Case
A 50-year-old woman experiences jaw discomfort while at work. It increases in intensity, accompanied by diaphoresis and nausea. An ambulance is called 40 minutes after symptom onset. On arrival to the emergency department, the woman has moderate pain, a blood pressure of 150/85 mm Hg and a heart rate of 90 beats/min. Results of cardiovascular and respiratory examinations are normal. The 12-lead electrocardiogram (ECG) is shown in Fig. 1.
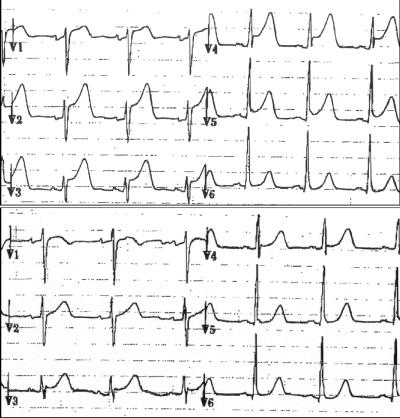
Fig. 1: Top: ECG taken soon after admission to emergency department, showing ST-segment elevation of 2–4 mm in precordial leads V1–V5. Bottom: ECG taken 35 minutes after the administration of fibrinolysis, showing nearly complete resolution of ST-segment elevation.
Question: What is the diagnosis for this patient?
Comment: This is a typical presentation of acute myocardial infarction (MI), although less usual in a woman of her age. A crucial factor in this case is the rapid call for help and the prompt ambulance response, enhancing the potential for myocardial salvage with reperfusion. The ECG shows an ST-segment elevation of 2–4 mm in precordial leads V1–V5 (Fig. 1), which suggests an acute MI of the anterior wall.
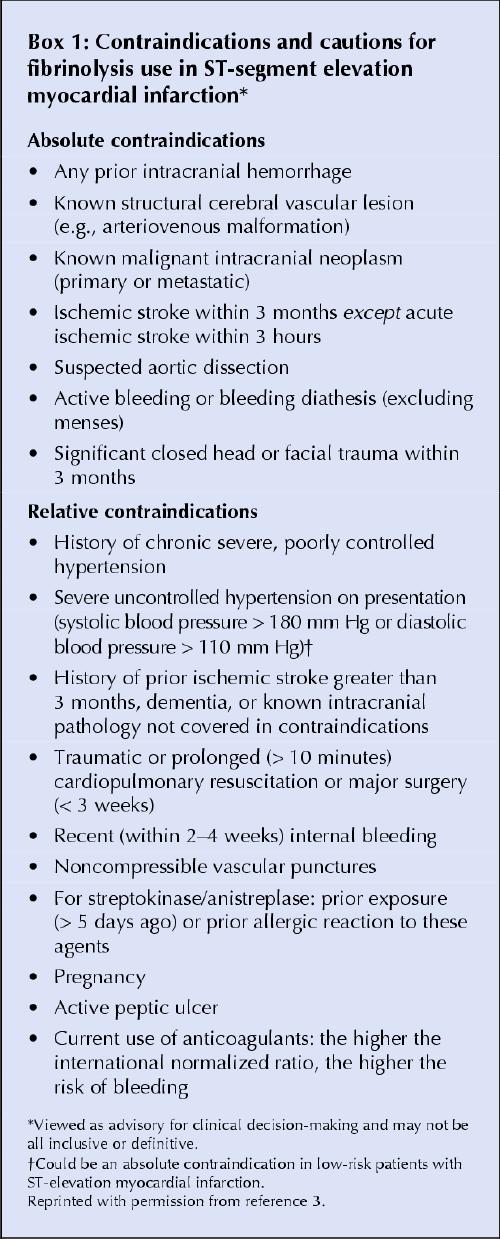
Question: The patient has had symptoms of acute MI for less than 90 minutes, and you determine that she requires reperfusion. She has no contraindications to fibrinolysis (see Box 1). You work in a community hospital that is 90 minutes away from a centre that performs percutaneous coronary interventions (PCIs). Should the patient be treated with fibrinolytic therapy, or should she be referred to a tertiary care centre for a PCI?
Box 1.
Comment: Reperfusion in ST-segment elevation MI (STEMI) limits myocardial damage and reduces mortality by about 30%, or even more in this case since the ischemic time is relatively short. The crucial concept is that saving time to reperfusion saves lives.2 The decision to treat with immediate fibrinolysis or transfer to a tertiary cardiac centre for primary angioplasty should be made quickly. A directed history and physical examination should be completed within 5–10 minutes after the patient is promptly seen so that a rapid 2-stage decision can be made: (1) Is reperfusion indicated (see Box 1)? and (2) Which reperfusion strategy should it be (Fig. 2)?
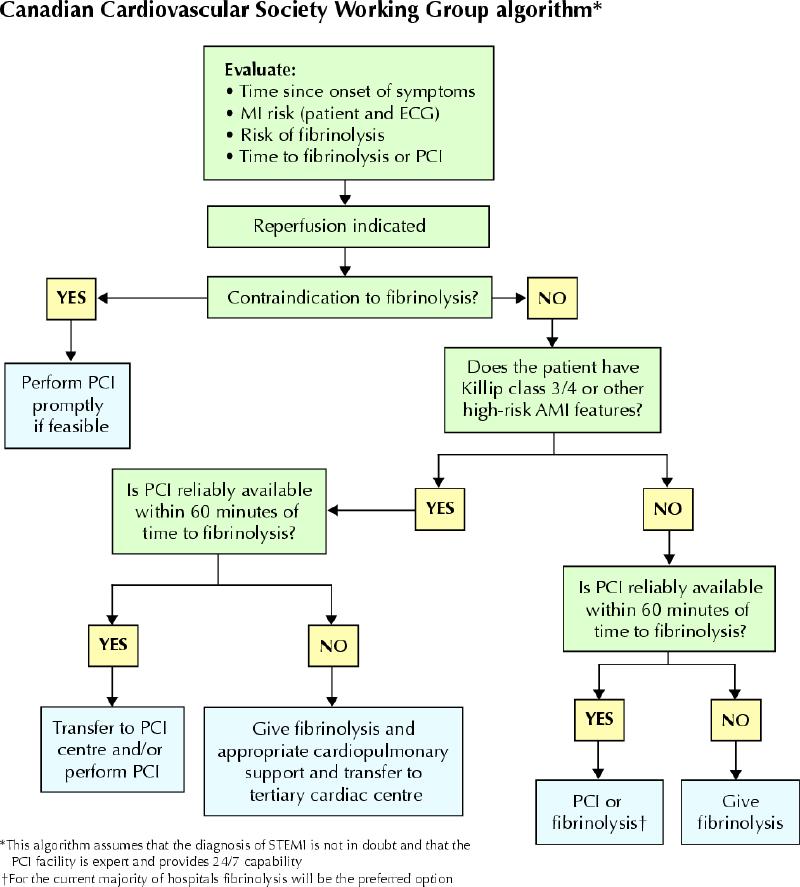
Fig. 2: Canadian Cardiovascular Society Working Group algorithm for the selection of patients for reperfusion after ST-segment myocardial infarction (STEMI). The algorithm applies to patients presenting within 12 hours after symptom onset; it assumes that the diagnosis of STEMI is not in doubt and indicates that, for the current majority of hospitals caring for non-high-risk STEMI patients, fibrinolysis is the preferred option. ECG = electrocardiogram, PCI = percutaneous coronary intervention. Reproduced with permission from reference 4.
In this case, because the patient is hemodynamically stable and has no heart failure or contraindications to fibrinoysis, and because transfer for PCI would impose a further treatment delay, largely exceeding 60 minutes, fibrinolysis is the preferred option.3
Question: What if your community hospital is within 30 minutes from a centre that could perform a PCI and therefore both fibrinolysis and angioplasty are possible within appropriate time frames? What treatment option should be favoured?
Comment: We believe that both options would be acceptable and that it is reasonable in this case to select immediate on-site fibrinolysis because (a) the patient is not at very high risk in terms of her clinical presentation (no evidence of heart failure or hemodynamic instability; (b) the ischemic time is less than 3 hours, a time frame when fibrinolysis is most effective;2,3 and (c) the fibrinolytic risk of major bleeding is low. Commonly used fibrinolytics in Canada are the bolus agents tenecteplase and reteplase; tissue plasminogen activator (tPA), also fibrin-specific, administered as a bolus but requiring a 90-minute step-down infusion; and the non-fibrin-specific agent streptokinase, which is given over an hour. Bolus agents are easier to administer, and the fibrin-specific agents act more quickly than streptokinase3 and have a lower mortality, especially in higher-risk cases. However, compared with streptokinase, they have a higher cost (about $2000 v. $400) and a slightly greater risk of cerebral hemorrhage (about 0.2% absolute excess), especially among elderly hypertensive women with a low body weight. Heparin is a necessary conjunctive therapy with fibrin-specific agents to sustain an antithrombotic effect.
Question: What other medications should be given to this patient?
Comment: The use of ASA alone reduces mortality by 20%– 25%, and chewing the tablets ensures a rapid effect.1 Adequate analgesia (e.g., morphine given intravenously) relieves discomfort and its deleterious effect on myocardial demand. Finally, intravenous β-blocker therapy should be given in the absence of contraindications, with an aim for an optimal heart rate of 50–60 beats/min and a systolic blood pressure of not less than 90–100 mm Hg. A standard protocol is 3 boluses of 5 mg of metoprolol given intravenously every 5–10 minutes.
Question: The patient's discomfort decreases significantly from its peak, 35 minutes after administration of the fibrinolytic agent. An ECG shows nearly complete resolution of the ST-segment elevation (Fig. 1, bottom panel). Fifty minutes later the ST-segment returns to normal, and the patient is asymptomatic. How should this be interpreted?
Comment: This patient has clear evidence of successful myocardial reperfusion. A decrease of 50%– 70% or more in the ST-segment elevation is an excellent indication of successful reperfusion.3 Besides continuous monitoring of the ECG lead with the greatest baseline ST-segment elevation, it is appropriate to obtain 12-lead ECGs every 15–30 minutes for about 1–3 hours immediately after fibrinolysis is begun, especially if rescue angioplasty may be an option.
Question: What if the patient's symptoms or ST-segment elevation do not resolve?
Comment: Had reperfusion not been successful and there was continuing evidence of myocardial ischemia, prompt transfer to a tertiary care facility for consideration of rescue PCI would have been a reasonable option.4 Rescue angioplasty should be considered if there has not been at least 50% resolution of the ST-segment elevation and significant reduction of pain and discomfort within 60–90 minutes after fibrinolysis. Rescue angioplasty should also be considered if ST-segment elevation recurs after an initially favourable response.
Question: If the patient has no complications, what other investigations should be performed in hospital?
Comment: Echocardiography and a symptom-limited modified Bruce protocol treadmill test are simple measures of cardiac function and reserve that should be performed while the patient is in hospital.
The risk of early recurrent ischemia after fibrinolysis is about 10%–15%, and the risk of reinfarction is less than 5%. The treadmill test is an excellent and noninvasive means of stratifying risk by evaluating coronary artery reserve and functional capacity. It can be performed early after infarction, depending on the patient's general condition, rapidity and ease of ambulation, and size of infarction. The ability to perform a stress test at a workload of 5–7 or more metabolic equivalents (METs) without a drop in blood pressure carries an excellent prognosis. Other favourable features are the absence of limiting angina, significant ventricular arrhythmias and marked ST-segment depression. Unfavourable results should prompt consideration of coronary angiography and revascularization as appropriate.
Question: What other treatments should be started for this patient?
Comment: The importance of an effective secondary prevention strategy aimed at comprehensive control of risk factors cannot be overemphasized. This patient has a strong family history of premature coronary artery disease and other risk factors, including smoking, hypertension and dyslipidemia. Her only medications are a multivitamin and hormone replacement therapy. Treatment with ASA (160 mg/d), a β-blocker, an angiotensin-converting-enzyme inhibitor and a statin should be started; the patient should be advised to stop the hormone replacement therapy. She should also receive counselling on diet, smoking cessation, weight loss and exercise. A follow-up visit should be planned for 1 month after discharge from hospital. If this option is available, the patient should be encouraged to enter a cardiac rehabilitation program.
Peter Bogaty Quebec Heart Institute Laval Hospital Sainte-Foy, Que. Christopher E. Buller Division of Cardiology St. Paul's Hospital University of British Columbia Vancouver, BC Paul Dorian Department of Medicine St. Michael's Hospital University of Toronto Toronto, Ont. Blair J. O'Neill Department of Medicine Dalhousie University Halifax, NS Paul W. Armstrong Department of Medicine University of Alberta Edmonton, Alta.
β See related article page 1042
Footnotes
The authors constitute the Canadian Cardiovascular Society Working Group, formed to review the new American College of Cardiology / American Heart Association STEMI guidelines and to adapt them for Canadian practice. In this first of 2 articles, they describe a case illustrating the selection of patients for reperfusion immediately after STEMI.
Competing interests: Dr. Armstrong has received research funding from Hoffman-LaRoche, Aventis, Boehringer Ingelheim, and educational and consultant funding from Hoffmann-LaRoche and Aventis. Dr. Dorian received speaker fees from Guidant Corp., Medtronic Inc., and St. Jude Medical Inc.
References
- 1.Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet 1988;2:349-60. [PubMed]
- 2.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 1996;348:771-5. [DOI] [PubMed]
- 3.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004;110: 588-636. [DOI] [PubMed]
- 4.Armstrong PW, Bogaty P, Buller CE, Dorian P, O'Neill BJ. The 2004 ACC/ AHA Guidelines: a perspective and adaptation for Canada by the Canadian Cardiovascular Society Working Group. Can J Cardiol 2004; 20 (11):1075-79. [PubMed]


