Abstract
Study Objectives:
Although important to recovery, sleeping in the hospital is difficult because of disruptions. Understanding how patients, hospital physicians, and nurses perceive sleep disruptions and identifying which disruptions are associated with objective sleep loss can help target improvement initiatives.
Methods:
Patients and hospital staff completed the Potential Hospital Sleep Disruptions and Noises Questionnaire (PHSDNQ). Cutoff points were defined based on means, and responses were dichotomized. Perceived percent disrupted for each item was calculated, and responses were compared across groups using chi-square tests. Objective sleep time of patients was measured using wrist actigraphy. The association between patient-reported disruptions and objective sleep time was assessed using a multivariable linear regression model controlling for subject random effects.
Results:
Twenty-eight physicians (78%), 37 nurses (88%), and 166 of their patients completed the PHSDNQ. Patients, physicians, and nurses agreed that pain, vital signs and tests were the top three disrupters to patient sleep. Significant differences among the groups' perceptions existed for alarms [24% (patients) vs. 46% (physicians) vs. 27% (nurses), p < 0.040], room temperature (15% vs. 0% vs. 5%, p < 0.031) and anxiety (18% vs. 21% vs. 38%, p < 0.031). Using survey and actigraphy data from 645 nights and 379 patients, the presence of pain was the only disruption associated with lower objective sleep duration (minutes) [−38.1 (95% confidence interval −63.2, −12.9) p < 0.003].
Conclusion:
Hospital staff and patients agreed that pain, vital signs and tests were top sleep disrupters. However, pain was associated with the greatest objective sleep loss, highlighting the need for proactive screening and management of patient pain to improve sleep in hospitals.
Citation:
Grossman MN, Anderson SL, Worku A, Marsack W, Desai N, Tuvilleja A, Ramos J, Fancisco MA, Lafond C, Balachandran JS, Mokhlesi B, Farnan JM, Meltzer DO, Arora VM. Awakenings? Patient and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. J Clin Sleep Med. 2017;13(2):301–306.
Keywords: disruptions, noise, pain, quality improvement, sleep
INTRODUCTION
Sleep is imperative to biological function and is of critical importance in the recovery process from acute illness.1 Despite the importance of sleep, hospitalized patients are frequently disrupted during the night.2,3 Prior work has demonstrated that inpatient sleep loss is associated with higher morning blood pressure and an increased recovery time.4,5
In addition to the pathophysiological effects of sleep loss, sleep disruptions negatively affect the patient experience. In fact, reducing noise was ranked the top priority of action for improving the patient experience in a large survey of hospital executives.6 Furthermore, quietness of the hospital environment is a patient-reported Hospital Consumer Assessment of Healthcare Providers and Systems measure.7
BRIEF SUMMARY
Current Knowledge/Study Rationale: This study, to the best of the authors' knowledge, is the first of its kind to examine patients' and providers' perceptions of in-hospital sleep disruptions and the effect of patient-reported sleep disruptions on objective sleep duration. Previous studies focused on noise as the primary disrupter to patient sleep, whereas this study analyzed the effect of a broader spectrum of sleep disruptions on general medicine wards.
Study Impact: This study shows that providers generally agree with patients regarding the factors that are perceived to be most disruptive to patient sleep in the hospital. Further, pain represents the disruption that is most significantly linked to objective sleep loss in the hospital setting, indicating the need for better pain control to improve the inpatient sleeping environment.
Previous studies on hospital environment and sleep have focused on noise as the primary disrupter to inpatient sleep.2,8 For example, Buxton et al. performed a laboratory-based study to assess the relationship between hospital noise and sleep physiology and found that noise caused a significant increase in heart rate during sleep.9 In addition, prior work by our group measured noise and sleep duration in hospitalized adult medical patients and found that more than 42% of patients reported noise disruptions during sleep, and the most common source of noise disruption was staff conversation. Although noise is a common and important cause of sleep disruptions, other contributing factors such as the effect of symptoms (e.g., pain), medical interventions (e.g., laboratory draws), and environmental factors (e.g., bed comfort) on inpatient sleep loss must also be considered.
Prior studies on in-hospital sleep disruptions examining the effect of environmental factors and clinical care activities have primarily focused on critical care units.5,10 The results, however, cannot be generalized to a broader hospital population because there are more patient factors contributing to sleep disruptions in critical care units compared to general medical wards. Furthermore, studies regarding the effect of medical symptoms such as pain on in-hospital sleep have generally been restricted to very specific subsets of patients (e.g., postoperative orthopedic patients).11 As such, there have been no systematic investigations to identify the potential contributing factors of sleep loss in the general medicine setting.
In order to improve inpatient sleep among hospitalized general medicine patients, the predominant causes of sleep loss must be identified. Once identified, the primary patient reported in-hospital sleep disruptions can be associated with objective sleep duration to target quality improvement interventions. Establishing agreement among patients, nurses, and physicians allows for a patient-centered approach for reducing disruptions to improve sleep hygiene and the patient experience. Concordance is important because many sleep disruptions are potentially actionable and could be prevented by health professionals.
The aims of this study were twofold. One aim was to assess the differences between nurses, physicians, and patients' perceptions of in-hospital sleep disruptions. It was hypothesized that in comparison with hospitalists, nurses would be more likely to agree with patients that noise is the top disrupter of patient sleep. The second aim was to assess the association between patient reported in-hospital sleep disruptions and objective sleep duration and efficiency. It was hypothesized that patients who identified noise as the most disruptive factor associated with their in-hospital sleep would have the lowest objective sleep duration.
METHODS
Study Design
A single institution, survey-based study at the University of Chicago Medicine was conducted to compare the perceptions of in-hospital sleep disruptions among patients, physicians, and nurses. In addition, the association between patient-reported in-hospital sleep disruptions and objective sleep duration and efficiency was assessed using data from an ongoing prospective study of hospital patients at the University of Chicago Medicine. This study was approved by the University of Chicago Institutional Review Board (12-1766; 16685B).
Data Collection
Patient and Hospital Staff Perceptions of Sleep Disruptions
To determine the most disruptive factors to patients' sleep, patients were surveyed regarding their previous night's sleep in the hospital. The study population included patients on two general medicine and hematology/oncology units at the University of Chicago Medicine. All English-speaking, awake, and cognitively intact patients on these units were included in the study. No protected health information was collected from the subjects. From June 2015 to August 2015 (9 w), patients were approached every other day (Monday-Friday) and asked to complete a Patient Sleep Assessment. The assessment included a Potential Hospital Sleep Disruptions and Noises Questionnaire (PHSDNQ), a 10-item survey that asks patients the extent to which each item disrupted their sleep the previous night on a scale of 1 to 5, 1 indicating that the item was not disruptive at all to 5 being extremely disruptive. The 10 items include pain, vital signs, tests, noise (all sources), medications, alarms, bed comfort, anxiety, room temperature, and staff conversation. This survey was developed by our group as a modification of a previous tool developed by Freedman et al.12 for studies in critical care units. The initial questionnaire asked patients to rate how disruptive different activities (e.g., light, vital signs, administration of medications) and noises (e.g. heart monitor alarm, ventilator, television) were to their sleep on a 10-point scale.12–14
To determine the factors that providers perceive to be most disruptive to inpatient sleep, floor nurses, nursing leaders, and hospitalists on the same two units were invited to participate in a similar survey. The survey was introduced to nurses at morning shift changes and daily huddles with the help of nursing champions (WM, AT, JR). Surveys and collection boxes were placed in nursing workrooms. Hospitalists were asked to complete the survey at monthly section meetings and committee meetings (AW). All provider participants were asked to check their name on a roster upon survey completion in order to track the response rate while maintaining anonymity.
All paper survey data were entered and stored on the REDCap Database Version 6.5.0 (Vanderbilt University, Nashville, TN, 2015).
Disruptions and Objective Sleep Duration
Data were collected from March 2010 to July 2015. The study population was patients aged 50 y or older hospitalized on the University of Chicago general medicine and hematology/oncology services. Eligible patients were community-dwelling, ambulatory adults. Patients were excluded if they were transferred from an intensive care unit, were cognitively impaired (score less than 17 on a telephone version of the Mini-Mental State Examination or a passing score on the Short Portable Mental Status Questionnaire), had a documented sleep disorder, were on bed rest, were readmitted within 2 w or had been hospitalized for more than 72 h prior to eligibility screening.15,16 These exclusion criteria were selected to ensure a study population for which actigraphy would be easy to interpret, as patients wore an Actiwatch (Actiwatch 2; Respironics Inc., Murrysville, PA), a validated approach for recording sleep duration. A protocol similar to that used by Shear et al. was followed.17
On the day of enrollment, the Pittsburgh Sleep Quality Index was administered to determine baseline sleep quality and hygiene and the Epworth Sleepiness Scale was used to characterize sleepiness in routine situations.18,19 On subsequent days of admission, the Daily Sleep Assessment was administered, which included the PHSDNQ to identify the factors that disrupted patients' sleep during the previous night. All paper survey data were entered and stored on the REDCap Database Version 6.5.0 (Vanderbilt University, 2015).
Data Analysis
Patient and Hospital Staff Perceptions of Sleep Disruptions
The distribution of patients' PHSDNQ responses was analyzed, and the mean response was calculated. The integer closest to the mean was defined as the cutoff point, and a patient “report of sleep disruption” was defined as 3 or higher. This was necessary given the non-normal distribution of the data and allowed for analysis via rank order. Using the dichotomized disruption data, the percentage of patients disrupted by each item was calculated. The disruptions were rank-ordered from most disruptive to least disruptive.
The distributions of providers' responses to the perceived in-hospital sleep disruption survey were also analyzed. Based on the mean of the responses, a cutoff point was defined, and a provider “report of sleep disruption” was defined as a 5. The perceived percent disrupted for each item was calculated for nurses and hospitalists. Responses across groups were compared using chi-square tests with statistical significance defined as p < 0.05.
Stata/SE Version 12 (StataCorp LP, 2011, College Station, TX) was used for all statistical analysis.
Disruptions and Objective Sleep Duration
Using the dichotomized disruption data, the percentage of patients disrupted by each item was calculated. The top five most disruptive items were identified.
Actiwatch data were downloaded to determine sleep duration and efficiency. Analysis using Actiware-Sleep 3.4 determined sleep time and efficiency. Sleep time was defined as total minutes of nighttime sleep, and sleep efficiency was defined as [100 × (minute of actual sleep / sleep onset – offset)]. Sleep onset was the time the patient fell asleep and sleep offset was the time the patient woke up, both of which were self-reported.
Five different multivariable linear regression models, controlling for subject random effects, were performed to examine the association between the top five patient-reported sleep disruptions and objective sleep duration in the hospital. All models were adjusted for other covariates that might affect sleep such as age, sex, race, severity of illness (Charlson Comorbidity Index), length of hospital stay, obstructive sleep apnea risk (Berlin questionnaire) and body mass index (overweight and obese). Identical models were performed to analyze the association between the top five patient-reported sleep disruptions and sleep efficiency.
For those disruptions that were associated with significant objective sleep loss in the individual models, a combined multivariable linear regression model controlling for subject and random effects was performed to determine which variable most significantly contributed to the results. This model was also controlled for age, sex, race, obstructive sleep apnea risk, and body mass index (overweight and obese).
RESULTS
Patient and Hospital Staff Perceptions of Sleep Disruptions
Patient results are based on data from the PHSDNQ. The questionnaire was administered from June 2015 to August 2015. During that time, 166 patient surveys were collected (Table 1).
Table 1.
Participant characteristics.
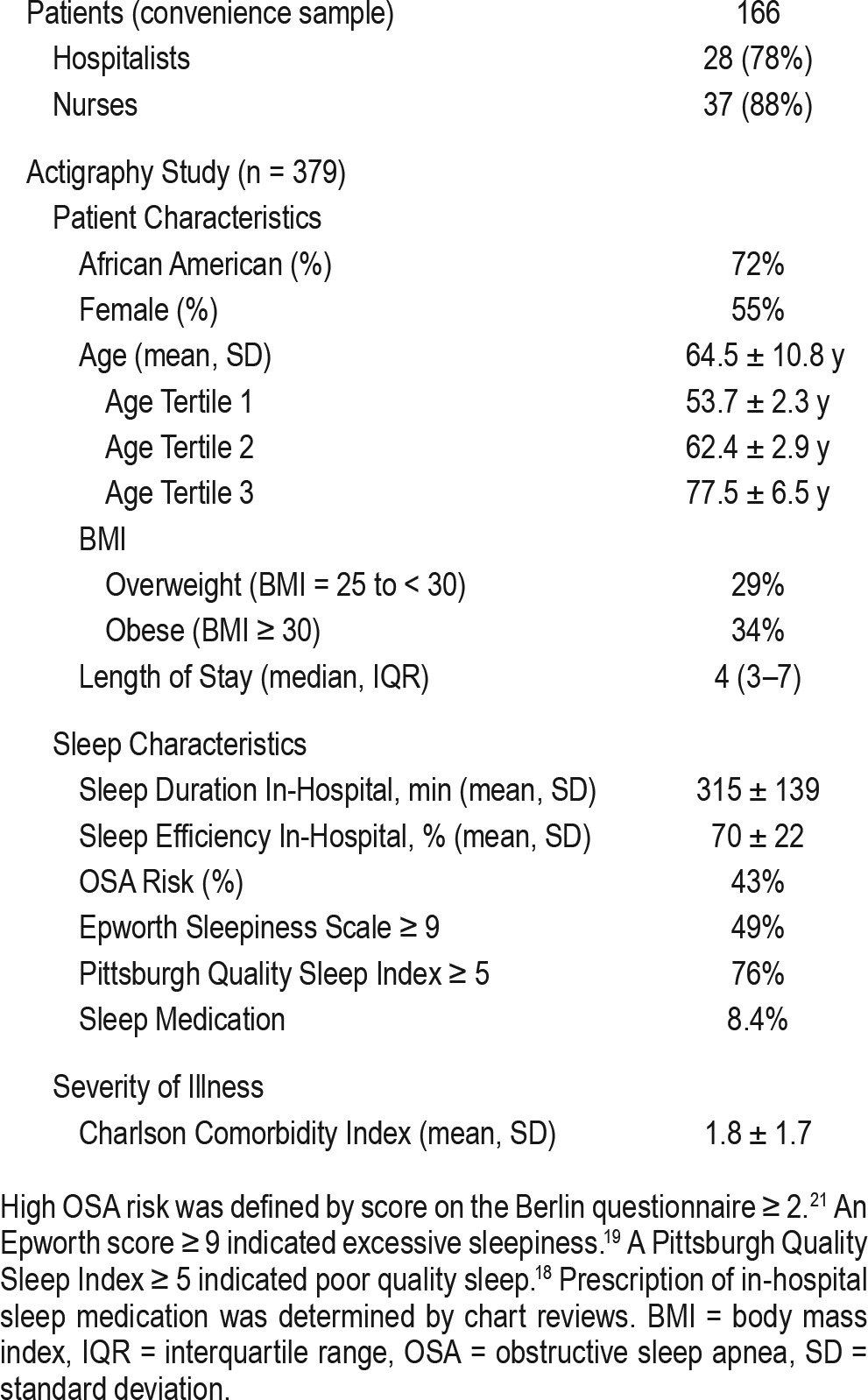
Dichotomized subjective survey data of patients were rank ordered from the most disruptive factor to the least disruptive factor (Figure 1). Patients reported that pain (46%), vital signs (39%), tests (34%), noise (all sources) (27%), and medications (25%) were the five most disruptive factors to their in-hospital sleep. There were subtle differences among patients' perceptions of sleep disruptions on the two general medicine units that were studied. However, pain, vital signs, and tests were the top three patient-reported disruptions on both units.
Figure 1. Patient-reported in-hospital sleep disruptions.
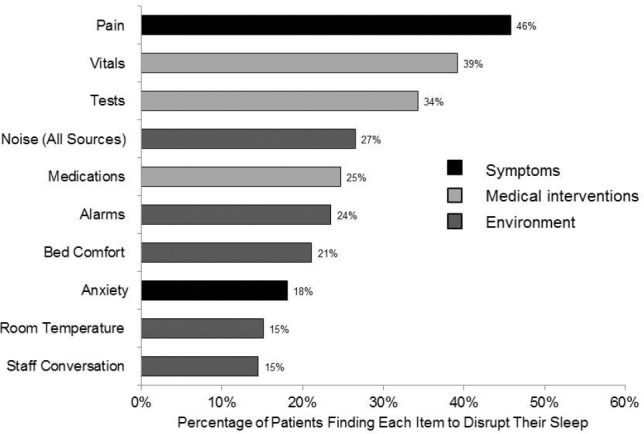
Using the dichotomized disruption data, the proportion of patients disrupted by each item was calculated. The disruptions were placed in rank-order from most disruptive to least disruptive. (n = 166).
During the same time period, 28 hospitalists (78% response rate) and 37 nurses (88% response rate) completed a similar survey. Perceived rank order of the disruptions was compared across the three groups. Although patients, hospitalists, and nurses agreed that pain, vital signs, and tests were among the top three disruptive factors to patient sleep, several discrepancies among the groups were noted. For example, hospitalists reported alarms to be a top disruption, whereas patients and nurses ranked alarms to be the sixth and third most disruptive, respectively. Further, nurses ranked noise (all sources) to be a top disrupter, whereas patients and hospitalists both perceived noise to be the fourth most disruptive factor to in-hospital sleep. Significant levels of disagreement among the groups were identified for three disruptive factors: alarms [21% (patients) vs. 46% (hospitalists) vs. 27% (nurses), p = 0.019], room temperature (16% vs. 0% vs. 5%, p = 0.027), and anxiety (19% vs. 21% vs. 38%, p = 0.047) (Figure 2).
Figure 2. Comparing perceptions of patients, hospitalists, and nurses.
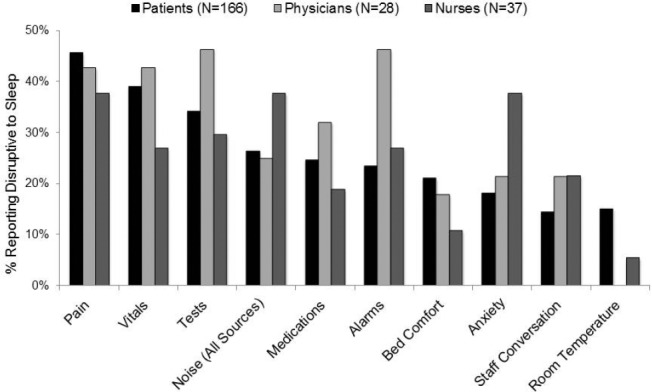
Dichotomized survey data of physicians and nurses were compared to patient responses using chi-square tests. Significant levels of disagreement among the groups were identified for three disruptive factors: alarms [24% (patients) vs. 46% (physicians) vs. 27% (nurses), p = 0.040], and anxiety (18% vs. 21% vs. 38%, p = 0.031) and room temperature (15% vs. 0% vs. 5%, p = 0.031).
Disruptions and Objective Sleep Duration
From March 2010 to July 2015, 574 eligible individuals consented to the actigraphy study. The majority of the patients were African American (74%) and female (56%). The mean age was 64.5 y ± 10.76 y. Median length of stay was 4 days (interquartile range 3–7). Average sleep in the hospital was 315 ± 139 min (Table 1).
Dichotomized patient-reported sleep disruptions from the PHSDNQ were placed in rank order. The top five disruptive factors were identified (the same as in aim 1 with a slightly different order) as tests (46%), vital signs (44%), pain (37%), medications (35%), and noise (all sources) (29%).
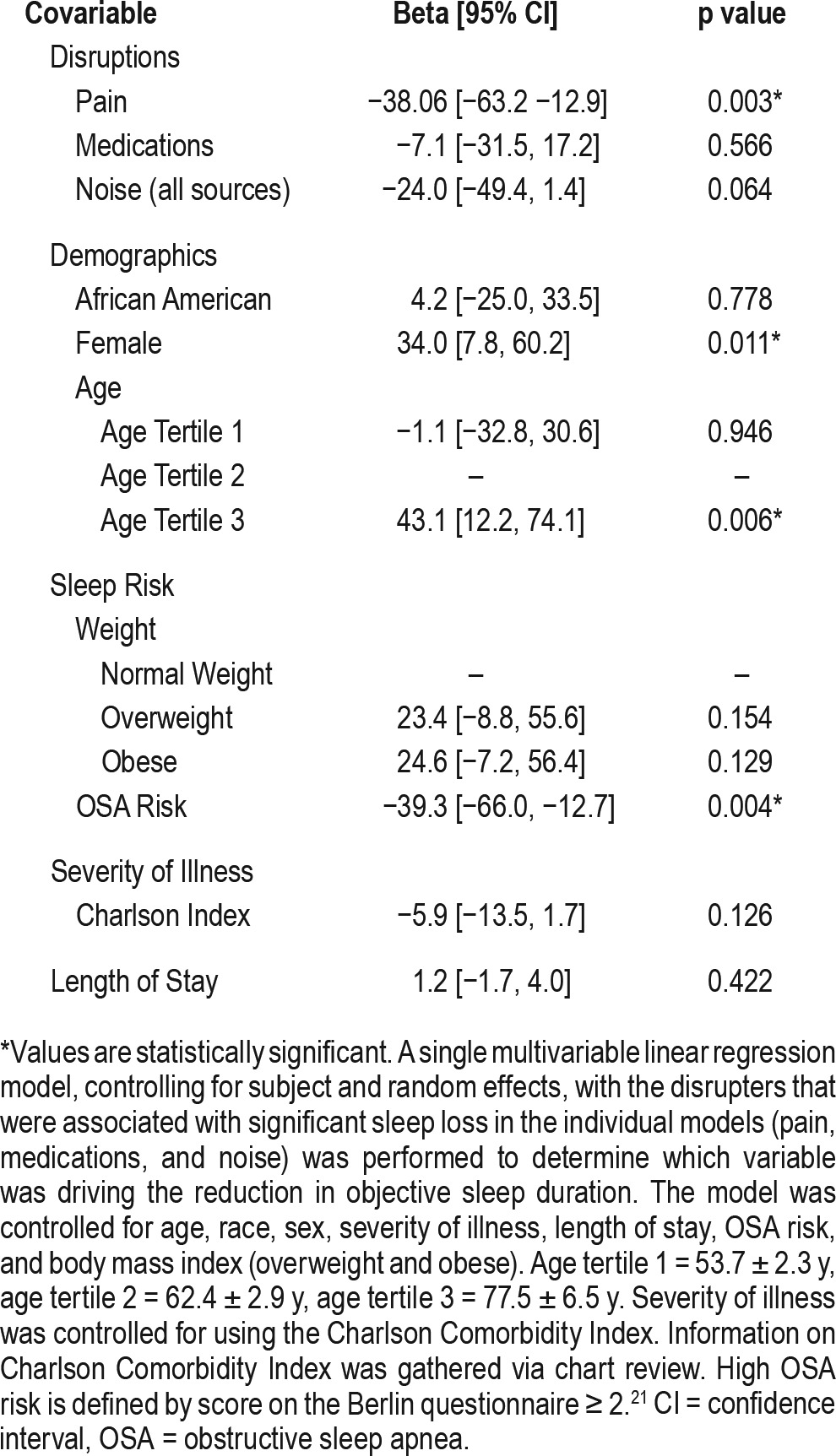
In multivariable regression models testing each disruption's association with objective sleep duration, sleep duration (in minutes) was significantly less for patients who reported being disrupted by pain [−43.4 (95% confidence interval [CI] −66.7, −20.1) p < 0.001], medications [−23.1 (95% CI −45.9, −0.34) p = 0.047], and noise (all sources) [−33.7 (95% CI −58.1, −9.3) p = 0.007). There was no significant difference in sleep du -ration among patients who reported being disrupted by tests [−19.9 (95% CI −41.6, 1.9) p = 0.073] and vital signs [−1.8 (95% −23.1, 19.6) p = 0.870]. In the combined model testing the three disrupters found to be significantly associated with sleep loss, pain was again the disrupter that led to the most statistically significant objective sleep loss [−38.2 (95% −62.7, −13.7) p < 0.002] (Table 2).
Table 2.
Regression model for patient reported sleep disruptions and sleep time (n = 645 nights from 379 subjects).
In multivariable regression models testing each disruption's association with sleep efficiency (percent), none of the disrupters significantly reduced sleep efficiency. Although approaching statistical significance, it is worth noting that pain [−3.4 (−7.0, 0.10) p = 0.057] was not associated with sleep inefficiency. A combined model was not tested because of lack of statistical significance.
DISCUSSION
This study, to the best of the authors' knowledge, is the first of its kind to examine patients' and providers' perceptions of in-hospital sleep disruptions and the effect of patient-reported sleep disruptions on objective sleep duration. Unlike previous studies that focused on noise as the primary disrupter to patient sleep, this study analyzed the effect of a broader spectrum of sleep disruptions on general medicine wards. As hypothesized, nurses were more likely to agree with patients and perceive medical symptoms and environmental factors to be the most disruptive factors to in-hospital sleep, whereas hospitalists indicated that they perceived medical interventions (e.g., tests) to most significantly disrupt patient sleep. Contrary to our second hypothesis, patients who reported being disrupted by pain, and not noise, experienced the most significant sleep loss.
When comparing groups, providers generally agreed with patients' assessment of the top five disrupters to their sleep. That being said, physicians were more likely to overestimate the effect of a disruptive factor whereas nurses tended to underestimate its effect on patients' ability to sleep. There were significant differences among the three groups in regard to the perceived effect of alarms, room temperature, and anxiety. These differences could be explained by a variety of reasons. In terms of alarms, hospitalists were much more likely than patients and nurses to report this factor to be disruptive to patient sleep. It may be that hospitalists are more sensitized to the presence of alarm fatigue due to recent reports.15 Nurses were more likely than doctors to agree with patients on the effect of room temperature. This could be because nurses spend more time in patient rooms during normal sleeping hours and therefore experience the room temperature more often. Finally, nurses were more likely to overestimate the effect of anxiety on patients' ability to sleep, whereas hospitalists' responses were more similar to patients. This could indicate that nurses are sensitized to anxiety and its association with sleeping difficulty.
When analyzing the association between patient-reported disruptions and objective sleep duration, pain was one of the most commonly reported disruptions and also led to the highest reduction in sleep duration. This relationship might be expected given that pain, unlike intermittent disruptions such as medical interventions, is likely to persist throughout the night. This idea is supported by the finding that even though patients reported vital signs and tests to be top disruptive factors to their sleep, their sleep was not significantly decreased. The importance of pain's influence on sleep time is concordant with the findings of Miller et al.11; however, that study was confined to patients who had undergone a joint replacement. Prior work by Whelan et al.20 at our institution has shown that pain is often poorly controlled among general medicine patients, and our work further demonstrates the need for better pain management considering the importance of sufficient sleep in recovery from acute illness.
There are several limitations of this study. First, this is a single-institution study on general medicine wards at an academic medical center. This limits the ability to generalize the findings to patients at other hospitals. Second, patients and hospital staff completed the perceived sleep disruption survey with slightly different aims in mind. Patients were focusing on what disrupted their previous night's sleep, whereas hospitalists and nurses were answering the survey based on their perceptions of global disruptions. Third, two separate patient populations are represented in the study. The data from the perception of the sleep disruptions survey were gathered via a convenience sample. As such, there were no exclusion criteria for participating patients. The actigraphy data span a 5-y period and are therefore not necessarily representative of the current state. Further, due to the inclusion and exclusion criteria of the actigraphy study, the data represent a very specific group of patients. In general, these are older, community-dwelling patients who were admitted from home. As such, despite being older, these patients may be healthier than those patients in the convenience sample study, because patients were excluded if they had been transferred from an intensive care unit, nursing home, etc. Further, these patients may be less conditioned to alarms and other hospital disruptions than the first group. Finally, the actigraphy results were not validated against the gold standard of polysomnography. However, measures were put in place to ensure that sleep time was accurately calculated. The sleep interval for each patient was based on self-reported sleep onset at night and awakening in the morning, which was taken from the Karolinska Sleep Log. This helped to establish concurrent validity, as the actigraphy data correlate with patients' Karolinska scores. Further, discriminant validity has been established because it has been shown that actigraphy can distinguish noisy from non-noisy hospital rooms.2
This study has important implications for hospital quality improvement interventions addressing sleep. To improve the in-hospital sleep environment and reduce sleep disruptions, it is important to ensure that patients and providers are in agreement regarding the most disruptive factors to patient sleep. Clinicians generally agreed with patients regarding the main sources of disruptions: pain, vital signs, tests, medications and noise (all sources). For areas with discrepancies, such as alarms, more education of providers is warranted. Perhaps most importantly, pain was associated with the greatest objective sleep loss in patients, highlighting the importance for better pain control among general medicine patients. Quality improvement initiatives targeting factors that are agreed upon and lead to objectively poor sleep are recommended because they are likely to be more successful.
DISCLOSURE STATEMENT
Funding from the National Institute on Aging (5T35AG029795-08), National Heart, Lung, and Blood Institute (5R25HL116372-02) and the American Medicine Sleep Foundation. Dr. Balachandran is on the speakers bureau for Itamar Medical. Dr. Mokhlesi has received grant and/or research support from NIH/NHLBI; has received grant and/or research support from and has consulted for Philips/Respironics; is on the speakers' bureau for Zephyr Medical Technologies; and has consulted for Itamar Medical. Dr. Worku is an employee of Anthem with salary and stock benefits. Dr. Arora receives royalties from McGraw Hill Publishing; receives honoraria from the American Board of Internal Medicine; and holds stock in Acadia Pharmaceuticals. Dr. Meltzer holds stock in Acadia Pharmaceuticals. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Valerie Press, MD, MPH; Matthew Churpek, MD, MPH, PhD; Dana Edelson, MD, MS; and Christopher Lyttle, MA for their valuable assistance and guidance.
ABBREVIATIONS
- BMI
body mass index
- CI
confidence interval
- IQR
interquartile range
- OSA
obstructive sleep apnea
- PHSDNQ
Potential Hospital Sleep Disruptions and Noises Questionnaire
- SD
standard deviation
REFERENCES
- 1.Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172(1):68–70. doi: 10.1001/archinternmed.2011.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manian FA, Manian CJ. Sleep quality in adult hospitalized patients with infection: an observational study. Am J Med Sci. 2015;349(1):56–60. doi: 10.1097/MAJ.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 4.Arora VM, Chang KL, Fazal AZ, et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185–2186. doi: 10.1111/j.1532-5415.2011.03644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delaney LJ, Van Haren F, Lopez V. Sleeping on a problem: the impact of sleep disturbance on intensive care patients - a clinical review. Ann Intensive Care. 2015;5:3. doi: 10.1186/s13613-015-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf J. The State of Patient Experience in American Hospitals 2013: Positive Trends and Opportunities for the Future. Southlake, TX: The Beryl Institute; 2013. [Google Scholar]
- 7.Hospital Consumer Assessment of Healthcare Providers and Systems Web site. [Accessed August 19, 2015]. http://www.hcahpsonline.org/home.aspx.
- 8.Fillary J, Chaplin H, Jones G, Thompson A, Holme A, Wilson P. Noise at night in hospital general wards: a mapping of the literature. Br J Nurs. 2015;24(10):536–540. doi: 10.12968/bjon.2015.24.10.536. [DOI] [PubMed] [Google Scholar]
- 9.Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170–179. doi: 10.7326/0003-4819-157-3-201208070-00472. [DOI] [PubMed] [Google Scholar]
- 10.Pisani MA, Friese RS, Gehlbach BK, Schwab RJ, Weinhouse GL, Jones SF. Sleep in the intensive care unit. Am J Respir Crit Care Med. 2015;191(7):731–738. doi: 10.1164/rccm.201411-2099CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller A, Roth T, Roehrs T, Yaremchuk K. Correlation between sleep disruption on postoperative pain. Otolaryngol Head Neck Surg. 2015;152(5):964–968. doi: 10.1177/0194599815572127. [DOI] [PubMed] [Google Scholar]
- 12.Freedman NS, Kotzer N, Schwab RJ. Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Respir Crit Care Med. 1999;159(4 Pt 1):1155–1162. doi: 10.1164/ajrccm.159.4.9806141. [DOI] [PubMed] [Google Scholar]
- 13.Topf M. Personal and environmental predictors of patient disturbance due to hospital noise. J Appl Psychol. 1985;70(1):22–28. [PubMed] [Google Scholar]
- 14.Gabor JY, Cooper AB, Hanly PJ. Sleep disruption in the intensive care unit. Curr Opin Crit Care. 2001;7(1):21–27. doi: 10.1097/00075198-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Validation of a telephone version of the mini-mental state examination. J Am Geriatr Soc. 1992;40(7):697–702. doi: 10.1111/j.1532-5415.1992.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 16.Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Reliability and validity of the Short Portable Mental Status Questionnaire administered by telephone. J Geriatr Psychiatry Neurol. 1994;7(1):33–38. [PubMed] [Google Scholar]
- 17.Shear TC, Balachandran JS, Mokhlesi B, et al. Risk of sleep apnea in hospitalized older patients. J Clin Sleep Med. 2014;10(10):1061–1066. doi: 10.5664/jcsm.4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 19.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 20.Whelan CT, Jin L, Meltzer D. Pain and satisfaction with pain control in hospitalized medical patients: no such thing as low risk. Arch Intern Med. 2004;164(2):175–180. doi: 10.1001/archinte.164.2.175. [DOI] [PubMed] [Google Scholar]
- 21.Chung F, Yegneswaran B, Liao P, et al. Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology. 2008;108(5):822–830. doi: 10.1097/ALN.0b013e31816d91b5. [DOI] [PubMed] [Google Scholar]


