Abstract
Background
In 2004 the Centers for Medicare & Medicaid Services (CMS) changed reimbursement for physicians and advanced practitioners caring for patients receiving hemodialysis from a capitated to a tiered fee-for-service system, encouraging increased face-to-face visits. This early version of a pay-for-performance initiative targeted a care process: more frequent provider visits in hemodialysis. While more frequent provider visits in hemodialysis are associated with fewer hospitalizations and re-hospitalizations, it is unknown whether encouraging more frequent visits through reimbursement policy also yielded these benefits.
Study Design
We used a retrospective cohort, interrupted time-series study design to examine whether the 2004 nephrologist reimbursement reform led to reduced hospitalizations and re-hospitalizations. We also used published data to estimate a range of annual economic costs associated with more frequent visits.
Setting & Participants
Medicare beneficiaries in the United States receiving hemodialysis in the two years prior to and following reimbursement reform.
Predictor
The two years following nephrologist reimbursement reform.
Outcomes
Odds of hospitalization and 30-day hospital readmission for all causes and fluid overload; US dollars.
Results
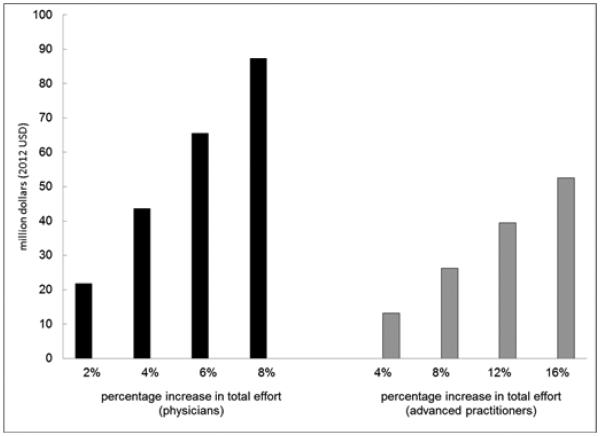
We found no significant change in all-cause hospitalization or re-hospitalization, and slight reductions in hospitalization and re-hospitalization for fluid overload following reimbursement reform; the estimated economic cost associated with additional visits ranged from $13 to $87 million per year, depending on who (physicians or advanced practitioners) spent additional time visiting patients and how much additional effort was involved.
Limitations
Due to limited information about how much additional time providers spent seeing patients after reimbursement reform, we could only examine a range of potential economic costs associated with the reform.
Conclusions
A Medicare reimbursement policy designed to encourage more frequent visits during outpatient hemodialysis may have been costly. The policy was associated with fewer hospitalizations and re-hospitalizations for fluid overload, but had no effect on all-cause hospitalizations or re-hospitalizations.
Keywords: hemodialysis, physician visit frequency, rehospitalization, economic incentives, health policy, pay for performance (P4P), Quality Incentive Program (QIP), physician reimbursement, fee-for-service, health care costs, payment reform, end-stage renal disease (ESRD), fluid overload
Pay-for-performance (P4P) initiatives are central to many healthcare reform efforts. In P4P care models, provider reimbursement depends upon the quality of care provided. Quality of care can be determined either by delivery of care processes that are deemed important, or by achievement of specific health outcomes.1 Recently enacted Medicare programs paying for transitional care management and chronic care coordination are examples of national P4P initiatives targeting care processes. The end-stage renal disease (ESRD) quality incentive program is an example of a P4P initiative focused on patients with kidney disease that targets both care processes and health outcomes. Although quality measures focusing on care processes can be more sensitive to the quality of care provided, they are only useful if the targeted care process can be modified in a way that yields improved health outcomes.2 Efforts to change provider behavior through payment reform have not always had the intended effect on health outcomes. 3-10
In 2004, the Centers for Medicare & Medicaid Services (CMS) transformed physician reimbursement for the roughly 400,000 patients receiving hemodialysis in the United States.11 The reimbursement reform targeted a specific care process: the frequency of face-to-face provider visits. Prior to 2004, nephrologist reimbursement was capitated—nephrologists received the same monthly payment regardless of how frequently they saw their patients. In 2004 reimbursement changed to a tiered fee-for-service system, where nephrologists and/or their proxy care providers are paid more for each additional face-to-face visit up to four visits per month, creating an economic incentive to see patients more often.12 Unlike traditional fee-for-service payment, additional visits under the new policy were reimbursed regardless of a documented medical need for the visit. Following the reform, physician reimbursement for outpatient hemodialysis visits increased by 18% if they saw patients at least four times in a month and decreased by 12% and 22% for two-to-three and one visit per month, respectively.12 As expected, many physicians increased visit frequency or hired advanced practitioners to do so.13-15 Due to increased visit frequency, dialysis payments to nephrologists increased by $65 million in the year following reimbursement reform.15
Costs associated with hemodialysis care are high, and health outcomes are poor.11, 16 Policy-makers had hoped that encouraging more frequent visits to patients receiving incenter maintenance hemodialysis would improve health outcomes by aligning economic incentives.12 Analyses of national cohorts in the period following reimbursement reform have suggested that patients seen more frequently by their physician (or advanced practitioner) benefit from slight reductions in hospitalization rates and more substantial reductions in 30-day hospital readmissions.17, 18 However, it is unknown whether changes in practice that occurred in response to the 2004 reimbursement reform led to similar improvements. One leading healthcare provider’s description of the effort to see patients four or more times per month as “checking off boxes,” highlights the potential ineffectiveness of these additional visits.14
In this study, we examine whether reimbursement reform from a capitated to a tiered fee-for-service system led to reductions in hospitalization and 30-day hospital readmissions among patients receiving hemodialysis. We focus on these particular health outcomes because they are associated with increased visit frequency in cross-sectional studies where visit frequency variation reflects differences in how individual providers choose to care for their patients. Additionally, we estimate the economic costs associated with the reimbursement reform under several scenarios.
METHODS
Data and Patient Selection
Medicare’s physician reimbursement reform for dialysis care occurred on January 1st, 2004. We identified prevalent patients receiving in-center hemodialysis in the United States in the two years prior to and following physician reimbursement reform (January 1, 2002 through December 31, 2005) from the US Renal Data System (USRDS), a registry of virtually all patients with treated ESRD in the United States. The USRDS contains data on patients, dialysis facilities, hospitalizations, and Medicare claims. We obtained data on population density from census-based rural-urban commuting area (RUCA) codes.19
In the analysis of hospitalizations, we divided the four-year study period into 24 two-month intervals. On the first day of each two-month interval, we selected a cohort of point prevalent patients receiving hemodialysis (generating 24 cohorts in total). We tracked patients from each cohort for two months to determine if they were hospitalized during that period. The same patient appeared in multiple two-month cohorts if he or she continued to receive in-center hemodialysis. We updated patient co-morbidities and Medicaid eligibility at the start of each new cohort period. We only included patients with six months of prior Medicare Parts A&B coverage at the start of each cohort in order to have a sufficient look-back period to ascertain patient comorbidities (Figure S1, available as online supplementary material).
In the analysis of re-hospitalization, we identified all patients discharged from the hospital during the study period, only including hospitalizations two days or longer. We determined whether patients were re-hospitalized within 30 days of hospital discharge. We separated index hospitalizations into 24 cohorts according to the two-month interval when patients were discharged from the hospital. We updated co-morbidities and Medicaid eligibility at the beginning of each cohort, and only included patients with six months of prior Medicare Parts A&B coverage at the start of each two-month interval. An individual patient could have multiple index hospitalizations.
Study Outcomes, Covariates, and Statistical Analysis
The primary study outcomes were the odds of hospitalization during each 2-month interval and the odds of re-hospitalization within 30 days of hospital discharge. We also examined hospitalizations and re-hospitalizations for fluid overload (part a of Item S1).20 Baseline characteristics of the hospitalization and re-hospitalization cohorts are shown in Table 1. Due to large population size, we used a 10% standardized difference as a marker of heterogeneity when comparing differences in characteristics between groups.21
Table 1.
Baseline Characteristics of Re-Hospitalization and Hospitalization Cohorts.
| Re-hospitalization1 | Hospitalization2 | |||||
|---|---|---|---|---|---|---|
| pre-reform (n=467,993 ) |
post-reform (n=498,416 ) |
Std Diff |
pre-reform (n=1,658,675 ) |
post-reform (n=1,735,235 ) |
Std Diff |
|
| Demographic and Socioeconomic Characteristics |
||||||
| Mean age, y | 63.7 | 63.7 | 0.2 | 63.7 | 63.8 | 0.8 |
| Male sex | 52.0 | 51.1 | 1.9 | 48.0 | 47.5 | 0.9 |
| Race/ethnicity3 | ||||||
| American Indian | 1.6 | 1.6 | 0.2 | 1.6 | 1.6 | 0.1 |
| Black | 39.2 | 39.8 | 1.1 | 38.6 | 38.6 | 0.1 |
| White | 56.1 | 55.3 | 1.6 | 55.9 | 55.7 | 0.5 |
| Other race | 3.1 | 3.3 | 1.2 | 3.9 | 4.2 | 1.3 |
| Hispanic ethnicity | 11.8 | 12.3 | 1.3 | 12.0 | 12.6 | 1.9 |
| Medicaid coverage | 48.8 | 50.1 | 2.5 | 43.8 | 44.5 | 1.6 |
| Comorbidities | ||||||
| Diabetes | 62.5 | 64.8 | 4.6 | 51.8 | 54.3 | 4.8 |
| Coronary disease | 26.5 | 26.9 | 0.9 | 15.4 | 15.8 | 1.0 |
| Cancer | 7.3 | 7.6 | 1.3 | 5.3 | 5.5 | 1.1 |
| Heart failure | 51.2 | 54.8 | 6.9 | 31.1 | 33.5 | 5.2 |
| Pulmonary disease | 28.4 | 32.2 | 8.0 | 17.0 | 19.5 | 6.5 |
| Cerebrovascular disease | 18.9 | 19.8 | 2.2 | 10.9 | 11.4 | 1.5 |
| PVD | 31.5 | 32.1 | 1.2 | 19.5 | 20.0 | 1.1 |
| Smoking history | 5.9 | 7.4 | 5.8 | 3.1 | 3.8 | 3.8 |
| Paralysis | 3.4 | 3.3 | 0.4 | 1.8 | 1.8 | 0.3 |
| Drug or alcohol use | 5.0 | 5.8 | 3.4 | 2.2 | 2.4 | 1.4 |
| Mean dialysis vintage, d* | 1081 | 1214 | 17.5 | 1092 | 1222 | 17.1 |
| Geographic and Facility Characteristics |
||||||
| Metropolitan | 83.0 | 82.8 | 0.6 | 82.1 | 81.7 | 1.2 |
| For-profit facility | 73.5 | 75.9 | 5.4 | 72.6 | 75.1 | 5.5 |
| Hospital-based facility | 18.5 | 16.4 | 5.6 | 19.0 | 16.8 | 5.6 |
| Mean facility size, no. of | ||||||
| patients | 100.0 | 98.4 | 2.6 | 100.9 | 99.1 | 3.0 |
ESRD, end-stage renal disease; PVD, peripheral vascular disease; Std Diff, standardized difference
Unless otherwise indicated, values shown are percentage of hospitalizations. ‘n’ denotes the number of index hospitalizations, which can occur more than once for a given patient. The same patient can appear in the pre-reform and post-reform groups if he or she received dialysis in both periods. This cohort includes index hospitalizations in 157,262 patients prior to reimbursement reform and in 168,654 patients following reform.
Unless otherwise indicated, values shown are percentages of patient hemodialysis time. ‘n’ denotes patient hemodialysis time represented by the number of two-month intervals. A given patient can contribute to more than one two-month interval. The same patient can appear in the pre-reform and post-reform groups if he or she received dialysis in both periods. This cohort includes two-month intervals of hemodialysis time in 229,728 patients prior to reimbursement reform and 248,278 patients following reform.
1,926 patients were excluded from the analyses prior to forming cohorts due to missing ethnicity.
We used multivariable interrupted time-series logistic regression analysis to determine whether there was a change in either the odds of hospitalization and 30-day hospital readmission, or the trend in these outcomes over time following reimbursement reform. A similar approach has been commonly used to analyze the effect of policies on health outcomes, including analyses conducted at both the aggregate and individual patient levels.22-24 We conducted our analyses at the level of individual patients and adjusted for patient, dialysis facility, and geographic characteristics listed in Table 1, along with seasonal variation in hospitalizations. Dialysis facility size was included in the models as a continuous covariate, while duration of dialysis (vintage) prior to each cohort inception and age were included as categorical variables. We excluded the first two months following the reimbursement reform in order to allow time for providers to respond to the new policy. Because the same patient could appear in multiple cohorts, in all analyses we used cluster-robust standard errors to account for correlation among repeated measures.25, 26
In the interrupted time-series regression models we used the following three variables to characterize the effect of reimbursement reform on hospitalization and re-hospitalization: 1) a “numeric date” variable representing the date of a specific cohort’s inception or index hospitalization; 2) a “policy reform” variable indicating the periods prior to and following the 2004 nephrologist reimbursement reform; and 3) a numeric date times policy reform interaction term. The coefficient for the numeric date times policy reform interaction describes how the trend in hospitalizations (or re-hospitalizations) changed following reimbursement reform (part b of Item S1).
Estimating Economic Cost of Additional Visits After Reimbursement Reform
Because reimbursement increases did not match the rate of inflation, by 2006, the inflation-adjusted amount paid by CMS per patient receiving hemodialysis had returned to its level prior to the 2004 reimbursement reform.15 Consequently, any lasting economic cost of extra visits resulting from the reimbursement reform must be understood in terms of the opportunity cost. The opportunity cost is an economic concept that quantifies the cost of an activity by the value to society associated with the next best use of the resources devoted to that activity. In the case of more frequent provider visits resulting from reimbursement reform, the opportunity cost of more frequent visits refers to the value of physician or advanced practitioner time if it were spent doing other productive activities, such as seeing patients in an ambulatory practice or in the hospital.
We used published physician and advanced practitioner salaries to estimate the opportunity cost of increased face-to-face visits. 27, 28 We estimated the opportunity cost as the product of the average full-time physician’s (or advanced practitioner’s) salary and the proportion of his or her total time spent seeing additional patients in response to reimbursement reform. We used responses from surveys of physicians and advanced practitioners to estimate the amount of time spent seeing patients receiving outpatient dialysis prior to the reimbursement reform and the average number of patients cared for by each full-time practitioner.13, 29-31 We used a published report of visit frequency before and after the reform13 and a compared published relative value units (RVUs) associated with outpatient dialysis care before and after reimbursement reform12 to identify a range of potential incremental time physicians and advanced practitioners may have spent seeing patients in response to reform. We used data on hemodialysis prevalence to convert costs per practitioner into aggregate economic cost of increased visits (part c of Item S1).32 Because of reports that advanced practitioners, on average, spend more time with their hemodialysis patients compared to physicians, we tested a higher range of additional advanced practitioner time spent in the outpatient hemodialysis setting as a result of reimbursement reform. 33
This project was approved by Institutional Review Boards at Baylor College of Medicine and Stanford University (ID numbers: Baylor, H-36408; Stanford, 17904). Informed consent was waived due to a less-than-minimum risk to patients and the de-identified nature of the data.
RESULTS
Baseline Characteristics
There were 343,844 patients included in the analysis of all-cause hospitalizations. The pre-reform period included 229,728 patients, while the post-reform period included 248,278 patients. Many patients were followed up in both periods. Groups were similar in all characteristics measured in the pre-reform and post-reform periods, except that patients in the post-reform period had been on dialysis for more days on average (Table 1). This likely reflected longer survival among the prevalent dialysis population combined with longer wait times for kidney transplantation. Patients were hospitalized during 27.1% of the 24 two-month follow-up intervals before and after reimbursement reform.
There were 259,818 patients included in the analysis of all-cause re-hospitalizations. The pre-reform period included 157,262 patients, while the post-reform period included 168,654 patients. Many patients contributed index hospitalizations in both periods. Groups were similar in all characteristics in the pre-reform and post-reform periods except that patients in the post-reform period had been on dialysis for more days on average (Table 1). Patients were re-hospitalized in 33.6% and 34.4% of months following hospital discharge prior to and following reimbursement reform, respectively.
Regression Results
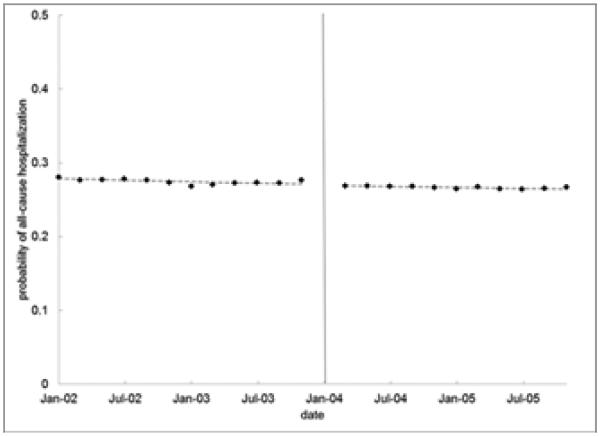
The odds of all-cause hospitalization during any two-month interval declined by approximately 0.4% every two months (95% confidence interval [CI], 0.3%-0.5%). However, there was no significant change in the odds of hospitalization immediately following reimbursement reform, and there was no significant change in the downward trend of reduced hospitalizations over time observed following reimbursement reform (p-value for policy reform times date interaction=0.2). (Figure 1a; Table 2; Table S1)
Figure 1.
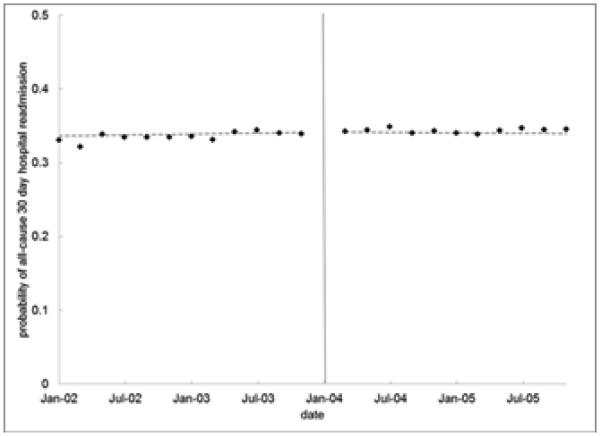
Unadjusted and Predicted Probabilities of All-Cause Hospitalization and Re-hospitalization Following Physician Reimbursement Reform
Figure 1A: Two-Month Probability of Hospitalization.
Figure 1B: Probability of Re-hospitalization.
Note: Points are unadjusted probabilities. Dotted lines are predicted probabilities from model results.
Table 2.
Results from Interrupted Time Series Regression Analyses.
| Comparison | OR (95% CI) | P | ||
|---|---|---|---|---|
| All-Cause Hospitalization: | ||||
| Date | 0.996 (0.995-0.997) | <0.001 | ||
| Post policy reform | 0.994 | 0.981 | 1.006 | 0.3 |
| Post policy reform * date since reform | 1.001 | 0.999 | 1.003 | 0.2 |
| All-Cause Re-hospitalization: | ||||
| Date | 1.002 | 1.000 | 1.004 | 0.09 |
| Post policy reform | 1.005 | 0.983 | 1.028 | 0.7 |
| Post policy reform * date since reform | 0.997 | 0.994 | 1.000 | 0.06 |
| Hospitalization for Fluid Overload: | ||||
| Date | 1.004 | 1.001 | 1.008 | 0.01 |
| Post policy reform | 1.021 | 0.987 | 1.057 | 0.2 |
| Post policy reform * date since reform | 0.988 | 0.983 | 0.992 | <0.001 |
| Re-hospitalization for Fluid Overload: | ||||
| Date | 1.011 | 1.004 | 1.017 | 0.002 |
| Post policy reform | 1.052 | 0.984 | 1.124 | 0.1 |
| Post policy reform * date since reform | 0.978 | 0.969 | 0.987 | <0.001 |
Note: Both regression models control for patient, facility, and geographic characteristics included in Table 1 of the main text, along with seasonal variation using dummy variables for each 2-month period in the calendar year. See Tables S1 and S2 for detailed regression results. CI, confidence interval; OR, odds ratio.
There was a small, non-significant, increase in the likelihood of all-cause 30-day hospital readmission over time prior to the policy (odds ratio [OR], 1.002; 95% CI, 1.000-1.004). The likelihood of being readmitted did not change immediately following reimbursement reform. There was a very slight, non-significant, relative decline in the odds of readmission over time in the post-reform period (OR, 0.997; 95% CI, 0.994-1.000). (Figure 1b; Table 2; Table S2)
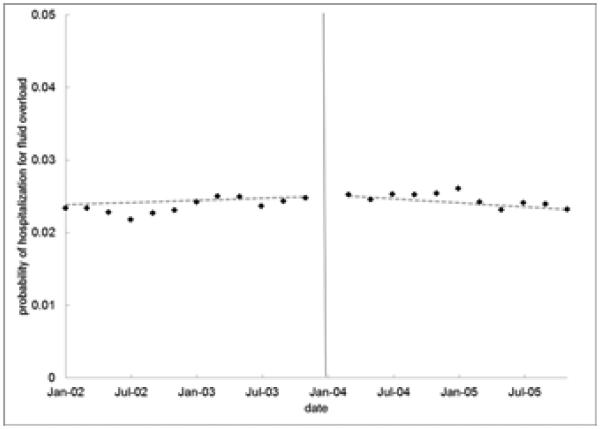
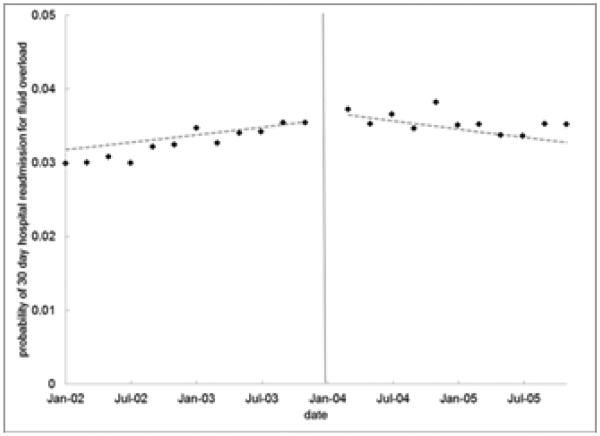
On average during the study period, patients had a 2.4% probability of hospitalization for fluid overload in a two month period and a 3.4% probability of being readmitted to the hospital for fluid overload within 30 days of a hospital discharge. The likelihoods of both hospitalization and re-hospitalization for fluid overload increased slightly over time in the period prior to reimbursement reform and did not change significantly immediately after the policy reform. The trends toward increasing hospitalizations and re-hospitalizations over time stopped−or reversed—in the two-years following reimbursement reform, indicating relative declines over time after the policy. (Figures 2a-2b; Table 2) Using average marginal effects, the fluid overload models predicted that, by the end of the study period (two years after the reform), the absolute probability of hospitalization for fluid overload in a two-month period was 0.3% lower as a result of the policy, while the probability of re-hospitalization for fluid overload was 1.1% lower as a result of the policy.
Figure 2.
Unadjusted and Predicted Probabilities of Hospitalization and Re-hospitalization for Fluid Overload Following Physician Reimbursement Reform.Figure 2A: Two-Month Probability of Hospitalization for Fluid Overload.Figure 2B: Probability of Re-hospitalization for Fluid Overload.
Note: Points are unadjusted probabilities. Dotted lines are predicted probabilities from model results.
Economic Cost of Reimbursement Reform
The opportunity cost of more frequent visits depends upon how much incremental time physicians or advanced practitioners spend seeing patients on in-center hemodialysis as a result of reimbursement reform. If all additional visits were performed by physicians, the opportunity cost (based on 2012 physician and advanced practitioner salaries) would range from $22 to $87 million per year if they spent between 2% and 8% of their time doing so. If all additional visits were performed by advanced practitioners, the corresponding opportunity cost would range from $13 to $53 million per year, assuming 4% to 16% of advanced practitioners’ time were spent seeing these patients more frequently (Figure 3).
Figure 3.
Range of Estimated Economic Costs of Additional Provider Visits.Note: Economic cost estimates were derived from published data.
Sensitivity Analyses
In a sensitivity analyses, we examined whether the effect of the policy varied according to the frequency of visits at a dialysis facility. None of our findings were sensitive to the frequency of visits to a patient’s facility in the period following the reimbursement reform (part d of Item S1).
Discussion
A policy enacted by CMS in 2004 transformed nephrologist reimbursement for outpatient hemodialysis care to a tiered fee-for-service system and created an economic incentive for physicians and advanced practitioners to see patients more frequently. Despite evidence that this policy had its intended effect (i.e., physician and advanced practitioner visits increased in 2004), we did not find associated reductions in the likelihood of all-cause hospitalization or 30 day hospital readmissions. These findings are consistent with prior analyses of this policy which failed to demonstrate a significant change in patient outcomes including survival, listing for kidney transplantation, patient satisfaction or other hemodialysis quality metrics,13, 15
In contrast to all-cause hospitalizations and re-hospitalizations, the nephrologist reimbursement reform policy was associated with a slight reduction in the likelihood of hospitalization for fluid overload and a larger reduction in the likelihood of re-hospitalization for fluid overload over time. This suggests that some patients—those who were recently discharged from the hospital and who were at risk for complications from fluid overload—eventually benefited from the policy. This is consistent with studies of physician visit frequency in the period following the 2004 nephrologist reimbursement reform demonstrating that that additional visits are of greater value for specific high-risk patient populations than they are for all patients receiving hemodialysis. For instance, we previously found that one additional physician (or advanced practitioner) visit in the period following hospital discharge predicted a 3.5% decrease in the absolute probability of a patient being re-hospitalized within 30 days,18 while more frequent visits of patients who recently initiated dialysis were associated with an increased likelihood of receiving an arteriovenous fistula or graft.34
When considering the magnitude of increase in visit frequency following reimbursement reform—a survey of 12 dialysis facilities found visit frequency increased from 1.52 to 3.14 visits per month following reimbursement reform, while an analysis of all Medicare patients found a 9.8% increase in the proportion of patients seen four or more times per month from January 2004 to March 2004—it is surprising that we did not observe significant reductions in the likelihood of all-cause hospitalization or 30-day hospital readmission following reimbursement reform. One possible explanation for this discrepancy is that the additional physician (and advanced practitioner) visits resulting from reimbursement reform were, in many instances, qualitatively different from the average visit observed in cross-sectional analyses of physician visit frequency. The amount of time nephrologists spend with their patients during face-to-face encounters has been associated with health outcomes.35 It is possible that the added visits, and associated time spent seeing patients, were often too short in duration to lead to activities that improve health outcomes. This could explain why patient satisfaction, which has been associated with more frequent visits in a cross-sectional study of visit frequency, did not improve when examined before and after the reimbursement reform.13 This also raises the possibility that the reimbursement reform did not yield other benefits that have been associated with more physician visits in cross-sectional studies such as improved achievement of clinical performance targets.34, 36, 37
Another explanation for the discrepancy between the added time spent seeing patients and the absence of broad improvements in hospitalizations and re-hospitalizations is that many of the patients who were seen more frequently as a result of the policy may not have required additional visits. For many of the healthier patients receiving hemodialysis, increased healthcare in the form of more frequent physician visits may be of little or no value. In an analysis of the sources of variation in visit frequency following reimbursement reform, we demonstrated that patient characteristics explained less than 1% of the variation in visit frequency and that the majority of visit frequency variation was explained by facility-specific and other geographic factors. Patients most likely to benefit from more frequent contact, including patients who were recently hospitalized and who were new to hemodialysis, were less likely to be seen more frequently.38
According to published estimates, payments to physicians for outpatient hemodialysis increased by $65.3 million in 2004 after reimbursement reform. After adjusting for inflation and an increase in the number of patients receiving hemodialysis, this represented a 6.0% increase in payments per patient year. Payment per patient year had returned to its pre-reform level by 2006.15 Despite the eventual return to pre-reform values, we found that the economic cost associated with additional visits in the period following reimbursement reform may have been high. Within a range of potential conservative increases in physician effort in response to the reimbursement reform, the economic cost of increased visits resulting from the policy ranged from $22 million to $87 million per year. Due to their lower salary on average, the economic cost is lower if patients are seen by advanced practitioners. When considering the absence of a benefit from the reimbursement reform on overall hospitalizations and re-hospitalizations, combined with our finding that the reform led to reduced hospitalizations and re-hospitalizations for fluid overload, the high economic cost of increased visits could be reduced if physicians were to direct their attention toward caring for patients most likely to benefit from additional care.
Our findings are consistent with previously observed limitations of fee-for-service payment systems as well as limitations of P4P programs focused on encouraging processes of care. Because the 2004 physician reimbursement policy encouraged a higher volume of care, it can be viewed as a transition from capitated payment to fee-for-service, and is consistent with literature describing the absence of a clear connection between volume of care delivered and health outcomes.39 Alternatively, because the policy was designed, in part, to improve health outcomes, and because additional visits did not require additional medical justification, the reimbursement reform can be viewed as an early P4P program directed at encouraging more face-to-face physician visits during outpatient dialysis. From this perspective, our findings are consistent with literature suggesting that policy efforts designed to encourage care processes have limited efficacy.3-6
This study has several limitations. First, we focus on the policy as a whole; we do not attempt to disentangle the various mechanisms by which the policy may have changed practices. For instance, we do not attempt to measure the effect of increased visits on rates of hospitalizations. Second, because we do not know exactly how much additional time was spent with patients or what percentage of increased visits were performed by advanced practitioners, our estimates of the potential opportunity cost associated with the policy span a wide range. While we conservatively estimated that additional hemodialysis visits would require 2%-8% of physician effort, it is quite possible that an even higher fraction of effort might be required, depending on the fraction of nephrologists’ practices devoted to hemodialysis care, the number of facilities at which nephrologists care for patients, the numbers of patients per facility and traffic times, among other factors.
In summary, we find that a national Medicare reimbursement reform designed to encourage increased face-to-face visits by physicians (nephrologists) and advanced practitioners to patients receiving hemodialysis was not associated with significant improvements in overall hospitalizations or 30-day hospital readmission, but did lead to reductions in fluid overload hospitalizations. Combined with previous studies that have failed to identify a benefit from this policy, these analyses suggest that the 2004 CMS reimbursement reform resulted in unnecessary use of some healthcare resources without materially improving health outcomes for most patients. They also suggest that efforts to encourage the care of patients most likely to benefit from additional visits, such as those at risk for fluid overload complications, could be cost-effective. Finally, our analysis highlights the importance of evaluating downstream health consequences of national reimbursement reform.
Supplementary Material
ACKNOWLEDGEMENTS
The authors acknowledge Bo Zhau, MS, for assistance with data analysis during manuscript revisions.
Support: F32 HS019178 from Agency for Healthcare Research and Quality (Dr Erickson) and DK085446 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK; Dr Chertow); Dr Bhattacharya thanks the National Institute on Aging for supporting his work on this study (R37 150127-5054662-0002). This work was conducted under a data use agreement between Dr Winkelmayer and the NIDDK; an NIDDK officer reviewed the manuscript and approved it for submission. The data reported here have been supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
N Section: Because an author of this article is an editor for AJKD, the peer-review and decision-making processes were handled entirely by an Associate Editor (Csaba P. Kovesdy, MD) who served as Acting Editor-in-Chief. Details of the journal’s procedures for potential editor conflicts are given in the Information for Authors & Journal Policies.
Financial Disclosure: The authors declaure that they have no other relevant financial interests.
Contributions: Research idea and study design: KFE, JB, GMC, WCW; data acquisition: KFE, WCW; data analysis/interpretation: KFE, JB, GMC, WCW; statistical analysis: KFE, JB; supervision or mentorship: WCW, JB, GMC. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work were appropriately investigated and resolved. KFE takes responsibility that this study has been reported honestly, accurately, and transparently; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Peer Review: Evaluated by 3 external peer reviewers, a statistician, and an Acting Editor-in-Chief.
Supplementary Material
Table S1: Regression results for analysis of hospitalizations.
Table S2: Regression results for analysis of rehospitalizations.
Figure S1: Cohort selection diagram.
Item S1: Supplemental methods.
Note: The supplementary material accompanying this article (doi:____) is available at www.ajkd.org
Supplementary Material Descriptive Text for Online Delivery
Supplementary Table S1 (PDF). Regression results for analysis of hospitalizations.
Supplementary Table S2 (PDF). Regression results for analysis of hospitalizations.
Supplementary Figure S1 (PDF). Cohort selection diagram.
Supplementary Item S1 (PDF). Supplemental methods.
REFERENCES
- 1.National Quality Measures Clearing House, NQMC . In: Selecting Quality Measures. Agency for Healthcare Research and Quality: US Department of Health and Human Services, editor. Rockville, MD: 2014. [Google Scholar]
- 2.Mant J. Process versus outcome indicators in the assessment of quality of health care. International Journal for Quality in Health Care. 2001;13:475–480. doi: 10.1093/intqhc/13.6.475. [DOI] [PubMed] [Google Scholar]
- 3.Campbell S, Reeves D, Kontopantelis E, Middleton E, Sibbald B, Roland M. Quality of primary care in England with the introduction of pay for performance. New England Journal of Medicine. 2007;357:181–190. doi: 10.1056/NEJMsr065990. [DOI] [PubMed] [Google Scholar]
- 4.Rosenthal MB, Frank RG. What is the empirical basis for paying for quality in health care? Medical Care Research & Review. 2006;63:135–157. doi: 10.1177/1077558705285291. [DOI] [PubMed] [Google Scholar]
- 5.Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Annals of Internal Medicine. 2006;145:265–272. doi: 10.7326/0003-4819-145-4-200608150-00006. [DOI] [PubMed] [Google Scholar]
- 6.Glickman SW, Ou F-S, DeLong ER, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007;297:2373–2380. doi: 10.1001/jama.297.21.2373. [DOI] [PubMed] [Google Scholar]
- 7.Werner RM, Kolstad JT, Stuart EA, Polsky D. The effect of pay-for-performance in hospitals: lessons for quality improvement. Health Affairs. 30:690–698. doi: 10.1377/hlthaff.2010.1277. [DOI] [PubMed] [Google Scholar]
- 8.Ryan AM, Blustein J, Casalino LP. Medicare's flagship test of pay-for-performance did not spur more rapid quality improvement among low-performing hospitals. Health Affairs. 31:797–805. doi: 10.1377/hlthaff.2011.0626. [DOI] [PubMed] [Google Scholar]
- 9.Eijkenaar F, Emmert M, Scheppach M, Schoffski O. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy. 110:115–130. doi: 10.1016/j.healthpol.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Ryan AM, McCullough CM, Shih SC, Wang JJ, Ryan MS, Casalino LP. The intended and unintended consequences of quality improvement interventions for small practices in a community-based electronic health record implementation project. Medical Care. 52:826–832. doi: 10.1097/MLR.0000000000000186. [DOI] [PubMed] [Google Scholar]
- 11.Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2012 annual data report. Am J Kidney Dis. 2013;61(suppl 1):e1–e480. doi: 10.1053/j.ajkd.2012.11.031. 1. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Medicare and Medicaid Services: Department of Health and Human Services Medicare program; revisions to payment policies under the physician fee schedule for calendar year 2004. Final rule with comment period. Federal Register. 2003;68:63195–63395. [PubMed] [Google Scholar]
- 13.Mentari EK, DeOreo PB, O'Connor AS, Love TE, Ricanati ES, Sehgal AR. Changes in Medicare reimbursement and patient-nephrologist visits, quality of care, and health-related quality of life. American Journal of Kidney Diseases. 2005;46:621–627. doi: 10.1053/j.ajkd.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 14.Mueller J. Has the CMS rule of "4 visits per month" influenced patient outcomes? Increased frequency of visits has promoted improved patient/provider relationships. Nephrology Nursing Journal: Journal of the American Nephrology Nurses' Association. 2007;34:343–344. [PubMed] [Google Scholar]
- 15.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Medicare Reimbursement Reform for Provider Visits and Health Outcomes in Patients on Hemodialysis. Forum for Health Economics & Policy. 2014;0:1558–9544. doi: 10.1515/fhep-2012-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorodetskaya I, Zenios S, McCulloch CE, et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int. 2005;68:2801–2808. doi: 10.1111/j.1523-1755.2005.00752.x. [DOI] [PubMed] [Google Scholar]
- 17.Slinin Y, Guo H, Li S, et al. Association of Provider-Patient Visit Frequency and Patient Outcomes on Hemodialysis. Jounal of American Society of Nephrology. 2012;23(9):1560–7. doi: 10.1681/ASN.2012010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Physician Visits and 30-Day Hospital Readmissions in Patients Receiving Hemodialysis. Journal of the American Society of Nephrology. 2014 doi: 10.1681/ASN.2013080879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WWAMI Rural-Urban Commuting Area Codes (RUCA): WWAMI Rural Health Research Center. 2005 [Google Scholar]
- 20.Arneson TJ, Liu J, Qiu Y, Gilbertson DT, Foley RN, Collins AJ. Hospital treatment for fluid overload in the Medicare hemodialysis population. Clinical Journal of The American Society of Nephrology: CJASN. 5:1054–1063. doi: 10.2215/CJN.00340110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in Medicine. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. Journal of Clinical Pharmacy & Therapeutics. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 23.Hemmelgarn BR, Zhang J, Manns BJ, et al. Nephrology visits and health care resource use before and after reporting estimated glomerular filtration rate. JAMA. 2010;303:1151–1158. doi: 10.1001/jama.2010.303. [DOI] [PubMed] [Google Scholar]
- 24.Card D, Dobkin C, Maestas N. Does Medicare save lives? National Bureau of Economic Research Bulletin on Aging & Health.Quarterly Journal of Economics. 2009;124:597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kung-Yee Liang SLZ. Longitudinal data analysis using generalized linear models. Biometrica. 1986;73:13–22. [Google Scholar]
- 26.Huber PJ. The Behavior of Maximum Likelihood Estimates under Nonstandard Conditions. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. 1967;1:221–233. [Google Scholar]
- 27.Medscape . Physician Compensation Report. Web MD; New York, NY: 2013. [Google Scholar]
- 28.National Kidney Foundation: Council of Advanced Practitioners 2012 Salary and Benefits Survey Synopsis. 2012 [Google Scholar]
- 29.Fluck RJ, Fouque D, Lockridge RS., Jr. Nephrologists' perspectives on dialysis treatment: results of an international survey. BMC Nephrology. 2014;15:16. doi: 10.1186/1471-2369-15-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harley KT, Streja E, Rhee CM, et al. Nephrologist caseload and hemodialysis patient survival in an urban cohort. Journal of the American Society of Nephrology. 2013;24:1678–1687. doi: 10.1681/ASN.2013020123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holley JL. Nephrologists as primary care providers: a review of the issues. American Journal of Kidney Diseases. 1998;31:574–583. doi: 10.1053/ajkd.1998.v31.pm9531172. [DOI] [PubMed] [Google Scholar]
- 32.Collins AJ, Foley RN, Chavers B. United States Renal Data System 2011 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. Am J Kidney Dis. 2012;59(suppl 1):e1–e420. doi: 10.1053/j.ajkd.2011.11.015. 1. [DOI] [PubMed] [Google Scholar]
- 33.Washam C. Nephrologists and Physician Extenders Enhance Partnership as Dialysis Population Grows. Nephrology Times. 1(82008):15. [Google Scholar]
- 34.Erickson KF, Mell M, Winkelmayer WC, Chertow GM, Bhattacharya J. Provider Visits and Early Vascular Access Placement in Maintenance Hemodialysis. Journal of the American Society of Nephrology. 2014;2014 doi: 10.1681/ASN.2014050464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kawaguchi T, Karaboyas A, Robinson BM, et al. Associations of frequency and duration of patient-doctor contact in hemodialysis facilities with mortality. Journal of the American Society of Nephrology. 2013;24:1493–1502. doi: 10.1681/ASN.2012080831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Plantinga LC, Jaar BG, Fink NE, et al. Frequency of patient-physician contact in chronic kidney disease care and achievement of clinical performance targets. International Journal for Quality in Health Care. 2005;17:115–121. doi: 10.1093/intqhc/mzi010. [DOI] [PubMed] [Google Scholar]
- 37.Plantinga LC, Fink NE, Sadler JH, et al. Frequency of patient-physician contact and patient outcomes in hemodialysis care. Journal of the American Society of Nephrology. 2004;15:210–218. doi: 10.1097/01.asn.0000106101.48237.9d. [DOI] [PubMed] [Google Scholar]
- 38.Erickson KF, Tan KB, Winkelmayer WC, Chertow GM, Bhattacharya J. Variation in Nephrologist Visits to Patients on Hemodialysis across Dialysis Facilities and Geographic Locations. Clinical Journal of The American Society of Nephrology: CJASN. 2013;8:987–994. doi: 10.2215/CJN.10171012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fisher ES, Goodman D, Skinner J, Bronner K. Health care spending, quality, and outcomes. The Dartmouth Institute for Health Policy and Clinical Practice; Hannover, NH: 2009. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.