42 Despite this, disturbed sleep has been associated with drinking (or using cannabis) to cope in veterans with PTSD.43,44 Given this literature, along with established relationships between substance use disorders themselves and disturbed sleep,45 it is not surprising that our study found an association between substance use coping and sleep. However, it is interesting that this association remained even beyond the effects of PTSD, suggesting that substance use coping contributes uniquely to the variance in disturbed sleep across all veterans. As recommended by Vandrey and colleagues,41 it may be useful to intervene on disturbed sleep early, after it is determined that an individual is utilizing substances use to cope, to both reduce the likelihood of the development of substance use disorders and potentially improve PTSD symptoms, if present. It is important to note that we did not find that risky drinking itself was independently associated with sleep disturbance in our sample, although veterans with alcohol dependence were screened out as part of study exclusion criteria. The only additional alcohol variable that was correlated with sleep in our sample was maximum number of drinks per day, which did not retain significance in regression analyses.
There are several important limitations to consider in the context of this study. First, due to the preliminary nature of the data, our sample size was small. Further, the exclusion criteria limited the sample to veterans between 21 and 40 y old, no history of moderate or severe TBI, and without co-morbid depression or alcohol dependence, which may affect generalizability across all OEF/OIF/OND veterans. Although we also excluded for abuse/dependence on illicit substances other than cannabis, we do not have detailed information on the specific substances used. Additionally, given that the sample was primarily composed of Caucasian males, our findings may not extend to female veterans and those of other races/ethnicities. It is also crucial to emphasize that this is a cross-sectional study design and we cannot draw causal conclusions from the results. However, the study did have many strengths. First, the sample was non-treatment seeking and recruited from a community with a high veteran population, encompassing several settings where veterans are known to congregate. Second, our use of the three-group design allowed us to separate the effects of trauma exposure from PTSD on sleep. Third, some of the exclusion criteria also represent strengths, such as screening out individuals with depression, alcohol dependence, and/or illicit substance abuse or dependence (excluding cannabis), given these disorders are highly comorbid with PTSD.46 This allowed us to examine the unique contribution of PTSD, unconfounded by symptoms of depression or substance dependence. Fourth, we used the CAPS,20 the gold standard clinical interview, for determination of group status and PTSD diagnosis, as well as other well-validated measures for the determination of psychiatric comorbidities (MINI19) and sleep (PSQI25). Finally, we had available data on a variety of risk and resilience factors, such as measures from the DRRI and COPE, which allowed us to examine additional correlates of disturbed sleep in OEF/OIF/ OND veterans, beyond demographics, psychopathology, and those used by Pietrzak et al.5
Although preliminary, these results have important clinical implications. Our results confirm that veterans, in general, are at high risk for poor sleep,10,11 and are novel in that we show this is true regardless of trauma exposure history and PTSD status. As such, all veterans should be educated about proper sleep hygiene, and this should be integrated into overall care. The Veterans Health Administration has already begun to enhance collaborative care models where primary care providers, mental health specialists, and sleep specialists work together to identify and treat sleep disorders, as described by Edinger and colleagues.47 It would be useful to further test and expand this and other collaborative care models throughout the Veterans Health Administration and community agencies where veterans are treated, as many veterans seek healthcare services through a number of community-based healthcare agencies. Further, higher levels of disturbed sleep in veterans with PTSD indicate that this represents a unique subset of the veteran population who may benefit from increased clinical and programmatic focus on sleep interventions. Cognitive behavioral therapy targeting sleep has shown promise in treating sleep disturbances in the context of PTSD, with a recent meta-analysis of eleven randomized control trials demonstrating a decrease in PTSD, depressive, and sleep symptoms for individuals given sleep-specific cognitive behavioral therapy.48
Given the ubiquitous nature of disturbed sleep among OEF/ OIF veterans, addressing other contributing factors is important. This study is one of the first to examine correlates of disturbed sleep, other than demographics and specific psychopathology, in OEF/OIF/OND veterans.5 Further, we were able to show that several of these correlates were important predictors even after taking into account PTSD status. We have identified neuroticism, which is related to psychiatric disorders,37 as a risk factor for disturbed sleep in veterans, further supporting the importance of addressing comorbid psychopathology in this population. The finding of substance use coping as a significant predictor also represents an area of potential intervention. Addressing maladaptive coping strategies in veterans, such as using drugs and alcohol to cope, may be a way to improve disturbed sleep,41 as current clinical screening protocols mostly focus on detecting substance use disorders. It is important to identify and address risk factors for worse sleep in veterans, given evidence that in addition to being a commonly reported symptom,8 sleep has been shown to predict future psychopathology.14,15 Thus, targeting sleep in veterans can improve current symptomatology (for those who have it), in addition to helping prevent the development of future psychiatric disorders. Additional research into risk and protective factors for sleep in OEF/OIF/OND veterans is warranted to better treat this population.
ENDNOTES
A: Note that a DSM-IV definition of PTSD was used, since the study began prior to publication of DSM-5. However, there is information available that corresponds to DSM-5 criteria.
B: Note that we chose to exclude the Sleep Medication sub-scale, as use of medication was part of the exclusion criteria for our study.
C: i.e., alcohol abuse as assessed by the MINI, TLFB measures: quantity/frequency of consumption, total number of binge days, maximum number of drinks per day.
DISCLOSURE STATEMENT
The Virginia Commonwealth University IRB approved all study procedures. This work was supported in part by NIH grants R01 AA020179 and K02 AA023239 to Ananda B. Amstadter. Mackenzie J. Lind is supported by NIH grant T32 MH020030. Scott McDonald has received grant and/or research support from VA RR&D (1Ik2RX000703-01). The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- ANCOVA
analysis of covariance
- CAPS
Clinician-Administered PTSD Scale
- CD-RISC
Connor-Davidson Resilience Scale
- CES
Combat Experiences Scale
- DRRI
Deployment Risk and Resiliency Inventory
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- LEC
Life Events Checklist
- MINI
Mini-International Neuropsychiatric Interview
- NEO-FFI
NEO Five-Factor Inventory
- NEO-PI
NEO Personality Inventory
- OEF
Operation Enduring Freedom
- OIF
Operation Iraqi Freedom
- OND
Operation New Dawn
- PSQI
Pittsburgh Sleep Quality Index
- PTSD
posttraumatic stress disorder
- SA
strongly agree
- SD
strongly disagree
- TBI
traumatic brain injury
- TE
trauma exposure
- TLFB
timeline follow back
REFERENCES
- 1.Wright KM, Huffman AH, Adler AB, Castro CA. Psychological screening program overview. Mil Med. 2002;167(10):853–861. [PubMed] [Google Scholar]
- 2.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 3.Schnurr PP, Lunney CA, Bovin MJ, Marx BP. Posttraumatic stress disorder and quality of life: extension of findings to veterans of the wars in Iraq and Afghanistan. Clin Psychol Rev. 2009;29(8):727–735. doi: 10.1016/j.cpr.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Fulton JJ, Calhoun PS, Wagner HR, et al. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/ OIF) Veterans: a meta-analysis. J Anxiety Disord. 2015;31:98–107. doi: 10.1016/j.janxdis.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Pietrzak RH, Morgan CA, 3rd, Southwick SM. Sleep quality in treatment-seeking veterans of Operations Enduring Freedom and Iraqi Freedom: the role of cognitive coping strategies and unit cohesion. J Psychosom Res. 2010;69(5):441–448. doi: 10.1016/j.jpsychores.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24(1):1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gellis LA, Gehrman PR, Mavandadi S, Oslin DW. Predictors of sleep disturbances in Operation Iraqi Freedom/Operation Enduring Freedom veterans reporting a trauma. Mil Med. 2010;175(8):567–573. doi: 10.7205/milmed-d-09-00123. [DOI] [PubMed] [Google Scholar]
- 8.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175(10):759–762. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 10.Bramoweth AD, Germain A. Deployment-related insomnia in military personnel and veterans. Curr Psychiatry Rep. 2013;15(10):401. doi: 10.1007/s11920-013-0401-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Plumb TR, Peachey JT, Zelman DC. Sleep disturbance is common among servicemembers and veterans of Operations Enduring Freedom and Iraqi Freedom. Psychol Serv. 2014;11(2):209–219. doi: 10.1037/a0034958. [DOI] [PubMed] [Google Scholar]
- 12.Lewis V, Creamer M, Failla S. Is poor sleep in veterans a function of post-traumatic stress disorder? Mil Med. 2009;174(9):948–951. doi: 10.7205/milmed-d-04-0208. [DOI] [PubMed] [Google Scholar]
- 13.Morin CM, Jarrin DC. Epidemiology of insomnia. Sleep Med Clin. 2013;8(3):281–297. doi: 10.1016/j.jsmc.2022.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67(12):1240–1258. doi: 10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]
- 15.Pigeon WR, Campbell CE, Possemato K, Ouimette P. Longitudinal relationships of insomnia, nightmares, and PTSD severity in recent combat veterans. J Psychosom Res. 2013;75(6):546–550. doi: 10.1016/j.jpsychores.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Pace-Schott EF, Germain A, Milad MR. Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. Biol Mood Anxiety Disord. 2015;5:3. doi: 10.1186/s13587-015-0018-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatry. 2002;159(10):1696–1701. doi: 10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- 18.Mellman TA, Pigeon WR, Nowell PD, Nolan B. Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma. J Trauma Stress. 2007;20(5):893–901. doi: 10.1002/jts.20246. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- 20.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM. Clinician-Administered PTSD Scale for DSM-IV. Boston, MA: National Center for PTSD; 1998. [DOI] [PubMed] [Google Scholar]
- 21.Weathers FW, Keane TM, Davison JRT. Clinican-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. 4th ed. Washington, DC: American Psychiatric Association; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 23.Drinking Levels Defined. National Institute on Alcohol Abuse and Alcoholism Web stie. [Accessed August 7, 2016]. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
- 24.Sobell LC, Sobell MB. Timeline followback: a technique for assessing self-reported ethanol consumption. In: Allen J, Litten RZ, editors. Measuring Alcohol Consumption: Psychological and Biological Methods. Totowa, NJ: Humans Press; 1992. pp. 41–72. [Google Scholar]
- 25.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 26.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 27.King DW, King LA, Vogt DS. Manual for the Deployment Risk and Resilience Inventory (DRRI): A Collection of Measures for Studying Deployment-Related Experiences in Military Veterans. Boston, MA: National Center for PTSD; 2003. [Google Scholar]
- 28.King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: a collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychol. 2006;18(2):89–120. [Google Scholar]
- 29.Costa PT, McCrae RR. Odessa, FL: Psychological Assessment Services; 1989. The NEO-PI/NEO-FFI manual supplement. [Google Scholar]
- 30.Zillig LMP, Hemenover SH, Dienstbier RA. What do we assess when we assess a Big 5 trait? A content analysis of the affective, behavioral, and cognitive processes represented in Big 5 personality inventories. Pers Soc Psychol Bull. 2002;28(6):847–858. [Google Scholar]
- 31.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 32.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 33.Babson KA, Blonigen DM, Boden MT, Drescher KD, Bonn-Miller MO. Sleep quality among U.S. military veterans with PTSD: a factor analysis and structural model of symptoms. J Trauma Stress. 2012;25(6):665–674. doi: 10.1002/jts.21757. [DOI] [PubMed] [Google Scholar]
- 34.Nicassio PM, Ormseth SR, Custodio MK, Olmstead R, Weisman MH, Irwin MR. Confirmatory factor analysis of the Pittsburgh Sleep Quality Index in rheumatoid arthritis patients. Behav Sleep Med. 2014;12:1–12. doi: 10.1080/15402002.2012.720315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCrae RR, Costa PT. The five-factor theory of personality. In: John OP, Robins RW, Pervin LA, editors. The Five-Factor Theory of Personality. New York, NY: Guilford; 2008. pp. 159–181. [Google Scholar]
- 36.Boland EM, Ross RJ. Recent advances in the study of sleep in the anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder. Psychiatr Clin North Am. 2015;38(4):761–776. doi: 10.1016/j.psc.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 37.Malouff JM, Thorsteinsson EB, Schutte NS. The relationship between the five-factor model of personality and symptoms of clinical disorders: a meta-analysis. J Psychopathol Behav Assess. 2005;27(2):101–114. [Google Scholar]
- 38.Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. Am J Psychiatry. 2006;163(5):857–864. doi: 10.1176/ajp.2006.163.5.857. 5. [DOI] [PubMed] [Google Scholar]
- 39.Duggan KA, Friedman HS, McDevitt EA, Mednick SC. Personality and healthy sleep: the importance of conscientiousness and neuroticism. PLoS One. 2014;9(3):e90628. doi: 10.1371/journal.pone.0090628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hintsanen M, Puttonen S, Smith K, et al. Five-factor personality traits and sleep: evidence from two population-based cohort studies. Health Psychol. 2014;33(10):1214–1223. doi: 10.1037/hea0000105. [DOI] [PubMed] [Google Scholar]
- 41.Vandrey R, Babson KA, Herrmann ES, Bonn-Miller MO. Interactions between disordered sleep, post-traumatic stress disorder, and substance use disorders. Int Rev Psychiatry. 2014;26(2):237–247. doi: 10.3109/09540261.2014.901300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roehrs TA, Roth T. Sleep disturbance in substance use disorders. Psychiatr Clin North Am. 2015;38(4):793–803. doi: 10.1016/j.psc.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonn-Miller MO, Babson KA, Vujanovic AA, Feldner MT. Sleep problems and PTSD symptoms interact to predict marijuana use coping motives: a preliminary investigation. J Dual Diagn. 2010;6(2):111–122. [Google Scholar]
- 44.Nishith P, Resick PA, Mueser KT. Sleep difficulties and alcohol use motives in female rape victims with posttraumatic stress disorder. J Trauma Stress. 2001;14(3):469–479. doi: 10.1023/A:1011152405048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 47.Edinger JD, Grubber J, Ulmer C, Zervakis J, Olsen M. A collaborative paradigm for improving management of sleep disorders in primary care: a randomized clinical trial. Sleep. 2016;39(1):237–247. doi: 10.5665/sleep.5356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ho FY, Chan CS, Tang KN. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2016;43:90–102. doi: 10.1016/j.cpr.2015.09.005. [DOI] [PubMed] [Google Scholar]


