Abstract
Arthroscopic procedures for treatment of hip pathology are growing exponentially as a result of continued improvements in the understanding of intra- and extra-articular hip anatomy and technological advancements in instrumentation. Nevertheless, it has been reported that the main cause of revision hip arthroscopy is related to a suboptimal intrasurgical management of the abnormal morphology in femoroacetabular impingement (FAI). Under-resection, over-resection, and in some cases combined under-resection and over-resection at different locations of the cam lesion at the femoral head-neck junction may lead to poor outcomes as a result of residual impingement or the iatrogenic creation of structural instability. Thus, an intraoperative assessment technique capable of revealing in real time the effect of the resection is vital for a successful procedure. Therefore, we present a technical note describing our preferred method to dynamically assess overall hip range of motion, motion at risk, and evaluation of the osteoplasty after surgical correction of FAI.
Femoroacetabular impingement (FAI) is one of the main causes of groin pain in active patients and has recently been recognized as one of the most common etiologies leading to osteoarthritis in the nondysplastic hip.1 The understanding of chondrolabral pathology and bony deformities associated with symptomatic FAI is evolving rapidly, and thus the numbers of trained hip arthroscopists and hip arthroscopy procedures are both increasing in recent years.2
Favorable clinical outcomes after hip arthroscopy have been reported in the literature, with several case series indicating good to excellent short- and intermediate-term clinical outcomes3, 4, 5 with low rates of complications. Nevertheless, treatment failures do occur in patients after arthroscopic surgery. Some patients continue to experience pain and poor functional outcomes and may be candidates for a revision procedure in the setting of recurrent or missed structural pathology.6 Under-resection, over-resection, and in some cases both under-resection and over-resection may lead to suboptimal outcomes as a result of residual impingement or the creation of structural instability.7
Philippon et al.8 and Ilizaliturri9 reported that failure to recognize or adequately reshape impinging bone might constitute the most common complication when treating FAI arthroscopically. Cadaveric studies revealed that arthroscopic trimming of the anterior femoral neck and acetabular rim is prone to error, and that performing adequate resection can be difficult, even in a laboratory setting.10, 11 Further, the use of radiography, either for preoperative planning or for intraoperative computer-assisted navigation, is complex and may not improve the accuracy of osteoplasty.12, 13, 14 Therefore, performing an intraoperative examination to fully evaluate hip range of motion, and to ascertain that there is no residual impingement, is of utmost importance to ensure that appropriate resection has been performed.
To improve results, and to allow for a reproducible method for real-time surgical decision making, the purpose of this technical note is to describe our dynamic hip examination technique for arthroscopic intraoperative osteoplasty control, without using fluoroscopic guidance.
Surgical Technique
Anesthesia and Patient Positioning
The patient is placed in a modified supine position on a traction table (Steris/Amsco, Mentor, OH). A combined epidural with a lumbar plexus sciatic regional block is our preferred anesthetic modality. After induction, a bilateral hip examination is performed to assess for range of motion. To prevent neurologic complications, an extra-wide perineal post is used to minimize pressure on the pudendal nerve and to force the femoral head laterally, shifting the vector of forces. The feet are placed in padded boots and secured. Traction is applied to the operative limb with 10 to 25 kg of force, with gentle countertraction applied to the contralateral limb (confirmed with a “vacuum sign” and 1 cm of joint distraction). The leg is positioned with 10° of lateral tilt, 10° of flexion, neutral abduction, and 15° of internal rotation. The knee ligaments are protected during the internal rotation by the use of an assistant slightly flexing the knee and guiding the limb during this maneuver. The time of traction application is noted, and continuous traction time is limited to less than 2 hours.
Diagnostic Arthroscopy
Routine preparation and draping of the affected hip is then performed, and standard anterolateral (ALP) and midanterior (MAP) portals are established to gain access to the central compartment (Fig 1). A 70° arthroscope is introduced through the ALP, and a diagnostic arthroscopy is performed to evaluate for intra-articular pathology. An interportal capsulotomy connecting the ALP and MAP is performed from the 12- to 3-o'clock position with a beaver blade (Arthrex, Naples, FL) approximately 1 cm distal to the labrum. FAI morphology, chondral damage, and any labral pathology are specifically and systematically addressed. All indicated procedures, including acetabular osteoplasty, subspinal decompression, labral repair, debridement, and femoral head-neck osteoplasty are then performed based on preoperative evaluation, diagnosis, and intraoperative findings.
Fig 1.
Right hip with the patient in the supine position illustrating the 2 standard portals for hip arthroscopy. (ALP, anterolateral portal; ASIS, anterosuperior iliac spine; MAP, midanterior portal.)
Dynamic Examination Technique
The dynamic examination is performed to guide the surgeon as to the amount of bone resection required and determine if sufficient osteoplasty has been performed to adequately address the impingement. The technique allows the surgeon to visualize if there is remnant bone that needs to be resected and allows the surgeon to precisely identify those areas. Furthermore, the technique allows the surgeon to specifically evaluate “motion at risk” if specific movements are required (i.e., in ice skating, gymnastics, or certain labor-intensive jobs). The examination can be repeated as many times as necessary until an adequate bony resection has been performed. Fluoroscopic examination is not necessary during the osteoplasty, if an appropriate dynamic examination is performed.15 When no bony impingement or labral displacement is observed during the dynamic examination, the osteoplasty is considered satisfactory. The key points of the dynamic examination technique are summarized in Table 1, and the technique is demonstrated in Video 1.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Have an appropriate fracture table that allows a large range of motion of the hip | An incomplete dynamic examination can lead to under-resection on the osteoplasty |
| Perform the examination after the assessment of the labrum and after the osteoplasty | |
| Always perform capsule closure |
After the treatment of central compartment pathologies, the traction is released and evaluation of the peripheral compartment begins. During examination of the peripheral compartment, the dynamic examination is performed looking for an excessive displacement of the labrum during a full range of motion of the hip. The camera is positioned in the MAP for proper visualization of the contact between the labrum and the femoral head. Through the other working portal (ALP), the capsule is retracted to improve visualization. To improve the dynamic examination, on some traction tables it is necessary to remove the foot from the foot pad or boot to increase the degrees of freedom of hip motion to complete an appropriate evaluation.
The dynamic examination starts by moving the hip from full extension into flexion in neutral abduction while directly visualizing the motion with the arthroscope. The hip is flexed to approximately 85° to 90° and then moved until full extension is again reached. Most of the patients with FAI typically lose the suction seal after 70° of flexion because of levering of the hip out of the socket by the cam lesion (Fig 2). This loss of seal should be re-established with an appropriate resection.
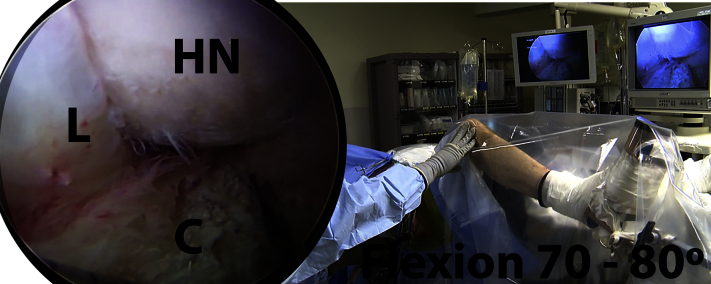
Fig 2.
Patient in the supine position with the right hip in around 70°-80° of flexion, neutral abduction and rotation. At this moment, the hip starts to lose the suction seal as a result of mixed-type impingement as seen in the arthroscopic view with the camera in the midanterior portal. (C, capsule; HN, head-neck junction; L, labrum.)
The hip is then sequentially abducted, and a 45° abduction test is performed in both extension and in 90° of flexion to evaluate possible superolateral impingement (Fig 3). Next, the hip is maneuvered into flexion with maximal internal rotation, and an anterior FAI (ie, FADIR) test is performed (Fig 4). These sequential maneuvers allow for a dynamic assessment of the bony morphology and the areas requiring resection.
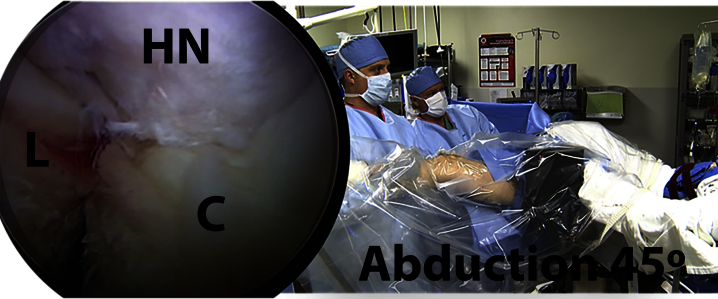
Fig 3.
Patient positioned supine in the traction table and arthroscopic view from the midanterior portal of the abduction test at 0° of flexion in a right hip to evaluate possible superolateral impingement. (C, capsule; HN, head-neck junction; L, labrum.)
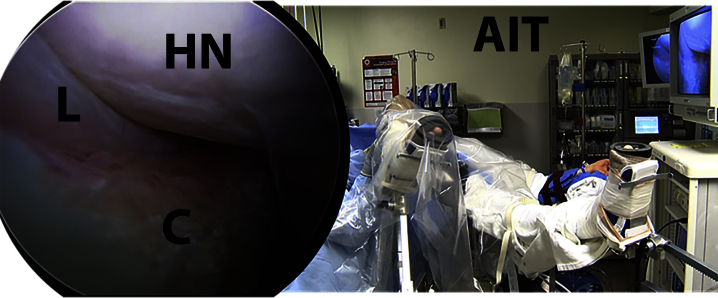
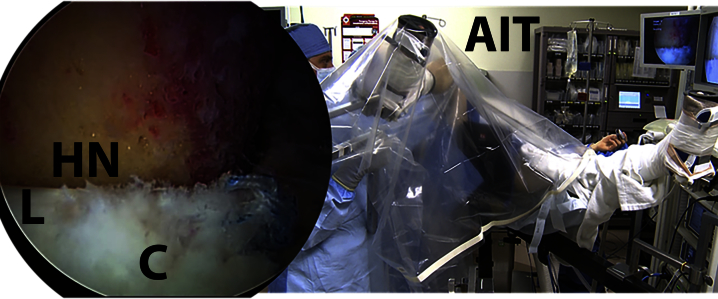
Fig 4.
Anterior impingement test in the right hip with the respective arthroscopic view from the midanterior portal showing the abutment of the head-neck junction against the acetabulum. (AIT, anterior impingement test; C, capsule; HN, head-neck junction; L, labrum.)
After dynamic assessment, the femoral head-neck osteoplasty is initiated with the burr in the ALP and the 70° arthroscope in the MAP, with the hip positioned at 45° of flexion, neutral rotation, and adduction/abduction. The proximal osteoplasty limit is approximately 15 mm from the labral edge after rim trimming and labral repair. The distal limit is defined as the distal ridge that usually is directly beneath the zona orbicularis. The lateral limit is defined as the lateral epiphyseal vessels and the Weitbrecht ligament medially, at an approximately 6-o'clock position. Usually, this initial position allows an osteoplasty from the 6- to the 10-o'clock position on the head-neck junction, to perform the osteoplasty in a position between 10 and 12 o'clock on the head-neck junction, a hip extension, slight traction, and exchange of the working portal to midanterior are needed.
The hip is then dynamically examined in the same manner as previously described, and further osteoplasty is performed as necessary based on these dynamic examination findings (Figs 5 and 6). Once the desired intra-articular result has been achieved, the hip is brought into flexion to relax the anterior capsule and facilitate the closure. An intra-articular cannula (Arthrex) is inserted through the MAP. A suture-shuttling device (SutureLasso; Arthrex) is used to approximate the proximal leaf of the capsule to the distal leaf passing a no. 2 Vycril in a suture relay technique. The bird-beak penetrator (Arthropierce, Smith & Nephew, Andover, MA) is then used to retrieve the lasso through the capsule on the distal side of the capsulotomy. The lasso is used to pass a permanent suture, achieving a side-to-side anastomosis. This is tied arthroscopically with racking half-hitch knots outside of the capsule. A total of 2 to 4 side-to-side sutures are placed to complete the capsular closure.
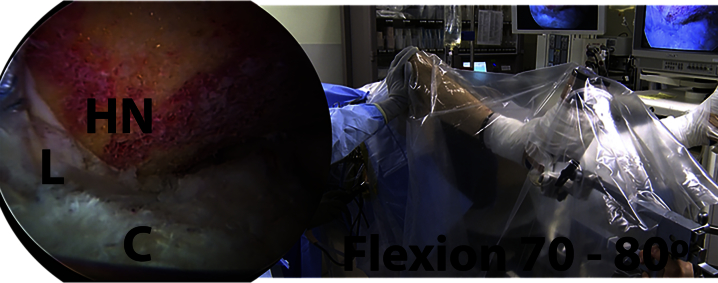
Fig 5.
After the labral repair and femoral osteoplasty, the initial dynamic test is repeated seeking for reminiscent impingement. Figure shows the right hip at 90° of flexion in neutral abduction and rotation and the arthroscopic view from the midanterior portal showing proper reshaping without suction seal loss. (C, capsule; HN, head-neck junction; L, labrum.)
Fig 6.
Patient positioned supine on the traction table. Figure shows the repetition of anterior impingement test on the right hip with the respective arthroscopic view from the midanterior portal after the labral repair and femoral osteoplasty, showing the absence of abutment of the head-neck junction against the acetabulum. (AIT, anterior impingement test; C, capsule; HN, head-neck junction; L, labrum.)
Discussion
The aim of femoral and acetabular osteoplasties for FAI is to restore impingement-free flexion/rotation without compromising the neck strength, joint surface area, joint stability, and suction seal. To accomplish these objectives, the surgeon must understand how diminished head-neck offset, acetabular overcoverage, and femoral version contribute to impingement. More importantly, it is important to have a method to plan and monitor bony resection during each case. Lavigne et al.14 described “dynamic evaluation” of the osteoplasty during an open “surgical dislocation” technique introduced by Ganz et al.16 With controlled dislocation, it is possible to visualize or palpate areas of impingement in positions of flexion, internal rotation, and adduction. The dynamic examination technique presented in this article allows the surgeon to test the hip in a full range of motion at all sites of possible impingement, seeking under-resected bone or early loss of the suction seal.
Previous studies documented bony FAI pathomorphology as the reason for most of the revision FAI surgery.8, 17, 18, 19 Philippon et al.8 noted that 36 of 37 hips meeting indications for revision hip arthroscopy had evidence of radiographic impingement lesions that were not addressed, or inadequately addressed, at the index procedure. Ross et al.19 reported 90% of patients undergoing secondary hip arthroscopy surgery were noted to have residual femoral and/or acetabular deformity, most often in the form of cam-type (36%) or combined cam- and pincer-type (50%) pathomorphology. Residual cam-type deformity in their series was most often encountered at the superolateral head-neck junction, on average at the 1:15-o'clock location. During the dynamic examination, this superolateral area on the femoral head can be addressed through the abduction test in extension and the remaining impingement is identified and treated.
Many hip arthroscopists use intraoperative fluoroscopy to avoid inadequate resection with residual impingement.19 Recently, Larson and Wulf 7 and Matsuda20 have described techniques wherein fluoroscopy is used to control the femoral or acetabular osteoplasty during arthroscopy. Previous studies have shown that it is unlikely that radiation exposure during fluoroscopy-assisted hip arthroscopy is high enough to cause health risks to the surgeon or patient.21, 22 However, a recently published study identified a lack of knowledge of radiation safety among orthopedic surgeons treating patients with FAI and reveals the need for greater education about this subject.23 Nogier et al.24 recently described a hip arthroscopy technique that eliminates the use of intraoperative fluoroscopy to reduce complications. This technique may reduce the use of intraoperative fluoroscopy and limit the patient's exposure to only pre- and postoperative imaging radiation. The advantages and disadvantages of this technique are summarized in Table 2.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| No need of fluoroscopy | Need of an assistant, out of the surgical field, to move the limb |
| Allows the visualization of any remaining bony “bump” after the osteoplasty | Sometimes visualization is compromised as a result of a small capsulotomy |
| Allows verification of the suction seal and labrum displacement | |
| Allows the evaluation of the motion at risk for each patient |
The hip dynamic examination technique described minimizes the use of fluoroscopy, the surgeon only needs fluoroscopy to check the joint distraction before the surgery starts. Therefore, even without fluoroscopy, the dynamic examination allows a complete assessment and treatment of the FAI with a minimal radiation exposition. We recommend this technique either in isolation or in combination with the use of fluoroscopy depending on physician comfort and experience. We encourage further research into dynamic examination techniques, as further study will help elucidate specific treatment recommendations.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.J.P. receives royalties from Smith & Nephew, Arthrosurface, DonJoy, Slack, Elsevier, Linvatec, and Bledsoe; receives board membership fees from ISHA; is a paid consultant for Smith & Nephew and MIS; and owns stock or stock options in Smith & Nephew, Arthrosurface, HIPCO, and MIS. Research or institutional support has been received from Smith & Nephew, Siemens, Vail Valley Medical Center, Ossur, and Arthrex.
Supplementary Data
This video details our technique of intraoperative dynamic examination of the hip. Standard anterolateral and midanterior portals are created in a right hip and a 70° arthroscope is used. First, a diagnostic arthroscopy is performed, inspecting both the central and peripheral compartment. Then, after intra-articular pathology is addressed and treated, the traction is released and the evaluation of the peripheral compartment begins. At this moment, the dynamic examination is performed looking for an excessive displacement of the labrum during a full range of motion of the hip. The camera is positioned in the midanterior portal for proper visualization of the contact between the labrum and the femoral head. Through the anterolateral portal, the capsule is retracted to improve visualization. The dynamic examination starts by moving the hip from extension to flexion in neutral abduction. The hip is flexed to approximately 85°-90° and then moved until full extension. Most of the patients with FAI usually lose the suction seal after 70° of flexion. Sequentially, a 45° abduction test is performed in extension and 90° of flexion to evaluate possible superolateral impingement. Next, a flexion with maximal internal rotation maneuver is performed, and an anterior FAI test is performed. Further osteoplasty is based on dynamic examination findings. When no labral displacement is observed during the dynamic examination, the osteoplasty is considered satisfactory.
References
- 1.Ganz R., Parvizi J., Beck M., Leunig M., Nötzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Colvin A.C., Harrast J., Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:e23. doi: 10.2106/JBJS.J.01886. [DOI] [PubMed] [Google Scholar]
- 3.Byrd J.W., Jones K.S. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 4.Potter B.K., Freedman B.A., Andersen R.C., Bojescul J.A., Kuklo T.R., Murphy K.P. Correlation of Short Form-36 and disability status with outcomes of arthroscopic acetabular labral debridement. Am J Sports Med. 2005;33:864–870. doi: 10.1177/0363546504270567. [DOI] [PubMed] [Google Scholar]
- 5.O'Leary J.A., Berend K., Vail T.P. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy. 2001;17:181–188. doi: 10.1053/jars.2001.21481. [DOI] [PubMed] [Google Scholar]
- 6.Ward J.P., Rogers P., Youm T. Failed hip arthroscopy: Causes and treatment options. Orthopedics. 2012;35:612–617. doi: 10.3928/01477447-20120621-11. [DOI] [PubMed] [Google Scholar]
- 7.Larson C.M., Wulf C.A. Intraoperative fluoroscopy for evaluation of bony resection during arthroscopic management of femoroacetabular joint impingement in the supine position. Arthroscopy. 2009;25:1183–1192. doi: 10.1016/j.arthro.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 9.Ilizaliturri V.M., Jr. Complications of arthroscopic femoroacetabular impingement treatment: A review. Clin Orthop Relat Res. 2008;467:760–768. doi: 10.1007/s11999-008-0618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mardones R., Lara J., Donndorff A. Surgical correction of “cam-type” femoroacetabular impingement: A cadaveric comparison of open versus arthroscopic debridement. Arthroscopy. 2009;25:175–182. doi: 10.1016/j.arthro.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Zumstein M., Hahn F., Sukthankar A., Sussmann P.S., Dora C. How accurately can the acetabular rim be trimmed in hip arthroscopy for pincer-type femoral acetabular impingement: A cadaveric investigation. Arthroscopy. 2009;25:164–168. doi: 10.1016/j.arthro.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Brunner A., Horisberger M., Herzog R.F. Evaluation of a computed tomography-based navigation system prototype for hip arthroscopy in the treatment of femoroacetabular cam impingement. Arthroscopy. 2009;25:382–391. doi: 10.1016/j.arthro.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 13.Tannast M., Kubiak-Langer M., Langlotz F., Puls M., Murphy S.B., Siebenrock K.A. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. doi: 10.1002/jor.20309. [DOI] [PubMed] [Google Scholar]
- 14.Lavigne M., Parvizi J., Beck M., Siebenrock K.A., Ganz R., Leunig M. Anterior femoroacetabular impingement: Part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. [PubMed] [Google Scholar]
- 15.Bhatia S., Briggs K.K., Philippon M.J., Soares E. Post-operative alpha angle not associated with outcomes 5 years following hip arthroscopy for FAI. Arthroscopy. 2016;32:e12–e13. doi: 10.1007/s00167-018-4933-3. [DOI] [PubMed] [Google Scholar]
- 16.Ganz R., Gill T.J., Gautier E., Ganz K., Krugel N., Berlemann U. Surgical dislocation of the adult hip. A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 17.Bogunovic L., Gottlieb M., Pashos G., Baca G., Clohisy J.C. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res. 2013;471:2523–2529. doi: 10.1007/s11999-013-3015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larson C.M., Giveans M.R., Samuelson K.M., Stone R.M., Bedi A. Outcomes after revision arthroscopy for hip impingement. Am J Sports Med. 2014;42:1785–1790. doi: 10.1177/0363546514534181. [DOI] [PubMed] [Google Scholar]
- 19.Ross J.R., Larson C.M., Adeoyo O.A., Kelly B.T., Bedi A. Residual deformity is the most common reason for revision hip arthroscopy: A three-dimensional CT study. Clin Orthop Relat Res. 2015;473:1388–1395. doi: 10.1007/s11999-014-4069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuda D.K. Fluoroscopic templating technique for precision arthroscopic rim trimming. Arthroscopy. 2009;25:1175–1182. doi: 10.1016/j.arthro.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 21.Budd H., Patchava A., Khanduja V. Establishing the radiation risk from fluoroscopic-assisted arthroscopic surgery of the hip. Int Orthop. 2012;36:1803–1806. doi: 10.1007/s00264-012-1557-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaymer C.E., Achten J., Auckett R., Cooper L., Griffin D. Fluoroscopic radiation exposure during hip arthroscopy. Arthroscopy. 2013;29:870–873. doi: 10.1016/j.arthro.2013.01.024. [DOI] [PubMed] [Google Scholar]
- 23.Saroki A.J., Wijdicks C., Philippon M.J., Bedi A. Orthopaedic surgeons' use and knowledge of ionizing radiation during surgical treatment for femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2016;24:3962–3970. doi: 10.1007/s00167-015-3734-1. [DOI] [PubMed] [Google Scholar]
- 24.Nogier A., Boyer T., Khan M.T. Hip arthroscopy: Less invasive technique. Arthrosc Tech. 2014;3:e101–e106b. doi: 10.1016/j.eats.2013.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video details our technique of intraoperative dynamic examination of the hip. Standard anterolateral and midanterior portals are created in a right hip and a 70° arthroscope is used. First, a diagnostic arthroscopy is performed, inspecting both the central and peripheral compartment. Then, after intra-articular pathology is addressed and treated, the traction is released and the evaluation of the peripheral compartment begins. At this moment, the dynamic examination is performed looking for an excessive displacement of the labrum during a full range of motion of the hip. The camera is positioned in the midanterior portal for proper visualization of the contact between the labrum and the femoral head. Through the anterolateral portal, the capsule is retracted to improve visualization. The dynamic examination starts by moving the hip from extension to flexion in neutral abduction. The hip is flexed to approximately 85°-90° and then moved until full extension. Most of the patients with FAI usually lose the suction seal after 70° of flexion. Sequentially, a 45° abduction test is performed in extension and 90° of flexion to evaluate possible superolateral impingement. Next, a flexion with maximal internal rotation maneuver is performed, and an anterior FAI test is performed. Further osteoplasty is based on dynamic examination findings. When no labral displacement is observed during the dynamic examination, the osteoplasty is considered satisfactory.