Abstract
Lateral compartment disease combined with valgus alignment can lead to progressive knee joint degeneration. In the symptomatic patient with isolated lateral compartment disease, a varus-producing distal femoral osteotomy can unload the diseased lateral compartment. This osteotomy may be combined with other cartilage or meniscal restorative techniques to optimize knee joint preservation and pain relief. The osteotomy can be performed with a medial closing-wedge or lateral opening-wedge technique. Both techniques have been reported to improve knee-related quality of life in patients with lateral compartment disease. Advantages of the medial closing-wedge technique are direct bone apposition leading to inherent stability of the construct, as well as reliable bony healing, and less hardware irritation. Advantages of the lateral opening-wedge technique are a single bony cut and therefore more of an ability to adjust correction intraoperatively. However, this technique requires bone grafting and has a high rate of hardware irritation or removal. We present a surgical technique for the medial closing-wedge distal femoral osteotomy using an anteromedial-distal femoral locking plate.
Abnormal mechanical alignment of the lower extremity is a risk factor for progressive joint degeneration.1 Traditionally, valgus alignment with lateral compartment knee osteoarthritis was treated with a varus-producing distal femoral osteotomy (DFO), whereas varus alignment with medial compartment osteoarthritis was treated with a valgus-producing high tibial osteotomy (HTO). With improvements in arthroplasty techniques and implants, realigning osteotomies have become less common over time.2, 3
Recently, there has been an increasing interest in biological joint restoration in young patients because of improvements in cartilage repair techniques.4 Successful cartilage repair relies on appropriate mechanical alignment of the limb to prevent excessive mechanical stress on the cartilage or osteochondral grafts.4 Genu valgum is most commonly caused by a hypoplastic lateral femoral condyle; therefore, osteotomy on the femoral side best avoids an oblique joint line after correction of alignment. Both medial closing-wedge and lateral opening-wedge osteotomies of the distal femur have been reported for correction of genu valgum.5 Patient-reported knee quality of life is improved by either technique.6, 7, 8, 9 Advantages of each technique are detailed in Table 1.
Table 1.
Advantages of Medial and Lateral Distal Femoral Osteotomies
| Advantages of medial closing wedge |
| Direct bony contact leads to inherent stability and reliable bony healing compared to the need for bone grafting of an opening-wedge technique. |
| There is less hardware irritation because of the plate not being directly under the iliotibial band. |
| Advantages of lateral opening wedge |
| Opening-wedge osteotomy leads to an ability to correct and adjust the amount of distraction to optimize the mechanical axis. |
| It is a familiar approach to the lateral-distal femur. |
| There is access to the lateral compartment for concomitant procedures. |
Young patients with valgus alignment and lateral compartment disease including isolated lateral compartment arthritis, lateral meniscal deficiency, and/or focal chondral or osteochondral lateral compartment defects are excellent candidates for a DFO. Our preference is a medial closing-wedge technique because of the inherent stability of the construct, ease of surgical technique, and reliable bony healing. Concomitant joint-restoring procedures including meniscal transplantation or cartilage restoration can be performed at the time of osteotomy or in a staged manner. This article provides a detailed, step-wise method that enables the reproducible creation of a medial closing-wedge DFO for the valgus knee using locking-plate fixation.
Surgical Technique
Preoperative Planning
In patients presenting with lateral-based knee pain, a detailed history is obtained and physical examination performed. Imaging starts with 4-view knee radiographs in addition to standing full-length alignment radiographs (Fig 1). Magnetic resonance imaging is commonly used to evaluate meniscal and cartilage injuries (Fig 2). If patients are identified to have isolated symptomatic lateral compartment disease with valgus alignment on full-length radiographs, then they are candidates for the procedure. Indications and contraindications are outlined in Table 2. Full-length radiographs are used to calculate the angle between the mechanical axis of the femur and that of the tibia (Fig 3). This represents the angle of correction to achieve neutral mechanical alignment of the patient. The medial-proximal tibial angle and lateral-distal femoral angle should also be calculated to identify the origin of the osseous deformity (Fig 4). Commonly, genu valgum occurs because of femoral malalignment and should be corrected with a DFO, whereas genu varum occurs because of tibial malalignment and should be corrected with an HTO. However, this generality is not always the case—particularly in the setting of post-traumatic malalignment. Therefore, these angular measurements should always be performed during preoperative templating to ensure that an oblique joint line is not iatrogenically created. In rare circumstances, both a DFO and an HTO may be necessary to ensure a balanced osteotomy to maintain a joint line that is parallel and horizontal. In addition, the joint congruence angle may be calculated in the setting of joint space narrowing to ensure that overcorrection does not occur, given that joint space narrowing frequently is partially corrected after correction of osseous malalignment.
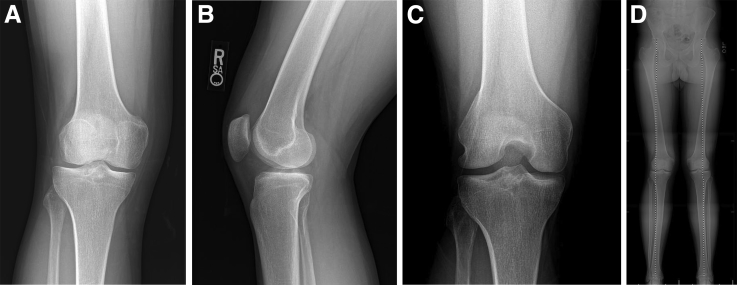
Fig 1.
A 33-year-old male patient with chronic right lateral compartment knee pain with ambulation and impact activities. Anteroposterior (A), 45° posteroanterior flexion (B), and lateral (C) plain weight-bearing radiographic views show preservation of the joint space. (D) A full-length standing alignment view shows genu valgum with the weight-bearing axis in the center of the right knee lateral compartment. (R, right; SA, standing.)
Fig 2.
T2 magnetic resonance images in the coronal (A), sagittal (B), and axial (C) planes show a 15-mm × 22-mm osteochondral lateral tibial defect. (S, superior.)
Table 2.
Indications and Contraindications of Medial Closing-Wedge Distal Femoral Osteotomy
| Indications |
| Valgus alignment |
| Meniscal deficiency of lateral compartment |
| Chondral or osteochondral lesions of lateral compartment |
| Isolated lateral compartment osteoarthritis |
| Contraindications |
| Inflammatory arthritis |
| Medial and/or patellofemoral osteoarthritis |
| Flexion contracture >15° |
| Deformity >15° |
| <90° of knee flexion |
| Relative contraindications |
| Tobacco use |
| The medial closing-wedge osteotomy creates direct osseous apposition that promotes healing even in the setting of nicotine use, as compared with that which may occur with an opening-wedge technique. Nevertheless, we prefer to have patients fully cease nicotine use before surgery. |
| Obesity with body mass index >30 |
| Age >50 yr |
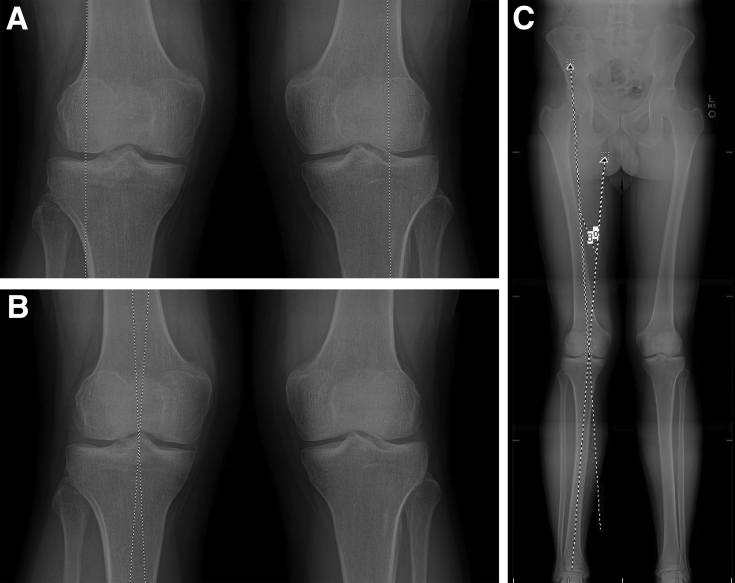
Fig 3.
Osteotomy correction is planned using preoperative weight-bearing full-length standing radiographs. (A) The preoperative weight-bearing axis shows genu valgum through the middle of the lateral compartment. (B) Our preferred method of preoperative planning is the mechanical axis method. Correction should be performed to a neutral axis by 2 separate lines. The first line runs from the center of the superior dome of the femoral head through the center of the intercondylar notch. The second line is drawn from the tibial interspinous point to the center of the ankle joint. (C) The angle formed by the intersection of these 2 lines is equal to the osteotomy correction angle. (L, left; MS, marking system.)
Fig 4.
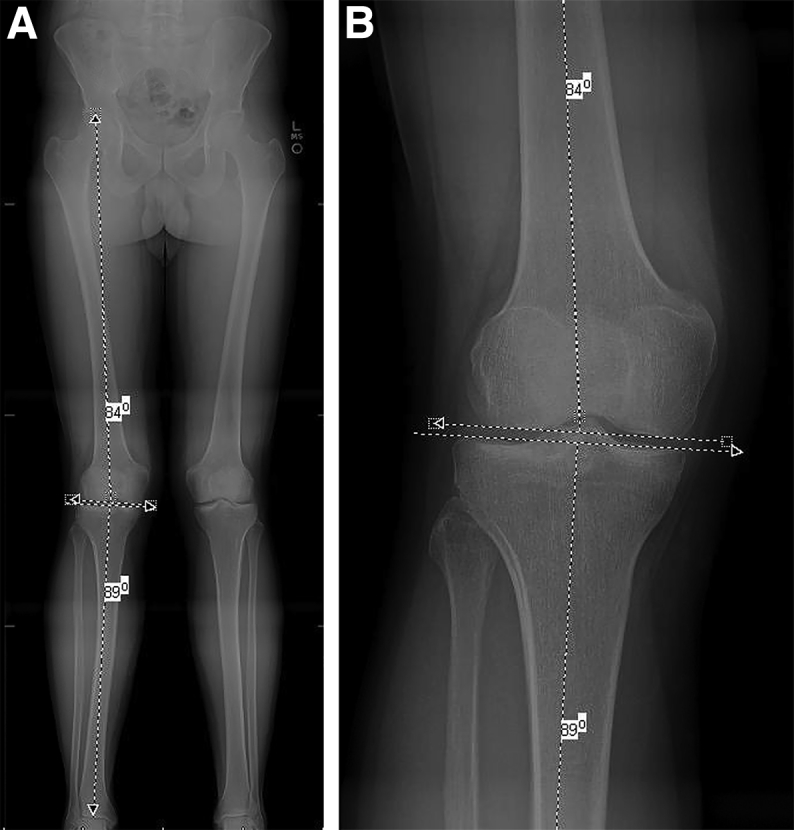
(A) The mechanical medial-proximal tibial angle and the mechanical lateral-distal femoral angle should be evaluated to identify the origin of the deformity. (B) Osteotomy correction of an angular deformity should be performed at the origin of the deformity. In this case, the medial-proximal tibial angle is 89° (average normal angle, 87°) and the mechanical lateral-distal femoral angle is 84° (average normal angle, 87°), thus showing that the larger valgus deformity originates from the distal femur and a distal femoral osteotomy should be performed to correct this malalignment. In the setting of significant arthrosis and joint space narrowing, the joint line congruence angle may also be calculated to ensure that overcorrection does not occur because deformity through the joint will frequently be corrected with alignment axis correction. (L, left; MS, marking system.)
Patient Positioning, Diagnostic Arthroscopy, and Concomitant Procedures
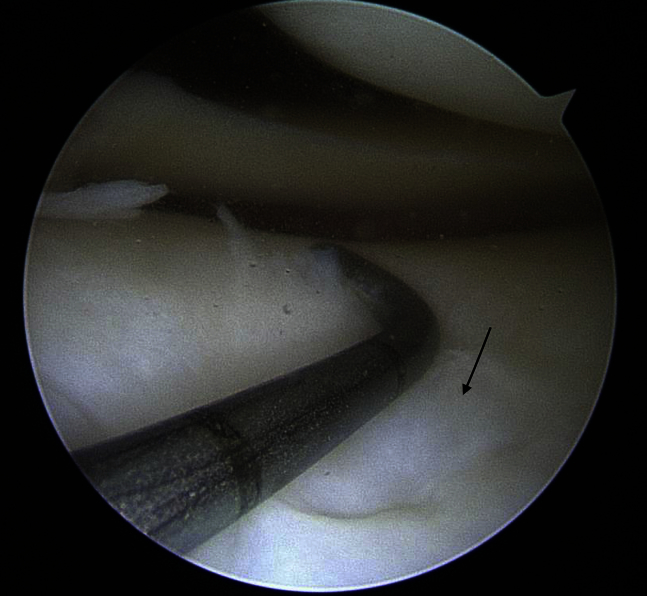
The patient is placed supine on a radiolucent table to allow radiographic evaluation from the hip to the ankle. Fluoroscopy comes in from the operative side of the table. The patient undergoes preparation and draping with the lower leg placed in a stockinet and wrapped in adherent wrap to a position just distal to the tibial tubercle. A diagnostic arthroscopy can be performed to confirm that there is isolated lateral compartment disease (Fig 5). Concomitant procedures can be performed at this time to address lateral compartment chondral or meniscal disease or deficiency.
Fig 5.
Intraoperative arthroscopic evaluation before distal femoral osteotomy. The patient is in the supine position with a lateral post on the right leg. Viewing from the anterolateral portal with the leg in the figure-of-4 position confirms osteochondral damage isolated to the lateral compartment (arrow).
Approach and Exposure
After completion of the concomitant procedures, attention is turned to the DFO. An incision is made on the distal anteromedial aspect of the femur from 8 cm proximal to the patella to the middle third of the patella (Video 1). An incision should be made to facilitate use in future arthroplasty if needed. Dissection is taken down through the generally avascular plane in the vastus medialis oblique fascia and the intermuscular septum (Video 1). If small perforating vessels are encountered, these are coagulated with the electrocautery. The proximal third of the medial patellofemoral ligament, as well as the distal insertion of the vastus medialis oblique, can be incised to allow mobilization of the quadriceps and adequate exposure of the distal femur for plate positioning. The intermuscular septum adjacent to the medial femoral cortex is then incised in line with the femur using electrocautery. A blunt rasp or Cobb elevator can be used to carefully dissect soft tissues off of the posterior femur with care taken to work directly on the posterior femoral cortex (Video 1). Wide blunt-tipped radiolucent Hohmann retractors (Synthes, West Chester, PA) can then be placed along the anterior and posterior cortices of the femur at the level of the osteotomy to protect the neurovascular structures. Dissection should be distal enough to have good exposure of the anteromedial condyle of the femur proximally to safely place the locking plate under direct visualization.
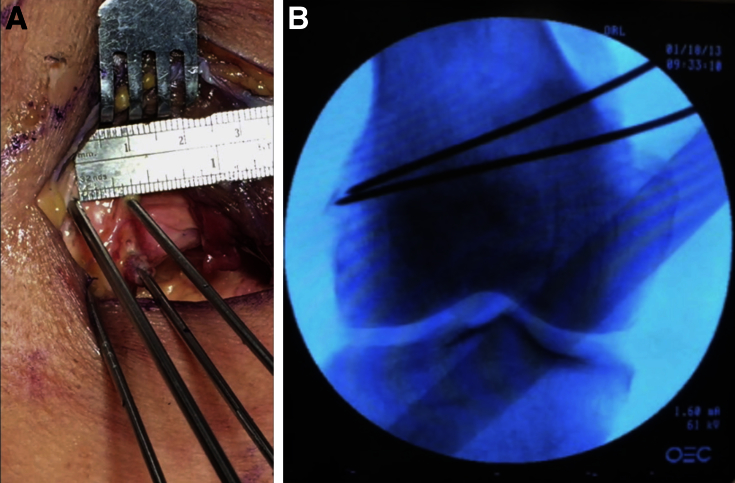
Osteotomy
Kirschner wires (K-wires) are used to mark the osteotomy cut both proximally and distally to allow for an appropriate wedge to be resected. The initial 2 wires are placed anteriorly and posteriorly to establish the inferior wedge of the osteotomy. These wires should be confirmed to be parallel to each other so that no flexion or extension is created with the osteotomy (Video 1, Fig 6). In addition, the wires should begin at the meta-diaphyseal position on the medial femur and end in the proximal metaphysis of the distal lateral femur. This position allows closure of the wedge with anatomic medial cortical approximation and uses the inherently reduced rigidity of the lateral metaphyseal cortex to improve wedge closure without fracture. Care should also be taken to obtain a perfect anteroposterior fluoroscopic view of the distal femur to ensure that angular malalignment is not created. The lengths of the wires should be measured and used for direct intraoperative correlation to calculate the desired wedge size width (Table 3).10 Once the desired wedge size is confirmed, a second pair of wires is placed in a convergent fashion, thus establishing the proximal margin of the wedge. The calculated wedge size should be equal to the distance between the 2 sets of wires. These wires also serve as a boundary to guide the saw blade and ensure that over-resection does not occur.
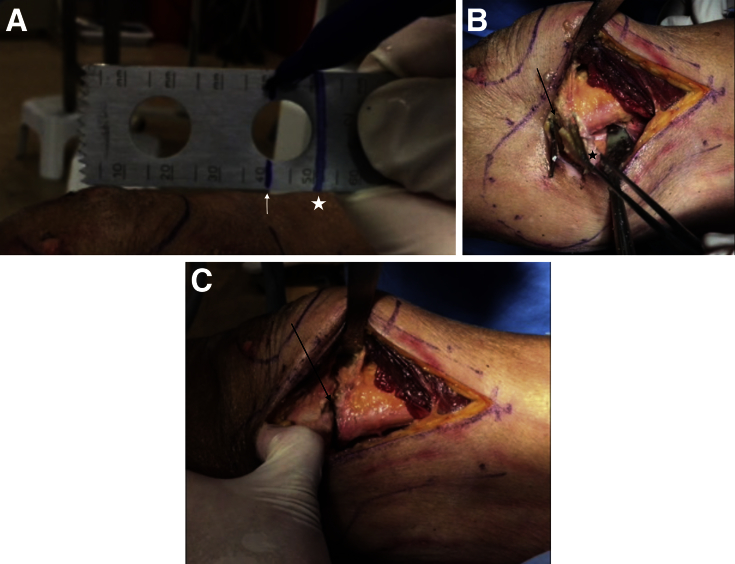
Fig 6.
(A) The patient is in the supine position, with the surgeon viewing the right leg from the left side of the patient. Distal is to the left and proximal is to the right of the image. An intraoperative photograph shows the medial cortex of the femur with K-wires placed to guide the osteotomy cuts. Care is taken to ensure that the K-wires are perpendicular to the long axis of the femur and parallel to each other. A ruler is used to confirm the osteotomy size based on preoperative calculations. (B) Posteroanterior fluoroscopic image of wires placed to guide the osteotomy, with medial on the right side and lateral on the left side of the image.
Table 3.
Trigonometric Calculation of Osteotomy Size Based on Templated Correction Angle and Mediolateral Diameter of Osteotomy
| Mediolateral Diameter of Osteotomy | Preoperatively Measured Correction Angle |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4° | 5° | 6° | 7° | 8° | 9° | 10° | 11° | 12° | 13° | 14° | 15° | 16° | 17° | 18° | 19° | |
| 50 mm | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 16 |
| 55 mm | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| 60 mm | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
| 65 mm | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
| 70 mm | 5 | 6 | 7 | 8 | 10 | 11 | 12 | 13 | 15 | 16 | 17 | 18 | 20 | 21 | 22 | 23 |
| 75 mm | 5 | 6 | 8 | 9 | 10 | 12 | 13 | 14 | 16 | 17 | 18 | 20 | 21 | 22 | 24 | 25 |
| 80 mm | 6 | 7 | 8 | 10 | 11 | 13 | 14 | 15 | 17 | 18 | 19 | 21 | 22 | 24 | 25 | 26 |
NOTE. Data represent the wedge size in millimeters. The wedge size can also be planned before surgery and confirmed intraoperatively. The mediolateral diameter of the osteotomy site is measured intraoperatively by measuring the length of the 2 initial guidewires that are placed from medial to lateral. The intraosseous lengths of the anterior and posterior guidewires are then averaged to provide the diameter reference for the chart.10 This wedge size should be used to guide placement of the second set of 2 guidewires that determine the wedge resection size.
With retractors placed along both the anterior and posterior cortices to protect the quadriceps tendon and posterior neurovascular structures, respectively, the sagittal saw is marked to the depth of the cut to avoid violation of the lateral cortex. This depth should be approximately 5 to 10 mm shorter than the previously measured lengths of the wires to ensure that the lateral cortex is not violated. The marks on the saw are used to judge the depth of the cut (Video 1, Fig 7A). The saw is used to create both medial-to-lateral cuts under fluoroscopic guidance, and the wedge of bone should then be easily removed from the medial cortex, with confirmation of a complete osteotomy of the anterior and posterior cortices (Fig 7B). Difficulty with wedge removal typically occurs when the anterior or posterior margins of the wedge have not been fully completed.
Fig 7.
(A) Lengths of proximal K-wire (shorter mark [arrow]) and distal K-wire (longer mark [star]) drawn on the saw blade to avoid plunging the saw and fracturing or cutting the lateral cortex. (B) Intraoperative photograph with the patient in the supine position (distal is to the left and proximal is to the right) after removal of the osteotomy wedge (star), leaving the open osteotomy site between the K-wires (arrow). (C) Intraoperative photograph in the same position after gently closing the osteotomy site (arrow).
At this time, a marking pen or surgical electrocautery device may be used to mark corresponding positions on the proximal and distal osteotomy edges parallel to the femoral shaft. These marks can be approximated to avoid iatrogenic malrotation if the lateral cortex is inadvertently fractured during osteotomy closure. The osteotomy is then gently relaxed into a closed position in a controlled manner to avoid lateral cortical fracture (Fig 7C). The wedge should close with minimal resistance. If resistance is encountered with wedge closure, a blunt radiopaque instrument such as a freer elevator or the curved edge of a metal ruler may be used to palpate the anterior and posterior edges of the osteotomy to ensure that the osteotomy has been fully completed. After this confirmation, if continued resistance is encountered, K-wires or a small drill may be used to gently perforate and slightly weaken the lateral cortex to assist the wedge closure under fluoroscopic guidance. The alignment rod is then used to confirm the desired alignment between the center of the femoral head, the desired position at the knee joint, and the center of the ankle joint (Video 1, Fig 8).
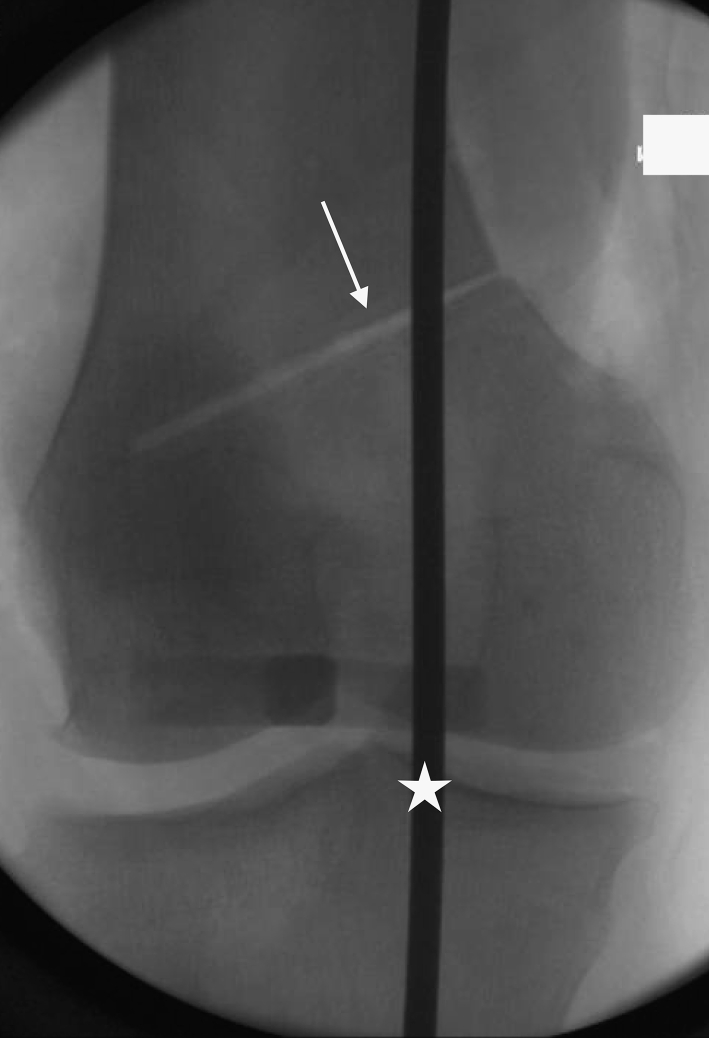
Fig 8.
Posteroanterior fluoroscopic image of the knee with the alignment rod centered over the femoral head proximally and the middle of the ankle joint distally, showing correction of the mechanical axis to slight varus after closing the osteotomy (arrow) with the alignment rod going through just medial to the center of the knee (star).
Plate Fixation
After the osteotomy is closed and the desired correction is obtained, the anteromedial-distal femoral locking plate (Synthes) is placed on the anteromedial femur in the appropriate position. There are 2 small spacers placed on the proximal and distal aspects of the plate. These spacers are designed to maintain periosteal vascular flow after plate fixation and improve the biological aspects of the construct. A 2.0-mm threaded K-wire is placed in the anterior distal screw hole to provisionally fix the plate in place (Video 1). The proximal aspect of the plate should be positioned parallel to the middle of the femoral shaft. Calibrated locking guides are screwed into the distal plate, and the posterior distal screw is drilled and placed in locking fashion unicortically. The other 3 distal screws are then placed in unicortical locking fashion to the metaphyseal segment (Video 1). A bicortical nonlocking screw is used to bring the plate down to the diaphyseal femur and compress the osteotomy site (Video 1). The other proximal screws are then placed unicortically in locking fashion, and the spacers are removed. The nonlocking screw is removed and replaced with a bicortical locking screw (Video 1). Proper positioning of hardware is confirmed (Fig 9).
Fig 9.
Anteroposterior radiograph showing proper placement of the locking plate. The arrow shows the healed osteotomy site.
Closure, Dressing, and Postoperative Protocol
The wound is copiously irrigated with normal saline solution, and meticulous hemostasis is obtained. Closure is then completed in layers with the medial patellofemoral ligament repaired if partially transected. The patient is placed in a hinged knee brace with a soft dressing and cooling device. Continuous passive motion is used starting on postoperative day 1. The complete rehabilitation protocol is outlined in Table 4. Pearls and pitfalls of the described technique are outlined in Table 5. Full-length radiographs are obtained at 6 weeks postoperatively to confirm correction of mechanical alignment (Fig 10).
Table 4.
Rehabilitation Protocol for Medial Closing-Wedge Distal Femoral Osteotomy
| Weight bearing |
| The patient is allowed only touch-down weight bearing for 4 wk. |
| The patient progresses to weight bearing as tolerated from week 4 to week 6. |
| Range of motion |
| CPM of 0°-30° is started and is advanced to 0°-90° as tolerated for the first 6 wk. The goal is to perform CPM for 3-4 h per day as able. |
| The patient progresses to full range of motion from 6-12 wk. |
| The patient should have full range of motion by 12 wk. |
| Brace wear |
| The patient wears a hinged knee brace locked in extension for the first 2 wk except when performing range-of-motion exercises. |
| An unlocked hinged knee brace is worn during the day after 2 wk. The patient keeps the brace locked in extension at night for the first 6 wk. |
| Bracing is discontinued at 6 wk. |
| Exercises |
| The patient may do heel slides, quadriceps sets, straight-leg raises, and hamstring and calf stretching for the first 6 wk. |
| Spinning on a stationary bicycle with no resistance is added at 6 wk. |
| Mini-squats, stationary bicycling with resistance, and swimming are added at 8 wk. |
| A treadmill and walking or running program are added at 12 wk. |
| The patient should progress to activities as tolerated over a period of 3-6 mo postoperatively. |
CPM, continuous passive motion.
Table 5.
Pearls and Pitfalls of Medial Closing-Wedge Distal Femoral Osteotomy
| Pearls |
| Radiolucent retractors allow fluoroscopic visualization while the osteotomy is performed. |
| The surgeon should mark the saw 5-10 mm shorter than the length of the wire to avoid plunging and violating the lateral cortex. Two separate marks may be used to correspond to the lengths of the anterior and posterior wires, respectively. |
| Gentle and/or slow closing of the osteotomy gap should be performed to avoid fracture of the lateral cortex. Confirmation of completion of both the anterior and posterior components of the osteotomy can be performed with a blunt radiopaque instrument such as a freer or metallic ruler. In addition, careful perforation of the lateral cortex with K-wires or a small drill may aid in slightly weakening the lateral cortex and avoiding fracture. |
| The proximal aspect of the plate should be aligned parallel to the longitudinal axis of the femur before distal screw placement. |
| The intermuscular septum should only be divided directly adjacent to the femoral cortex to avoid the genicular arteries and veins. When encountered, these should be carefully ligated to avoid postoperative complications. |
| If there is condylar deformity, plate placement should be adjusted to avoid screw penetration of the posterior cortex. Distal angular locking screws should always be placed in a unicortical fashion to avoid posterior neurovascular injury. |
| Pitfalls |
| Fracture of the lateral cortex at the osteotomy site destabilizes the osteotomy. If this occurs, the surgeon should ensure that the medial femoral marks that were placed before osteotomy closure are carefully approximated to avoid iatrogenic malrotation. Lateral cortical fracture does not require additional fixation because the medial locking plate used in this technique provides adequate stability even without an intact hinge. If the lateral cortex is fractured and displacement of the osteotomy occurs, the plate can be used as a reduction aid. In this setting, the distal metaphyseal screws can be placed and the bicortical proximal screw can then be used to reduce the femoral shaft to the plate, thereby reducing the displacement and compressing the osteotomy. If this is unsuccessful or a large displacement occurs, a large reduction clamp can be used through a small lateral skin incision centered over the lateral femoral condyle to reduce the osteotomy before proximal shaft screw placement. |
| Dissecting into the soft tissues posteriorly can cause potential neurovascular injury. The venous plexus at the distal aspect of the medial femur should be carefully coagulated during exposure. In addition, this procedure can be easily performed without use of a tourniquet, thereby allowing immediate identification and repair of vascular injury if this occurs. |
| Over-resection, under-resection, or failure in preoperative planning can occur, leading to inappropriate mechanical axis correction. |
| Penetration of the posterior cortex by the distal locking screws can occur. This should be avoided because all distal locking screws should be placed in a unicortical fashion. |
| Patella instability can occur as a result of transection without repair of the MPFL and distal VMO attachment. |
| Delayed bone healing is possible, requiring prolonged restricted weight bearing and possible revision with bone grafting. |
MPFL, medial patellofemoral ligament; VMO, vastus medialis oblique.
Fig 10.

The postoperative full-length standing radiograph shows a neutral weight-bearing axis.
Discussion
A varus-producing DFO can be an excellent option to improve pain and function in patients with isolated lateral compartment disease and valgus alignment. The DFO can be performed concomitantly with other joint-preserving procedures including cartilage restoration procedures and/or meniscal transplantation. Given the quality of knee arthroplasty techniques and implants, DFO has become most commonly used for joint preservation in the young patient with the goal to preserve the native knee joint and postpone or avoid total knee arthroplasty.
There are 2 main approaches for a varus-producing DFO: lateral opening wedge and medial closing wedge. The medial closing wedge is the traditional approach. Historically, fixation for the medial closing-wedge DFO occurred with the use of staples; fixation has since evolved to plate and screw fixation constructs, including blade plates and contoured one-third tubular plates.11, 12, 13 Recently, a technique using a proximal tibial locking plate was described.14 In this article we have presented a simple, reproducible surgical technique using a pre-contoured medial-distal femoral locking plate designed for a medial closing-wedge DFO. If desired, the lateral opening-wedge osteotomy can also be completed with a blade plate, distal condylar screw, or lateral-distal femoral plate and screw construct.
We prefer the described medial closing-wedge technique because of reliable bony healing, inherent construct stability, minimal hardware complications, and technique safety and ease. Classic teaching included the possibility of altering leg length with the lateral opening-wedge technique. However, Madelaine et al.15 recently reported on their series and noted no alteration of leg length in 29 patients. Jacobi et al.16 reported on their series of lateral opening-wedge osteotomies and noted significant delayed healing and plate irritation requiring removal. They have abandoned the lateral opening-wedge technique for a medial closing-wedge technique.16
Overall, there is a high reoperation rate in patients with DFOs, commonly because of the need for hardware removal or, at later time points, conversion to total knee arthroplasty. Patients should to be counseled that there is a 25% to 40% rate of reoperation.5, 17 Reported outcomes show a higher conversion rate to arthroplasty in patients with medial closing-wedge osteotomies, but this is confounded by the fact that many of these historical patients were indicated to undergo surgical treatment of lateral compartment arthritis to avoid arthroplasty.5 Moreover, given the historical nature of these studies, these patients had longer reported follow-up, as compared with other studies documenting outcomes and complications after lateral opening-wedge DFOs.5 These data may not apply well to contemporary indications for the DFO used for joint preservation with concomitant cartilage- or meniscus-restoring procedures in young active patients. In this population, the rate of conversion to arthroplasty will likely be significantly reduced. Cameron et al.7 reported a 92% survival rate at midterm in their series of patients undergoing lateral opening-wedge osteotomy for joint preservation, which was significantly better than results documented in patients undergoing osteotomy for lateral compartment arthritis.
DFO can reliably correct valgus mechanical alignment of the lower extremity, decrease pain, and increase function in patients with lateral compartment disease. The osteotomy can be performed in a medial closing-wedge or lateral opening-wedge manner. The technique presented in this article provides a safe, reproducible method to perform the medial closing-wedge DFO. Moreover, the pearls and pitfalls that are discussed will allow the treating surgeon to first avoid and, when necessary, address many of the intraoperative complications that may occur during this surgical procedure. Excellent postoperative outcomes including reliable healing, improved function, and decreased pain can be expected when this procedure is correctly indicated and performed.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: T.G.M. receives support from Arthrex.
Supplementary Data
Distal femoral medial closing-wedge osteotomy on the right distal femur of a cadaveric specimen. The patient is positioned in the supine position, with viewing from the left side of the patient. Distal is to the left of the view and proximal is to the right. Dissection is taken down through the interval between the vastus medialis oblique and the intermuscular septum, exposing the medial cortex of the femur. The osteotomy site is marked with K-wires based on preoperative templating. Proximal and distal osteotomy cuts are made with care taken not to cut or fracture the lateral cortex, and the osteotomy is gently closed. An anteromedial-distal medial femur locking plate (Synthes) is placed and confirmed to be in the correct position using intraoperative fluoroscopy. The wound is then closed in layers.
References
- 1.Sharma L., Song J., Felson D.T., Cahue S., Shamiyeh E., Dunlop D.D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 2.Niinimäki T.T., Eskelinen A., Ohtonen P., Junnila M., Leppilahti J. Incidence of osteotomies around the knee for the treatment of knee osteoarthritis: A 22-year population-based study. Int Orthop. 2012;36:1399–1402. doi: 10.1007/s00264-012-1508-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nwachukwu B.U., McCormick F.M., Schairer W.W., Frank R.M., Provencher M.T., Roche M.W. Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplasty. 2014;29:1586–1589. doi: 10.1016/j.arth.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Moran C.J., Pascual-Garrido C., Chubinskaya S. Restoration of articular cartilage. J Bone Joint Surg Am. 2014;96:336–344. doi: 10.2106/JBJS.L.01329. [DOI] [PubMed] [Google Scholar]
- 5.Wylie J.D., Jones D.L., Hartley M.K. Distal femoral osteotomy for the valgus knee: Medial closing wedge versus lateral opening wedge: A systematic review. Arthroscopy. 2016;32:2141–2147. doi: 10.1016/j.arthro.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Wang J.-W., Hsu C.-C. Distal femoral varus osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am. 2005;87:127–133. doi: 10.2106/JBJS.C.01559. [DOI] [PubMed] [Google Scholar]
- 7.Cameron J.I., McCauley J.C., Kermanshahi A.Y., Bugbee W.D. Lateral opening-wedge distal femoral osteotomy: Pain relief, functional improvement, and survivorship at 5 years. Clin Orthop Relat Res. 2015;473:2009–2015. doi: 10.1007/s11999-014-4106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dewilde T.R., Dauw J., Vandenneucker H., Bellemans J. Opening wedge distal femoral varus osteotomy using the Puddu plate and calcium phosphate bone cement. Knee Surg Sports Traumatol Arthrosc. 2012;21:249–254. doi: 10.1007/s00167-012-2156-6. [DOI] [PubMed] [Google Scholar]
- 9.Backstein D., Morag G., Hanna S., Safir O., Gross A. Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty. 2007;22:2–6. doi: 10.1016/j.arth.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 10.Hernigou P. Open wedge tibial osteotomy: Combined coronal and sagittal correction. Knee. 2002;9:15–20. doi: 10.1016/s0968-0160(01)00111-9. [DOI] [PubMed] [Google Scholar]
- 11.Wang J.-W., Hsu C.-C. Distal femoral varus osteotomy for osteoarthritis of the knee. Surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1, pt 1):100–108. doi: 10.2106/JBJS.E.00827. [DOI] [PubMed] [Google Scholar]
- 12.Kosashvili Y., Safir O., Gross A., Morag G., Lakstein D., Backstein D. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: A minimum ten-year follow-up. Int Orthop. 2009;34:249–254. doi: 10.1007/s00264-009-0807-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edgerton B.C., Mariani E.M., Morrey B.F. Distal femoral varus osteotomy for painful genu valgum. A five-to-11-year follow-up study. Clin Orthop Relat Res. 1993;(288):263–269. [PubMed] [Google Scholar]
- 14.Tírico L.E.P., Demange M.K., Bonadio M.B., Helito C.P., Gobbi R.G., Pecora J.R. Medial closing-wedge distal femoral osteotomy: Fixation with proximal tibial locking plate. Arthrosc Tech. 2015;4:e687–e695. doi: 10.1016/j.eats.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madelaine A., Lording T., Villa V., Lustig S., Servien E., Neyret P. The effect of lateral opening wedge distal femoral osteotomy on leg length. Knee Surg Sports Traumatol Arthrosc. 2016;24:847–854. doi: 10.1007/s00167-014-3387-5. [DOI] [PubMed] [Google Scholar]
- 16.Jacobi M., Wahl P., Bouaicha S., Jakob R.P., Gautier E. Distal femoral varus osteotomy: Problems associated with the lateral open-wedge technique. Arch Orthop Trauma Surg. 2010;131:725–728. doi: 10.1007/s00402-010-1193-1. [DOI] [PubMed] [Google Scholar]
- 17.Chahla J., Mitchell J.J., Liechti D.J. Opening- and closing-wedge distal femoral osteotomy: A systematic review of outcomes for isolated lateral compartment osteoarthritis. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116649901. 2325967116649901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distal femoral medial closing-wedge osteotomy on the right distal femur of a cadaveric specimen. The patient is positioned in the supine position, with viewing from the left side of the patient. Distal is to the left of the view and proximal is to the right. Dissection is taken down through the interval between the vastus medialis oblique and the intermuscular septum, exposing the medial cortex of the femur. The osteotomy site is marked with K-wires based on preoperative templating. Proximal and distal osteotomy cuts are made with care taken not to cut or fracture the lateral cortex, and the osteotomy is gently closed. An anteromedial-distal medial femur locking plate (Synthes) is placed and confirmed to be in the correct position using intraoperative fluoroscopy. The wound is then closed in layers.