Abstract
Adhesive capsulitis of the ankle is also known as frozen ankle and results in marked fibrosis and contracture of the ankle capsule. Arthroscopic capsular release is indicated for symptomatic frozen ankle that is resistant to conservative treatment. It is contraindicated for ankle stiffness due to degenerative joint disease, intra-articular malunion, or adhesion of the extensors of the ankle. The procedure consists of endoscopic posterior ankle capsulectomy and arthroscopic anterior ankle capsulotomy. It has the advantages of being minimally invasive surgery and allowing early postoperative vigorous mobilization of the ankle joint.
Ankle stiffness can be a disabling sequela after ankle trauma. This can result from secondary osteoarthrosis of the ankle, osteochondral fractures with loose bodies, intra-articular malunion, fibrosis of the periarticular tendons and muscles, or post-traumatic adhesive capsulitis.1, 2, 3 Adhesive capsulitis of the ankle is also known as frozen ankle and results in marked fibrosis and contracture of the ankle capsule.1, 2 The diagnosis is mainly based on clinical assessment. Patients with frozen ankle will complain of painful stiffness of the involved ankle and recurrent episodes of swelling and difficulty navigating stair or slope surfaces.1 The pain is most commonly deep posterior ankle pain. Extra-articular ankle stiffness due to adhesion of the periarticular tendons or muscles should be evaluated clinically before arthroscopic treatment is considered. A limitation of the toes' passive dorsiflexion with the ankle in dorsiflexion suggests tight long toe flexors, and a limitation of the toes' passive plantar flexion with the ankle in plantar flexion suggests tight long toe extensors.1 Sometimes, the diagnosis of frozen ankle needs to be confirmed by ankle arthrography. The arthrographic findings include a decrease in the joint capacity, obliteration of the normal anterior and posterior recesses, and extravasation of contrast material along the needle track.2 Currently, treatment options for the ankle include physical therapy focusing on active and passive range of motion, as well as ankle joint mobilization techniques. Shaffer et al.4 showed that after 8 weeks of immobilization after ankle fracture, 10 weeks of mobilization with physical therapy can successfully restore range of motion, strength, and function of the ankle joint. Physical therapy focusing on active and passive range of motion, as well as ankle joint mobilization techniques, has been shown to be the most beneficial for patients identified early.5 However, it may fail to improve the range of motion if it is started late after the capsular fibrosis becomes mature and contracts. If conservative care is unsuccessful, surgical treatment may be necessary.
Arthroscopic capsular release of the ankle joint is indicated for symptomatic adhesive capsulitis of the ankle that is resistant to conservative treatment. It is contraindicated for ankle stiffness due to degenerative joint disease, intra-articular malunion, or adhesion of the extensors of the ankle (Table 1).
Table 1.
Indications and Contraindications of Arthroscopic Capsular Release of Ankle
| Indication |
| Symptomatic adhesive capsulitis of ankle that is resistant to conservative treatment |
| Contraindications |
| Asymptomatic stiffness of ankle |
| Ankle stiffness due to degenerative joint disease |
| Intra-articular malunion |
| Extra-articular causes of ankle stiffness (e.g., adhesion of extensors of ankle) |
Technique
Preoperative Planning and Patient Positioning
The range of motion of the ankle joint is recorded. The motion of the toes is also studied to exclude fibrosis of the tendons as the extra-articular cause of ankle stiffness. Radiographs of the ankle are taken to exclude significant degeneration of the ankle joint or intra-articular malunion as the cause of ankle stiffness. The patient is placed in the prone position. A thigh tourniquet is applied to provide a bloodless operative field.
Placement of Posterior Portals
Posterior ankle endoscopy6 is performed with the posteromedial and posterolateral portals. The posterolateral portal is located at the lateral edge of the Achilles tendon just above the posterior calcaneal tuberosity. The posteromedial portal is at the intersection point between the medial edge of the Achilles tendon and the line joining the undersurface of the first metatarsal and the sustentaculum tali (Fig 1).7 Five-millimeter portal incisions are made, the subcutaneous tissue is spread, and the investing fascia is penetrated by a hemostat.
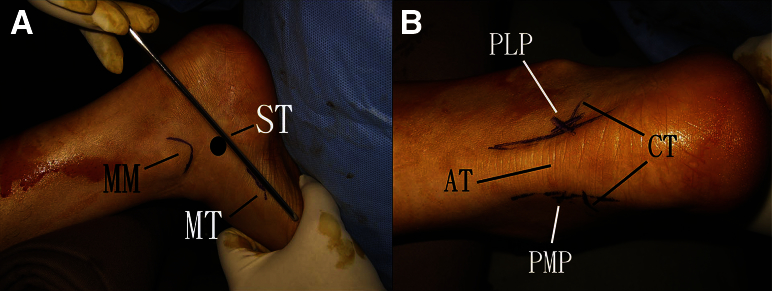
Fig 1.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. Posterior ankle endoscopy is performed with the posteromedial and posterolateral portals. (A) The posteromedial portal is at the intersection point between the medial edge of the Achilles tendon and the line joining the undersurface of the first metatarsal (MT) and the sustentaculum tali (ST). (MM, medial malleolus.) (B) The posterolateral portal (PLP) is located at the lateral edge of the Achilles tendon (AT) just above the posterior calcaneal tuberosity (CT). (PMP, posteromedial portal.)
Posterior Ankle Capsulectomy
A 4.0-mm 30° arthroscope (Dyonics; Smith & Nephew, Andover, MA) is used for this procedure.
Debridement of Posterolateral Ankle Gutter
The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. The first structure that is exposed during debridement of the lateral side of the posterior ankle is the posterior subtalar joint because of its thin capsule. The joint is traced laterally, and the posterolateral ankle gutter is reached. The fibrous tissue at the gutter is debrided by means of an arthroscopic shaver (Dyonics; Smith & Nephew) (Fig 2).
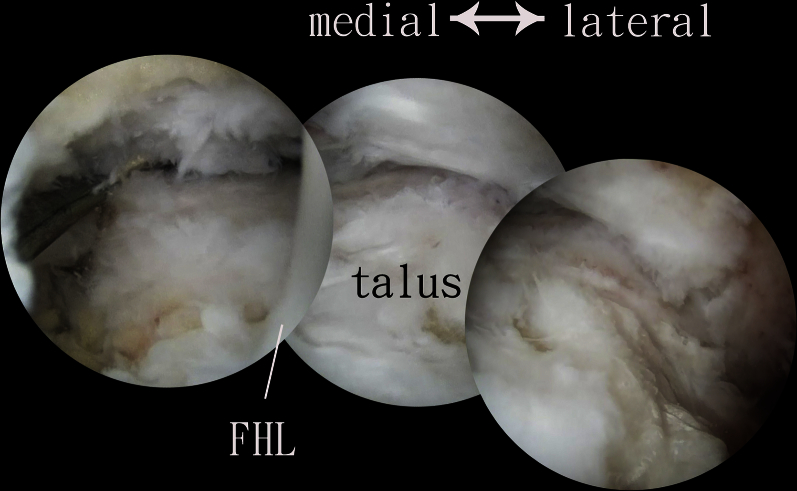
Fig 2.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. The fibrous tissue at the posterolateral ankle gutter (PLAG) is debrided by means of an arthroscopic shaver. (PSTJ, posterior subtalar joint.)
Debridement of Posterior Ankle Capsule Lateral to Flexor Hallucis Longus Tendon
The posterolateral portal is the viewing portal, and the posteromedial portal is the working portal. After clearance of the posterolateral gutter, the shaver can follow the contour of the talar dome and the fibrotic capsule lateral to the flexor hallucis longus (FHL) tendon is resected. The shaver stays lateral to the FHL tendon. The opening of the shaver should face laterally, and suction is kept to a minimum during debridement adjacent to the FHL tendon. This can reduce the risk of damage to the FHL tendon and muscle (Fig 3).
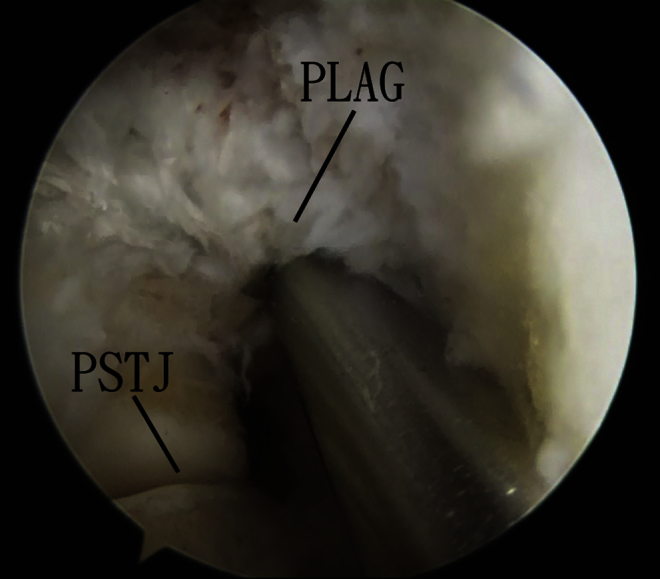
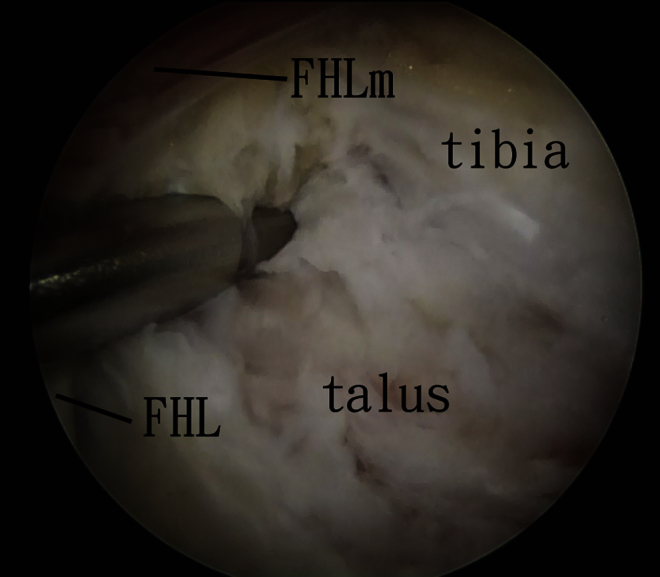
Fig 3.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The posterolateral portal is the viewing portal, and the posteromedial portal is the working portal. After clearance of the posterolateral gutter, the shaver can follow the contour of the talar dome and the fibrotic capsule lateral to the flexor hallucis longus tendon is resected. The shaver stays lateral to the flexor hallucis longus tendon. (FHLm, flexor hallucis longus muscle.)
Debridement of Posterior Ankle Capsule Medial to FHL Tendon
The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. The shaver stays lateral to the FHL tendon and pushes the FHL tendon medially to expose the posterior ankle capsule medial to the FHL tendon. This part of the posterior ankle capsule is then resected by the shaver (Fig 4). The opening of the shaver should face laterally, and suction is kept to a minimum during debridement adjacent to the FHL tendon.
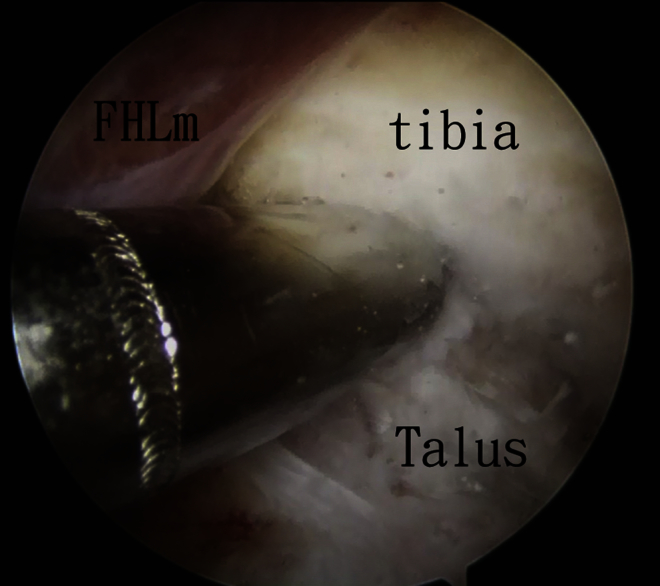
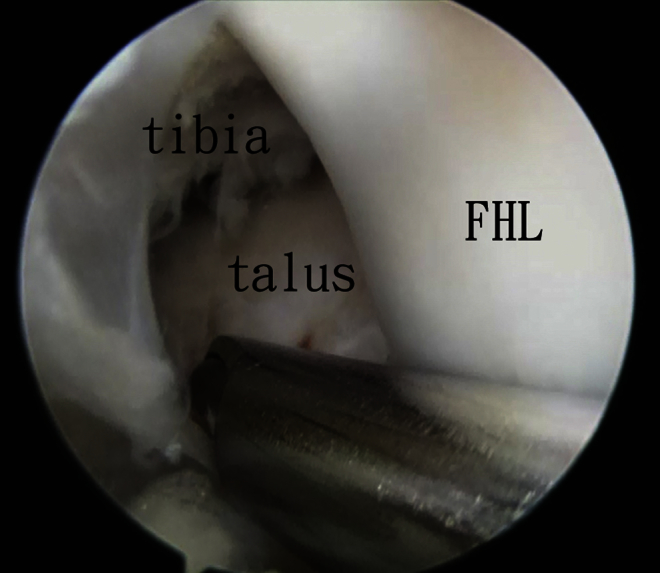
Fig 4.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. The shaver stays lateral to the flexor hallucis longus (FHL) tendon and pushes the FHL tendon medially to expose the posterior ankle capsule medial to the FHL tendon. This part of the posterior ankle capsule is then resected by the shaver. (FHLm, flexor hallucis longus muscle.)
Debridement of Posteromedial Ankle Gutter
Two approaches are used for debridement of the posteromedial ankle gutter: (1) The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. The shaver stays at the medial side of the FHL tendon, and the posteromedial corner of the ankle is debrided (Fig 5). (2) The posterolateral portal is the viewing portal, and the posteromedial portal is the working portal. The shaver is medial to the FHL tendon to debride the posteromedial ankle gutter (Fig 6). The ankle should not undergo dorsiflexion during this step to reduce the risk of impingement of the posterior tibial neurovascular bundle by the shaft of the shaver.
Fig 5.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. The shaver stays at the medial side of the flexor hallucis longus (FHL) tendon, and the posteromedial corner of the ankle is debrided.
Fig 6.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The posterolateral portal is the viewing portal, and the posteromedial portal is the working portal. The shaver is medial to the flexor hallucis longus (FHL) tendon to debride the posteromedial ankle gutter.
The completeness of posterior ankle capsulectomy can be confirmed by probing the posterior joint line from the posteromedial gutter to the posterolateral gutter. The ankle can undergo dorsiflexion passively to confirm the gain of motion, and the articular cartilage of the posterior part of the talar dome can be examined (Fig 7).
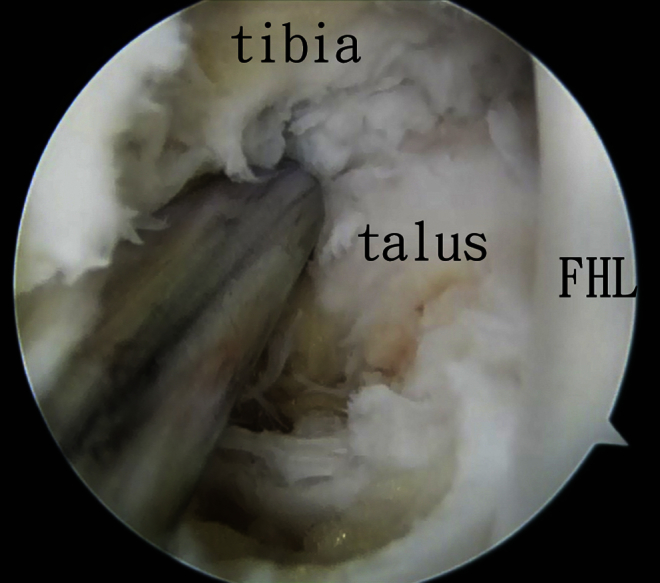
Fig 7.
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The completeness of posterior ankle capsulectomy can be confirmed by probing the posterior joint line from the posteromedial gutter to the posterolateral gutter. The ankle can undergo dorsiflexion passively to confirm the gain of motion, and the articular cartilage of the posterior part of the talar dome can be examined. (FHL, flexor hallucis longus tendon.)
Anterior Ankle Capsular Release
The knee is flexed and anterior ankle arthroscopy is performed with the standard anteromedial and anterolateral portals (Fig 8).1, 8 A 2.7-mm 30° arthroscope (Henke Sass Wolf, Tuttlingen, Germany) is used. The arthroscopic view is upside down, and the surgeon should orient himself or herself accordingly. The fibrous tissue of the anterior gutter is debrided and the fibrotic anterior ankle capsule is stripped from the distal tibia by an arthroscopic shaver (Dyonics; Smith & Nephew) (Fig 9, Video 1, Table 2).
Fig 8.
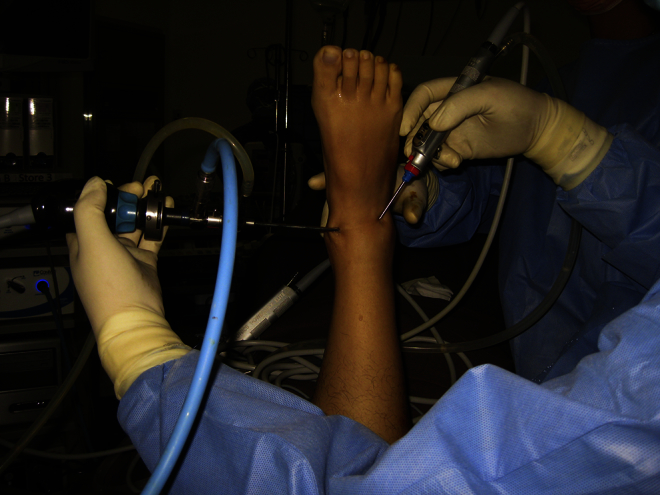
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. The knee is flexed, and anterior ankle arthroscopy is performed with the standard anteromedial and anterolateral portals.
Fig 9.
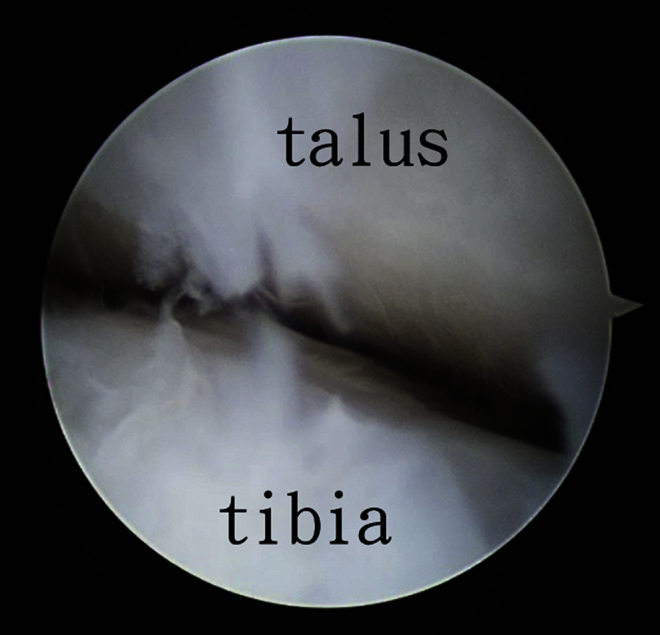
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. Anterior ankle arthroscopy is performed with the knee flexed. The arthroscopic view is upside down.
Table 2.
Pearls and Pitfalls of Arthroscopic Capsular Release of Ankle
| Pearls |
| Complete posterior ankle capsulectomy should be performed. |
| The posterior ankle endoscopic approach can deal with the flexor hallucis longus pathology. |
| Anterior ankle arthroscopy should be performed with the patient in the supine position if there is a concomitant cartilaginous lesion. |
| Pitfalls |
| Detailed preoperative assessment should be performed to exclude intra-articular malunion, ankle osteoarthritis, or extensor tendon adhesions before the arthroscopic release is conducted. |
| The ankle cannot undergo dorsiflexion during debridement of the posteromedial ankle gutter. |
Discussion
The principle of surgical treatment of symptomatic capsular contracture of a stiff joint is complete release of the joint capsule with early vigorous mobilization to prevent recurrence of the stiffness. Arthroscopic capsular release can achieve this goal because of the minimal soft-tissue trauma and small operative incisions allowing early postoperative mobilization exercise. However, a pure arthroscopic procedure can be technically difficult because of the limited joint space. The release of the posterior ankle capsule in the reported technique is performed mainly through an endoscopic approach and is feasible even if the posterior ankle capsule is markedly contracted. Moreover, this endoscopic approach allows treatment of the concomitant fibrosis of the FHL tendon and muscle.3, 7, 9 This is the reason the posteromedial portal is higher than the posterolateral portal to approach the FHL muscle and tendon in case adhesiolysis of the muscle and tendon is needed. Moreover, a higher posteromedial portal may reduce the risk of injury to the posterior tibial neurovascular bundle during debridement of the posteromedial ankle gutter.10, 11 In addition, the ankle should not undergo dorsiflexion during debridement of the posteromedial ankle gutter. Otherwise, the posterior tibial neurovascular bundle may be compressed by the shaft of the arthroscopic instruments.12
Capsulotomy rather than capsulectomy is performed during the anterior ankle capsular release. This reduces the risk of injury to the extensor tendons and anterior tibial neurovascular bundle, which are just anterior to the anterior capsule. This is an arthroscopic approach, and the adhesions of the extensor tendons cannot be dealt with by this approach. Performing anterior ankle arthroscopy with the knee flexed allows complete ankle capsular release without the need for a change in the position of the patient. However, surgeons need practice to orient themselves to the upside-down arthroscopic view. If there is a concomitant chondral lesion that needs to be dealt with during anterior ankle arthroscopy, it is better to turn the patient supine to perform the procedure in a standard manner.
To our knowledge, there is no study concerning open surgery for post-traumatic adhesive capsulitis of the ankle. In the series of Cui et al.13 of 5 patients with post-traumatic adhesive capsulitis of the ankle, steroid injections were given. Four of the 5 patients did not respond to steroid injections, and 3 underwent arthroscopic surgery. Foot Function Index scores indicated that 2 of the patients treated with arthroscopic debridement had improved function. Lui et al.1 found that ankle range of motion may improve up to 18° with dorsiflexion and up to 23° with plantar flexion after arthroscopic debridement.
In summary, the reported technique has the advantages of being minimally invasive surgery with minimal soft-tissue trauma, having better cosmetic results, and allowing early postoperative mobilization exercise. The potential risks of this technique are injury to the periarticular tendons and the anterior and posterior tibial neurovascular bundles (Table 3).
Table 3.
Advantages and Risks of Arthroscopic Capsular Release of Ankle
| Advantages |
| The technique allows early postoperative vigorous mobilization exercise of the ankle. |
| There is less surgical trauma. |
| The technique results in better cosmesis. |
| The technique can deal with various concomitant intra-articular and extra-articular pathologies. |
| Risks |
| Injury to the flexor hallucis longus tendon is possible. |
| Injury to the posterior and anterior tibial neurovascular bundles is possible. |
| Injury to the extensor tendons at the anterior ankle is possible. |
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. Posterior ankle endoscopy is performed through the posteromedial and posterolateral portals. In step 1, the posteromedial portal is the viewing portal and the posterolateral portal is the working portal. The posterolateral ankle gutter is debrided. In step 2, the posterolateral portal is the viewing portal and the posteromedial portal is the working portal. The posterior ankle capsule is resected with the shaver staying at the lateral side of the flexor hallucis longus tendon. In step 3, debridement of the posterolateral ankle gutter is performed. The shaver stays at the medial side of the flexor hallucis longus tendon. The ankle should not undergo dorsiflexion during this step.
References
- 1.Lui T.H., Chan W.K., Chan K.B. The arthroscopic management of frozen ankle. Arthroscopy. 2006;22:283–286. doi: 10.1016/j.arthro.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Goldman A.B., Katz M.C., Freiberger R.H. Posttraumatic adhesive capsulitis of the ankle: Arthrographic diagnosis. AJR Am J Roentgenol. 1976;127:585–588. doi: 10.2214/ajr.127.4.585. [DOI] [PubMed] [Google Scholar]
- 3.Lui T.H. Endoscopic adhesiolysis of the flexor hallucis longus muscle. Foot Ankle Spec. 2014;7:492–494. doi: 10.1177/1938640014546859. [DOI] [PubMed] [Google Scholar]
- 4.Shaffer M.A., Okereke E., Esterhai J.L. Effects of immobilization on plantar-flexion torque, fatigue resistance, and functional ability following an ankle fracture. Phys Ther. 2000;80:769–780. [PubMed] [Google Scholar]
- 5.Shamsi B., Falk J.N., Pettineo S.J., Ali S. Clinical review of adhesive capsulitis of the ankle: An introductory article and clinical review. Foot Ankle Online J. 2011;4:2. [Google Scholar]
- 6.van Dijk C.N., Scholten P.E., Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871–876. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 7.Lui T.H. Flexor hallucis longus tendoscopy: A technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17:107–110. doi: 10.1007/s00167-008-0623-x. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H. Ankle arthroscopy with patient in prone position. Arch Orthop Trauma Surg. 2008;128:1283–1285. doi: 10.1007/s00402-007-0435-3. [DOI] [PubMed] [Google Scholar]
- 9.Lui T.H. Arthroscopic synovectomy for zone 2 flexor hallucis longus tenosynovitis. Arthrosc Tech. 2015;4:e403–e405. doi: 10.1016/j.eats.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lui T.H., Chan L.K. Posterior ankle and hindfoot endoscopy: A cadaveric study. Foot Ankle Surg. 2016;22:186–190. doi: 10.1016/j.fas.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Lui T.H. Arthroscopic management of posteromedial ankle impingement. Arthrosc Tech. 2015;4:e425–e427. doi: 10.1016/j.eats.2015.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lui T.H. Lateral plantar nerve neuropraxia after FHL tendoscopy: Case report and anatomic evaluation. Foot Ankle Int. 2010;31:828–831. doi: 10.3113/FAI.2010.0828. [DOI] [PubMed] [Google Scholar]
- 13.Cui Q., Milbrandt T., Millinton S., Anderson M., Hurwitz S. Treatment of posttraumatic adhesive capsulitis of the ankle: A case series. Foot Ankle Int. 2005;26:602–606. doi: 10.1177/107110070502600805. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic capsular release of right ankle joint. The patient is in the prone position. Posterior ankle endoscopy is performed through the posteromedial and posterolateral portals. In step 1, the posteromedial portal is the viewing portal and the posterolateral portal is the working portal. The posterolateral ankle gutter is debrided. In step 2, the posterolateral portal is the viewing portal and the posteromedial portal is the working portal. The posterior ankle capsule is resected with the shaver staying at the lateral side of the flexor hallucis longus tendon. In step 3, debridement of the posterolateral ankle gutter is performed. The shaver stays at the medial side of the flexor hallucis longus tendon. The ankle should not undergo dorsiflexion during this step.