Abstract
Shoulder instability is often associated with an impaction fracture of the humeral head, commonly referred to as a “Hill-Sachs lesion.” This lesion is present in both anterior and posterior instability. Forty percent to 90% of anterior shoulder dislocations have associated Hill-Sachs lesions, whereas 29% to 86% of posterior shoulder dislocations have reverse Hill-Sachs lesions. Both of these lesions can contribute to recurrent instability of the shoulder and require surgery to be treated. Currently, the most common procedures to address Hill-Sachs lesions are the remplissage procedure (transfer of the infraspinatus into the posterior humeral head defect), capsular shift, disimpaction technique, humeral head resurfacing, bone block transfer, or shoulder arthroplasty. Reverse Hill-Sachs lesions are managed with similar procedures, such as the remplissage-equivalent technique described by McLaughlin, which involves transfer of the subscapularis tendon to fill the humeral head defect. The procedure has the advantage of “exteriorizing” the humeral head defect, but in the case of large lesions, it can result in significant loss of the articulating articular surface. The purpose of this article is to describe an arthroscopically assisted disimpaction technique with supplemental grafting using a balloon osteoplasty technique for a reverse Hill-Sachs lesion with bone cement to support and maintain the reduction.
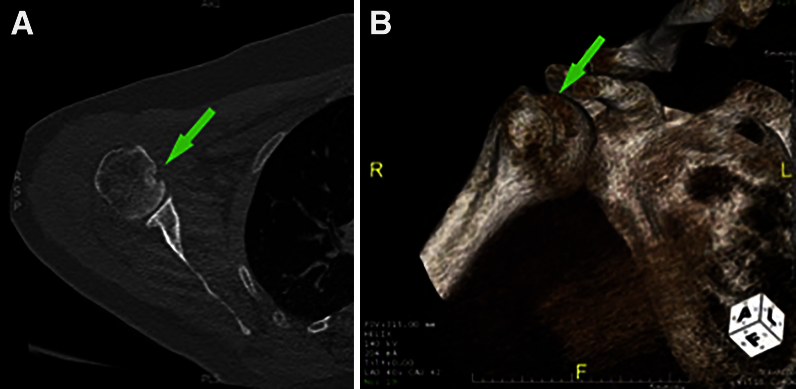
A Hill-Sachs lesion is a compression fracture on the posterosuperolateral aspect of the humeral head, which most commonly occurs during an anterior glenohumeral instability injury. The incidence of Hill-Sachs lesions is estimated to be 40% to 90% among anterior shoulder instability events. A reverse Hill-Sachs lesion is an anteromedial humeral head impression fracture that is caused by a posterior shoulder dislocation (Fig 1).1 Reverse Hill-Sachs lesions can contribute to recurrent instability of the shoulder, especially when comprising greater than 25% of the articular surface of the humeral head.1, 2, 3 Posterior locked shoulder dislocations are rare, accounting for fewer than 3% of all shoulder dislocations, and they are usually caused by epileptic seizures, high-energy trauma, or electrocution.4
Fig 1.
(A) Axial computed tomography image showing a reverse Hill-Sachs lesion (arrow). (B) Anterior aspect of a 3-dimensional computed tomography rendition of the reverse Hill-Sachs lesion (arrow). (F, foot; L, left; R, right.)
Recurrent or persistent shoulder instability is an indication for surgery. Failure to address a corresponding Hill-Sachs lesion places the shoulder at an increased risk of recurrence.5, 6 Numerous ways to treat a Hill-Sachs lesion have been described. One treatment option is to constrain the glenohumeral joint through a capsular shift to limit external rotation and thus prevent the Hill-Sachs lesion from engaging. Other methods that have been described are filling the defect with osteoarticular allograft, transferring the subscapularis tendon into the reverse Hill-Sachs lesion (McLaughlin procedure), transferring the infraspinatus tendon into the Hill-Sachs lesion (remplissage procedure), performing a proximal humeral osteotomy, or even performing a total shoulder or reverse total shoulder arthroplasty to address the issue of humeral head loss.7, 8, 9, 10
Recently, acute reduction of Hill-Sachs lesions has been described using percutaneous osteoplasty methods to fill the humeral head defect and thus restore the articular surface of the humeral head. These techniques originally involved humeral head reduction with bone tamps through a cortical window. Kazel et al.11 used the term “humeroplasty” to describe this fixation. More recently, Sandmann et al.12 described the use of a kyphoplasty balloon with subsequent filling of the defect with bone substitute (similar to the fixation of a vertebral compression fracture), which they performed on cadaveric specimens. Stachowicz et al.13 described the same technique used on cadavers. To our knowledge, there is only one mention of this technique being used in live patients: Jacquot et al.14 used fluoroscopic guidance to perform a humeroplasty on 4 different shoulders with reverse Hill-Sachs lesions. However, they did not use arthroscopy to aid in the reduction. The purpose of this article is to describe the use of a balloon osteoplasty with simultaneous use of fluoroscopic guidance and arthroscopy to observe reduction of a reverse Hill-Sachs lesion, which—to our knowledge—has never been reported in the literature.
Technique
Setup, Positioning, and Labral Repair
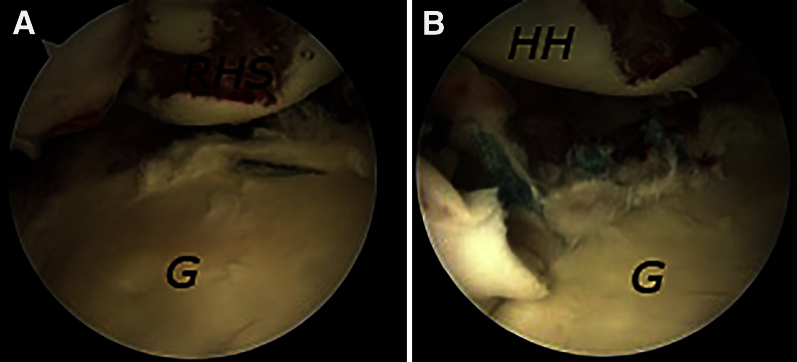
The patient is placed in the lateral decubitus position. Standard posterior, anterior, superior, midglenoid, and posterolateral portals are used during the case. An initial diagnostic arthroscopy of the shoulder is performed, with inspection of the labrum, anteriorly and posteriorly. If a tear is found, then it is fixed with suture anchors (Fig 2).
Fig 2.
(A) View from the anterior portal showing a posterior labral tear and reverse Hill-Sachs lesion (RHS) of the humeral head. (B) Same view after the posterior labrum is repaired with 3 suture anchors. (G, glenoid; HH, humeral head.)
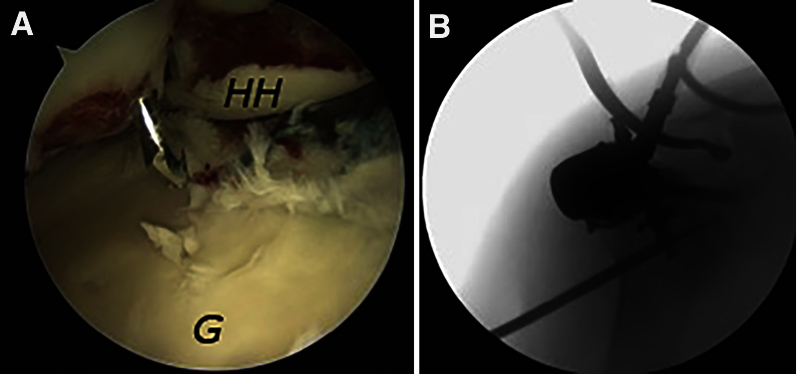
Positioning of Guide and Reduction of Hill-Sachs Lesion
Under arthroscopic visualization, an anterior cruciate ligament (ACL) guide is introduced through the posterior portal while the surgeon is viewing from the anterosuperior portal (Fig 3). The drill guide is positioned to ensure that its start point is well below the axillary nerve's path along the deltoid, approximately 10 cm below the lateral border of the acromion (Fig 3). A small, 5-mm incision is made over the skin, and the underlying soft tissues are bluntly spread until the humerus is encountered. A sweeping motion allows for blunt clearance of surrounding soft tissues. By use of a drill guide to protect the surrounding soft tissues, a 5-mm unicortical drill is used to penetrate the humeral head and is directed superiorly through the humerus toward the intra-articular aim point on the ACL guide. The correct trajectory is confirmed by a combination of fluoroscopy and direct arthroscopic visualization (Fig 4). Once the tip of the drill abuts the reverse Hill-Sachs defect, the drill is used to lightly manipulate and unlock the fragments of the fracture and grossly correct the joint surface.
Fig 3.
In the lateral position, viewing from posteriorly, an anterior cruciate ligament guide is placed against the humeral head (HH) defect to accurately place the guide pin. (G, glenoid.)
Fig 4.
(A) In the lateral position, viewing from the anterior portal, the drill bit is shown exiting the humeral head (HH) defect, serving as a guide pin for the cannula. The cannula will be used to introduce the balloon, which is deployed to reduce the Hill-Sachs defect. (G, glenoid.) (B) Anteroposterior fluoroscopic picture of the drill exiting the humeral head defect.
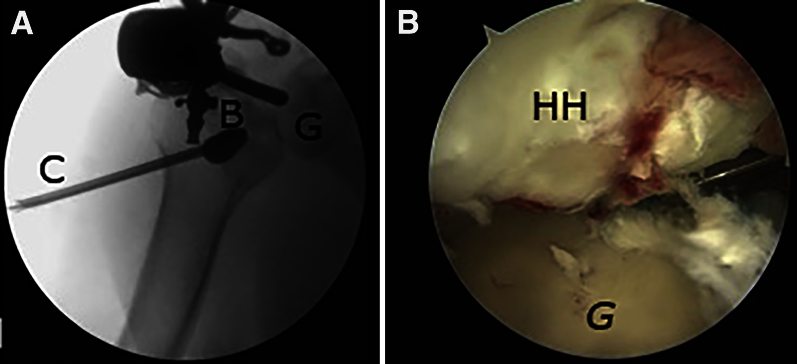
Balloon Placement and Fixation
Next, a Kyphon balloon system (Medtronic, Minneapolis, MN) is inserted and the pressure is inflated to approximately 150 mm Hg (Fig 5). C-arm and direct visualization through the arthroscopic camera is used to directly observe restoration of the joint surface. An arthroscopic liberator can be inserted through an accessory portal to ensure that the fragment is not over-reduced. If the fragment becomes dislodged, the surgeon must make a decision, weighing attempted closed versus open reduction and fixation options versus abandonment of the technique depending on the size of the resultant defect. The balloon osteoplasty device is removed, and a calcium phosphate filler (Medtronic) is inserted to eliminate the defect and reinforce the restored articular surface (Fig 6). An amount of 5 to 10 cm3 of bone filler is generally sufficient to backfill the defect. Arthroscopic visualization is used to confirm there is no extrusion of the product into the joint. Once the calcium phosphate sets, the reduced Hill-Sachs lesion is probed for stability. After this is confirmed with dynamic range of motion under arthroscopic visualization, all arthroscopic equipment is removed and the wounds are closed and dressed sterilely.
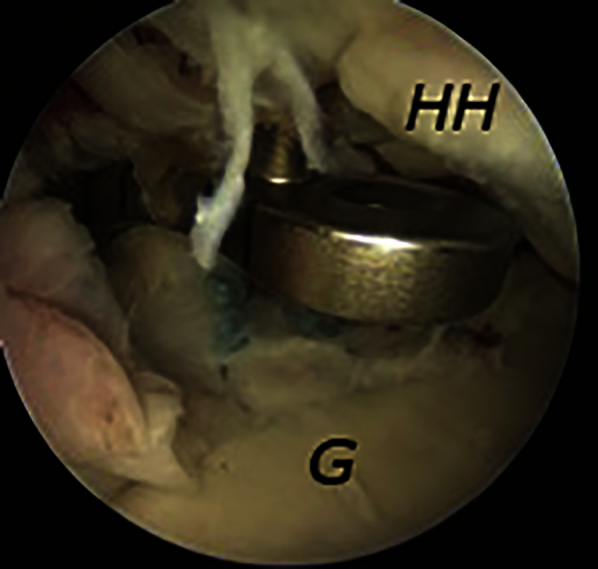
Fig 5.
(A) Insertion of the cannula (C) and inflation of the balloon (B) to 150 mm Hg, facilitating reduction of the Hill-Sachs lesion. (B) In the lateral position, viewing from the posterior portal, the humeral head (HH) defect is shown, after it has been reduced by the balloon (visualized in A). (G, glenoid.)
Fig 6.
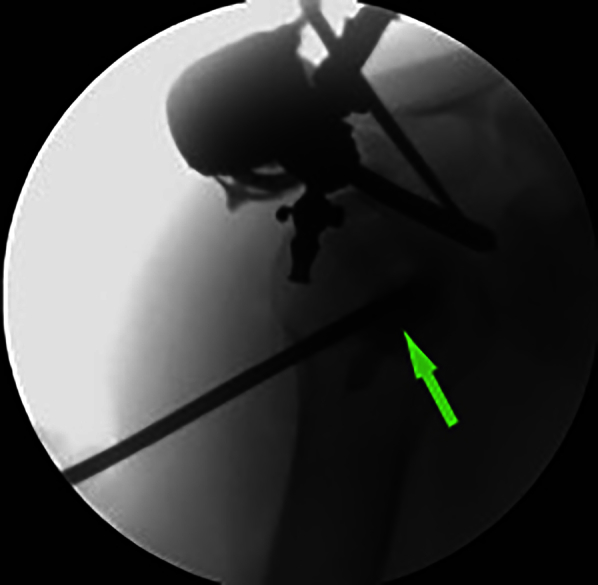
Fluoroscopic image showing insertion of the cannula with injection of calcium phosphate (visualized as density in the humeral head [arrow]) to fill the void left after the Hill-Sachs lesion has been reduced.
Postoperative Care
The patient is placed in a sling (an abduction pillow can be used if a reverse Hill-Sachs lesion is present). The patient is kept in the sling for 6 weeks, with hand, wrist, and elbow exercises allowed immediately. Shoulder pendulum exercises are instituted immediately. Passive range of motion is limited to neutral internal rotation, 30° of external rotation, and 90° of forward elevation for 6 weeks. At the 6-week visit, radiographs are taken to confirm adequate position of the reduction, and strengthening can begin.
Discussion
Traumatic shoulder instability resulting in a large Hill-Sachs or reverse Hill-Sachs lesion presents a challenge for the shoulder surgeon to treat. There are several techniques used to treat these lesions including a capsular shift, remplissage (for a Hill-Sachs lesion) or McLaughlin procedure (for a reverse Hill-Sachs lesion), bone block transfers such as the Latarjet procedure, disimpaction, or arthroplasty. In this article, we describe arthroscopic reduction and balloon osteoplasty with fixation using bone cement as an alternative treatment option. This type of fixation has not been previously reported in human subjects to our knowledge. Video 1 shows this method being performed on an acute reverse Hill-Sachs lesion, but the same technique can be used in the treatment of a standard Hill-Sachs lesion.
Recently, cortical bone tamps have been used as an alternative to the aforementioned methods to anatomically reduce and fill the humeral head defect. Kazel et al.11 were the first authors to coin the term “humeroplasty,” when they created Hill-Sachs lesions in 14 cadaveric specimens and then used a curved bone tamp to significantly reduce the size of the lesions. Sandmann et al.12 advanced the technique further and used a kyphoplasty balloon to reduce the size of a Hill-Sachs lesion. They used 6 cadaveric specimens for their study and showed that a balloon kyphoplasty system could reduce the size of a Hill-Sachs lesion by 80%, but they noted that further studies needed to be performed to evaluate the technique under arthroscopic conditions. Stachowicz et al.13 injected bone cement after using the kyphoplasty balloon. They used 18 cadaveric humeri and were able to show a 99.3% reduction to the original humeral head volume. Finally, Jacquot et al.14 were the first surgeons in the literature to perform humeroplasty on reverse Hill-Sachs lesions with balloon kyphoplasty and bone cement in live patients. They performed the operation in 3 patients and used fluoroscopic guidance to aid in the placement of the kyphoplasty balloon to ensure adequate reduction. In all 3 cases, the reverse Hill-Sachs lesion was well reduced; there were no recurrent dislocations; and all of the patients had resumed work and daily activities with no limitations.
In our technique, we use arthroscopy and an ACL guide to ensure adequate location of our cortical bone window in the lateral humerus. We also use fluoroscopic guidance to ensure good placement of the kyphoplasty balloon and bone cement. With this adaptation, we are able to provide a near anatomic reduction of a reverse Hill-Sachs lesion with preservation of the articular surface (Video 1). We believe this technique may be a promising approach in patients with acute, larger humeral head defects that require fixation.
Our technique has several advantages over other techniques for addressing humeral head defects. First, it allows for a relatively “anatomic” reduction of the defect. Second, the anatomy of the shoulder is minimally altered. There is no alteration of the rotator cuff muscles as would be seen with the McLaughlin or remplissage procedure. Furthermore, our technique may make subsequent surgical procedures technically easier. The main disadvantage of this technique is that it needs to be performed in a relatively acute setting. The precise definition of “acute” is unknown, however, because it is not known when or if these lesions become irreducible. There is a further risk that some of the articular cartilage fragment could dislodge into the joint. This could be dealt with subsequent shoulder arthroscopy and then conversion to the remplissage or McLaughlin procedure or shoulder arthroplasty. Advantages and disadvantages are shown in Table 1, and pearls and pitfalls can be found in Table 2.
Table 1.
Advantages and Disadvantages
| Advantages |
| Anatomic reduction of joint |
| Preservation of humeral head articular surface |
| Less alteration of native anatomy |
| Minimally invasive approach |
| Disadvantages |
| Technique may be limited to treating acute impaction fractures |
| Possibility of complications including cement extrusion, fragment dislodgement, and inadequate reduction with comminuted fragments |
| Insignificant research on outcomes to validate this technique |
Table 2.
Pearls and Pitfalls
| Pearls |
| Use proper portal placement to ensure access to the Hill-Sachs lesion and associated pathology. |
| Use a low-profile anterior cruciate ligament guide to allow accurate placement of the drill for fragment reduction. |
| Use a drill to manipulate the fragment or perform disimpaction with tamping to assist reduction. |
| Perform intra-articular placement of an arthroscopic liberator to prevent over-reduction or dislodgement of the fragment. |
| Slowly inflate the balloon while watching reduction under arthroscopy to avoid “over-reduction.” |
| Use an adequate amount of calcium phosphate to fill the defect. |
| Use a cautious approach to rehabilitation to prevent fragment dislodgement. |
| Pitfalls |
| Inadequate visualization or access to the Hill-Sachs lesion is possible. |
| Incorrect placement of the drill guide outer sleeve may place the axillary nerve at risk. |
| Overaggressive tamping may dislodge the fragment into the joint. |
| Improper cement technique can lead to extravasation of the cement into the joint or underfilling and fragment settling. |
| Overaggressive rehabilitation can lead to loss of reduction. |
Arthroscopically assisted reduction with internal fixation of an acute Hill-Sachs lesion is a promising approach in the patient with shoulder instability and an impaction fracture of the humeral head. The technique has been shown to reliably reduce these defects in cadaveric models, and we demonstrate its use in the clinical setting. Further study with larger numbers of patients and longer-term outcome with validated metrics is encouraged to determine the ultimate value of this approach.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.R. receives support from Arthroscopy Association of North America, Journal of Shoulder and Elbow Surgery, Orthopedics Today, and Hawkins Foundation (board member); Mitek and DePuy (paid consultant); and Arthrex (paid consultant and presenter). J.B. receives support from Arthroscopy Association of North America, Journal of Shoulder and Elbow Surgery, Orthopedics Today, and Hawkins Foundation (board member); Mitek and DePuy (paid consultant); and Arthrex (paid consultant and presenter). J.M.T. receives support from Arthroscopy Association of North America, Journal of Shoulder and Elbow Surgery, Orthopedics Today, and Hawkins Foundation (board member); Mitek and DePuy (paid consultant); and Arthrex (paid consultant and presenter).
Supplementary Data
Surgical technique for arthroscopic reduction and balloon humeroplasty in the treatment of acute Hill-Sachs lesions. The patient is positioned in the lateral decubitus position. Standard posterior, anterior, superior, midglenoid, and posterolateral portals are used in the shoulder. After a standard diagnostic evaluation of the shoulder is performed, the decision is made to perform an arthroscopic reduction and balloon humeroplasty. An anterior cruciate ligament guide is introduced through the posterior portal. The drill guide is positioned well below the axillary nerve's path, approximately 10 cm below the lateral border of the acromion, to penetrate the humeral head superiorly through the humerus. The drill is used to lightly manipulate and unlock the fragments of the reverse Hill-Sachs defect to correct the joint surface. A Kyphon balloon system is inserted and the pressure inflated to approximately 150 mm Hg. The balloon osteoplasty device is removed, and a calcium phosphate filler is inserted to eliminate the defect. Arthroscopic visualization is used to confirm there is no extrusion of the product into the joint. Once the calcium phosphate sets, the reduced Hill-Sachs lesion is probed for stability. After this is confirmed with dynamic range of motion under arthroscopic visualization, all arthroscopic equipment is removed and the wounds are closed and dressed sterilely.
References
- 1.Provencher M.T., Frank R.M., Leclere L.E. The Hill-Sachs lesion: Diagnosis, classification, and management. J Am Acad Orthop Surg. 2012;20:242–252. doi: 10.5435/JAAOS-20-04-242. [DOI] [PubMed] [Google Scholar]
- 2.Rouleau D., Hebert-Davies J. Incidence of associated injury in posterior shoulder dislocation: Systematic review of the literature. J Orthop Trauma. 2012;26:246–251. doi: 10.1097/BOT.0b013e3182243909. [DOI] [PubMed] [Google Scholar]
- 3.Saupe N., White L.M., Bleakney R. Acute traumatic posterior shoulder dislocation: MR findings. Radiology. 2008;248:185–193. doi: 10.1148/radiol.2481071003. [DOI] [PubMed] [Google Scholar]
- 4.Robinson C.M., Aderinto J. Posterior shoulder dislocations and fracture-dislocations. J Bone Joint Surg Am. 2005;87:639–650. doi: 10.2106/JBJS.D.02371. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 6.Steinmann S.P. Posterior shoulder instability. Arthroscopy. 2003;19(suppl 1):102–105. doi: 10.1016/j.arthro.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Bigliani L.U., Kurzweil P.R., Schwartzbach C.C., Wolfe I.N., Flatow E.L. Inferior capsular shift procedure for anterior-inferior shoulder instability in athletes. Am J Sports Med. 1994;22:578–584. doi: 10.1177/036354659402200502. [DOI] [PubMed] [Google Scholar]
- 8.Chapovsky F., Kelly J.D., IV Osteochondral allograft transplantation for treatment of glenohumeral instability. Arthroscopy. 2005;21:1007. doi: 10.1016/j.arthro.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Kropf E.J., Sekiya J.K. Osteoarticular allograft transplantation for large humeral head defects in glenohumeral instability. Arthroscopy. 2007;23:322.e1–322.e5. doi: 10.1016/j.arthro.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 10.McLaughlin H.L. Posterior dislocation of the shoulder. J Bone Joint Surg Am. 1952;24:584–590. [PubMed] [Google Scholar]
- 11.Kazel M.D., Sekiya J.K., Greene J.A., Bruker C.T. Percutaneous correction (humeroplasty) of humeral head defects (Hill-Sachs) associated with anterior shoulder instability: A cadaveric study. Arthroscopy. 2005;21:1473–1478. doi: 10.1016/j.arthro.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Sandmann G.H., Ahrens P., Schaeffeler C. Balloon osteoplasty—A new technique for minimally invasive reduction and stabilisation of Hill-Sachs lesions of the humeral head: A cadaver study. Int Orthop. 2012;36:2287–2291. doi: 10.1007/s00264-012-1644-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stachowicz R.Z., Romanowski J.R., Wissman R., Kenter K. Percutaneous balloon humeroplasty for Hill-Sachs lesions: A novel technique. J Shoulder Elbow Surg. 2013;22:e7–e13. doi: 10.1016/j.jse.2012.12.035. [DOI] [PubMed] [Google Scholar]
- 14.Jacquot F., Costil V., Werther J.R. Balloon treatment of posterior shoulder dislocation with reverse Hill-Sachs injury: Description of a new technique. Int Orthop. 2013;37:1291–1295. doi: 10.1007/s00264-013-1877-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for arthroscopic reduction and balloon humeroplasty in the treatment of acute Hill-Sachs lesions. The patient is positioned in the lateral decubitus position. Standard posterior, anterior, superior, midglenoid, and posterolateral portals are used in the shoulder. After a standard diagnostic evaluation of the shoulder is performed, the decision is made to perform an arthroscopic reduction and balloon humeroplasty. An anterior cruciate ligament guide is introduced through the posterior portal. The drill guide is positioned well below the axillary nerve's path, approximately 10 cm below the lateral border of the acromion, to penetrate the humeral head superiorly through the humerus. The drill is used to lightly manipulate and unlock the fragments of the reverse Hill-Sachs defect to correct the joint surface. A Kyphon balloon system is inserted and the pressure inflated to approximately 150 mm Hg. The balloon osteoplasty device is removed, and a calcium phosphate filler is inserted to eliminate the defect. Arthroscopic visualization is used to confirm there is no extrusion of the product into the joint. Once the calcium phosphate sets, the reduced Hill-Sachs lesion is probed for stability. After this is confirmed with dynamic range of motion under arthroscopic visualization, all arthroscopic equipment is removed and the wounds are closed and dressed sterilely.