Abstract
Plantar fibromatosis is a rare benign but often locally aggressive tumor of the plantar aponeurosis. Nonsurgical treatment is the first line of treatment for symptomatic lesions. Because of the high recurrence rate associated with surgical treatment, operation is indicated only when the lesions are highly symptomatic and conservative measures fail or the diagnosis is in question. The purpose of this technical note is to report the details of endoscopic subtotal fasciectomy. This may reduce the risks of skin necrosis and dehiscence, infection, and formation of painful hypertrophic scars.
Plantar fibromatosis is a rare benign but often locally aggressive tumor of the plantar aponeurosis.1, 2 Exacerbated proliferation of connective tissue produces thick collagen fibers, which forms slow growing irregular masses or nodules predominantly in the medial and central bands of the plantar aponeurosis.1 Alcoholic hepatic dysfunction, diabetes mellitus, use of anticonvulsants, and genetic factors may account for a higher risk of the disease.1 It is associated with palmar fibromatosis (Dupuytren's disease) and penile fibromatosis (Peyronie's disease).1, 2 Clinical and pathologic studies have classified plantar fibromatosis into 3 stages: (1) proliferative with increased activity of fibroblasts; (2) involutional with typical nodule formation; and (3) residual with a reduction of fibroblast activity, collagen maturation, and late tissue contractures.1, 3 Patients with plantar fibromatosis may or may not present with clinical symptoms.1, 2 Symptoms commonly include the feeling of a mass in the foot, difficulty in fitting shoes, and pain and tenderness while weightbearing.1, 2 The pain is sometimes disabling when the nodules increase in size due to an inflammatory reaction or if there is extension to the adjacent muscles or neurovascular structures.4 Associated toe deformity is rarely reported because the aponeurosis is not extended to the distal phalanges.4, 5, 6 No causal therapy is available, and treatment remains symptomatic.7 Nonsurgical treatment is the first line of treatment to reduce the progression of symptoms and includes intralesional cortisone or collagenase injections, stretching exercise, custom-molded orthotics, anti-inflammatory drugs, physical therapy, shockwave therapy, and radiotherapy.1, 2, 3, 7, 8 These modalities frequently do not halt the tumor progression, but they may decrease the patient's symptoms to a tolerable level.2 Because of the high recurrence rate associated with surgical treatment, operation is indicated only when the lesions are highly symptomatic and conservative measures fail or the diagnosis is in question.6, 9 The surgical options include local excision, wide excision, and subtotal and complete plantar fasciectomy.3, 6, 8 There is a high incidence of recurrence after both local and wide excision because of the diffuse nature of the lesion along the plantar aponeurosis.9 Subtotal plantar fasciectomy, however, has been reported to decrease the risk of recurrence in both primary and recurrent tumor cases.2, 3 Although adjuvant radiotherapy may result in improved local control, there are risks of radiation-induced impaired function of the foot, impaired wound healing, lymph edema, marked fibrosis, fracture of irradiated bone, and radiation-induced malignancy. In view of its potentially serious side effects, postoperative radiotherapy should be used highly selectively for this benign disease.6, 9
In this technical note, an endoscopic technique of subtotal fasciectomy is reported. It is indicated for highly symptomatic lesions that are unresponsive to conservative treatment. It is contraindicated if the lesions involve the deep muscles of the sole, the plantar skin, or the neurovascular bundles of the sole (Table 1).
Table 1.
Indications and Contraindications of Endoscopic Subtotal Fasciectomy of the Foot
| Indications | Contraindications |
|---|---|
| 1. Highly symptomatic lesions that are not responded to conservative treatment | 1. Lesions invading the deep muscles of the sole |
| 2. Lesions invading the plantar skin | |
| 3. Involvement of neurovascular bundles of the sole |
Technique
Preoperative Assessment and Patient Positioning
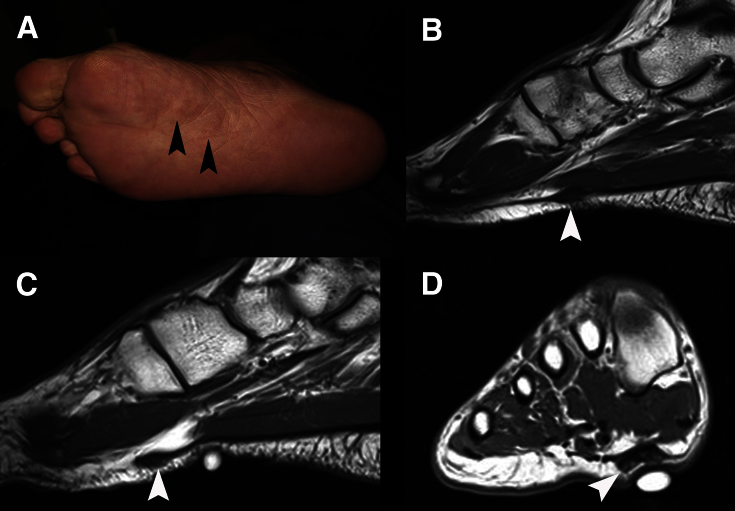
Nodules can be felt at the plantar aponeurosis, and usually involve the medial and central part of the aponeurosis. Magnetic resonance imaging can confirm the diagnosis and detect deep extension of the disease or the presence of other pathology (Fig 1).3
Fig 1.
Endoscopic subtotal fasciectomy of the right foot. (A) Clinical photograph of the illustrated case shows the 2 plantar fibromata (arrowheads). (B) Sagittal view of magnetic resonance imaging shows the proximal fibroma (arrowhead). (C) Sagittal view of magnetic resonance imaging shows the distal fibroma (arrowhead). (D) Coronal view of magnetic resonance shows that the lesion does not invade to the skin nor the underlying muscle (arrowhead).
The patient is in supine position with the legs spread. A thigh tourniquet is applied to provide a bloodless operative field. Fluid inflow is by gravity and no arthropump is used. A 4.0-mm 30° arthroscope (Dyonics, Smith & Nephew, Andover, MA) is used for this procedure.
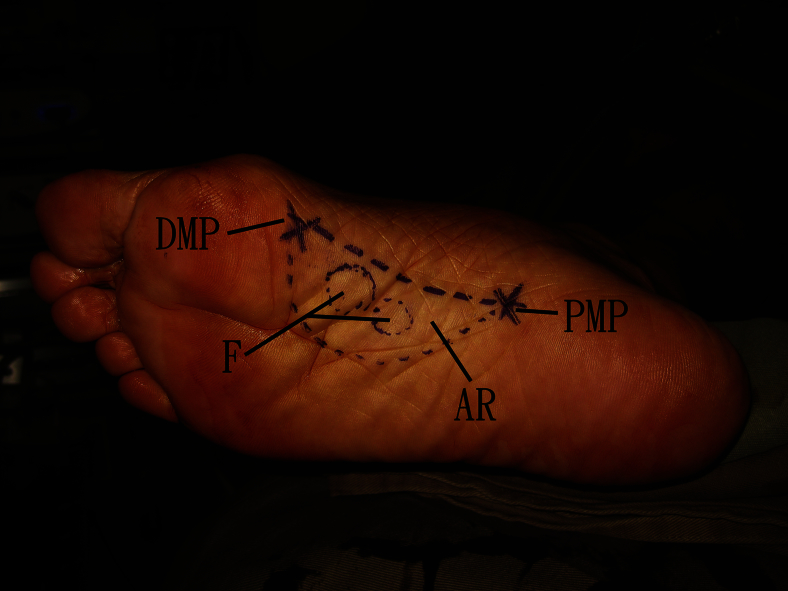
Portal Placement
The lesions and the planned area of resection (AR) of the plantar aponeurosis are outlined on the plantar skin. The resection margins are approximately 1.5 cm around the tumor except at the medial side that is limited by the medial edge of the plantar aponeurosis.2 This forms the roadmap of the subsequent endoscopic procedures. The proximal medial and distal medial portals are located at the proximal and distal ends of the medial edge of the AR, respectively (Fig 2). Longitudinal incisions of 1 to 1.5 cm are made at the portal sites. The subcutaneous tissue is bluntly dissected down to the plantar aponeurosis. The subcutaneous tissue between the portals is stripped from the aponeurosis by means of dental swabs via the portals. This is the initial working area of the procedure.
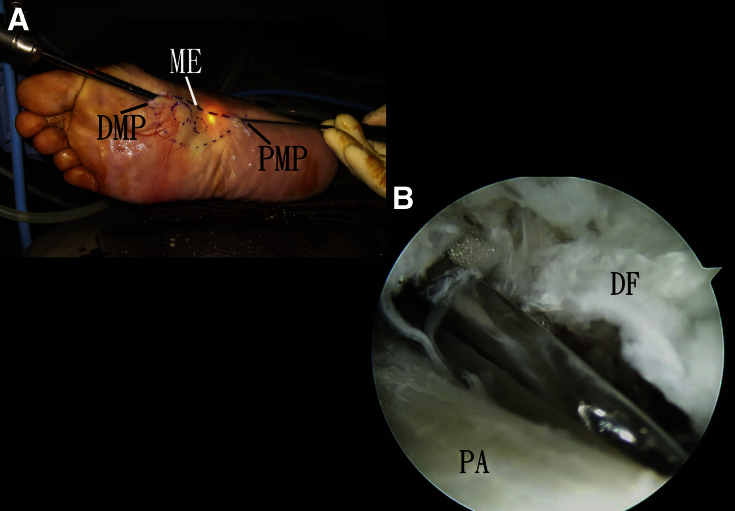
Fig 2.
Endoscopic subtotal fasciectomy of the right foot. The fibroma (F) and the planned area of resection (AR) of the plantar aponeurosis are outlined on the plantar skin. The resection margins are approximately 1.5 cm around the tumor except at the medial side that is limited by the medial edge of the plantar aponeurosis. The proximal medial (PMP) and distal medial (DMP) portals are located at the proximal and distal ends of the medial edge of the AR, respectively.
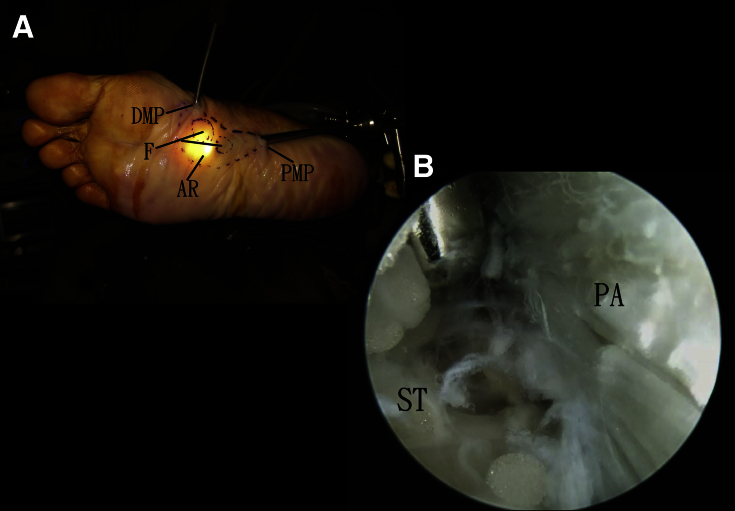
Endoscopic Release of the Superficial Surface of the Planned Area of Resection of the Plantar Aponeurosis
The proximal medial portal is the viewing portal. The subcutaneous tissue over the AR is stripped from the aponeurosis by an arthroscopic shaver (Dyonics, Smith & Nephew) or a small periosteal elevator via the distal medial portal (Fig 3). The subcutaneous tissue can be levered by the arthroscope when the camera is pushed dorsally fulcrum at the proximal medial portal. The cutting end of the shaver should not face toward the subcutaneous tissue to avoid damage to the dermal vasculature. There is no arthroscopic landmark of the boundary of the AR, especially its lateral limit. The shaver end can be easily palpated through the plantar skin and the area of arthroscopic visualization can be identified by the light spot of the arthroscope. The movement of the shaver should be in radial motion rather than sweeping motion centered at the distal medial portal. Release of the subcutaneous tissue close to the distal medial portal is important to avoid hindrance of further lateral motion of the shaver. Passive toe plantarflexion will tense up the aponeurosis and facilitate the dissection. The dissection should not go beyond the AR.
Fig 3.
Endoscopic subtotal fasciectomy of the right foot. The proximal medial portal is the viewing portal. The subcutaneous tissue over the AR is stripped from the aponeurosis by a small periosteal elevator (A) or an arthroscopic shaver (B) via the distal medial portal. (AR, planned area of resection of the plantar aponeurosis; DMP, distal medial portal; F, fibroma; PA, plantar aponeurosis; PMP, proximal medial portal; ST, subcutaneous tissue.)
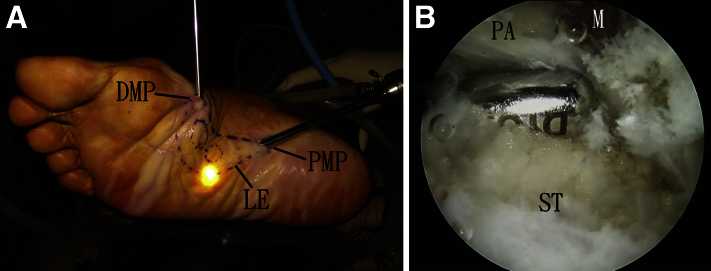
Endoscopic Release of the Lateral Edge of the Planned Area of Resection of the Plantar Aponeurosis
The proximal medial portal is the viewing portal. The light spot should go along the lateral outline of the AR. The lateral edge of the AR is released by an arthroscopic shaver and arthroscopic scissors (Arthrex, Naples, FL) (Fig 4). The surgeon should avoid dissection further into the underlying muscle. Passive toe plantarflexion will tense up the aponeurosis and facilitate the dissection. As the dissection is parallel to the axis of the foot at the distal portion of the lateral edge of the AR, the risk of injury to the emerging digital nerves is reduced when they cross the fascial extension to the toes.
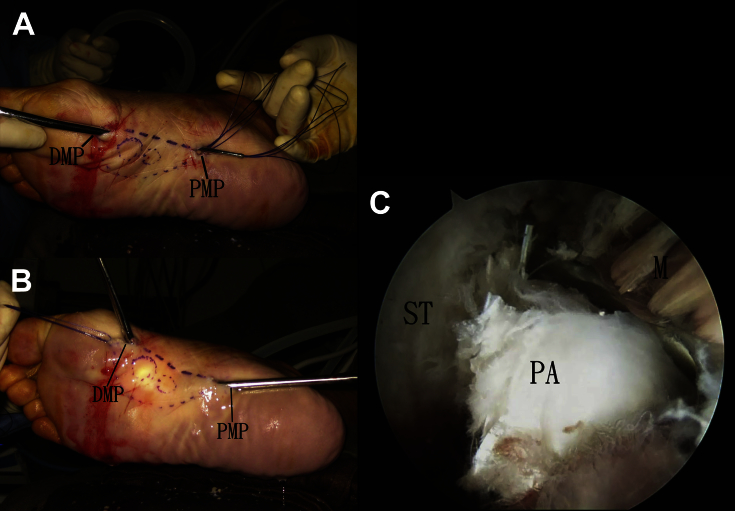
Fig 4.
Endoscopic subtotal fasciectomy of the right foot. The proximal medial portal is the viewing portal. (A) The light spot should go along the lateral outline of the AR. (B) The lateral edge of the AR is released by an arthroscopic shaver. (AR, planned area of resection of the plantar aponeurosis; DMP, distal medial portal; LE, lateral edge of planned resection area; M, muscles deep to the plantar aponeurosis; PA, plantar aponeurosis; PMP, proximal medial portal; ST, subcutaneous tissue.)
Endoscopic Release of the Medial Edge of the Planned Area of Resection of the Plantar Aponeurosis
The medial edge of the AR is the junction between the plantar aponeurosis and the deep fascia covering the abductor hallucis muscle. The proximal medial and distal medial portals are interchangeable as the viewing and working portals. The medial edge is released with an arthroscopic scissors and a retrograde knife (Smith & Nephew).
The proximal medial portal is the viewing portal. The middle part of the medial edge is cut open by an arthroscopic scissors via the distal medial portal. The distal part of the medial edge is cut by a retrograde knife via the distal medial portal. The arthroscope is then switched to the distal medial portal, and the proximal part of the medial edge is cut by the retrograde knife via the proximal medial portal (Fig 5). Release of the medial edge by an arthroscopic scissors via the proximal medial portal is not suitable. The heel will hinder proper placement of the scissors, and there will be tendency to cut into the plantar aponeurosis.
Fig 5.
Endoscopic subtotal fasciectomy of the right foot. (A) The distal medial portal (DMP) is the viewing portal. The medial edge (ME) of the plantar aponeurosis is released by a retrograde knife via the proximal medial portal (PMP). (B) The PMP is the viewing portal. The ME of the plantar aponeurosis is released by an arthroscopic scissors via the DMP. (DF, deep fascia over the hallucis abductus muscle; PA, plantar aponeurosis.)
Endoscopic Release of the Proximal Edge of the Planned Area of Resection of the Plantar Aponeurosis
The skin of the proximal medial portal is retracted to expose the plantar aponeurosis. A short length of the proximal edge of the AR is cut open by a SuperCut scissors (Stille, Lombard, IL) and the underlying muscle is freed from the aponeurosis. Two sets of stay stitches are applied to the aponeurosis just distal to the proximal edge of the AR with No. 1 PDS sutures (Ethicon, Somerville, NJ) by an eyed needle. The remaining part of the proximal edge is then cut by the SuperCut scissors (Fig 6).
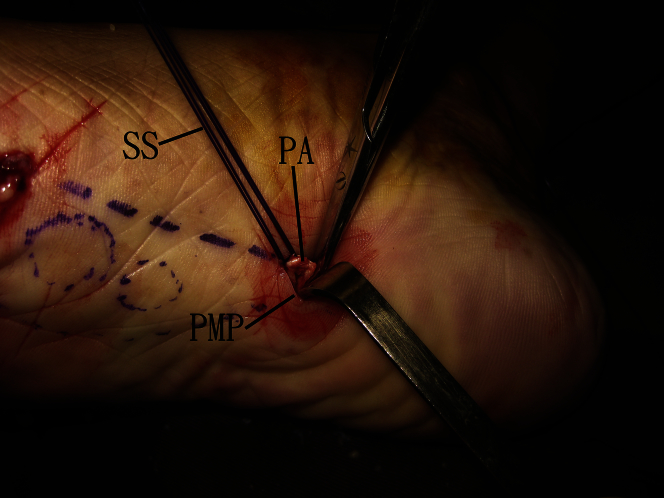
Fig 6.
Endoscopic subtotal fasciectomy of the right foot. Two sets of stay stitches (SS) are applied to the aponeurosis just distal to the proximal edge of the AR with No. 1 PDS sutures (Ethicon) by an eyed needle. The plantar aponeurosis (PA) is cut proximal to the stay stitches. (AR, planned area of resection of the plantar aponeurosis; PMP, proximal medial portal.)
Endoscopic Release of the Deep Surface of the Planned Area of Resection of the Plantar Aponeurosis
A small-sized suction tip is passed from the distal medial portal to the proximal medial portal. This serves as the conduit for the passage of the stay stitches to the distal medial portal. The plantar aponeurosis is then retracted toward the distal medial portal by pulling the stay stitches. The proximal medial portal is the viewing portal. The underlying muscle is stripped from the aponeurosis by a small periosteal elevator via the distal medial portal. Any residual fibrous band is cut by an arthroscopic scissors via the distal medial portal (Fig 7).
Fig 7.
Endoscopic subtotal fasciectomy of the right foot. (A) A small-sized suction tip is passed from the distal medial portal to the proximal medial portal (PMP). This serves as the conduit for the passage of the stay stitches to the distal medial portal (DMP). (B) The plantar aponeurosis is then retracted toward the DMP by pulling the stay stitches. (C) The PMP is the viewing portal. The underlying muscle is stripped from the aponeurosis by a small periosteal elevator via the DMP. (M, muscles deep to the plantar aponeurosis; PA, plantar aponeurosis; ST, subcutaneous tissue.)
Release of the Distal Edge of the Planned Area of Resection of the Plantar Aponeurosis
The aponeurosis together with the fibroma is retracted out of the distal medial portal. The digital nerve will remain inside the foot. The distal edge of the AR can be safely cut outside the distal medial portal (Video 1, Fig 8, Table 2).
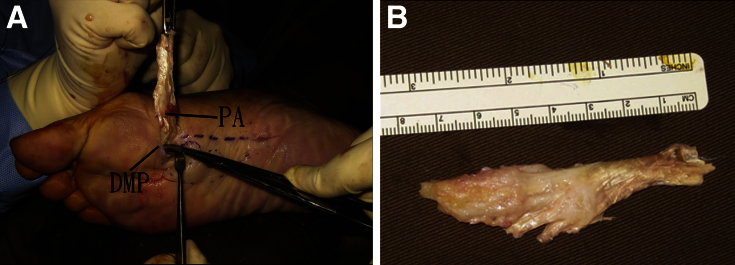
Fig 8.
Endoscopic subtotal fasciectomy of the right foot. (A) The plantar aponeurosis (PA) together with the fibroma is retracted out of the distal medial portal (DMP). The distal edge of the planned area of resection of the plantar aponeurosis (AR) is cut outside the DMP. (B) The resected PA.
Table 2.
Pearls and Pitfalls of Endoscopic Subtotal Fasciectomy of the Foot
| Pearls | Pitfalls |
|---|---|
| 1. The lesions and the planned area of resection are outlined on the plantar skin | 1. Do not extend the superficial release out of the boundary of the planned area of resection |
| 2. The distal part of the lateral edge of the planned area of resection should be parallel to the foot axis | 2. Do not dissect into the superficial tissue during superficial release |
| 3. Release of distal parts of the superficial and deep surfaces should be careful and under direct arthroscopic visualization to avoid damage of the emerging digital nerves when they cross the fascial extension to the toes | 3. Do not cut into the plantar aponeurosis during the release of the medial edge |
| 4. The plantar aponeurosis is brought out of the distal medial portal before resection | 4. Do not cut into the underlying muscles during the release of the lateral edge, proximal edge, and deep surface of the planned area of resection |
Discussion
The main concern of surgical treatment of plantar fibromatosis is the risk of local recurrence. Total fasciectomy has been proposed by some authors to be the primary operation of choice because it carries the lowest risk of recurrence.6, 8 However, total fasciectomy disrupts the tenuous blood supply coming from the deep aspect of the foot through the plantar fascia to the subcutaneous tissue and skin and the passive arch stability.2 Currently, the standard procedure consists of subtotal fasciectomy, as it represents a less invasive option with good results.1 Endoscopic subtotal fasciectomy may not reduce the risk of recurrence. However, the recurrence rate is expected to be comparable with that of the open surgery. Prospective studies are required for validation.
Other concerns of the surgical treatment include wound and neural complications. Skin necrosis and dehiscence, infection, retracted and painful scarring, and difficulties with shoe wearing can occur after open approaches.1 The plantar skin is nourished by the medial and lateral plantar arteries. There is clear demarcation between the skin supplied by the medial and lateral plantar arteries.2 Arterioles of the plantar arteries nourish the dermis from the midline of the foot toward its medial and lateral aspects.1 The ideal incision should be made between these 2 zones of vascularity on the nonweightbearing portion of the arch and limits devascularization of the plantar skin.2 Longitudinal or zigzag incisions medial to the midline of the foot can increase the risk of ischemia and necrosis of the skin on the medial side of the wound. Moreover, the longitudinal incision can produce hypertrophic and painful scars because they transverse the Langer's tension lines of the skin.1 In the reported endoscopic technique, the incisions are small and the chance of formation of painful hypertrophic scars is less than that of the open approach. The risk of ischemia and necrosis of the skin is also less because the dermal vascular network is less likely disturbed by the 2 small portal incisions.
Numbness or painful neuromas can occur when branches of the plantar nerves are injured during surgery.1 Branches of the plantar nerves become superficial between the digital projections of the plantar aponeurosis and innervate the toes. Dissection at these areas may injure the branches leading to permanent paresthesia or anesthesia and neuroma formation.1 There are several measures in the endoscopic technique to reduce the risk of neural injury:
-
1.
Dissection of the superficial and deep surfaces of the aponeurosis close to its fascial extensions to the toes should be performed under direct arthroscopic visualization.
-
2.
The distal part of the lateral edge of the AR should be longitudinal and parallel to the emerging digital nerves at the fascial extensions to the toes.
-
3.
Dissection into the muscles of the sole should be avoided during the release of the proximal and lateral edge and the deep surface of the AR.
-
4.
Dissecting the fascia from its deeper portion after releasing its proximal origin may help to identify, dissect, and protect the plantar nerves and their branches.1
In summary, the endoscopic technique has the advantages of smaller wounds, better cosmesis, less chance of painful hypertrophic scars, less risk of wound dehiscence, ischemia, or necrosis. The potential risks of this technique include vascular injury, nerve injury, local recurrence, and disruption of the foot arch stability (Table 3). This approach is technically demanding and should be reserved to the experienced foot and ankle arthroscopists.
Table 3.
Advantages and Risks of Endoscopic Subtotal Fasciectomy of the Foot
| Advantages | Risks |
|---|---|
| 1. Smaller wounds | 1. Vascular injury |
| 2. Better cosmesis | 2. Nerve injury |
| 3. Less chance of painful hypertrophic scars | 3. Local recurrence |
| 4. Less risk of wound dehiscence, ischemia, or necrosis | 4. Disruption of the foot arch stability |
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Endoscopic subtotal fasciectomy of the right foot. The proximal medial portal is the viewing portal. The superficial surface and the lateral edge of the planned resected area of the plantar aponeurosis are released via the distal medial portal. The medial edge of the planned resected area is released with the proximal medial and distal medial portals interchanged as the viewing and distal portals. Stay stitches are applied to the proximal end of the planned resected area of the aponeurosis, and the aponeurosis is cut proximal to the stitches. The stitches are passed to the distal medial portal. The aponeurosis is then retracted to the distal medial portal. The underlying muscle is stripped from the deep surface of the aponeurosis and any fibrous band is cut. The aponeurosis is retracted out of the distal medial portal and resected.
References
- 1.Souza B.G., de Souza Júnior G.Z., Rodrigues R.M., Dias D.S., de Oliveira V.M. Surgical treatment of a case of Ledderhose's disease: A safe plantar approach to subtotal fasciectomy. Case Rep Orthop. 2015;2015:509732. doi: 10.1155/2015/509732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sammarco G.J., Mangone P.G. Classification and treatment of plantar fibromatosis. Foot Ankle Int. 2000;21:563–569. doi: 10.1177/107110070002100706. [DOI] [PubMed] [Google Scholar]
- 3.Omor Y., Dhaene B., Grijseels S., Alard S. Ledderhose disease: Clinical, radiological (ultrasound and MRI), and anatomopathological findings. Case Rep Orthop. 2015;2015:741461. doi: 10.1155/2015/741461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adib O., Noizet E., Croue A., Aubé C. Ledderhose's disease: Radiologic/pathologic correlation of superficial plantar fibromatosis. Diagn Interv Imaging. 2014;95:893–896. doi: 10.1016/j.diii.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 5.Yasui Y., Takao M., Miyamoto W., Matsushita T. Plantar fibromatosis with flexion contracture and valgus deformity of the great toe. J Orthop Sci. 2016;21:395–398. doi: 10.1016/j.jos.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 6.van der Veer W.M., Hamburg S.M., de Gast A., Niessen F.B. Recurrence of plantar fibromatosis after plantar fasciectomy: Single-center long-term results. Plast Reconstr Surg. 2008;122:486–491. doi: 10.1097/PRS.0b013e31817d61ab. [DOI] [PubMed] [Google Scholar]
- 7.Veith N.T., Tschernig T., Histing T., Madry H. Plantar fibromatosis—Topical review. Foot Ankle Int. 2013;34:1742–1746. doi: 10.1177/1071100713505535. [DOI] [PubMed] [Google Scholar]
- 8.Beckmann J., Kalteis T., Baer W., Grifka J., Lerch K. Plantar fibromatosis: Therapy by total plantarfasciectomy. Zentralblatt fur Chirurgie. 2004;129:53–57. doi: 10.1055/s-2004-816231. [DOI] [PubMed] [Google Scholar]
- 9.de Bree E., Zoetmulder F.A., Keus R.B., Peterse H.L., van Coevorden F. Incidence and treatment of recurrent plantar fibromatosis by surgery and postoperative radiotherapy. Am J Surg. 2004;187:33–38. doi: 10.1016/j.amjsurg.2002.11.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic subtotal fasciectomy of the right foot. The proximal medial portal is the viewing portal. The superficial surface and the lateral edge of the planned resected area of the plantar aponeurosis are released via the distal medial portal. The medial edge of the planned resected area is released with the proximal medial and distal medial portals interchanged as the viewing and distal portals. Stay stitches are applied to the proximal end of the planned resected area of the aponeurosis, and the aponeurosis is cut proximal to the stitches. The stitches are passed to the distal medial portal. The aponeurosis is then retracted to the distal medial portal. The underlying muscle is stripped from the deep surface of the aponeurosis and any fibrous band is cut. The aponeurosis is retracted out of the distal medial portal and resected.