Abstract
Background
Coffee and tea are two of the most commonly consumed beverages in the world. The association of coffee and tea intake with coronary artery calcium and major adverse cardiovascular events remains uncertain.
Methods
We examined 6,508 ethnically-diverse participants with available coffee and tea data from the Multi-Ethnic Study of Atherosclerosis. Intake for each was classified as never, occasional (<1 cup/day), and regular (≥1 cup/day). A coronary artery calcium progression ratio was derived from mixed effect regression models using loge(calcium score+1) as the outcome with coefficients exponentiated to reflect coronary artery calcium progression ratio vs. the reference. Cox proportional hazards analyses were used to evaluate the association between beverage intake and incident cardiovascular events.
Results
Over a median follow-up of 5.3 years for coronary artery calcium and 11.1 years for cardiovascular events, participants who regularly drank tea (≥1 cup/day) had a slower progression of coronary artery calcium compared with never drinkers after multivariable adjustment. This correlated with a statistically significant lower incidence of cardiovascular events for ≥1 cup/day tea drinkers (adjusted HR 0.71; 95% CI 0.53–0.95). Compared to never coffee drinkers, regular coffee intake (≥1 cup/day) was not statistically associated with coronary artery calcium progression or cardiovascular events (adjusted HR 0.97 [0.78, 1.20]). Caffeine intake was marginally inversely associated with coronary artery calcium progression.
Conclusions
Moderate tea drinkers had slower progression of coronary artery calcium and reduced risk for cardiovascular events. Future research is needed to understand the potentially protective nature of moderate tea intake.
Keywords: Cardiovascular events, Coffee, Tea, Caffeine, Coronary artery calcium
Introduction
Coffee and tea are two of the most commonly consumed beverages in the world.1 Caffeine, the most studied active compound in coffee and tea, has well-known short-term cardiovascular effects, including increased plasma renin levels, peripheral vasoconstriction, increased blood pressure, and cardiac arrhythmias.2–5 Despite these effects, coffee intake is associated with a lower incidence of diabetes and favorable effects on endothelial function.6,7 The association of coffee and tea intake with clinical cardiovascular outcomes, however, is still controversial. A recent meta-analysis of cohort studies found that moderate coffee intake was associated with lower cardiovascular disease risk,8 but a previous meta-analysis did not find such association.9 There are also conflicting data on the associations between coffee and tea intake with coronary artery calcification, a measure of subclinical atherosclerosis.10–12
Research in this field is challenging due to potential confounding of coffee and tea consumption with demographic and other nutritional variables. Associations with clinical outcomes may be due to coffee or tea intake itself, to what is added or eaten with these beverages, or related to socioeconomic factors. Therefore, in assessing the cardiovascular implications of coffee and tea intake, it is critical to study a diverse population with sociodemographic and clinical characteristics. Moreover, simultaneously assessing the underlying disease (subclinical atherosclerosis) as well as the cardiovascular events themselves in a single large prospective cohort study may support a casual association. In the Multi-Ethnic Study of Atherosclerosis (MESA), we sought to investigate the association between coffee and tea intake with coronary artery calcium prevalence, progression, and cardiovascular events.
Methods
Study Population
MESA is a prospective study that investigates the prevalence, risk factors, and progression of subclinical cardiovascular disease.13 MESA is a population-based sample of 6,814 men and women aged 44–84 years selected from 6 field centers (Columbia University; Johns Hopkins University; Northwestern University; University of California-Los Angeles; University of Minnesota; and Wake Forest University). We excluded participants with a history of cardiovascular disease at baseline (n=25) and participants who missed data on coffee, tea and caffeine intake (n=281). The final study sample included 6,508 participants. The institutional review boards approved this study at all sites and written informed consent was obtained from all participants.
Coffee, tea, caffeine, and other dietary information
At MESA Exam 1 (2000–2002), participants completed a 120-item food frequency questionnaire adapted from the Insulin Resistance Atherosclerosis Study and validated in White, African-American, and Hispanic persons.14,15 It was modified to include usual foods eaten by individuals of Chinese decent.13 Participants reported the frequency of coffee (caffeinated and decaffeinated were not differentiated) and black or green tea (included together) intake as never, 1–3/month, 1/week, 2–3/week, 5–6/week, 1/day, 2–3/day, 4–5/day, or ≥6 cups/day. Caffeine intake was calculated as milligrams/day from the total of all caffeinated beverages (not just coffee and tea) and food. Total fat, carbohydrates, red meat, vegetables, alcohol consumption, and fruit were quantified in grams/day.
For further details on Dietary Information, Covariates, and Computed Tomography, please see the online Supplemental Methods.
Clinical Events
Events were obtained by follow-up telephone interviews by trained personnel conducted every 9–12 months. Interviewers inquired about interim hospitalizations, cardiovascular diagnoses, procedures, and death. Of the 92% of living participants who completed interviews, obtained medical records for hospital admissions and outpatient diagnoses were 98% and 95%, respectively. Incident cardiovascular disease was defined as myocardial infarction, angina resulting in revascularization, resuscitated cardiac arrest, stroke, and cardiovascular death. “Hard” cardiovascular events included incident cardiovascular events except angina resulting in revascularization. Further details on MESA event adjudication, conducted by a committee of physicians, are available at http://www.mesa-nhlbi.org.
Statistical Analysis
We conducted three types of analyses for the association between coffee, tea, or caffeine intake collected at MESA Exam 1 with subclinical or clinical outcomes: cross-sectional analysis evaluating prevalent coronary artery calcium scores at MESA Exam 1; longitudinal analysis evaluating the change in coronary artery calcium scores from Exam 1 to Exam 5; and survival analysis evaluating incident cardiovascular events identified through the last MESA adjudication in 2013. Daily coffee and tea intake were categorized into none, <1 cup (occasional), and ≥1 cup (regular), and caffeine intake was categorized into tertiles. In addition to categorical analysis, we modeled coffee, tea and caffeine intake as continuous variables using restricted cubic splines (with knots at the none, 5–6 cups/week, 1 cup/day, and 2–3 cups/day for coffee and tea, and at the 5th, 35th, 65th and 95th percentiles of the caffeine intake distribution) to provide a flexible dose-response relationship.
For cross-sectional analyses, coronary artery calcium score was grouped into 3 categories (0, 1–99, and ≥100). We used multinomial logistic regression to calculate multivariable-adjusted prevalence ratios and 95% confidence intervals for coronary artery calcium score 1–99 and coronary artery calcium score ≥100 comparing each category of coffee/tea intake to the group with no consumption, and tertile 2 and 3 to the 1st tertile of caffeine intake.
For longitudinal analyses of the association between coffee, tea, and caffeine intake with the change in coronary artery calcium score from Exam 1 through Exam 5, we modeled loge(calcium score+1) using mixed effect models allowing for random variations in baseline coronary artery calcium scores and longitudinal slope for coronary artery calcium score progression across participants.19 Coronary artery calcium scores were log-transformed since the distribution of coronary artery calcium scores was markedly right skewed, and the coefficients from the mixed effect models using log-transformed outcomes were exponentiated to reflect coronary artery calcium progression ratio.
Finally, for survival analyses we used Cox proportional hazards models to estimate the hazard ratios (95% confidence intervals) for incident cardiovascular events associated with coffee, tea, and caffeine intake. Study participants contributed follow-up time from Exam 1 until the date of incident cardiovascular event, death, loss-to-follow-up, or study close out on December 31st, 2013.
We used four models with progressive degrees of adjustment to account for potential confounding factors. Model 1 adjusted for age, sex, race/ethnicity, education, and number of follow-up years. Model 2 was further adjusted for possible lifestyle confounders, including smoking, physical activity, alcohol consumption, and intake of total fat, fruits, vegetables, and red meat. Model 3 was further adjusted for body mass index, systolic and diastolic blood pressure, use of antihypertensive medications, total cholesterol, high-density lipoprotein cholesterol, triglycerides, lipid-lowering medications, diabetes, diabetes medications, and family history of coronary heart disease disease. Model 4 was further adjusted for C-reactive protein and fibrinogen.
We conducted several sensitivity analyses. First, in the longitudinal analyses, we excluded participants with 0 coronary artery calcium score at baseline given their different score trajectories. Second, we excluded Chinese participants given higher tea intake and lower incidence of events compared to other race/ethnicity groups. Finally, we used hard cardiovascular events excluding angina resulting in revascularization as endpoint. For all analyses, a two-sided p value <0.05 was considered statistically significant. All analyses were performed using STATA version 12 (StataCorp LP, College Station, Texas).
Results
Baseline participant demographics, cardiovascular risk factors, and dietary characteristics overall and stratified by coronary artery calcium presence or absence at baseline are shown in Table 1. The average age was 62.3 years, and included 52.9% women. The percentage of participants drinking 0, <1, and ≥1 cups/day of coffee were 25.0%, 24.0%, and 50.9%, respectively. More than half of the participants (57.6%) reported never drinking tea, whereas 29.5% reported <1 cup/day and 12.9% drank ≥1 cup/day. Coffee and tea consumption stratified by ethnicity are shown in Table 2. The prevalence of coronary artery calcium 0, 1–99, and ≥100 was 49.9%, 26.5%, and 23.6%, respectively. Over a median follow-up of 11.1 years, the incidence of all cardiovascular events and hard cardiovascular events was 10.8 and 7.5 per 1000 person-years, respectively.
Table 1.
Characteristics of study population overall and stratified by coronary artery calcium presence at enrollment
| Overall | No CAC | CAC > 0 | p-value | |
|---|---|---|---|---|
| N | 6,508 | 3,249 | 3,259 | |
| Age, years | 62.2 ± 10.2 | 58.0 ± 9.1 | 66.4 ± 9.5 | <0.001 |
| Male | 3,083 (47.4) | 1,200 (36.9) | 1,883 (57.8) | <0.001 |
| Daily coffee consumption | <0.001 | |||
| Never | 1,554 (25.0) | 833 (27.0) | 721 (23.1) | |
| <1 cup | 1,492 (24.0) | 768 (24.9) | 724 (23.2) | |
| ≥1 cup | 3,159 (50.9) | 1,483 (48.1) | 1,676 (53.7) | |
| Tea | 0.06 | |||
| Never | 3,562 (57.6) | 1,722 (56.1) | 1,840 (59.1) | |
| <1 cup | 1,825 (29.5) | 939 (30.6) | 886 (28.4) | |
| ≥1 cup | 800 (12.9) | 411 (13.4) | 389 (12.5) | |
| Caffeine consumption, mg/day** | 116.6 (32.2 – 254.1) | 110.6 (30.2 – 244.8) | 124.1 (34.2 – 278.1) | 0.18 |
| Race | <0.001 | |||
| White | 2,540 (39.0) | 1,096 (33.7) | 1,444 (44.3) | |
| Chinese-American | 801 (12.3) | 399 (12.3) | 402 (12.3) | |
| Black | 1,742 (26.8) | 981 (30.2) | 761 (23.4) | |
| Hispanic | 1,425 (21.9) | 773 (23.8) | 652 (20.0) | |
| Education | 0.20 | |||
| <High school | 1,165 (17.9) | 560 (17.3) | 605 (18.6) | |
| High school or equivalent | 3,007 (46.3) | 1,493 (46.0) | 1,514 (46.5) | |
| College, graduate or professional school | 2,328 (35.8) | 1,192 (36.7) | 1,136 (34.9) | |
| Smoking | <0.001 | |||
| Never | 3,289 (50.6) | 1,822 (56.1) | 1,467 (45.1) | |
| Former | 2,395 (36.8) | 1,010 (31.1) | 1,385 (42.5) | |
| Current | 817 (12.6) | 413 (12.7) | 404 (12.4) | |
| Diabetes | 810 (12.5) | 296 (9.1) | 514 (15.8) | <0.001 |
| Diabetes medication | 628 (9.6) | 224 (6.9) | 404 (12.4) | <0.001 |
| Family history of coronary heart disease | 2,607 (42.7) | 1,144 (37.2) | 1,463 (48.2) | <0.001 |
| Antihypertensive medication | 2,421 (37.2) | 925 (28.5) | 1,496 (45.9) | <0.001 |
| Lipid lowering medication | 1,067 (16.4) | 349 (10.8) | 718 (22.1) | <0.001 |
| Weekly alcohol (number of drinks) | 2.3 ± 5.3 | 2.0 ± 4.9 | 2.6 ± 5.6 | <0.001 |
| Body mass index, kg/m2 | 28.2 ± 5.4 | 28.2 ± 5.6 | 28.3 ± 5.3 | 0.46 |
| Systolic blood pressure, mm Hg | 126.5 ± 21.4 | 122.2 ± 20.3 | 130.8 ± 21.7 | <0.001 |
| Diastolic blood pressure, mm Hg | 71.9 ± 10.2 | 71.2 ± 10.2 | 72.6 ± 10.2 | <0.001 |
| Total cholesterol, mg/dl | 194.1 ± 35.7 | 193.8 ± 34.8 | 194.5 ± 36.5 | 0.39 |
| High-density lipoprotein cholesterol, mg/dl | 51.0 ± 14.9 | 52.6 ± 15.1 | 49.5 ± 14.5 | <0.001 |
| Low-density lipoprotein cholesterol, mg/dl | 117.1 ± 31.3 | 116.0 ± 30.5 | 118.3 ± 32.1 | <0.01 |
| Triglyceride, mg/dl | 131.4 ± 86.7 | 126.7 ± 81.5 | 136.1 ± 91.4 | <0.001 |
| eGFR, CKD-EPI equation mL/min/1.73 m2 | 78.0 ± 16.3 | 81.4 ± 15.3 | 74.5 ± 16.5 | <0.001 |
| Fibrinogen, mg/dl | 346.1 ± 73.6 | 338.8 ± 70.6 | 353.3 ± 75.7 | <0.001 |
| Dietary consumption | ||||
| Total fat, g/day | 56.5 ± 35.9 | 57.8 ± 37.7 | 55.1 ± 33.9 | <0.01 |
| Total carbohydrates, g/day | 215.2 ± 114.2 | 218.0 ± 118.3 | 212.4 ± 110.1 | 0.05 |
| Red meat, g/day | 0.4 ± 0.4 | 0.4 ± 0.4 | 0.4 ± 0.4 | <0.001 |
| Green leafy vegetables, g/day | 0.1 ± 0.2 | 0.1 ± 0.2 | 0.1 ± 0.2 | 0.03 |
| Fruit, g/day | 1.8 ± 1.5 | 1.8 ± 1.6 | 1.9 ± 1.5 | 0.33 |
| Total intentional exercise, met-min/week** | 840.0 (123.8 – 2043.8) | 750.0 (105.0 – 1920.0) | 900.0 (157.5 – 2100.0) | 0.01 |
| C-reactive protein, mg/l** | 1.9 (0.8 – 4.2) | 1.9 (0.8 – 4.2) | 1.9 (0.8 – 4.1) | 0.93 |
data are mean ± SD or number(%)
data are median (IQR)
Table 2.
Race/ethnicity distribution by tea and coffee consumption
| Coffee | |||
|---|---|---|---|
| None | <1 cup | ≥ 1 cups | |
| White | 417 (26.8%) | 420 (28.2%) | 1,626 (51.5%) |
| Chinese-American | 361 (23.2%) | 240 (16.1%) | 187 (6.0%) |
| Black | 502 (32.3%) | 510 (34.2%) | 589 (18.6%) |
| Hispanic | 274 (17.6%) | 322 (21.6%) | 757 (24.0%) |
| Tea | |||
| None | <1 cup | ≥ 1 cup | |
| White | 1,335 (37.5%) | 816 (44.7%) | 304 (38.0%) |
| Chinese-American | 231 (6.5%) | 276 (15.1%) | 281 (35.1%) |
| Black | 950 (26.7%) | 491 (26.9%) | 152 (19.0%) |
| Hispanic | 1,046 (29.4%) | 242 (13.3%) | 63 (7.9%) |
Coffee/Tea Intake and Coronary Artery Calcium
Participants who drank ≥1 cup/day of coffee had a greater prevalence of coronary artery calcium scores ≥100 compared to those who did not drink coffee in the model adjusted for demographic covariates (Table 3). This relationship was attenuated with multivariable adjustment (RR: 1.10 [CI: 0.89–1.35]). In fully-adjusted multivariable models, however, participants who drank ≥1 cup/day of tea had a lower prevalence of coronary artery calcium scores ≥100 compared to those who did not drink tea (0.64 [0.49–0.84]). For caffeine intake, participants in the 2nd tertile of caffeine intake were less likely to have coronary artery calcium presence ≥100 (0.81 [0.66–1.00]) compared to the 1st quintile (Figure 1).
Table 3.
Relative risk ratios* (95% CIs) for prevalent coronary artery calcium by categories of coffee, tea, and caffeine consumption
| Daily coffee consumption | |||
|---|---|---|---|
| None (n=1,554) | <1 cup (n=1,492) | ≥1 cup (n=3,159) | |
| CAC score 1 – 99 | |||
| No. of cases | 415 | 389 | 831 |
| Model 1 | 1.00 | 1.07 (0.89, 1.28) | 1.04 (0.88, 1.22) |
| Model 2 | 1.00 | 1.06 (0.88, 1.28) | 1.01 (0.85, 1.19) |
| Model 3 | 1.00 | 1.06 (0.87, 1.28) | 1.01 (0.85, 1.20) |
| Model 4 | 1.00 | 1.07 (0.88, 1.30) | 1.02 (0.85, 1.21) |
| CAC score ≥ 100 | |||
| No. of cases | 306 | 335 | 845 |
| Model 1 | 1.00 | 1.22 (0.99, 1.51) | 1.25 (1.04, 1.51) |
| Model 2 | 1.00 | 1.21 (0.96, 1.51) | 1.10 (0.90, 1.35) |
| Model 3 | 1.00 | 1.16 (0.92, 1.47) | 1.11 (0.90, 1.36) |
| Model 4 | 1.00 | 1.18 (0.93, 1.49) | 1.10 (0.89, 1.35) |
| Daily tea consumption | |||
| None (n=3,562) | <1 cup (n=1,825) | 1 cup (n=800) | |
| CAC score 1 – 99 | |||
| No. of cases | 945 | 455 | 230 |
| Model 1 | 1.00 | 0.93 (0.80, 1.08) | 0.89 (0.73, 1.09) |
| Model 2 | 1.00 | 0.94 (0.81, 1.10) | 0.91 (0.74, 1.13) |
| Model 3 | 1.00 | 0.96 (0.82, 1.13) | 0.91 (0.73, 1.13) |
| Model 4 | 1.00 | 0.96 (0.81, 1.12) | 0.90 (0.73, 1.12) |
| CAC score ≥ 100 | |||
| No. of cases | 895 | 431 | 159 |
| Model 1 | 1.00 | 0.96 (0.81, 1.14) | 0.65 (0.51, 0.83) |
| Model 2 | 1.00 | 1.01 (0.85, 1.21) | 0.66 (0.51, 0.85) |
| Model 3 | 1.00 | 1.04 (0.86, 1.24) | 0.65 (0.50, 0.84) |
| Model 4 | 1.00 | 1.03 (0.86, 1.24) | 0.64 (0.49, 0.84) |
| Caffeine consumption (mg/day) | |||
| 1st Tertile (<55) | 2nd Tertile (55–<167) | 3rd Tertile (167–1354) | |
| CAC score 1 – 99 | |||
| No. of cases | 581 | 590 | 555 |
| Model 1 | 1.00 | 1.02 (0.88, 1.19) | 0.96 (0.81, 1.12) |
| Model 2 | 1.00 | 1.02 (0.86, 1.20) | 0.92 (0.76, 1.10) |
| Model 3 | 1.00 | 1.00 (0.85, 1.19) | 0.89 (0.74, 1.06) |
| Model 4 | 1.00 | 0.99 (0.84, 1.18) | 0.89 (0.74, 1.07) |
| CAC score ≥ 100 | |||
| No. of cases | 480 | 514 | 539 |
| Model 1 | 1.00 | 0.99 (0.83, 1.18) | 1.04 (0.86, 1.25) |
| Model 2 | 1.00 | 0.87 (0.71, 1.06) | 0.86 (0.70, 1.06) |
| Model 3 | 1.00 | 0.83 (0.68, 1.01) | 0.83 (0.67, 1.02) |
| Model 4 | 1.00 | 0.81 (0.66, 1.00) | 0.82 (0.66, 1.01) |
Relative risk ratios were derived from multinomial logistic regression.
Model 1: age, sex, race/ethnicity, and education.
Model 2: model 1 + smoking (never, former, current), physical activity, total fat, alcohol consumption, fruits quartiles, vegetables quartiles, red meat quartiles
Model 3: model 2 + systolic and diastolic blood pressures, use of antihypertensive medications, lipid-lowering medications, diabetes medications, body mass index, family history of coronary heart disease, diabetes, high-density lipoprotein cholesterol, total cholesterol, triglyceride
Model 4: model 3 + C-reactive protein, and fibrinogen
Figure 1.
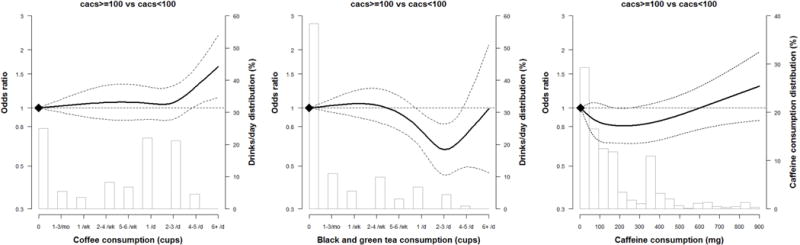
Odds ratio of coronary artery calcium scores (CAC score ≥100) by coffee, tea and caffeine consumption.
The curves represent the adjusted OR of CAC scores ≥100 Agatston unit) and coffee/tea/caffeine consumption. The reference values (diamond dots) were set at 0 drink per day. The dose response association was estimated by using a linear and a cubic spline term for coffee/tea consumption in the multivariable logistic regression.
The model adjusted for age, sex, race/ethnicity, education, smoking (never, former, current), physical activity, total fat, alcohol consumption, fruits quartiles, vegetables quartiles, red meat quartiles, systolic and diastolic blood pressures, use of antihypertensive medications, lipid-lowering medication, anti-diabetic medication, BMI, family history of CHD, diabetes, HDL-cholesterol, total cholesterol, and triglyceride.
For daily caffeine consumption, curves represent adjusted odds ratio (solid line) and their 95% confidence intervals (dashed lines) based on restricted cubic splines for caffeine intake among all participants with knots at the 5th, 35th, 65th and 95th percentiles of their sample distributions (corresponding to 0.5, 59, 161, 626 mg). The reference values (diamond dots) were set at 10th percentile (5 mg).
In longitudinal analyses, coffee intake was not associated with coronary artery calcium progression in fully-adjusted multivariable models (Table 4, Figure 2). In contrast, participants who drank ≥1 cup/day of tea had a reduced progression of coronary artery calcium (PR: 0.73 [0.61–0.87]). Participants with higher caffeine consumption also had less coronary artery calcium progression (PR: 0.87 [0.76–1.00] comparing 3rd vs 1st tertile). In sensitivity analysis, exclusion of participants with coronary artery calcium of 0 at baseline or exclusion of Chinese participants did not significantly change coronary artery calcium progression ratios (Supplemental Table 1). We found a statistically significant interaction between caffeine and smoking (p=0.008), as well as caffeine and sex (p=0.02) for coronary artery calcium progression. In stratified analyses, the associations were stronger in non-smokers and former smokers compared to current smokers (Supplemental Tables 2–4) and in men compared to women (Supplemental Tables 5–6).
Table 4.
Prospective: Coronary artery calcium progression ratios (95% CIs)* by categories of coffee and tea consumption among all individuals
| Daily coffee consumption | |||
|---|---|---|---|
| None | <1 cup | ≥1 cup | |
| N people/n visits | 1554/3913 | 1492/3811 | 3159/8064 |
| Model 1 | 1.00 | 1.14 (0.97, 1.33) | 1.17 (1.02, 1.34) |
| Model 2 | 1.00 | 1.13 (0.96, 1.32) | 1.06 (0.92, 1.22) |
| Model 3 | 1.00 | 1.10 (0.94, 1.28) | 1.06 (0.92, 1.22) |
| Model 4 | 1.00 | 1.11 (0.95, 1.29) | 1.06 (0.92, 1.22) |
| Daily tea consumption | |||
| None | <1 cup | ≥1 cup | |
| N people/n visits | 3562/8963 | 1825/4743 | 800/2029 |
| Model 1 | 1.00 | 0.92 (0.81, 1.05) | 0.72 (0.61, 0.86) |
| Model 2 | 1.00 | 0.95 (0.83, 1.08) | 0.74 (0.62, 0.88) |
| Model 3 | 1.00 | 0.97 (0.85, 1.10) | 0.74 (0.62, 0.88) |
| Model 4 | 1.00 | 0.96 (0.85, 1.09) | 0.73 (0.61, 0.87) |
| Caffeine consumption (mg/day) | |||
| 1st Tertile (<55) | 2nd Tertile (55–<167) | 3rd Tertile (167–1354) | |
| N people/n visits | 2174/5481 | 2165/5460 | 2169/5622 |
| Model 1 | 1.00 | 0.99 (0.87, 1.13) | 1.04 (0.91, 1.19) |
| Model 2 | 1.00 | 0.90 (0.79, 1.04) | 0.91 (0.79, 1.06) |
| Model 3 | 1.00 | 0.88 (0.77, 1.01) | 0.89 (0.77, 1.03) |
| Model 4 | 1.00 | 0.87 (0.76, 1.00) | 0.88 (0.76, 1.02) |
Progression ratio was derived from mixed effect regression models using loge(calcium+1) as the outcome
Model 1: age, sex, race/ethnicity, education, and number of follow-up years.
Model 2: model 1 + smoking (never, former, current), physical activity, total fat, alcohol consumption, fruits quartiles, vegetables quartiles, red meat quartiles
Model 3: model 2 + systolic and diastolic blood pressures, use of antihypertensive medications, lipid-lowering medication, anti-diabetic medication, body mass index, family history of coronary heart disease, diabetes, high-density lipoprotein cholesterol, total cholesterol, triglyceride
Model 4: model 3 + C-reactive protein, and fibrinogen
Figure 2.
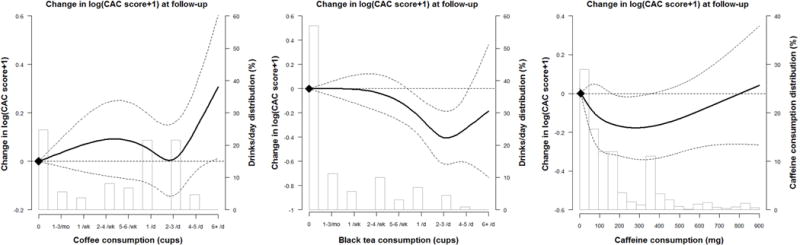
Change log (coronary artery calcium scores+1) during follow up among all participants by coffee, tea and caffeine consumption at baseline.
The curves represent the adjusted change of CAC scores and coffee/tea consumption. The dose response association of coffee/tea consumption was estimated by using a linear and a cubic spline term for coffee/tea consumption in the mixed effect regression. The reference values (diamond dots) were set at 0 drink per day. For caffeine intake, knots were set at the 5th, 35th, 65th and 95th percentiles of their sample distributions (corresponding to 0.5, 59, 161, 626 mg). The reference values (diamond dots) were set at 10th percentile (5 mg). The model adjusted for age, sex, race/ethnicity, education, smoking (never, former, current), physical activity, total fat, alcohol consumption, fruits quartiles, vegetables quartiles, red meat quartiles, systolic and diastolic blood pressures, use of antihypertensive medications, lipid-lowering medication, anti-diabetic medication, BMI, family history of CHD, diabetes, HDL-cholesterol, total cholesterol, and triglyceride.
Coffee/Tea Intake and Cardiovascular Events
Compared to participants who did not drink any coffee, those who drank <1 cup/day of coffee had an increased incidence of cardiovascular events (HR 1.28, [95% CI: 1.02–1.61] (Table 5), while tea intake of ≥1 cup/day was associated with a lower incidence of cardiovascular events compared with no tea intake (HR 0.71 [95% CI 0.53–0.95]). Caffeine intake was not associated with cardiovascular events. In sensitivity analyses, the associations were similar when we used hard cardiovascular events as the endpoint or when we excluded Chinese-American participants (Supplemental Tables 1,7). For cardiovascular events, there were no significant interactions between coffee, tea, or caffeine intake and sex, race/ethnicity, age, or smoking.
Table 5.
Hazard ratios between coffee and incident cardiovascular event
| Daily coffee consumption | |||
|---|---|---|---|
| None | <1 cup | ≥ 1 cups | |
| N event/n total | 146/1552 | 189/1492 | 380/3156 |
| IR per 1000 py | 8.6 | 11.9 | 11.3 |
| Model 1 | 1.00 | 1.33 (1.07, 1.66) | 1.12 (0.92, 1.37) |
| Model 2 | 1.00 | 1.29 (1.03, 1.61) | 0.97 (0.78, 1.19) |
| Model 3 | 1.00 | 1.29 (1.02, 1.61) | 0.96 (0.78, 1.19) |
| Model 4 | 1.00 | 1.28 (1.02, 1.61) | 0.97 (0.78, 1.20) |
| Daily tea consumption | |||
| None | <1 cup | ≥ 1 cups | |
| N event/n total | 460/3558 | 189/1824 | 68/800 |
| IR per 1000 py | 12.3 | 9.5 | 7.7 |
| Model 1 | 1.00 | 0.89 (0.75, 1.06) | 0.69 (0.53, 0.90) |
| Model 2 | 1.00 | 0.92 (0.76, 1.10) | 0.70 (0.53, 0.93) |
| Model 3 | 1.00 | 0.92 (0.77, 1.11) | 0.72 (0.54, 0.96) |
| Model 4 | 1.00 | 0.92 (0.76, 1.10) | 0.71 (0.53, 0.95) |
| Caffeine consumption (mg/day) | |||
| 1st Tertile (<55) | 2nd Tertile (55–<167) | 3rd Tertile (167–1354) | |
| N event/n total | 235/2172 | 266/2165 | 249/2166 |
| IR per 1000 py | 10.0 | 11.6 | 10.7 |
| Model 1 | 1.00 | 1.06 (0.89, 1.27) | 1.05 (0.87, 1.27) |
| Model 2 | 1.00 | 1.00 (0.82, 1.21) | 0.89 (0.72, 1.10) |
| Model 3 | 1.00 | 0.96 (0.79, 1.17) | 0.86 (0.70, 1.07) |
| Model 4 | 1.00 | 0.96 (0.79, 1.17) | 0.87 (0.70, 1.07) |
IR = incident rates, py = person years
Model 1: age, sex, race/ethnicity, and education.
Model 2: model 1 + smoking (never, former, current), physical activity, total fat, alcohol consumption, fruits quartiles, vegetables quartiles, red meet quartiles
Model 3: model 2 + systolic and diastolic blood pressures, use of antihypertensive medications, lipid-lowering medication, anti-diabetic medication, body mass index, family history of coronary heart disease, diabetes, high-density lipoprotein cholesterol, total cholesterol, triglyceride
Model 4: model 3 + C-reactive protein, and fibrinogen
Discussion
In this multi-ethnic study of men and women, we found that being a regular tea drinker was associated with a lower prevalence and progression of coronary artery calcium and a lower incidence of cardiovascular events. Conversely, being an occasional coffee drinker was associated with an increased incidence of cardiovascular events compared to never drinkers, but coffee intake was not associated with coronary artery calcium prevalence or progression. Also notable, we did not find that regular coffee intake was associated with an increased incidence of cardiovascular events. Moderate caffeine intake was associated with a slower progression of coronary artery calcium, but not with cardiovascular events. In stratified analyses, men and nonsmokers had stronger inverse associations between tea intake and coronary artery calcium progression than women or current smokers.
Although the relationship between coffee and cardiovascular disease has been well studied, the association between tea and cardiovascular disease is less clear. A meta-analysis found a non-significant trend towards a decreased rate of myocardial infarction in individuals drinking 3 cups/day of tea,20 but this study was likely limited by publication bias, preferentially including small studies with positive findings. Kuriyama et al reported an association of green tea consumption with reduced all-cause and cardiovascular disease mortality in a middle aged Japanese population.21 In the Coronary Artery Risk Development in Young Adults (CARDIA) Study, the authors found a lower odds of coronary artery calcium progression over 5 years in those who drank more than 2 cups/day of tea.11 Our findings are consistent with and extend those from CARDIA, as we discovered an inverse association between regular tea intake and cardiovascular events in an older, more diverse, and larger population. In addition, our results were consistent in sensitivity analysis after exclusion of Chinese participants, an ethnic group with a higher prevalence of tea consumption. Further, this relationship was seen most predominantly in those with coronary artery calcium at baseline, which could be related to the components in tea having greater benefits for those already with coronary artery disease.22,23
Proposed benefits of tea, specifically through polyphenols such as flavonoids,20,24 include antioxidant properties that decrease the oxidation of low-density lipoproteins,25 enhance nitric oxide release,26 improve short and long-term endothelial function,27 and decrease progression of atherosclerosis.28,29 In a meta-analysis with nearly 100,000 individuals, moderate intake of flavonoids was associated with decreased cardiovascular mortality.30 However, intervention studies in humans have yielded conflicting results, which may be due to differences in flavonoid administration, patient population, and bioavailability.31 Regardless, flavonoid consumption, primarily through a Mediterranean diet, is recommended by the American Heart Association for secondary prevention of cardiovascular disease.32
The majority of studies assessing the association between coffee and cardiovascular disease have shown a neutral to perhaps beneficial effect.6–8 However, in those finding a favorable effect, the dose-response relationship between coffee and cardiovascular disease has significantly differed.8,33,34 A recent meta-analysis described a nonlinear association where moderate coffee consumption was associated with a lower cardiovascular risk while higher and lower consumption was neutral.8 More recently, an analysis of over 200,000 individuals from the Nurses’ Health Study (NHS), NHS2, and Health Professionals Follow-up Study found a U-shaped association with moderate coffee consumption being associated with lower all-cause and cardiovascular mortality. When analysis was limited to never smokers, this relationship became linear, perhaps secondary to residual confounding.35 A potential limitation of these analyses include the predominantly white population of medical and health professionals, raising questions of generalizability, as compared with the diverse population in the present study.
In order to investigate the possible mechanisms behind the association of coffee and cardiovascular disease, others have studied the association of coffee with coronary artery calcium, a measure of subclinical atherosclerosis.36 In the Rotterdam Study, there was no association between coffee and coronary artery calcium in men, but women who drank >3 cups/day of coffee had a lower incidence of severe coronary artery calcium (defined as scores >400).10 Unfortunately, this study did not adjust for many known cardiovascular risk factors, including smoking, hypertension, diabetes, and lipid levels.
In CARDIA, there was no association between coffee intake with the prevalence or progression of coronary artery calcium.11 Results were not adjusted for several cardiovascular risk factors, but adjusted for smoking and physical activity. In the Kangbuk Samsung Health Study of Korean men and women, Choi et al found an U-shaped association with the lowest prevalence of coronary artery calcium in individuals drinking 3–4 cups/day of coffee.12 This dose response association was similar to that found in the meta-analysis of coffee intake and cardiovascular disease by Ding et al.8 In contrast, our study showed that occasional and regular coffee intake had a relatively neutral association with coronary artery calcium.
One potential explanation for the differences between studies may be cultural differences in coffee drinking. Another potential explanation for the differences between studies could be variable statistical adjustment.10,11 In the present analysis, occasional coffee drinkers had a higher rate of future cardiovascular events while regular drinkers had a neutral effect on cardiovascular events compared to never drinkers. Given that participants and their providers were informed of their computed tomography imaging results at baseline, it is possible that participants with higher coronary artery calcium scores or other high-risk features abstained from coffee intake due to perceived harm, such as deleterious effects on blood pressure. Our study may also be underpowered to detect an U-shaped pattern between coffee intake and cardiovascular events but the analysis of coronary artery calcium also did not identify a non-learner association. Finally, we cannot rule out residual confounding.
Limitations
While the observational nature of this study implies the potential for unmeasured confounders, our aim was to provide the best possible results with the available data, which includes a diverse population as opposed to a single ethnic group or specialized cohort, such as health professionals. In the future, we suggest that research methods must evolve from retrospective questionnaires to more careful tracking of diet, perhaps through smartphone fitness apps. On the MESA questionnaire, participants were not able to differentiate between decaffeinated or caffeinated beverages or between green and black tea. However, we included caffeine consumption in our analyses. As with any dietary study, responses were dependent on participant recall and subject to measurement error. However we judged that recall would be more accurate for never, occasional, and regular consumption, as compared with more granular categories. Further, coffee and tea intake have shown relatively high reproducibility and validity on questionnaires.35,37,38 Our study also has several strengths, including a diverse population, the use of carefully standardized and high quality field methods, and the assessment of coffee, tea, and caffeine with robust multivariable adjustment and sensitivity analyses. Further, to our knowledge, this is the first study to assess both subclinical and clinical cardiovascular outcomes in the same cohort.
Conclusions
In this large multi-ethnic sample, regular tea consumption was associated with decreased prevalence and progression of coronary artery calcium, and with a decreased incidence of cardiovascular events. Our study supports regular tea consumption as part of a heart healthy diet as recommended by the American Heart Association.32 In contrast, we found a neutral association between regular coffee and caffeine intake with coronary artery calcium and incident cardiovascular outcomes, suggesting regular intake is safe. Further studies are needed to delineate whether the protective association with tea consumption can be harnessed or if tea drinkers generally have healthier behaviors not measured in this study.
Supplementary Material
Clinical Significance.
Regular tea drinkers have slowed progression of coronary artery calcium and fewer cardiovascular events.
Regular coffee drinkers have coronary artery calcium scores and cardiovascular event rates that are similar to others, suggesting regular intake is safe.
These findings appear independent of caffeine intake.
Acknowledgments
This research was supported by contracts N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-TR-000040 and UL1-TR-001079 from NCRR. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
The other authors have no conflicts of interest to disclose.
References
- 1.USA NCA. National coffee drinking trends 2012. New York, NY: National Coffee Association USA; 2012. [Google Scholar]
- 2.Robertson D, Frolich JC, Carr RK, et al. Effects of caffeine on plasma renin activity, catecholamines and blood pressure. N Engl J Med. 1978;298:181–186. doi: 10.1056/NEJM197801262980403. [DOI] [PubMed] [Google Scholar]
- 3.Casugkua E, Bongiovi S, Paleari CD, et al. Haemodynamic effects of coffee and caffeine in normal volunteers: a placebo-controlled clinical study. J Intern Med. 1991;229:501–504. doi: 10.1111/j.1365-2796.1991.tb00385.x. [DOI] [PubMed] [Google Scholar]
- 4.Myers MG. Caffeine and cardiac arrhythmias. Ann Intern Med. 1991;114:147–150. doi: 10.7326/0003-4819-114-2-147. [DOI] [PubMed] [Google Scholar]
- 5.Corti R, Binggeli C, Sudano I, et al. Coffee acutely increases sympathetic nerve activity and blood pressure independently of caffeine content: role of habitual verses nonhabitual drinking. Circulation. 2002;106:2935–2940. doi: 10.1161/01.cir.0000046228.97025.3a. [DOI] [PubMed] [Google Scholar]
- 6.Huxley R, Lee CM, Barzi F, et al. Coffee, decaffeinated coffee, and tea consumption in relation to incident type 2 diabetes mellitus: a systematic review with meta-analysis. Arch Intern Med. 2009;169:2053–2063. doi: 10.1001/archinternmed.2009.439. [DOI] [PubMed] [Google Scholar]
- 7.Siasos G, Oikonomou E, Chrysomoou C, et al. Consumption of boiled Greek type of coffee is associated with improved endothelial function: the Ikaria study. Vasc Med. 2013;18:55–62. doi: 10.1177/1358863X13480258. [DOI] [PubMed] [Google Scholar]
- 8.Ding M, Bhupathiraju SN, Satija A, van Dam RM, Hu FB. Long-term coffee consumption and risk of cardiovascular disease: a systemic review and a dose-response meta-analysis of prospective cohort studies. Circulation. 2014;129:643–659. doi: 10.1161/CIRCULATIONAHA.113.005925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sofi F, Conti AA, Gori AM, et al. Coffee consumption and risk of coronary heart disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2007;17:209–223. doi: 10.1016/j.numecd.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 10.van Woudenbergh GJ, Vliegenthart R, van Rooij FJ, et al. Coffee consumption and coronary calcification: the Rotterdam Coronary Calcification Study. Arterioscler Thromb Vasc Biol. 2008;28:1018–1023. doi: 10.1161/ATVBAHA.107.160457. [DOI] [PubMed] [Google Scholar]
- 11.Reis JP, Loria CM, Steffen LM, et al. Coffee, decaffeinated coffee, caffeine, and tea consumption in young adulthood and atherosclerosis later in life: the CARDIA study. Arterioscler Thromb Vasc Biol. 2010;30:2059–2066. doi: 10.1161/ATVBAHA.110.208280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi Y, Chang Y, Ryu S, et al. Coffee consumption and coronary artery calcium in young and middle-aged asymptomatic adults. Heart. 2015;101:686–691. doi: 10.1136/heartjnl-2014-306663. [DOI] [PubMed] [Google Scholar]
- 13.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 14.Mayer-Davis EJ, Vitolins MZ, Carmichael SL, et al. Validity and reproducibility of a food frequency interview in a Multi-Cultural Epidemiology Study. Ann Epidemiol. 1999;9:314–324. doi: 10.1016/s1047-2797(98)00070-2. [DOI] [PubMed] [Google Scholar]
- 15.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 16.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) Study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 17.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 18.Bertoni AG, Whitt-Glover MC, Chung H, et al. The association between physical activity and subclinical atherosclerosis: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2009;169:444–454. doi: 10.1093/aje/kwn350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gassett AJ, Sheppard L, McClelland RL, et al. Risk factors for long-term coronary artery calcium progression in the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2015;4:e001726. doi: 10.1161/JAHA.114.001726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peters U, Poole C, Arab L. Does tea affect cardiovascular disease? A meta-analysis. Am J Epidemiol. 2001;154:495–503. doi: 10.1093/aje/154.6.495. [DOI] [PubMed] [Google Scholar]
- 21.Kuriyama S, Shimazu T, Ohmori K, et al. Green tea consumption and mortality due to cardiovascular disease, cancer, and all-causes in Japan: the Ohsaki study. JAMA. 2006;296:1255–1265. doi: 10.1001/jama.296.10.1255. [DOI] [PubMed] [Google Scholar]
- 22.Hertog MG, Feskens EJ, Hollman PC, Katan MB, Kromhout D. Dietary antioxidant flavonoids and risk of coronary artery heart disease: the Zutphen Elderly Study. Lancet. 1993;342:1007–1011. doi: 10.1016/0140-6736(93)92876-u. [DOI] [PubMed] [Google Scholar]
- 23.Rimm EB, Katan MB, Ascherio A, Stampfer MJ, Willet WC. Relation between intake of flavonoids and risk for coronary heart disease in male health professions. Ann Intern Med. 1996;125:284–289. doi: 10.7326/0003-4819-125-5-199609010-00005. [DOI] [PubMed] [Google Scholar]
- 24.Frei B, Higdon JV. Antioxidant activity of tea polyphenols in vivo: evidence from animal studies. J Nutr. 2003;133:3275S–3284S. doi: 10.1093/jn/133.10.3275S. [DOI] [PubMed] [Google Scholar]
- 25.de Whalley CV, Rankin SM, Hoult JR, Jessup W, Leake DS. Flavonoids inhibit the oxidative modification of low density lipoproteins by macrophages. Biochem Pharmacol. 1990;39:1743–1750. doi: 10.1016/0006-2952(90)90120-a. [DOI] [PubMed] [Google Scholar]
- 26.Freedman JE, Parker C, 3rd, Li L, et al. Select flavonoids and whole juice from purple grapes inhibit platelet function and enhance nitric oxide release. Circulation. 2001;103:2792–2798. doi: 10.1161/01.cir.103.23.2792. [DOI] [PubMed] [Google Scholar]
- 27.Duffy SJ, Keaney JF, Jr, Holbrook M, et al. Short- and long-term black tea consumption reverses endothelial dysfunction in patients with coronary artery disease. Circulation. 2001;104:151–156. doi: 10.1161/01.cir.104.2.151. [DOI] [PubMed] [Google Scholar]
- 28.Hayek T, Fuhrman B, Vaya J, et al. Reduced progression of atherosclerosis in apolipoprotein E-deficient mice following consumption of red wine, or its polyphenols quercetin or catechin, is associated with reduced susceptibility of LDL to oxidation and aggregation. Arterioscl Thromb Vasc Biol. 1997;17:2744–2752. doi: 10.1161/01.atv.17.11.2744. [DOI] [PubMed] [Google Scholar]
- 29.Geleijnse JM, Launer LJ, Hofman A, Pols HA, Witteman JC. Tea flavonoids may protect against atherosclerosis: the Rotterdam Study. Arch Intern Med. 1999;159:2170–2174. doi: 10.1001/archinte.159.18.2170. [DOI] [PubMed] [Google Scholar]
- 30.McCullough ML, Peterson JJ, Patel R, Jacques PF, Shah R, Dwyer JT. Flavonoid intake and cardiovascular disease mortality in a prospective cohort of US adults. Am J Clin Nutri. 2012;95:454–464. doi: 10.3945/ajcn.111.016634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manach C, Mazur A, Scalbert A. Polyphenols and prevention of cardiovascular disease. Curr Opin Lipidol. 2005;16:77–84. doi: 10.1097/00041433-200502000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Fleg JL, Forman DE, Berra K, et al. Secondary prevention of atherosclerotic cardiovascular disease in older adults: a scientific statement from the American Heart Association. Circulation. 2013;128:2422–2446. doi: 10.1161/01.cir.0000436752.99896.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu JN, Ho SC, Zhou C, et al. Coffee consumption and risk of coronary artery disease: a meta-analysis of 21 prospective cohort studies. Int J Cardiol. 2009;137:216–225. doi: 10.1016/j.ijcard.2008.06.051. [DOI] [PubMed] [Google Scholar]
- 34.Malerba S, Turati F, Galeone C, et al. A meta-analysis of prospective studies of coffee consumption and mortality for all causes, cancers and cardiovascular diseases. Eur J Epidemiol. 2013;28:527–539. doi: 10.1007/s10654-013-9834-7. [DOI] [PubMed] [Google Scholar]
- 35.Ding M, Satija A, Bhupathiraju SN, et al. Association of coffee consumption with total and cause-specific mortality in three large prospective cohorts. Circulation. 2015;132:2305–2315. doi: 10.1161/CIRCULATIONAHA.115.017341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–1260. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- 37.Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food questionnaire developed for the Tehran Lipid and Glucose Study. J Epidemiol. 2010;20:150–158. doi: 10.2188/jea.JE20090083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferraroni M, Tavani A, Decarli A, et al. Reproducibility and validity of coffee and tea consumption in Italy. Eur J Clin Nutri. 2004;48:674–680. doi: 10.1038/sj.ejcn.1601864. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


