Abstract
OBJECTIVE
Gut microbial translocation (MT) is a major driving force behind chronic immune activation during HIV-1 infection. HIV-1-related intestinal dysbiosis, including increases in mucosa-associated pathobionts, may influence MT and contribute to mucosal and systemic inflammation. Thus, it is critical to understand the mechanisms by which gut microbes and their metabolic products, such as butyrate, influence immune cell function during HIV-1 infection.
DESIGN
A cross-sectional study was performed to compare the relative abundance of butyrate-producing bacterial species (BPB) in colonic biopsies and stool of untreated, chronic HIV-1 infected (n=18) and uninfected (n=14) study participants. The effect of exogenously added butyrate on gut T cell activation and HIV-1 infection was evaluated using an ex vivo human intestinal cell culture model.
METHODS
Species were identified in 16S ribosomal RNA sequence datasets. Ex vivo isolated lamina propria (LP) mononuclear cells were infected with CCR5-tropic HIV-1Bal, cultured with enteric Gram-negative bacteria and a range of butyrate doses, and LP T cell activation and HIV-1 infection levels measured.
RESULTS
Relative abundance (RA) of total BPB and specifically of Roseburia intestinalis, were lower in colonic mucosa of HIV-1 infected versus uninfected subjects. In HIV-1 infected study participants, R. intestinalis RA inversely correlated with systemic indicators of MT, immune activation and vascular inflammation. Exogenous butyrate suppressed enteric Gram-negative bacteria-driven LP T cell activation and HIV-1 infection levels in vitro.
CONCLUSIONS
Reductions in mucosal butyrate from diminished colonic BPB may exacerbate pathobiont driven gut T cell activation and HIV replication, thereby contributing to HIV-associated mucosal pathogenesis.
Keywords: HIV-1 infection, microbiome, mucosal immunology, butyrate, T cells
INTRODUCTION
Human immunodeficiency virus (HIV)-1 disease is associated with dramatic alterations in the gut-associated lymphoid tissue (GALT) which occur early in the course of infection and contribute to HIV-associated chronic immune activation and disease progression[1]. HIV-associated GI tract pathology is characterized by early and high level HIV-1 replication and a dramatic depletion of mucosal effector CD4 T cells [2-4] especially T helper (Th) 17 and Th22 cells [5-11] in GALT and with generalized gut inflammation [12, 13] and significant epithelial barrier damage [14-18]. The cumulative impact of these structural and immunological changes is an increase in translocation of commensal bacterial products, and perhaps bacteria themselves, from the gut lumen into the lamina propria (LP) and ultimately into the systemic circulation. Microbial translocation (MT) has been associated with systemic immune activation [19] and predicts disease progression in untreated HIV-1 infected individuals [20]. Its persistence during effective anti-retroviral therapy (ART) predicts mortality and is associated with a number of comorbidities secondary to immune activation and inflammation [21, 22].
Intestinal bacterial communities (microbiome) and their metabolites are important in shaping and maintaining gut immunity [23-27]. Recent studies by our group and others demonstrated dysbiotic fecal and/or intestinal mucosal microbiomes during both untreated and ART-treated HIV-1 infection [28-41]. We demonstrated that the relative abundance (RA) of gram negative Proteobacteria and Prevotella spp. were increased whereas Firmicutes and Bacteroides spp. were reduced in the colonic mucosa of individuals with untreated HIV infection[28]. This dysbiotic profile was associated with increased markers of MT, as well as with levels of mucosal and systemic immune activation. Recent work exploring the impact of sexual preference on HIV-1 associated intestinal dysbiosis suggested that Prevotella rich microbiota were associated with sexual preference, specifically men who have sex with men (MSM), rather than with HIV-1 infection status per se [42]. Although the increase in RA of Prevotella in our study could have been due in part to sexual preference, our finding that mucosal Prevotella spp. RA correlated with colonic myeloid dendritic cell (mDC) and T cell activation [28, 29] provides a link between dominant mucosa-associated microbes and inflammation in the setting of MT. Moreover, we demonstrated that commensal bacteria of the Prevotella genus have direct pro-inflammatory potential by activating gut mDC and increasing HIV-1 replication and CD4 T cell death in an in vitro human intestinal cell model [29, 43]. Therefore, although the increase in Prevotella observed in our study [28, 29], as well as in others [33, 36, 39], may not be entirely due to HIV-1 infection, their increased abundance in the colonic mucosa of MSM could potentially still contribute to HIV-1-associated gut pathology.
Microbial metabolites, byproducts produced by intestinal bacteria, are also important in influencing immune responses [26, 44]. Recent studies have highlighted changes in the functional activity of the microbiota during HIV-1 infection and alterations in a number of metabolic pathways identified using metagenomics approaches [35, 39, 40]. In our study using 16S rRNA sequencing[28], we observed that colonic biopsies from HIV-1 infected study participants had significantly lower RA of bacterial families (Lachnospiraceae, Ruminococcaceae) and genera (Coprococcus) within the Firmicutes phylum that are known to contain species that produce the short chain fatty acid (SCFA) butyrate[45], compared to uninfected participants. Butyrate, a fermentation product of insoluble dietary fiber, is one of three primary SCFAs produced in the colon [46], and decreases in abundances of butyrate producing bacteria (BPB) occur in several inflammatory diseases of the GI tract, including Crohn's disease, ulcerative colitis and colon cancer[47-51]. Butyrate has been reported to play important roles in colonic T regulatory cell differentiation [52-54] and in modulating both gut and blood antigen presenting cell (APC) and T cell activation [55-57]. In addition, butyrate is an important energy source for colonic epithelial cells and promotes epithelial barrier integrity [58-61]. However, despite the known immunoregulatory role of butyrate, little is known about its role in regulating mucosal inflammation in the setting of HIV-1 infection.
In this work, we compared the RA of BPB species in the colonic mucosa and stool microbiomes of untreated persons with chronic HIV-1 infection versus uninfected persons. We evaluated associations between BPB RA and indicators of mucosal and systemic immune activation and inflammation during HIV-1 infection. Finally, to address potential mechanisms, we directly investigated the impact of exogenous butyrate on pathobiont-driven T cell activation and HIV-1 infection using an in vitro lamina propria mononuclear cell (LPMC) model.
METHODS
Clinical study participants and study design
Eighteen HIV-1 infected adult participants who were ART-naïve or had not been on treatment for more than 7 days prior to the study and 14 HIV-1 uninfected adult control participants were enrolled into this cross-sectional study at the University of Colorado Anschutz Medical Campus. Clinical characteristics of study participants are detailed in Supplementary Table 1. Exclusion criteria for this study are extensively detailed elsewhere [28, 29] and listed in supplementary data. This study was approved by the Colorado Multiple Institutional Review Board (COMIRB) at the University of Colorado Anschutz Medical Campus.
Clinical study sample processing and analysis
The collection, storage and processing of rectal swabs, colon biopsies, plasma and peripheral blood mononuclear cells (PBMC) from these study participants is extensively detailed elsewhere [28, 29]. Indicators of systemic inflammation (IL-6, high sensitivity C-reactive Protein (hsCRP), intestinal fatty acid binding protein (iFABP), LP-PLA2, IFNγ, TNFα and IL-10), peripheral blood and colonic CD4 and CD8 T cell activation (CD38+HLA-DR+) and levels of colonic mDC activation (CD40 expression) were previously evaluated in these study subjects and the methods detailed elsewhere [28, 29]
Bacterial 16S ribosomal RNA (rRNA) gene sequencing and identification of BPB species
Laboratory and analytic methods used to determine species level taxonomic classification of 16S rRNA sequence datasets generated from these study participants are detailed extensively elsewhere [28, 29, 43]. A species was identified when a sequence overlapped a Silva[62] database sequence by at least 95% sequence length with at least 99% sequence identity and the taxonomy of the database hit matched the taxonomy returned by SINA[63].
SYBR-Green quantitative PCR for Butyryl-CoA-CoA transferase transcripts
Butyryl-CoA-CoA transferase transcripts were quantified by qPCR using SYBR green PCR reagent (Supplementary Methods).
Virus and bacteria stock preparation
HIV-1Bal (AIDS Research and Reference Program #510) and mock-infected supernatant stocks were generated and frozen in single use aliquots at −80°C as previously described[43, 64]. Prevotella stercorea (DSM#18206, DSMZ, Braunschweig, Germany) was grown under anaerobic conditions, enumerated and stored in single use aliquots at −80°C as previously detailed[29, 43].
HIV-1 infection of LPMCs
LPMCs were isolated from macroscopically normal human jejunum tissue (n=9) and cultured in vitro as detailed previously [43, 64-67] and in Supplementary Methods. HIV-1Bal (80ng p24/1 × 106 LPMCs) was used to infect primary LPMCs by spinoculation [64]. LPMCs were mock infected in parallel. HIV-1Bal and mock infected LPMC were cultured with increasing concentrations (0mM, 0.2mM and 2mM) of butyric acid (Sigma-Aldrich, St Louis, MO). Live P. stercorea were added to appropriate wells of antibiotic-containing media at 2.5 bacteria to 1 LPMC and harvested at 4 days post infection.
Measurement of T cell activation and infection levels in the in vitro LPMC model
Measurements of CD4 and CD8 T cell activation and productive HIV-1 infection of CD4 T cells were carried out using multi-color flow cytometry as previously described [43, 64, 65]. Specific clones and fluorophores are detailed in Supplementary Table 2. All flow cytometry acquisition was performed on an LSRII Flow Cytometer (BD Biosciences, San Jose, CA). Routine quality control using the Cytometer Setup and Tracking feature with BD FACSDIVA software (V6.1) was performed daily as previously described[65]. Analysis was performed using BD FACSDIVA software. The flow gating scheme is illustrated in Supplementary Figure 1.
T cell cytokine production quantification
IL-17A and IFNγ levels were quantified in culture supernatant by ELISA according to manufacturer's recommendations (eBiosciences, San Diego, CA).
Statistical analysis
Statistical analysis and graphing was performed using GraphPad Prism Version 6 for Windows (Graphpad Software, San Diego, CA). Non-parametric tests were performed. Mann-Whitney tests were used to compare unmatched groups and correlations analyzed using Spearman's test. Differences between groups of matched paired data were performed using the Wilcoxon's matched-pairs signed-rank test and multiple groups of matched paired comparisons were performed using the Friedman test with multiple Dunn comparisons. Significance was determined at P< 0.05.
RESULTS
Butyrate-producing bacteria (BPB) are less abundant in colonic mucosa in untreated, HIV-1 infected individuals
The major colonic BPB species were identified based on previously published reports, in which BPB were classified by butyrate production in bacterial culture studies and DNA sequence analysis for enzymes required for butyrate synthesis [45]. In both study groups, 15 of the 18 reported colonic BPB species were detected in at least one subject in both stool (data not shown) and colonic biopsies (Table 1). For each study participant, the RA of each of the 15 BPB species from each sample type was summed to give a total BPB RA. In uninfected study participants the median total BPB RA in the colonic mucosa was significantly higher than that in the stool (Fig. 1A; p<0.05). The median total RA of BPB species was also higher in the colonic mucosa compared to stool of HIV-1 infected study participants, although this difference did not reach statistical significance (Fig. 1A). When comparisons were made between uninfected and HIV-1 infected study participants, the summed RA of BPB species was significantly lower in the colonic mucosa of HIV-1 infected subjects relative to controls (p=0.009), whereas summed RA of BPB species in the stool were similar (Fig. 1A).
Table 1.
Relative abundances of known colonic butyrate-producing bacteria in colonic tissue from HIV-1 uninfected and untreated, chronic HIV-1 infected study participants.
| Uninfected subjects | HIV-1 infected subjects | |||||
|---|---|---|---|---|---|---|
| Family | Species | Prevalence* | Abundance (%) # | Prevalence | Abundance (%) | P value |
| Ruminococcaceae | Faecalibacterium prausnitzii | 14/14 | 6.5 (0.23-16.05) | 17/17 | 2.575 (0.01-16.99) | 0.17 |
| Eubacteriaceae | Eubacterium rectale | 14/14 | 4.15 (0.003-20.65) | 17/17 | 0.71 (0.003-17.4) | 0.17 |
| Lachnospiraceae | Roseburia faecis | 14/14 | 0.736 (0.005-10.02) | 16/17 | 0.036 (0-4.646) | 0.17 |
| Lachnospiraceae | Roseburia inulinivorans | 14/14 | 0.239 (0.003-3.63) | 15/17 | 0.091 (0-10.62) | 0.85 |
| Lachnospiraceae | Roseburia intestinalis | 14/14 | 0.236 (0.006-1.55) | 14/17 | 0.016 (0-8.35) | 0.06 |
| Eubacteriaceae | Eubacterium hallii | 11/14 | 0.18 (0-1.356) | 10/17 | 0.001 (0-0.84) | 0.13 |
| Lachnospiraceae | Anaerostipes caccae | 14/14 | 0.06 (0003-4.761) | 15/17 | 0.029 (0-1.24) | 0.26 |
| Lachnospiraceae | Coprococcus comes | 11/14 | 0.053 (0-2.183) | 9/17 | 0.001 (0-1.826) | 0.41 |
| Clostridiales | Subdoligranulym variabile | 10/14 | 0.004 (0-0.315) | 9/17 | 0.002(0-0.068) | 0.36 |
| Lachnospiraceae | Coprococus catus | 9/14 | 0.003 (0-2.07) | 12/17 | 0.003 (0-0.63) | 0.74 |
| Lachnospiraceae | Roseburia hominis | 12/14 | 0.003 (0-0.867) | 8/17 | 0 (0-0.58) | 0.11 |
| Lachnospiraceae | Coprococcus eutactus | 9/14 | 0.0014 (0-2.18) | 12/17 | 0.0101 (0-1.997) | 0.46 |
| Ruminococcaceae | Anaerotruncus colihominis | 9/14 | 0.0014 (0-0.888) | 9/17 | 0.0011 (0-0.098) | 0.82 |
| Eubacteriaceae | Eubacterium cylindroides | 3/14 | 0 (0-1.575) | 5/17 | 0 (0-0.177) | 0.66 |
| Lachnospiraceae | Butyrivibrio fibrisolvens | 2/14 | 0 (0-0.0012) | 1/17 | 0 (0-0.0005) | 0.35 |
All bacteria belong to phylum Firmicutes, class Clostridia and order Clostridiales.
Number of individual subjects in which species was detected
Abundance of each species shown as percent of all classified species (median, range). Statistical analysis was performed using the Mann-Whitney test.
Figure 1. Communities of butyrate-producing bacteria (BPB) are reduced in colon mucosa of untreated HIV-1 infected study participants.
Relative abundances (RA) of the major colonic butyrate-producing species were evaluated in 16S rRNA sequence datasets derived from stool and colonic biopsies of 14 HIV-1 uninfected control (n=14) and untreated, chronic HIV-1 infected (n=17-18) study participants. (A) Summed RA were determined in the stool and colonic mucosa of HIV-1 uninfected (HIV−; n=14) (open circles) and untreated, chronic HIV-1 infected (HIV+; Stool n=18; colonic mucosa: n=17) (filled squares) study participants. (B) RA of Roseburia intestinalis in the colonic mucosa of HIV-1 uninfected (HIV−; n=14) (open circles) and untreated, chronic HIV-1 infected (HIV+; n=17) (filled squares) study participants. (C) Ratio of RA of P. stercorea to R. intestinalis (P. stercorea:R. intestinalis) in colonic mucosa of HIV-1 uninfected (HIV−; n=14) (open circles) and untreated, chronic HIV-1 infected (HIV+; n=14) (filled squares) study participants. RA of R. intestinalis were undetectable in 3 HIV-1 infected individuals therefore a ratio was not calculated for these study participants (n=14). (D) Correlations between P. stercorea:R. intestinalis and the number of activated (CD38+HLA-DR+) colon CD4 and CD8 T cells and activated colon CD1c+ mDC (CD40 expression levels) in HIV-1 infected study participants (n=14 for colon T cell activation; n=11 for colon CD1c+ mDC activation). Lines represent median values (A-C). Statistical analysis was performed using the Wilcoxon matched-pairs signed rank test to determine differences in matched groups (A), the Mann-Whitney test to determine differences between unmatched groups (A-C) and Spearman test to determine correlations between variables (D).
The majority of human colonic BPB use Butyryl-coenzyme A (CoA) CoA transferase for the last step of butyrate formation [68]. In stool samples of uninfected study participants (n=13), copies of the Butyryl-CoA CoA transferase gene (normalized to total 16S bacterial DNA) strongly correlated (r=0.90, p<0.0001) with summed RA of the major BPB in matched stool samples (Supplementary Figure 2). This confirmed the accuracy of identifying the predominant BPB species in our sample set based on 16S rRNA sequencing.
SCFAs are generated by commensal BPB from dietary fiber; therefore, we assessed associations between BPB abundance in colonic mucosa and the results of a dietary questionnaire completed by study participants [28]. As previously reported, although no significant differences were observed in the reported servings of fruit/vegetables consumed per week between uninfected controls and HIV-infected study participants, the median number of servings was lower in the HIV-infected cohort [28]. A trend towards a positive correlation was found between servings of fruit/vegetables and total colonic BPB RA among uninfected subjects (r=0.47, p=0.09; n=14). Conversely, among the HIV-1 infected group, no clear trend was observed in the association between servings of fruit/vegetables and total colonic BPB RA (r=0.08, p=0.76, n=17).
Roseburia intestinalis abundance is inversely associated with indicators of systemic inflammation in HIV-infected individuals
Among individual BPB species, the relative decrease in RA of Roseburia intestinalis neared statistical significance in the colonic mucosa of HIV-1 infected study participants (Fig. 1B; Table 1). R. intestinalis RA correlated inversely with plasma HIV-1 viral load and blood CD4 T cell activation levels (Table 2). Further, R. intestinalis RA inversely correlated with levels of plasma LPS and sCD14, indicators of MT and monocyte activation, as well as with plasma TNFα and IL-10 levels (Table 2). Finally, inverse correlations were noted between R. intestinalis and LP-PLA2, an indicator of vascular inflammation (Table 2). Significant correlations between other high abundance BPB (e.g. Faecalibacterium prausnitzii, Eubacterium rectale) and inflammatory biomarkers were not observed (data not shown).
Table 2.
Associations between abundances of colonic mucosa R. intestinalis and clinical, virological and immunological parameters in HIV-1 infected study participants.*
| Clinical parameters | Spearman test |
|---|---|
| Blood CD4 count | R= 0.41, p=0.11 |
| Plasma viral load | R= −0.58, p=0.02 |
| Systemic immune activation and inflammation | |
| Blood T cell activation | |
| CD38+ HLA-DR+ CD4 T cells (% of CD4 T cells) | R= −0.74, p=0.001 |
| CD38+ HLA-DR+ CD8 T cells (% of CD8 T cells) | R= −0.33, p=0.20 |
| Systemic inflammation | |
| Plasma IL-6 levels | R= −0.32, p=0.21 |
| Plasma C-reactive protein (CRP) levels | R= −0.22, p=0.39 |
| Plasma intestinal fatty acid bind protein (iFABP) levels | R= 0.23, p=0.37 |
| Plasma LP-PLA2 levels | R= −0.49, p<0.05 |
| Plasma IFNγ levels | R= 0.07, p=0.78 |
| Plasma TNFα levels | R= −0.68, p=0.003 |
| Plasma IL-10 levels | R= −0.61, p=0.01 |
| Systemic microbial translocation and monocyte activation | |
| Plasma LPS levels (n=16) | R= −0.74, p=0.001 |
| Plasma LTA levels | R= −0.43, p=0.08 |
| Plasma sCD14 levels | R= −0.58, p=0.02 |
| Colonic immune activation | |
| Myeloid CD1c+ dendritic cells (CD1c+ mDC) activation# (n=13) | R= −0.30, p=0.32 |
| Colonic T cell activation | |
| Number of activated (CD38+ HLA-DR+) CD4 T cells | R= −0.37, p=0.15 |
| Number of activated (CD38+ HLA-DR+) CD8 T cells | R= −0.27, p=0.29 |
n=17 unless otherwise noted
measured as CD40 expression levels. Statistical analysis was performed using the Spearman test with significant associations shown in bold.
Ratio of P. stercorea to R. intestinalis positively correlates with colonic immune activation in HIV-infected individuals
We previously reported higher RA of Prevotella species (i.e., P. stercorea and P. copri), with described pro-inflammatory potential, in the colonic mucosa of this same cohort of HIV-1 infected study participants [29]. Therefore, we next investigated a possible relationship between RA of Prevotella species and immune-modulatory BPB by calculating the ratio of P. stercorea to R. intestinalis (Ps:Ri) RA for each study participant. As expected, Ps:Ri was significantly higher in HIV-1 infected individuals compared to uninfected control subjects (Fig. 1C). Among the HIV-1 infected persons, Ps:Ri positively correlated with the percent of activated blood CD4 T cells (based on CD38+HLA-DR+ expression) and with plasma levels of sCD14 (Table 3). Moreover, Ps:Ri positively correlated with numbers of activated colonic mucosa CD4 and CD8 T cells and with levels of CD1c+ mDC activation (Fig. 1D) (Table 3).
Table 3.
Associations between ratio of colonic mucosa P. stercorea to R. intestinalis and clinical, virological and immunological parameters in HIV-1 infected study participants.*
| Clinical parameters | Spearman test |
|---|---|
| Blood CD4 count | R= −0.35, p=0.22 |
| Plasma viral load | R= 0.26, p=0.37 |
| Systemic immune activation and inflammation | |
| Blood T cell activation | |
| CD38+ HLA-DR+ CD4 T cells (% of CD4 T cells) | R= 0.66, p=0.01 |
| CD38+ HLA-DR+ CD8 T cells (% of CD8 T cells) | R= 0.02, p=0.95 |
| Systemic inflammation | |
| Plasma IL-6 levels | R= 0.18, p=0.52 |
| Plasma C-reactive protein (CRP) levels | R= −0.15, p=0.61 |
| Plasma intestinal fatty acid bind protein (iFABP) levels | R= −0.24, p=0.41 |
| Plasma LP-PLA2 levels | R= 0.50, p=0.07 |
| Plasma IFNγ levels | R= 0.26, p=0.38 |
| Plasma TNFα levels | R= 0.45, p=0.11 |
| Plasma IL-10 levels | R= 0.50, p=0.07 |
| Systemic microbial translocation and monocyte activation | |
| Plasma LPS levels | R= 0.16, p=0.59 |
| Plasma LTA levels | R= −0.02, p=0.94 |
| Plasma sCD14 levels | R= 0.63, p=0.02 |
| Colonic immune activation | |
| Myeloid CD1c+ dendritic cells (CD1c+ mDC) activation# (n=11) | R= 0.66, p=0.03 |
| Colonic T cell activation | |
| Number of activated (CD38+ HLA-DR+) CD4 T cells | R= 0.65, p=0.01 |
| Number of activated (CD38+ HLA-DR+) CD8 T cells | R= 0.81, p=0.0007 |
n=14 unless otherwise noted
measured as CD40 expression levels. Statistical analysis was performed using the Spearman test with significant associations shown in bold.
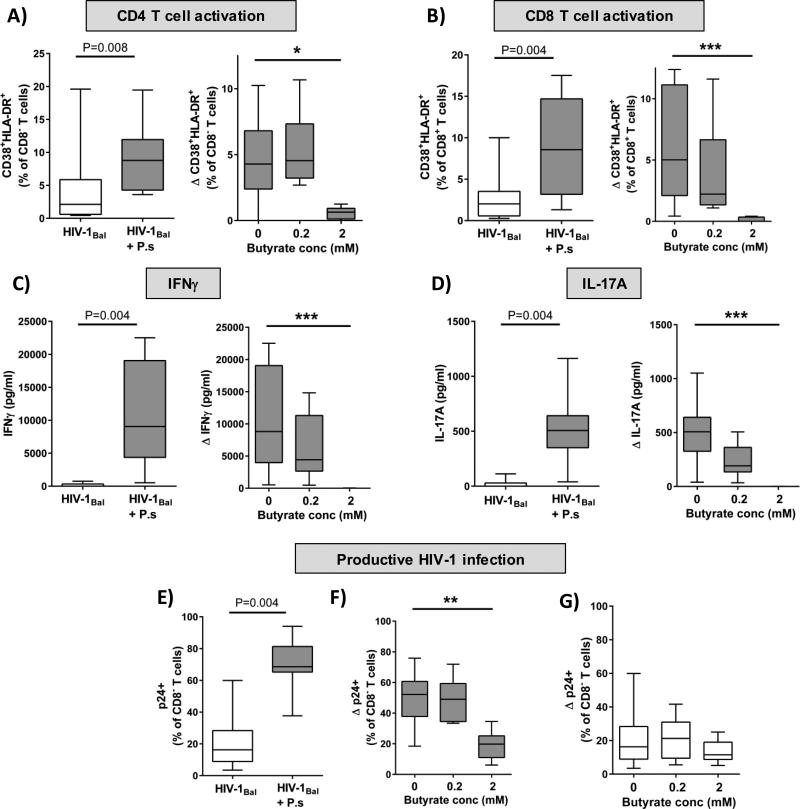
Butyrate reduces P. stercorea-driven activation of HIV-1 infected LP T cells and pro-inflammatory cytokine production in vitro
Findings from our clinical study led to the hypothesis that a loss of butyrate might exacerbate P. stercorea-driven intestinal T cell activation. Accordingly, we used an ex vivo human LPMC model that mimics the effects of translocating bacteria (i.e. MT) on LP T cell function [43, 64, 65] to examine whether exogenous butyrate modulates immune cell function. Butyrate was assessed at high (2mM) and low (0.2mM) concentrations, similar to concentrations used in other published studies [56, 69, 70]. Butyrate at these concentrations did not significantly (p= 0.154) reduce the number of CD4 T cells in unstimulated mock-infected cultures indicating a lack of general cellular toxicity.
In the absence of butyrate, the addition of P. stercorea to HIV-infected LPMC cultures significantly increased LP CD4 T cell activation levels above those induced with infection alone (Fig. 2A). The addition of 2mM butyrate significantly decreased P. stercorea-driven LP CD4 T cell activation (Fig. 2A) compared to levels observed in the absence of butyrate (0mM). Low dose butyrate (0.2mM) had minimal impact of P. stercorea-associated T cell activation levels. Similar suppressive effects of higher doses of butyrate were observed on LP CD8 T cell activation, which was also increased in the presence of P. stercorea (Fig. 2B). Furthermore, the addition of P. stercorea to HIV-infected LPMC cultures led to greater production of IFNγ and IL-17A (Fig. 2C and D) compared to HIV-infected cultures alone. Butyrate inhibited both IFNγ (Fig. 2C) and IL-17A (Fig. 2D) production in a dose dependent manner, with complete suppression observed at 2mM. Butyrate, at 2mM, was similarly able to decrease P. stercorea driven LP CD4 and CD8 T cell activation as well as cytokine production in the absence of HIV-1 infection (Supplementary Figure 3)
Figure 2. Butyrate reduces P. stercorea-enhanced LP T cell activation and HIV-1 productive infection.
Lamina propria mononuclear cells (LPMC) were spinoculated with CCR5-tropic HIV-1Bal and cultured with or without P. stercorea and butyrate (0.2mM, 2mM) for 4 days and levels of T cell activation, cytokine production and productive HIV-1 infection determined (n=9). Percentages of LP CD4 (A) and CD8 (B) T cells co-expressing CD38 and HLA-DR were assessed using multi-color flow cytometry. FMO and isotype control values have been subtracted. Levels of IFNγ (C) and IL-17A (D) in culture supernatants at day 4 were evaluated by ELISA. Percentages of p24-expressing LP CD4 T cells (E-G) were assessed using multi-color flow cytometry. P. stercorea-specific (Δ) values are shown as net values (P. stercorea/HIV-1 minus HIV-1 alone). Statistical significance was determined using the Wilcoxon matched pairs signed rank test and the Friedman's test with comparisons to no butyrate controls. (**P<0.01, ****P<0.0001). Data displayed as box and whiskers are represented with the box extending from the 25th to 75th percentile with the median value represented as the central line in the box and maximum and minimum values represented by the whisker.
Butyrate inhibits P. stercorea-driven HIV-1 infection in LP CD4 T cells
We next investigated butyrate's effects on P. stercorea-driven LP T cell infection. In agreement with our previous study [43], exposure of HIV-1Bal-infected LPMC to P. stercorea in the absence of butyrate significantly increased the percentage of productively infected (HIV-1 p24+) LP CD4 T cells compared to HIV-1Bal infection alone (Fig. 2E). Addition of 2mM butyrate suppressed P. stercorea-driven T cell infection to levels observed with virus infection alone, whereas 0.2mM butyrate had minimal effect (Fig. 2F). Butyrate had no observable impact on HIV-1Bal infection levels detected in the absence of P. stercorea (Fig. 2G), suggesting that butyrate does not impact baseline HIV-1 infection.
DISCUSSION
Microbial translocation has been linked to mucosal and systemic inflammation and is predictive of disease progression and mortality in HIV-1 infected individuals [21, 22]. It is therefore critically important to understand the mechanisms by which gut microbes influence immune function during HIV-1 infection. In this study, colonic mucosa BPB species were lower in abundance in untreated HIV-1 infected individuals relative to uninfected study participants. Abundance of R. intestinalis, a dominant BPB which was decreased to the greatest degree in untreated HIV-1 infected study participants, was inversely associated with indicators of systemic MT, immune activation and vascular inflammation. Moreover, in vitro studies demonstrated that higher levels (2mM) of butyrate inhibited pathobiont-driven LP T cell activation, cytokine production (IL-17A and IFNγ) and HIV-1 infection of CD4 T cells, whereas lower butyrate levels lacked this strong immunomodulatory effect. If extrapolated to the clinical HIV infection setting, the butyrate-driven decrease in IL-17 production might be considered counter-productive in the face of Th17 cell depletion. Yet, it is important to emphasize that our in vitro LPMC model mimics acute HIV infection, in which the activation of Th17 cells in response to enteric bacteria occurs in association with their increased productive infection and depletion. We postulate that in vivo, butyrate would mitigate the loss of LP Th17 cells by inhibiting this pathobiont-driven activation in response to MT. Taken together, our observations suggest that a loss of colonic mucosal BPB, with a presumptive decrease in mucosal butyrate levels, in conjunction with increased abundance of pro-inflammatory, pathobiont commensal bacteria could promote unregulated inflammatory responses and mucosal HIV-1 replication. This would then further drive epithelial barrier damage and MT.
In our study, total BPB were observed at higher RA in the mucosa than in the stool. Although our study did not measure butyrate levels directly, the specific reduction in BPB only in the colonic mucosa of HIV-1 infected individuals would likely indicate a decrease in butyrate at the mucosal surface and therefore reduced availability of this SCFA to colonic epithelial cells (colonocytes) and mucosal immune cells. While the RA and location of BPB species likely has an important impact on the amount of butyrate produced in the colon, other factors such as diet can play a large role. For instance, soluble fibers with high degrees of polymerization, such as inulin, are fermented in the gut which results in SCFA production [71-73]. Using a limited dietary questionnaire, our study observations suggest that HIV-1 infection may disrupt the normal association between diet and RA of BPB species, thereby potentially contributing to the dysbiosis of the intestinal microbiome seen during HIV-1 infection.
Butyrate plays several important roles in colonocyte function including acting as a metabolic energy source for colonocytes[58-60], increasing tight junction-mediated barrier integrity [74] and protecting colonocytes from cellular damage and stress [61, 75]. Further, by decreasing NFκB activation in metabolically stressed colonic epithelial cell lines, butyrate subsequently prevented transcytosis of E. coli in an in vitro epithelial cell/bacteria co-culture model [59]. Although we cannot infer causality, our observations that the abundance of R. intestinalis inversely associated with indicators of MT in HIV-1 infected persons suggest that reduced levels of butyrate may be a contributing factor to HIV-1-associated epithelial barrier breakdown that leads to MT.
Butyrate impacts cellular responses via G-coupled Protein Receptor (GPR) signaling (GPR41, GPR43 and GPR109a) and/or through inhibition of histone deacetylases (HDAC)[46, 76]. In our in vitro LPMC model, higher doses of butyrate were associated with the greatest inhibition of enteric bacteria-induced T cell activation and cytokine production in the presence or absence of HIV-1. Given that activated T cells are preferentially infected by HIV-1[77, 78], the decrease in enteric bacteria-driven LP T cell activation likely results in the decrease in the percentage of productively infected LP CD4 T cells. Butyrate has been shown to inhibit murine splenic T cell proliferation and to increase apoptosis of activated T cells via HDAC inhibition (HDACi)[55, 70]. Therefore, we postulate that butyrate dampens enteric-bacteria induced LP T cell activation via HDACi resulting in the modification of gene transcripts involved in T cell activation, cytokine production and/or cell death. Conversely, given the heterogeneous nature of our LPMC cultures, butyrate may also inhibit LP T cell activation indirectly through its effects on other cells such as mDCs, which we have shown to be critical in activation of LP T cells in response to enteric bacteria in vitro[65, 67]. Studies are now underway to determine if the butyrate-dependent decrease in T cell responses following exposure to bacteria are driven by inhibition of T cell activation and/or proliferation, increased death of activated T cells or, most likely, a combination of these factors and to address the signaling pathways that control these responses. In addition, butyrate itself has been shown to induce HIV-1 provirus expression in latently infected central memory CD4 T cells through its HDACi activity[79-81]. We did not see an observable effect of butyrate on HIV-1 replication in absence of enteric bacteria exposure; however, our in vitro LPMC HIV-1 infection model was not designed to reflect latency.
To understand whether viral replication drives reductions in BPB, an important follow up to this study would be to determine the effect of ART on abundances of BPB species. Several studies have examined the intestinal mucosal microbiomes of HIV-1 infected individuals on ART[35, 36] and observed lower RA of mucosa-associated genera that include BPB. Specifically, Mutlu et. al. examined the mucosal microbiome at several sites in the gastrointestinal tract in a cohort of HIV-1 infected individuals of which 90% were on ART[36]. Compared to a cohort of uninfected controls, HIV-1 infected individuals had lower RA of Faecalibacterium, Coprococcus and Roseburia genera which are known to contain several BPB species. Similarly, microbiome analysis of rectal mucosa secretions by McHardy et. al. determined a lower RA of Coprococcus, Eubacterium and Roseburia in ART-treated HIV-1 infected individuals compared to healthy controls, although this did not reach statistical significance[35]. These data suggest that reduced RA of BPB species may persist in some individuals despite ART.
There are several limitations to the current study. The exploratory microbiome analysis was not powered to specifically address changes in the RA of BPB species and their relationship with the various immunological and virological readouts. Although we applied stringent criteria for assigning species (99% sequence identity), we acknowledge that there are some limitations in the assignment of species-level taxonomy from short-read sequencing data. However, the decreased abundances of BPB species is supported by observations of lower RA of families and genera known to contain these species in the same study participants[28]. Moreover, due to insufficient quantities of stool from rectal swabs[82], we were unable to directly measure fecal butyrate levels in our study. Specific measures of dietary fiber intake rather than servings of fruits and vegetables would have helped elucidate relationships between dietary fiber, BPB abundance, and inflammation. Lastly, sexual preference was not matched between groups. As a result, the observed links between decreased mucosal BPB and increased inflammation need to be confirmed in a larger cohort of study participants controlling for sexual practice and diet and with measurement of fecal metabolites performed. Nevertheless, these findings suggest that strategies to increase butyrate levels, such as dietary modification or altering the microbial community through prebiotic and/or probiotic treatments could potentially reduce mucosal T cell activation, improve barrier integrity and decrease MT. The extent to which the HIV-associated mucosal pathology is reversible through dietary or microbiome manipulations of mucosal butyrate levels awaits future studies.
Supplementary Material
ACKNOWLEDGEMENTS
We wish to gratefully acknowledge all the clinical study participants as well as the physicians and staff at the University of Colorado Infectious Disease Group Practice Clinic and the University Hospital endoscopy clinic for their assistance with our clinical study. We would also like to thank Dr. Charles Robertson, Department of Medicine, University of Colorado Anschutz Medical Campus for assistance with the determination of mucosa-associated bacterial species. We acknowledge the AIDS reagent program for providing the virus stock.
This work was supported by the National Institutes of Health Grants R01 DK088663, R01 AI108404 and, in part, by NIH/NCATS Colorado CTSI Grant Number UL1 TR000154.
Footnotes
DISCLAIMERS: The authors have no disclaimers.
Authors’ contributions: SMD and JK participated equally in the conceptual design of the studies, performed experiments, analyzed the data and helped draft the manuscript; EJL processed clinical samples, performed assays and analyzed data; KG and MLS measured Butyryl-CoA CoA transferase gene expression; GA performed endoscopies; SG and ALL assisted with clinical study assays; AMD processed intestinal tissue; DNF performed bacterial species analysis of mucosal and stool samples; MDM provided access to surgical samples; CCW participated in the conceptual design of the studies and helped draft the manuscript.
REFERENCES
- 1.Brenchley JM, Price DA, Douek DC. HIV disease: fallout from a mucosal catastrophe? Nat Immunol. 2006;7:235–239. doi: 10.1038/ni1316. [DOI] [PubMed] [Google Scholar]
- 2.Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J Exp Med. 2004;200:749–759. doi: 10.1084/jem.20040874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guadalupe M, Reay E, Sankaran S, Prindiville T, Flamm J, McNeil A, et al. Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy. J Virol. 2003;77:11708–11717. doi: 10.1128/JVI.77.21.11708-11717.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehandru S, Poles MA, Tenner-Racz K, Horowitz A, Hurley A, Hogan C, et al. Primary HIV-1 infection is associated with preferential depletion of CD4+ T lymphocytes from effector sites in the gastrointestinal tract. J Exp Med. 2004;200:761–770. doi: 10.1084/jem.20041196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brenchley JM, Paiardini M, Knox KS, Asher AI, Cervasi B, Asher TE, et al. Differential Th17 CD4 T-cell depletion in pathogenic and nonpathogenic lentiviral infections. Blood. 2008;112:2826–2835. doi: 10.1182/blood-2008-05-159301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ciccone EJ, Greenwald JH, Lee PI, Biancotto A, Read SW, Yao MA, et al. CD4+ T cells, including Th17 and cycling subsets, are intact in the gut mucosa of HIV-1-infected long-term nonprogressors. J Virol. 2011;85:5880–5888. doi: 10.1128/JVI.02643-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim CJ, McKinnon LR, Kovacs C, Kandel G, Huibner S, Chege D, et al. Mucosal Th17 Cell Function Is Altered during HIV Infection and Is an Independent Predictor of Systemic Immune Activation. J Immunol. 2013;191:2164–2173. doi: 10.4049/jimmunol.1300829. [DOI] [PubMed] [Google Scholar]
- 8.Kim CJ, Nazli A, Rojas OL, Chege D, Alidina Z, Huibner S, et al. A role for mucosal IL-22 production and Th22 cells in HIV-associated mucosal immunopathogenesis. Mucosal Immunol. 2012;5:670–680. doi: 10.1038/mi.2012.72. [DOI] [PubMed] [Google Scholar]
- 9.Klatt NR, Brenchley JM. Th17 cell dynamics in HIV infection. Curr Opin HIV AIDS. 2010;5:135–140. doi: 10.1097/COH.0b013e3283364846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehandru S, Poles MA, Tenner-Racz K, Manuelli V, Jean-Pierre P, Lopez P, et al. Mechanisms of gastrointestinal CD4+ T-cell depletion during acute and early human immunodeficiency virus type 1 infection. J Virol. 2007;81:599–612. doi: 10.1128/JVI.01739-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salgado M, Rallon NI, Rodes B, Lopez M, Soriano V, Benito JM. Long-term nonprogressors display a greater number of Th17 cells than HIV-infected typical progressors. Clin Immunol. 2011;139:110–114. doi: 10.1016/j.clim.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 12.McGowan I, Elliott J, Fuerst M, Taing P, Boscardin J, Poles M, et al. Increased HIV-1 mucosal replication is associated with generalized mucosal cytokine activation. J Acquir Immune Defic Syndr. 2004;37:1228–1236. doi: 10.1097/01.qai.0000131846.12453.29. [DOI] [PubMed] [Google Scholar]
- 13.Voigt RM, Keshavarzian A, Losurdo J, Swanson G, Siewe B, Forsyth CB, et al. HIV-associated mucosal gene expression: region-specific alterations. AIDS. 2015;29:537–546. doi: 10.1097/QAD.0000000000000569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epple HJ, Allers K, Troger H, Kuhl A, Erben U, Fromm M, et al. Acute HIV infection induces mucosal infiltration with CD4+ and CD8+ T cells, epithelial apoptosis, and a mucosal barrier defect. Gastroenterology. 2010;139:1289–1300. doi: 10.1053/j.gastro.2010.06.065. [DOI] [PubMed] [Google Scholar]
- 15.Epple HJ, Schneider T, Troeger H, Kunkel D, Allers K, Moos V, et al. Impairment of the intestinal barrier is evident in untreated but absent in suppressively treated HIV-infected patients. Gut. 2009;58:220–227. doi: 10.1136/gut.2008.150425. [DOI] [PubMed] [Google Scholar]
- 16.Keating J, Bjarnason I, Somasundaram S, Macpherson A, Francis N, Price AB, et al. Intestinal absorptive capacity, intestinal permeability and jejunal histology in HIV and their relation to diarrhoea. Gut. 1995;37:623–629. doi: 10.1136/gut.37.5.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sankaran S, George MD, Reay E, Guadalupe M, Flamm J, Prindiville T, et al. Rapid onset of intestinal epithelial barrier dysfunction in primary human immunodeficiency virus infection is driven by an imbalance between immune response and mucosal repair and regeneration. J Virol. 2008;82:538–545. doi: 10.1128/JVI.01449-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Somsouk M, Estes JD, Deleage C, Dunham RM, Albright R, Inadomi JM, et al. Gut epithelial barrier and systemic inflammation during chronic HIV infection. AIDS. 2015;29:43–51. doi: 10.1097/QAD.0000000000000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–1371. doi: 10.1038/nm1511. [DOI] [PubMed] [Google Scholar]
- 20.Marchetti G, Cozzi-Lepri A, Merlini E, Bellistri GM, Castagna A, Galli M, et al. Microbial translocation predicts disease progression of HIV-infected antiretroviral-naive patients with high CD4+ cell count. AIDS. 2011;25:1385–1394. doi: 10.1097/QAD.0b013e3283471d10. [DOI] [PubMed] [Google Scholar]
- 21.Marchetti G, Tincati C, Silvestri G. Microbial translocation in the pathogenesis of HIV infection and AIDS. Clin Microbiol Rev. 2013;26:2–18. doi: 10.1128/CMR.00050-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zevin AS, McKinnon L, Burgener A, Klatt NR. Microbial translocation and microbiome dysbiosis in HIV-associated immune activation. Curr Opin HIV AIDS. 2016;11:182–190. doi: 10.1097/COH.0000000000000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaiko GE, Stappenbeck TS. Host-microbe interactions shaping the gastrointestinal environment. Trends Immunol. 2014;35:538–548. doi: 10.1016/j.it.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brestoff JR, Artis D. Commensal bacteria at the interface of host metabolism and the immune system. Nat Immunol. 2013;14:676–684. doi: 10.1038/ni.2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474:327–336. doi: 10.1038/nature10213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rooks MG, Garrett WS. Gut microbiota, metabolites and host immunity. Nat Rev Immunol. 2016;16:341–352. doi: 10.1038/nri.2016.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol. 2009;9:313–323. doi: 10.1038/nri2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dillon SM, Lee EJ, Kotter CV, Austin GL, Dong Z, Hecht DK, et al. An altered intestinal mucosal microbiome in HIV-1 infection is associated with mucosal and systemic immune activation and endotoxemia. Mucosal Immunol. 2014;7:983–994. doi: 10.1038/mi.2013.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dillon SM, Lee EJ, Kotter CV, Austin GL, Gianella S, Siewe B, et al. Gut dendritic cell activation links an altered colonic microbiome to mucosal and systemic T-cell activation in untreated HIV-1 infection. Mucosal Immunol. 2016;9:24–37. doi: 10.1038/mi.2015.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dinh DM, Volpe GE, Duffalo C, Bhalchandra S, Tai AK, Kane AV, et al. Intestinal microbiota, microbial translocation, and systemic inflammation in chronic HIV infection. J Infect Dis. 2015;211:19–27. doi: 10.1093/infdis/jiu409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellis CL, Ma ZM, Mann SK, Li CS, Wu J, Knight TH, et al. Molecular characterization of stool microbiota in HIV-infected subjects by panbacterial and order-level 16S ribosomal DNA (rDNA) quantification and correlations with immune activation. J Acquir Immune Defic Syndr. 2011;57:363–370. doi: 10.1097/QAI.0b013e31821a603c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gori A, Tincati C, Rizzardini G, Torti C, Quirino T, Haarman M, et al. Early impairment of gut function and gut flora supporting a role for alteration of gastrointestinal mucosa in human immunodeficiency virus pathogenesis. J Clin Microbiol. 2008;46:757–758. doi: 10.1128/JCM.01729-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lozupone CA, Li M, Campbell TB, Flores SC, Linderman D, Gebert MJ, et al. Alterations in the gut microbiota associated with HIV-1 infection. Cell Host Microbe. 2013;14:329–339. doi: 10.1016/j.chom.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lozupone CA, Rhodes ME, Neff CP, Fontenot AP, Campbell TB, Palmer BE. HIV-induced alteration in gut microbiota: driving factors, consequences, and effects of antiretroviral therapy. Gut Microbes. 2014;5:562–570. doi: 10.4161/gmic.32132. [DOI] [PubMed] [Google Scholar]
- 35.McHardy IH, Li X, Tong M, Ruegger P, Jacobs J, Borneman J, et al. HIV infection is associated with compositional and functional shifts in the rectal mucosal microbiota. Microbiome. 2013;1:26. doi: 10.1186/2049-2618-1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mutlu EA, Keshavarzian A, Losurdo J, Swanson G, Siewe B, Forsyth C, et al. A compositional look at the human gastrointestinal microbiome and immune activation parameters in HIV infected subjects. PLoS Pathog. 2014;10:e1003829. doi: 10.1371/journal.ppat.1003829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nowak P, Troseid M, Avershina E, Barqasho B, Neogi U, Holm K, et al. Gut microbiota diversity predicts immune status in HIV-1 infection. AIDS. 2015;29:2409–2418. doi: 10.1097/QAD.0000000000000869. [DOI] [PubMed] [Google Scholar]
- 38.Perez-Santiago J, Gianella S, Massanella M, Spina CA, Karris MY, Var SR, et al. Gut Lactobacillales are associated with higher CD4 and less microbial translocation during HIV infection. AIDS. 2013;27:1921–1931. doi: 10.1097/qad.0b013e3283611816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vazquez-Castellanos JF, Serrano-Villar S, Latorre A, Artacho A, Ferrus ML, Madrid N, et al. Altered metabolism of gut microbiota contributes to chronic immune activation in HIV-infected individuals. Mucosal Immunol. 2014 doi: 10.1038/mi.2014.107. [DOI] [PubMed] [Google Scholar]
- 40.Vujkovic-Cvijin I, Dunham RM, Iwai S, Maher MC, Albright RG, Broadhurst MJ, et al. Dysbiosis of the Gut Microbiota Is Associated with HIV Disease Progression and Tryptophan Catabolism. Sci Transl Med. 2013;5:193ra191. doi: 10.1126/scitranslmed.3006438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang L, Poles MA, Fisch GS, Ma Y, Nossa C, Phelan JA, et al. HIV-induced immunosuppression is associated with colonization of the proximal gut by environmental bacteria. AIDS. 2016;30:19–29. doi: 10.1097/QAD.0000000000000935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Noguera-Julian M, Rocafort M, Guillén Y, Rivera J, Casadellà M, Nowak P, et al. Gut Microbiota Linked to Sexual Preference and HIV Infection. EBioMedicine. 2016 doi: 10.1016/j.ebiom.2016.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dillon SM, Lee EJ, Donovan AM, Guo K, Harper MS, Frank DN, et al. Enhancement of HIV-1 infection and intestinal CD4+ T cell depletion ex vivo by gut microbes altered during chronic HIV-1 infection. Retrovirology. 2016;13:5. doi: 10.1186/s12977-016-0237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee WJ, Hase K. Gut microbiota-generated metabolites in animal health and disease. Nat Chem Biol. 2014;10:416–424. doi: 10.1038/nchembio.1535. [DOI] [PubMed] [Google Scholar]
- 45.Louis P, Flint HJ. Diversity, metabolism and microbial ecology of butyrate-producing bacteria from the human large intestine. FEMS Microbiol Lett. 2009;294:1–8. doi: 10.1111/j.1574-6968.2009.01514.x. [DOI] [PubMed] [Google Scholar]
- 46.Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer RJ. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. 2008;27:104–119. doi: 10.1111/j.1365-2036.2007.03562.x. [DOI] [PubMed] [Google Scholar]
- 47.Segain JP, Raingeard de la Bletiere D, Bourreille A, Leray V, Gervois N, Rosales C, et al. Butyrate inhibits inflammatory responses through NFkappaB inhibition: implications for Crohn's disease. Gut. 2000;47:397–403. doi: 10.1136/gut.47.3.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Frank DN, Robertson CE, Hamm CM, Kpadeh Z, Zhang T, Chen H, et al. Disease phenotype and genotype are associated with shifts in intestinal-associated microbiota in inflammatory bowel diseases. Inflamm Bowel Dis. 2011;17:179–184. doi: 10.1002/ibd.21339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104:13780–13785. doi: 10.1073/pnas.0706625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li E, Hamm CM, Gulati AS, Sartor RB, Chen H, Wu X, et al. Inflammatory bowel diseases phenotype, C. difficile and NOD2 genotype are associated with shifts in human ileum associated microbial composition. PLoS One. 2012;7:e26284. doi: 10.1371/journal.pone.0026284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Son JS, Khair S, Pettet DW, 3rd, Ouyang N, Tian X, Zhang Y, et al. Altered Interactions between the Gut Microbiome and Colonic Mucosa Precede Polyposis in APCMin/+ Mice. PLoS One. 2015;10:e0127985. doi: 10.1371/journal.pone.0127985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Furusawa Y, Obata Y, Fukuda S, Endo TA, Nakato G, Takahashi D, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504:446–450. doi: 10.1038/nature12721. [DOI] [PubMed] [Google Scholar]
- 53.Singh N, Gurav A, Sivaprakasam S, Brady E, Padia R, Shi H, et al. Activation of Gpr109a, receptor for niacin and the commensal metabolite butyrate, suppresses colonic inflammation and carcinogenesis. Immunity. 2014;40:128–139. doi: 10.1016/j.immuni.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Atarashi K, Tanoue T, Shima T, Imaoka A, Kuwahara T, Momose Y, et al. Induction of colonic regulatory T cells by indigenous Clostridium species. Science. 2011;331:337–341. doi: 10.1126/science.1198469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bailon E, Cueto-Sola M, Utrilla P, Rodriguez-Cabezas ME, Garrido-Mesa N, Zarzuelo A, et al. Butyrate in vitro immune-modulatory effects might be mediated through a proliferation-related induction of apoptosis. Immunobiology. 2010;215:863–873. doi: 10.1016/j.imbio.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 56.Chang PV, Hao L, Offermanns S, Medzhitov R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc Natl Acad Sci U S A. 2014;111:2247–2252. doi: 10.1073/pnas.1322269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saemann MD, Bohmig GA, Osterreicher CH, Burtscher H, Parolini O, Diakos C, et al. Anti-inflammatory effects of sodium butyrate on human monocytes: potent inhibition of IL-12 and up-regulation of IL-10 production. FASEB J. 2000;14:2380–2382. doi: 10.1096/fj.00-0359fje. [DOI] [PubMed] [Google Scholar]
- 58.Hague A, Butt AJ, Paraskeva C. The role of butyrate in human colonic epithelial cells: an energy source or inducer of differentiation and apoptosis? Proc Nutr Soc. 1996;55:937–943. doi: 10.1079/pns19960090. [DOI] [PubMed] [Google Scholar]
- 59.Lewis K, Lutgendorff F, Phan V, Soderholm JD, Sherman PM, McKay DM. Enhanced translocation of bacteria across metabolically stressed epithelia is reduced by butyrate. Inflamm Bowel Dis. 2010;16:1138–1148. doi: 10.1002/ibd.21177. [DOI] [PubMed] [Google Scholar]
- 60.Ploger S, Stumpff F, Penner GB, Schulzke JD, Gabel G, Martens H, et al. Microbial butyrate and its role for barrier function in the gastrointestinal tract. Ann N Y Acad Sci. 2012;1258:52–59. doi: 10.1111/j.1749-6632.2012.06553.x. [DOI] [PubMed] [Google Scholar]
- 61.Kelly CJ, Zheng L, Campbell EL, Saeedi B, Scholz CC, Bayless AJ, et al. Crosstalk between Microbiota-Derived Short-Chain Fatty Acids and Intestinal Epithelial HIF Augments Tissue Barrier Function. Cell Host Microbe. 2015;17:662–671. doi: 10.1016/j.chom.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quast C, Pruesse E, Yilmaz P, Gerken J, Schweer T, Yarza P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590–596. doi: 10.1093/nar/gks1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pruesse E, Peplies J, Glockner FO. SINA: accurate high-throughput multiple sequence alignment of ribosomal RNA genes. Bioinformatics. 2012;28:1823–1829. doi: 10.1093/bioinformatics/bts252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Steele AK, Lee EJ, Manuzak JA, Dillon SM, Beckham JD, McCarter MD, et al. Microbial exposure alters HIV-1-induced mucosal CD4+ T cell death pathways Ex vivo. Retrovirology. 2014;11:14. doi: 10.1186/1742-4690-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dillon SM, Manuzak JA, Leone AK, Lee EJ, Rogers LM, McCarter MD, et al. HIV-1 infection of human intestinal lamina propria CD4+ T cells in vitro is enhanced by exposure to commensal Escherichia coli. J Immunol. 2012;189:885–896. doi: 10.4049/jimmunol.1200681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dillon SM, Rogers LM, Howe R, Hostetler LA, Buhrman J, McCarter MD, et al. Human intestinal lamina propria CD1c+ dendritic cells display an activated phenotype at steady state and produce IL-23 in response to TLR7/8 stimulation. J Immunol. 2010;184:6612–6621. doi: 10.4049/jimmunol.1000041. [DOI] [PubMed] [Google Scholar]
- 67.Howe R, Dillon S, Rogers L, McCarter M, Kelly C, Gonzalez R, et al. Evidence for dendritic cell-dependent CD4(+) T helper-1 type responses to commensal bacteria in normal human intestinal lamina propria. Clin Immunol. 2009;131:317–332. doi: 10.1016/j.clim.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Louis P, Duncan SH, McCrae SI, Millar J, Jackson MS, Flint HJ. Restricted distribution of the butyrate kinase pathway among butyrate-producing bacteria from the human colon. J Bacteriol. 2004;186:2099–2106. doi: 10.1128/JB.186.7.2099-2106.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gibson PR, Rosella O, Wilson AJ, Mariadason JM, Rickard K, Byron K, et al. Colonic epithelial cell activation and the paradoxical effects of butyrate. Carcinogenesis. 1999;20:539–544. doi: 10.1093/carcin/20.4.539. [DOI] [PubMed] [Google Scholar]
- 70.Zimmerman MA, Singh N, Martin PM, Thangaraju M, Ganapathy V, Waller JL, et al. Butyrate suppresses colonic inflammation through HDAC1-dependent Fas upregulation and Fas-mediated apoptosis of T cells. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1405–1415. doi: 10.1152/ajpgi.00543.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boets E, Deroover L, Houben E, Vermeulen K, Gomand SV, Delcour JA, et al. Quantification of in Vivo Colonic Short Chain Fatty Acid Production from Inulin. Nutrients. 2015;7:8916–8929. doi: 10.3390/nu7115440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kleessen B, Hartmann L, Blaut M. Oligofructose and long-chain inulin: influence on the gut microbial ecology of rats associated with a human faecal flora. Br J Nutr. 2001;86:291–300. doi: 10.1079/bjn2001403. [DOI] [PubMed] [Google Scholar]
- 73.Pouteau E, Nguyen P, Ballevre O, Krempf M. Production rates and metabolism of short-chain fatty acids in the colon and whole body using stable isotopes. Proc Nutr Soc. 2003;62:87–93. doi: 10.1079/PNS2003208. [DOI] [PubMed] [Google Scholar]
- 74.Wang HB, Wang PY, Wang X, Wan YL, Liu YC. Butyrate enhances intestinal epithelial barrier function via up-regulation of tight junction protein Claudin-1 transcription. Dig Dis Sci. 2012;57:3126–3135. doi: 10.1007/s10620-012-2259-4. [DOI] [PubMed] [Google Scholar]
- 75.Rosignoli P, Fabiani R, De Bartolomeo A, Spinozzi F, Agea E, Pelli MA, et al. Protective activity of butyrate on hydrogen peroxide-induced DNA damage in isolated human colonocytes and HT29 tumour cells. Carcinogenesis. 2001;22:1675–1680. doi: 10.1093/carcin/22.10.1675. [DOI] [PubMed] [Google Scholar]
- 76.Canani RB, Costanzo MD, Leone L, Pedata M, Meli R, Calignano A. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol. 2011;17:1519–1528. doi: 10.3748/wjg.v17.i12.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Douek DC, Brenchley JM, Betts MR, Ambrozak DR, Hill BJ, Okamoto Y, et al. HIV preferentially infects HIV-specific CD4+ T cells. Nature. 2002;417:95–98. doi: 10.1038/417095a. [DOI] [PubMed] [Google Scholar]
- 78.Stevenson M, Stanwick TL, Dempsey MP, Lamonica CA. HIV-1 replication is controlled at the level of T cell activation and proviral integration. EMBO J. 1990;9:1551–1560. doi: 10.1002/j.1460-2075.1990.tb08274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Demonte D, Quivy V, Colette Y, Van Lint C. Administration of HDAC inhibitors to reactivate HIV-1 expression in latent cellular reservoirs: implications for the development of therapeutic strategies. Biochem Pharmacol. 2004;68:1231–1238. doi: 10.1016/j.bcp.2004.05.040. [DOI] [PubMed] [Google Scholar]
- 80.Imai K, Ochiai K, Okamoto T. Reactivation of latent HIV-1 infection by the periodontopathic bacterium Porphyromonas gingivalis involves histone modification. J Immunol. 2009;182:3688–3695. doi: 10.4049/jimmunol.0802906. [DOI] [PubMed] [Google Scholar]
- 81.Imai K, Yamada K, Tamura M, Ochiai K, Okamoto T. Reactivation of latent HIV-1 by a wide variety of butyric acid-producing bacteria. Cell Mol Life Sci. 2012;69:2583–2592. doi: 10.1007/s00018-012-0936-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rose DJ, Venema K, Keshavarzian A, Hamaker BR. Starch-entrapped microspheres show a beneficial fermentation profile and decrease in potentially harmful bacteria during in vitro fermentation in faecal microbiota obtained from patients with inflammatory bowel disease. Br J Nutr. 2010;103:1514–1524. doi: 10.1017/S0007114509993515. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.