Abstract
Following a failed course of conservative management, arthroscopic rotator cuff repair (ARCR) has become the gold standard treatment for patients presenting with symptomatic rotator cuff (RC) tears. Traditionally, the single-row repair technique was used. Although most patients enjoy good to excellent clinical outcomes, structural healing to bone remains problematic. As a result, orthopaedic surgeons have sought to improve outcomes with various technological and technical advancements. One such possible advancement is the double-row technique.
We present a method for repairing an RC tear using double-row suture anchors in a transosseous equivalent suture bridge technique. The double-row technique is believed to more effectively re-create the anatomic footprint of the tendon, as well as increase tendon to bone surface area, and apposition for healing. However, it requires longer operating times and is costlier. This report highlights this technique for ARCR in an adult by using a double-row transosseous equivalent suture bridge.
The rotator cuff (RC) is composed of the supraspinatus, infraspinatus, teres minor, and subscapularis muscles and their tendons—the supraspinatus being the most commonly injured.1 Most injuries in older patients are a result of gradual degenerative change, whereas younger individuals may have tears from repetitive overhead activities or due to traumatic etiology.
The majority of tears can initially be treated with nonoperative management including physical therapy, nonsteroidal anti-inflammatory drugs, and subacromial corticosteroid injections.2 Criteria for operative management include painful and symptomatic RC tears that have failed to respond to conservative management, acute traumatic tears, and massive RC tears in young (<60 years old), high-demand patients. These tears must be deemed reparable prior to operative intervention by assessing tear characteristics on advanced imaging, including size, fatty degeneration (Goutallier classification), and retraction.3 If operative management is decided on, anatomic RC repair (ARCR) of tears has become the gold standard treatment. Although most patients enjoy good to excellent clinical outcomes, structural healing to bone remains problematic, with healing rates ranging from 10% to 91% based on tear size.1 Accordingly, orthopaedic surgeons have sought to improve outcomes with various technological and technical advancements. One such possible advancement is the double-row technique.
We present a method for repairing an RC tear using double-row suture anchors in a transosseous-equivalent suture bridge technique. Although limited comparative studies with more traditional techniques exist, the double-row technique is believed to more effectively re-create the anatomic footprint of the tendon, as well as increase tendon to bone surface area, and apposition for healing.4, 5 This report highlights the technique for RC repair in an adult by using a double-row transosseous-equivalent suture bridge.
Surgical Technique
Preoperative Setup
A step-by-step video of the procedure can be seen in Video 1. The patient is placed in the lateral decubitus position using a bean bag–type support placed on the torso and pelvis on a standard operating table. All bony prominences are well padded with the nonoperative arm in 90° of flexion, the knees bent, and head in neutral alignment. The operative arm is then placed in a foam traction sleeve, and 10 lb of traction is applied with the lateral arm holder. The arm is placed in 40° to 50° of abduction and 15° of forward flexion.
Arthroscopic Portal Placement
We begin by making a standard posterior portal approximately 2 cm inferior and medial to the posterolateral corner of the acromion. The scope is inserted into the glenohumeral joint. Intra-articular structures are assessed, and the pathology is addressed using an anterior portal, which can be created using an inside-out or outside-in technique. This portal is approximately 1 to 2 cm inferior and medial to the anterolateral corner of the acromion through the rotator interval; care is taken to remain lateral and superior to the coracoid to avoid neurovascular injury.
Initial Assessment
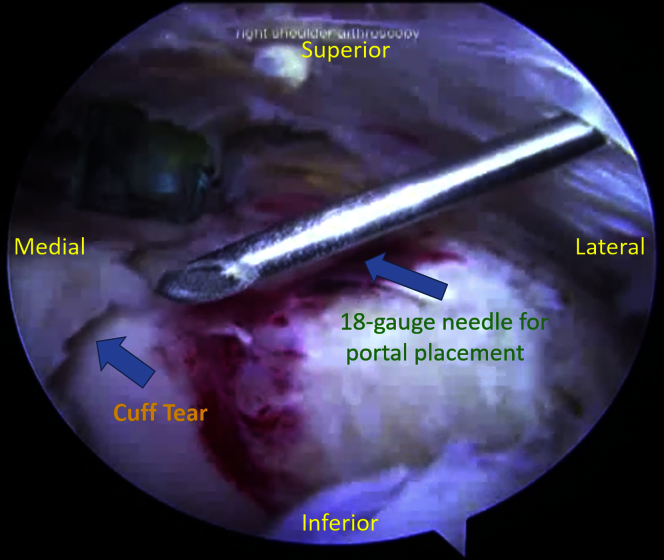
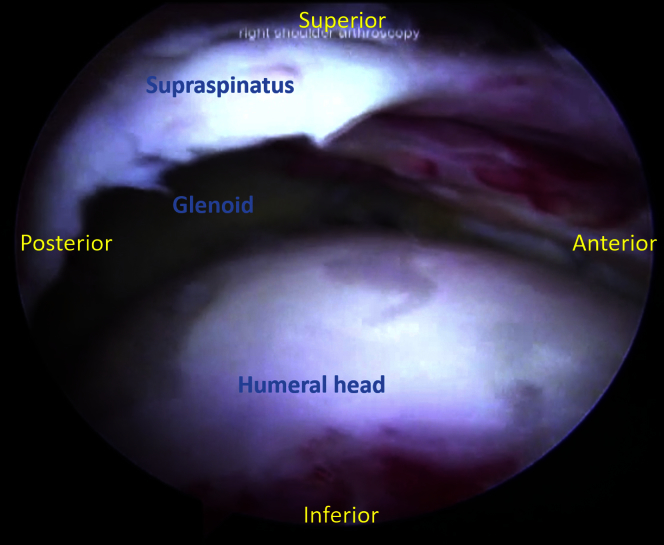
The arthroscope is then directed into the subacromial space using the same posterior portal. In our case, a large crescent-shaped RC tear is identified. An 18-gauge spinal needle is used to localize the position of the lateral portal (Fig 1). We try to position this portal at the midportion of the exposed footprint and 3 cm lateral to the lateral edge of the acromion. A 7-mm twist-in cannula is placed. The bursa is cleared using an arthroscopic motorized shaver (4.5-mm Synovator; Smith & Nephew). To further assess the RC tear, the arthroscope can be placed laterally directly through the cannula. Careful inspection of the tear may allow recognition of the tear pattern (Fig 2), which helps dictate the method of reduction; this can be facilitated using a cuff grasper. Failure to do so may lead to a nonanatomic repair, which increases the likelihood of failure. For example, if a U- or L-shaped tear is noted, marginal convergence sutures may be required for a more anatomic repair prior to anchor placement.
Fig 1.
Cannula localization. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, an 18-gauge spinal needle is used to localize the position of the lateral portal (Fig 1). We try to position this portal at the midportion of the exposed footprint and 3 cm lateral to the lateral edge of the acromion. A 7-mm twist-in cannula is placed.
Fig 2.
Assessing cuff tear morphology. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the lateral portal, one can inspect tear morphology, which helps dictate method of reduction; this can be facilitated using a cuff grasper. In this case, a large crescent-shaped rotator cuff tear is identified.
Footprint Preparation and Anchor Placement
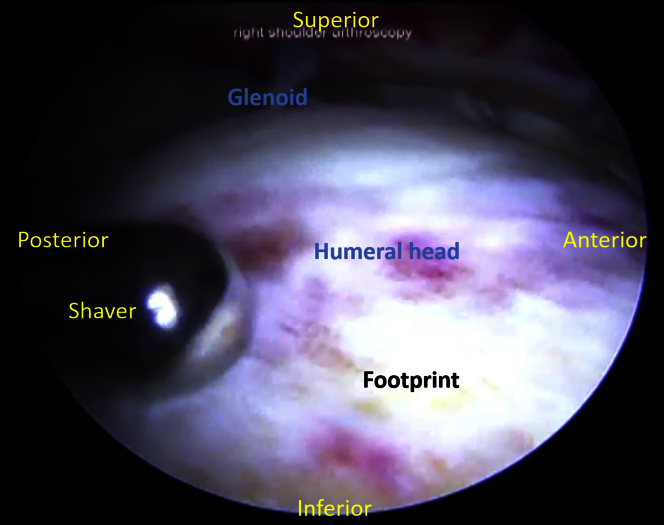
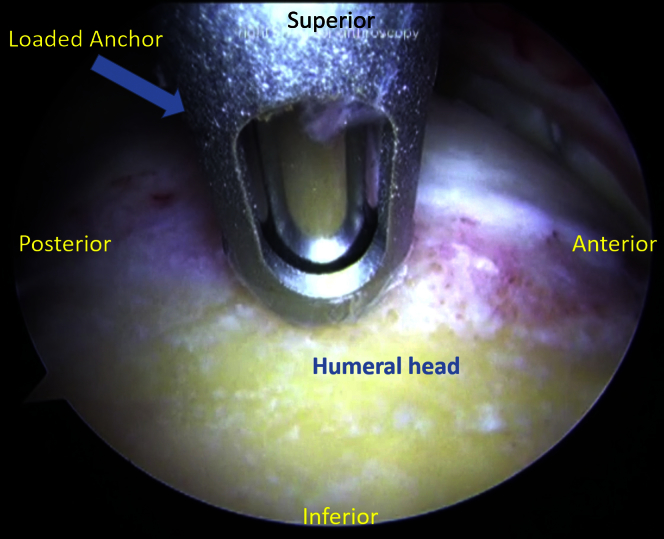
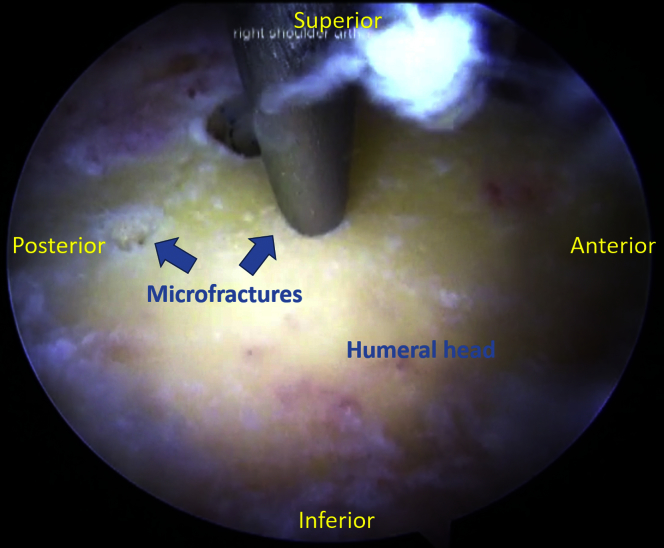
The footprint is now prepared using the shaver (Fig 3); the bone is gently abraded to preserve osseous integrity and minimize the possibility of suture anchor pullout. An elevator is used to release any bursal-sided adhesions and mobilize the RC. Additional releases are performed as necessary to create a tension-free repair. A spinal needle is used to localize placement for an anchor portal, which is typically placed just off the lateral margin of the acromion. An awl is used to create sockets for the suture anchors, which are placed at an angle of 45° relative to the plane of the tuberosity (Fig 4). The arm can always be rotated internally or externally to ease insertion of the awl and anchors. Typically, 2 to 3 medial anchors are placed and spaced out just lateral to the articular margin (medial aspect of the RC footprint), but this can vary based on surgeon preference and the size of the RC tear. The tip of the awl can be used to make several microfractures across the footprint to stimulate a healing response (Fig 5). Double-loaded, 4.5-mm screw-in suture anchors (Corkscrew FT; Arthrex) are placed into the previously created sockets. After each anchor is placed, it is tested for pullout by pulling on the sutures.
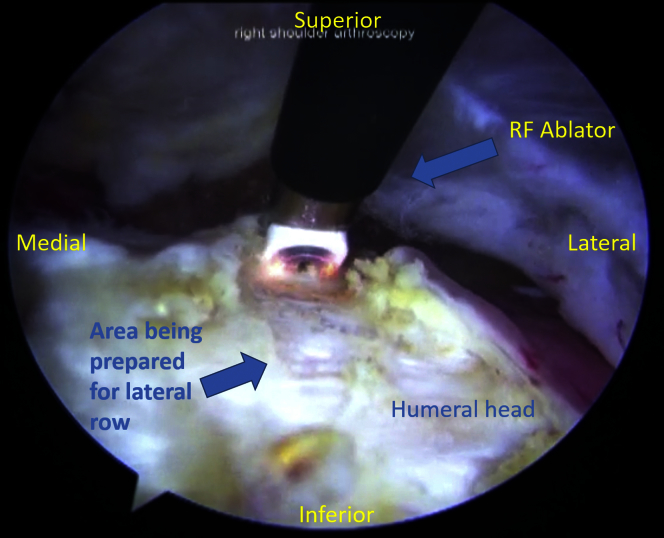
Fig 3.
Footprint preparation. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the lateral portal, preparation of the footprint with the shaver is shown. The bone is gently abraded to preserve osseous integrity and minimize the possibility of suture anchor pullout.
Fig 4.
Anchor placement. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the lateral portal, anchor placement is demonstrated. An awl is used to create sockets for the suture anchors, which are placed at an angle of 45° relative to the plane of the tuberosity. Double-loaded, 4.5-mm screw-in suture anchors are placed into the previously created sockets. After each anchor is placed, it is tested for pullout by pulling on the sutures.
Fig 5.
Microfracture. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the lateral portal, microfracture is demonstrated. The tip of the awl can be used to make several microfractures across the footprint to stimulate a healing response.
Suture Knot Tying
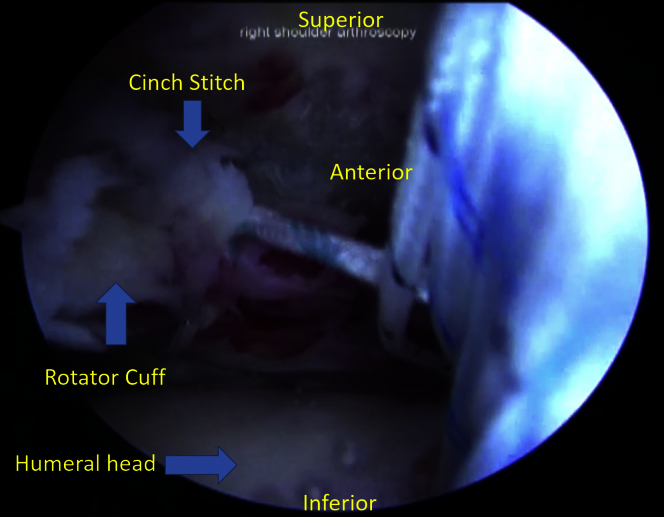
The arthroscope is now repositioned back into the posterior portal. Beginning anteriorly, sutures are then retrieved individually and passed in a horizontal mattress fashion using a suture-passing device (Expressew; DePuy Mitek) across the entire breadth of the tear. After each pass, sutures are retrieved and brought out through the anterior portal. Each pass is spaced about 3 mm. The suture-passing device is placed as far medially as possible, close to the musculotendinous junction, were the tissue quality is usually better to minimize suture cut-through. To secure the posterior edge of the tear, and to avoid the potential for dog-ear formation, a suture cinch stitch (FiberSnare; Arthrex) that is pre-looped at one end is passed (Fig 6). The free end of the suture snare is passed and secured through the looped end. The anterior tear edge is secured in similar fashion with a second cinch stitch.
Fig 6.
Cinch stitch. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, a cinch stitch is placed. To secure the posterior edge of the tear, and to avoid the potential for dog-ear formation, a suture cinch stitch that is prelooped at one end is passed. The free end of the suture snare is passed and secured through the looped end. The anterior tear edge is secured in similar fashion with a second cinch stitch.
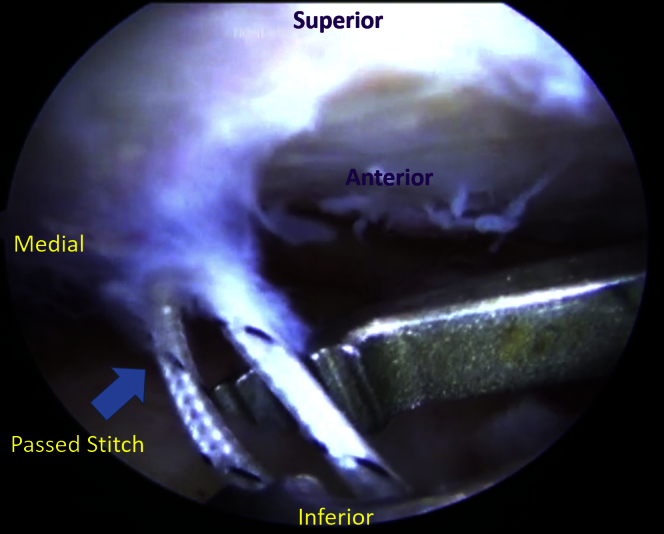
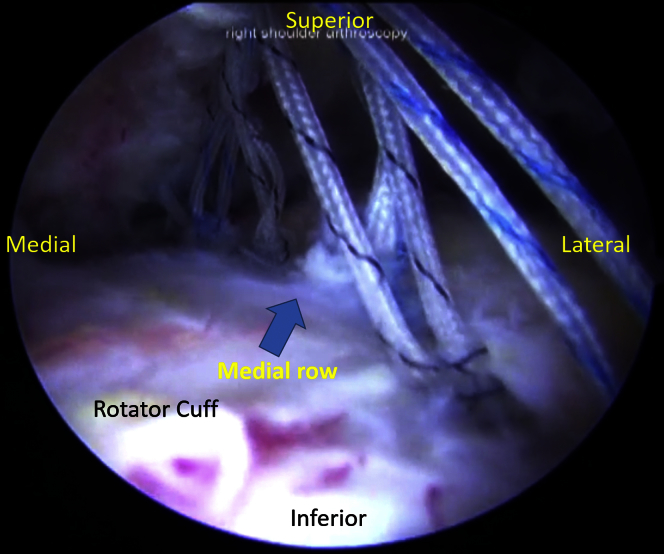
Beginning posteriorly, the mattress sutures are then tied individually using arthroscopic knot tying techniques per surgeon preference (Fig 7). In this case, a modified SMC sliding knot is performed, supported with 3 alternating half-hitches (Fig 8). The bone is exposed just lateral to the greater tuberosity using a radiofrequency ablator (Vapr Vue; DePuy Mitek) in preparation for lateral row anchor placement (Fig 9). Typically, 2 lateral row anchors are used. Alternating sutures are retrieved from the lateral portal and passed through the eyelet of the knotless lateral row anchor. An awl is used to create the socket for the anchor (Fig 10), which should be placed just lateral to the footprint in the greater tuberosity. If the bone quality appears poor, the anchor position can be moved to a more lateral position relative to the footprint edge. The anchor (SwiveLock; Arthrex) is placed into the socket, but prior to fully seating the anchor, the sutures are tensioned and bridged over the bursal surface of the RC (Fig 11). The anchor is then fully seated, and the sutures are cut flush with the anchor (Fig 12). This process is then repeated with the remaining sutures and a second lateral-row anchor. The additional eyelet suture commonly preloaded on the lateral row anchor can be passed if additional fixation is needed for any residual “dog-ear” deformity, or pulled out if not needed (Fig 13). Pearls and pitfalls can be found in Table 1.
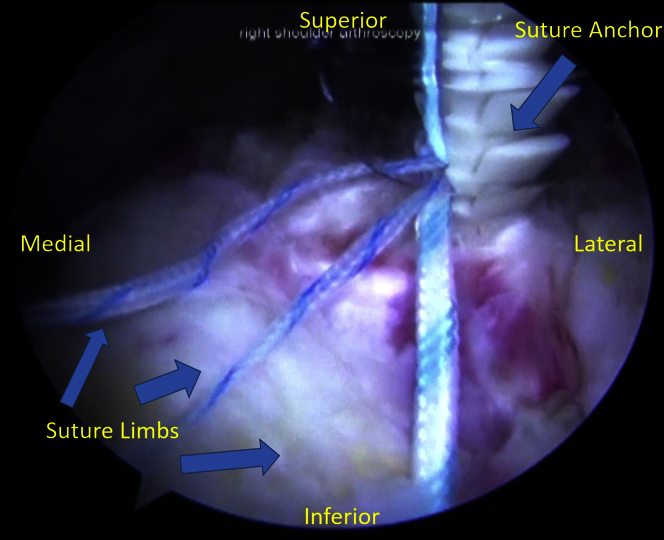
Fig 7.
Mattress sutures. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, the suture limbs from the anchor are passed. Beginning anteriorly, sutures are then retrieved individually and passed in a horizontal mattress fashion using a suture-passing device across the entire breadth of the tear. After each pass, sutures are retrieved and brought out through the anterior portal. Each pass is spaced about 3 mm. The suture-passing device is placed as far medially as possible, close to the musculotendinous junction, were the tissue quality is usually better to minimize suture cut-through.
Fig 8.
Tied medial row. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, the knotted medial row is observed. Beginning posteriorly, the mattress sutures are tied individually using arthroscopic knot-tying techniques per surgeon preference; in this case, a modified SMC sliding knot is performed, supported with 3 alternating half-hitches.
Fig 9.
Radioablation. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, the bone is exposed just lateral to the greater tuberosity using a radiofrequency (RF) ablator (DepuyMitek Vapr Vue) in preparation for lateral row anchor placement.
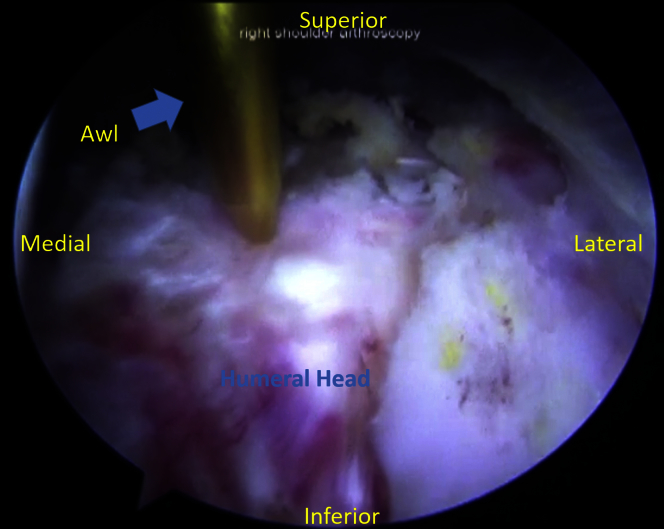
Fig 10.
Awl placement. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, the lateral row suture anchors are placed. An awl is used to create the socket for the anchor, which should be placed just lateral to the footprint in the greater tuberosity. If the bone quality appears poor, the anchor position can be moved to a more lateral position relative to the footprint edge.
Fig 11.
Lateral row placement. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, the lateral row suture anchors are placed. Alternating sutures are retrieved from the lateral portal and passed through the eyelet of the knotless lateral row anchor. An awl is used to create the socket for the anchor. The anchor is placed into the socket, but before fully seating the anchor, the sutures are tensioned and bridged over the bursal surface of the rotator cuff. The anchor is then fully seated, and the sutures are cut flush with the anchor.
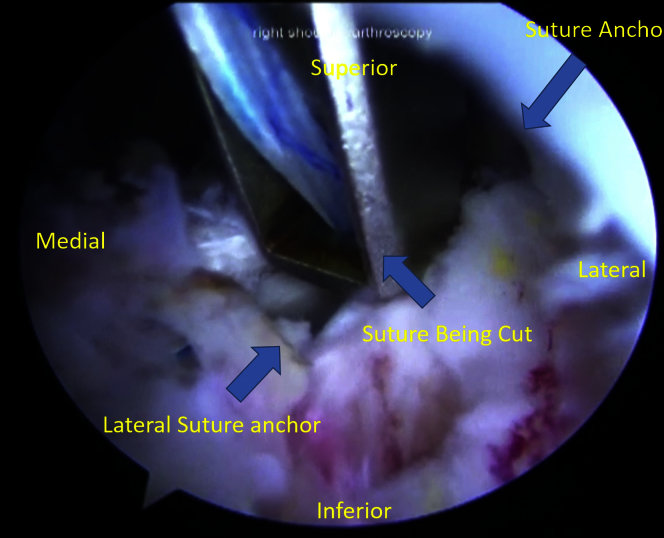
Fig 12.
Cutting sutures. With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the posterior portal, the anchor is then fully seated and the sutures are cut flush with the anchor. This process is then repeated with the remaining sutures and a second lateral row anchor. The additional eyelet suture commonly preloaded on the lateral row anchor can be passed if additional fixation is needed for any residual “dog-ear” deformity, or pulled out if not needed.
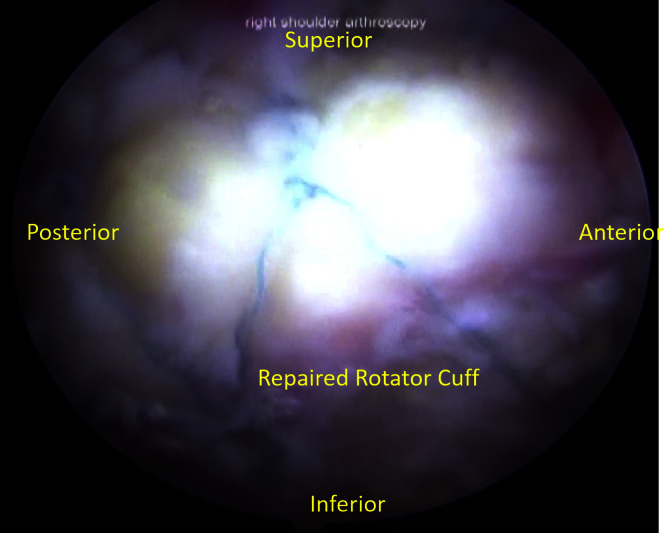
Fig 13.
With the patient placed in the lateral decubitus position, the right arm placed in 40°-50° of abduction and 15° of forward flexion and viewing from the lateral portal, the finished product can be appreciated.
Table 1.
Pearls, Pitfalls, and Complications of Rotator Cuff Repair Using the Transosseous-Equivalent Technique
| Pearls | Pitfalls | Complications |
|---|---|---|
| Inspection through the lateral portal may allow for recognition of cuff tear pattern | Failure to recognize tear pattern may lead to nonanatomic repair | Injury to suprascapular or axillary nerves |
| When preparing the footprint, gently abrade the bone to preserve osseous integrity and minimize possibility of suture anchor pull-out | With anterior portal, remain lateral and superior to the coracoid to avoid neurovascular injury | Stiffness |
| The tip of the awl can be used to make several microfractures across the footprint to stimulate a healing response | Remember to test each anchor after placement | Recurrent tendon tear |
| Placing the suture passing device as far medially as possible minimizes suture cut-through | To avoid the potential for dog-ear formation, a suture cinch stitch that is prelooped at one end is passed | Infection |
| Before fully seating the anchor, the sutures are tensioned as the bridge over the bursal surface of the rotator cuff |
Postoperative Protocol
A standard postoperative rehabilitation protocol is used consisting of sling for 6 weeks with passive range of motion only. From weeks 6 through 12, active range of motion is instituted, followed by a strengthening program starting at 12 weeks.
Discussion
As the incidence of arthroscopic RC tears continues to increase in tandem with an aging population, greater emphasis is being placed on understanding which factors lead to improved outcomes.6 Etiology of RC failure classically has been attributed to 4 categories: biologic, technical, anatomic, and mechanical.7
Biologic factors involved qualities inherent to individual patients—diabetes, vascular pathology, or tobacco use—that may inhibit healing potential.8, 9 Technical factors typically involve surgeon expertise and may include quality of anchors and/or suture materials used. The combination of increased surgeon experience and continued product innovation currently make technical complications a rare cause of failure.
The anatomic footprint has been described as a “consistent, measurable pattern” of RC tendon insertion onto humerus,10 and numerous studies have commented on the significance of its restoration during arthroscopic RC repair.10, 11, 12, 13 Tendon healing occurs at the tendo-osseous junction. Although histologic and biomechanical characteristics after RC repair are inferior to that of the native enthesis, previous authors have demonstrated that potential for healing increases as the surface area for bone-tendon interface is maximized, which allows for greater fibrovascular tissue formation.14, 15
A multitude of advantages has been associated with the double-row technique. The double-row suture technique provides significantly more pressurized contact area, with Tuoheti et al. reporting that double-row constructs resulted in 42% greater contact area than transosseous repairs and 60% greater contact area than single-row constructs. Mazzocca et al. confirmed that double-row repair restored a greater percentage of the footprint than single-row techniques.16, 17 A myriad of biomechanical studies also have demonstrated superiority of double-row compared with single-row repairs, particularly in regard to load to failure and gap formation at repair site. These advantages ultimately have been shown to lead to greater structural integrity of the cuff repair.17, 18, 19, 20, 21
Despite the plethora of evidence that the double-row technique is anatomically and biomechanically superior to single-row and transosseous, results regarding clinical outcomes remains equivocal. Three Level I studies by Franceschi et al.,22 Burks et al.,23 and Grasso et al.24 demonstrated no significant difference in outcome scores (University of California Los Angeles [UCLA] shoulder score; ASES score created by the Society of the American Shoulder and Elbow Surgeons; Constant-Murley; Disabilities of the Arm, Shoulder and Hand [DASH]) between single- and double-row repairs. Franceschi et al. randomized 60 patients to receive either single-row (30) or double-row (30) repair. Mean operative time was found to be significantly less in the single-row cohort than double-row (42 ± 18.9 minutes vs 65 ± 23.4 minutes, P = .005). Both groups demonstrated statistically significant improvements in UCLA scores at a mean of 22.5 months' follow-up. Despite this, final UCLA outcome scores were not statistically different between groups (P > .05), and magnetic resonance arthrography demonstrated similar healing rates between single- and double-row repair. Burks et al. similarly randomized 40 patients to receive either single-row (20) or double-row ARCR. A variety of outcome scores measured (Western Ontario Rotator Cuff Index [WORC], Constant-Murley, ASES, UCLA, and Single Assessment Numeric Evaluation [SANE]) along with physician-measured external and internal rotation measurements demonstrated no significant differences at a 1-year follow-up between single- and double-row repair groups. Additionally, musculoskeletal radiologists blinded to treatment group evaluated footprint, thickness, or signal content between groups at 6 weeks, 3 months, and 1 year postoperatively and found no significant differences between single- and double-row groups. The final study by Grasso et al. randomized 80 patients to receive either single-row (40) or double-row (40) ARCR. Mean-follow up was 24.8 ± 1.4 months. The authors performed a multivariate analysis accounting for age, gender, shape and size of RC tear, degree of retraction and fatty degeneration, and single- or double-row repair and found that repair type was not independently associated with improved outcomes. The combination from these 3 Level I prospective studies demonstrates that despite biomechanical advantages conferred by double-row repair, clinical outcomes between single- and double-row ARCR are equivalent across a variety of subjective and objective outcome measures.
Recent meta-analyses report that single-row repairs result in higher rates of retear than double-row techniques (25.9% vs 14.2%, P < .001),25 with double-row methods demonstrating a greater degree of structural healing than single-row.26 Despite these promising results, no definitive conclusion regarding subjective patient outcomes between repair techniques can be drawn.27 In light of this ambiguity, it is also worth considering the additional operative time and cost associated with the double-row. Advantages and disadvantages of the technique can be found in Table 2.
Table 2.
Advantages and Disadvantages of the Transosseous-Equivalent Double-Row Technique Versus Single-Row Suture Repair
| Advantages | Disadvantages |
|---|---|
| Provides more pressurized contact area | Equivocal improvement in clinical outcomes |
| Restores a greater percentage of footprint | Longer operating times |
| Higher load to failure | Greater cost |
| Less gap formation at repair site | |
| Lower incidence of retears |
Although ARCR outcomes are generally good, the procedure is not without complications. Some potential complications include injury to the suprascapular or axillary nerves, stiffness (the incidence as well as the duration can be lessened by aggressive physical rehabilitation), deltoid detachment (open repair only), recurrent tendon tear (most commonly secondary to failure of cuff tissue to heal, resulting in suture pull out), and infection.28
As patients continue to achieve greater long-term follow-up with double-row techniques, it will be worth re-examining whether outcomes between single- and double-row methods remain similar.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
The patient is placed in the lateral decubitus position. The right arm is placed in 40°-50° of abduction and 15° of forward flexion. The arthroscope is then directed into the subacromial space. The footprint is prepared using the shaver. An awl is used to create sockets for the suture anchors, which are placed at an angle of 45° relative to the plane of the tuberosity. Double-loaded, 4.5-mm screw-in suture anchors are placed into the previously created sockets. Sutures are then retrieved individually and passed in a horizontal mattress fashion using a suture-passing device across the entire breadth of the tear. To secure the posterior edge of the tear, and to avoid the potential for dog-ear formation, a suture cinch stitch prelooped at one end is passed. The free end of the suture snare is passed and secured through the looped end. The anterior tear edge is secured in similar fashion with a second cinch stitch. The mattress sutures are then tied individually. Typically 2 lateral row anchors are used. Alternating sutures are retrieved from the lateral portal and passed through the eyelet of the knotless lateral row anchor. An awl is used to create the socket for the anchor, which should be placed just lateral to the footprint in the greater tuberosity. The anchor is placed into the socket. The anchor is then fully seated, and the sutures are cut flush with the anchor.
References
- 1.Burkhart S.S., Lo I.K. Arthroscopic rotator cuff repair. J Am Acad Orthop Surg. 2006;14:333–346. doi: 10.5435/00124635-200606000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Itoi E. Rotator cuff tear: Physical examination and conservative treatment. J Orthop Sci. 2013;18:197–204. doi: 10.1007/s00776-012-0345-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolf B.R., Dunn W.R., Wright R.W. Indications for repair of full-thickness rotator cuff tears. Am J Sports Med. 2007;35:1007–1016. doi: 10.1177/0363546506295079. [DOI] [PubMed] [Google Scholar]
- 4.Ozbaydar M., Elhassan B., Esenyel C. A comparison of single- versus double-row suture anchor techniques in a simulated repair of the rotator cuff: An experimental study in rabbits. J Bone Joint Surg Br. 2008;90:1386–1391. doi: 10.1302/0301-620X.90B10.20862. [DOI] [PubMed] [Google Scholar]
- 5.Nelson C.O., Sileo M.J., Grossman M.G., Serra-Hsu F. Single-row modified Mason-Allen versus double-row arthroscopic rotator cuff repair: A biomechanical and surface area comparison. Arthroscopy. 2008;24:941–948. doi: 10.1016/j.arthro.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Ensor K.L., Kwon Y.W., Dibeneditto M.R., Zuckerman J.D., Rokito A.S. The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg. 2013;22:1628–1632. doi: 10.1016/j.jse.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Dines J.S., Bedi A., ElAttrache N.S., Dines D.M. Single-row versus double-row rotator cuff repair: Techniques and outcomes. J Am Acad Orthop Surg. 2010;18:83–93. doi: 10.5435/00124635-201002000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Bishop J.Y., Santiago-Torres J.E., Rimmke N., Flanigan D.C. Smoking predisposes to rotator cuff pathology and shoulder dysfunction: A systematic review. Arthroscopy. 2015;31:1598–1605. doi: 10.1016/j.arthro.2015.01.026. [DOI] [PubMed] [Google Scholar]
- 9.Rudzki J.R., Adler R.S., Warren R.F. Contrast-enhanced ultrasound characterization of the vascularity of the rotator cuff tendon: Age- and activity-related changes in the intact asymptomatic rotator cuff. J Shoulder Elbow Surg. 2008;17:96S–100S. doi: 10.1016/j.jse.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Curtis A.S., Burbank K.M., Tierney J.J., Scheller A.D., Curran A.R. The insertional footprint of the rotator cuff: An anatomic study. Arthroscopy. 2006;22:609.e601. doi: 10.1016/j.arthro.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: An anatomic description of the shoulder's “suspension bridge”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 12.Dugas J.R., Campbell D.A., Warren R.F., Robie B.H., Millett P.J. Anatomy and dimensions of rotator cuff insertions. J Shoulder Elbow Surg. 2002;11:498–503. doi: 10.1067/mse.2002.126208. [DOI] [PubMed] [Google Scholar]
- 13.Apreleva M., Ozbaydar M., Fitzgibbons P.G., Warner J.J. Rotator cuff tears: The effect of the reconstruction method on three-dimensional repair site area. Arthroscopy. 2002;18:519–526. doi: 10.1053/jars.2002.32930. [DOI] [PubMed] [Google Scholar]
- 14.Rodeo S.A., Arnoczky S.P., Torzilli P.A., Hidaka C., Warren R.F. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am. 1993;75:1795–1803. doi: 10.2106/00004623-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Oguma H., Murakami G., Takahashi-Iwanaga H., Aoki M., Ishii S. Early anchoring collagen fibers at the bone-tendon interface are conducted by woven bone formation: Light microscope and scanning electron microscope observation using a canine model. J Orthop Res. 2001;19:873–880. doi: 10.1016/S0736-0266(01)00021-3. [DOI] [PubMed] [Google Scholar]
- 16.Tuoheti Y., Itoi E., Yamamoto N. Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med. 2005;33:1869–1874. doi: 10.1177/0363546505278256. [DOI] [PubMed] [Google Scholar]
- 17.Mazzocca A.D., Millett P.J., Guanche C.A., Santangelo S.A., Arciero R.A. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33:1861–1868. doi: 10.1177/0363546505279575. [DOI] [PubMed] [Google Scholar]
- 18.Kim D.H., Elattrache N.S., Tibone J.E. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34:407–414. doi: 10.1177/0363546505281238. [DOI] [PubMed] [Google Scholar]
- 19.Smith C.D., Alexander S., Hill A.M. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88:2425–2431. doi: 10.2106/JBJS.E.00697. [DOI] [PubMed] [Google Scholar]
- 20.Meier S.W., Meier J.D. The effect of double-row fixation on initial repair strength in rotator cuff repair: A biomechanical study. Arthroscopy. 2006;22:1168–1173. doi: 10.1016/j.arthro.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Mahar A., Tamborlane J., Oka R., Esch J., Pedowitz R.A. Single-row suture anchor repair of the rotator cuff is biomechanically equivalent to double-row repair in a bovine model. Arthroscopy. 2007;23:1265–1270. doi: 10.1016/j.arthro.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Franceschi F., Ruzzini L., Longo U.G. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: A randomized controlled trial. Am J Sports Med. 2007;35:1254–1260. doi: 10.1177/0363546507302218. [DOI] [PubMed] [Google Scholar]
- 23.Burks R.T., Crim J., Brown N., Fink B., Greis P.E. A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: Magnetic resonance imaging and early clinical evaluation. Am J Sports Med. 2009;37:674–682. doi: 10.1177/0363546508328115. [DOI] [PubMed] [Google Scholar]
- 24.Grasso A., Milano G., Salvatore M., Falcone G., Deriu L., Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: A prospective randomized clinical study. Arthroscopy. 2009;25:4–12. doi: 10.1016/j.arthro.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 25.Millett P.J., Warth R.J., Dornan G.J., Lee J.T., Spiegl U.J. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: A systematic review and meta-analysis of Level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23:586–597. doi: 10.1016/j.jse.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Mascarenhas R., Chalmers P.N., Sayegh E.T. Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: A systematic review of overlapping meta-analyses. Arthroscopy. 2014;30:1156–1165. doi: 10.1016/j.arthro.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 27.Ying Z.M., Lin T., Yan S.G. Arthroscopic single-row versus double-row technique for repairing rotator cuff tears: A systematic review and meta-analysis. Orthop Surg. 2014;6:300–312. doi: 10.1111/os.12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Audige L., Blum R., Muller A.M., Flury M., Durchholz H. Complications following arthroscopic rotator cuff tear repair: A systematic review of terms and definitions with focus on shoulder stiffness. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115587861. 2325967115587861. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the lateral decubitus position. The right arm is placed in 40°-50° of abduction and 15° of forward flexion. The arthroscope is then directed into the subacromial space. The footprint is prepared using the shaver. An awl is used to create sockets for the suture anchors, which are placed at an angle of 45° relative to the plane of the tuberosity. Double-loaded, 4.5-mm screw-in suture anchors are placed into the previously created sockets. Sutures are then retrieved individually and passed in a horizontal mattress fashion using a suture-passing device across the entire breadth of the tear. To secure the posterior edge of the tear, and to avoid the potential for dog-ear formation, a suture cinch stitch prelooped at one end is passed. The free end of the suture snare is passed and secured through the looped end. The anterior tear edge is secured in similar fashion with a second cinch stitch. The mattress sutures are then tied individually. Typically 2 lateral row anchors are used. Alternating sutures are retrieved from the lateral portal and passed through the eyelet of the knotless lateral row anchor. An awl is used to create the socket for the anchor, which should be placed just lateral to the footprint in the greater tuberosity. The anchor is placed into the socket. The anchor is then fully seated, and the sutures are cut flush with the anchor.