Abstract
Objective
To examine the role of patient, hospital, and community characteristics on racial and ethnic disparities in in‐hospital postsurgical complications.
Data Sources
Healthcare Cost and Utilization Project, 2011 State Inpatient Databases; American Hospital Association Annual Survey of Hospitals; Area Health Resources Files; Centers for Medicare & Medicaid Services Hospital Compare database.
Methods
Nonlinear hierarchical modeling was conducted to examine the odds of patients experiencing any in‐hospital postsurgical complication, as defined by Agency for Healthcare Research and Quality Patient Safety Indicators.
Principal Findings
A total of 5,474,067 inpatient surgical discharges were assessed using multivariable logistic regression. Clinical risk, payer coverage, and community‐level characteristics (especially income) completely attenuated the effect of race on the odds of postsurgical complications. Patients without private insurance were 30 to 50 percent more likely to have a complication; patients from low‐income communities were nearly 12 percent more likely to experience a complication. Private, not‐for‐profit hospitals in small metropolitan or micropolitan areas and higher nurse‐to‐patient ratios led to fewer postsurgical complications.
Conclusions
Race does not appear to be an important determinant of in‐hospital postsurgical complications, but insurance and community characteristics have an effect. A population‐based approach that includes improving the socioeconomic context may help reduce disparities in these outcomes.
Keywords: Postsurgical complications, surgery, racial/ethnic differences in health care, community socioeconomic status, health insurance, health disparities
Improving patient safety and the quality of health care is a national priority in the United States (AHRQ 2014a). Despite significant advances in medicine and public health, disparities in the quality of health care persist and the specific causes remain unclear (AHRQ 2014b). Racial disparities in inpatient care are well documented (Smedley, Stith, and Nelson 2003); however, less is known about the quality of care that minorities receive with regard to surgical procedures. In particular, little is known about the multiple factors that may contribute to racial disparities in postsurgical outcomes.
The importance of patient‐related characteristics in explaining racial disparities in postsurgical complications is equivocal. Some studies report no such differences after controlling for sociodemographic and medical characteristics (Fiscella et al. 2005; Metersky et al. 2011), whereas other studies show higher rates of postsurgical complications among patients who are black compared with those who are non‐Hispanic white (Coffey, Andrews, and Moy 2005; Gaskin et al. 2008; Brooks Carthon et al. 2013).
The degree to which hospital characteristics contribute to differences in outcomes among racial and ethnic groups also remains unclear. Some studies show that differences in postsurgical outcomes between black and non‐Hispanic white populations may be attributable to the hospitals at which minorities are likely to be treated (Gaskin et al. 2008; Ly et al. 2010). In contrast, other researchers have found that disparities for black patients in postsurgical outcomes persist even after they control for a broad range of hospital characteristics (hospital ownership, hospital bed size, hospital volume, average daily census, utilization rate, patient‐to‐nurse ratio, health system membership, safety‐net status, technology sophistication) (Fiscella et al. 2005; Gaskin et al. 2011; Brooks Carthon et al. 2013; Dehal, Abbas, and Johna 2013) and hospital environmental characteristics (market competition, patient racial, payer and income mix, urban–rural, income of the hospital county) (Fiscella et al. 2005; Gaskin et al. 2011; Brooks Carthon et al. 2013).
In this paper, we purport that patient safety be viewed within a broader systems and community context to aid in understanding disparities. In particular, community characteristics have largely been unexplored, with the exception of community socioeconomic status (SES). Moreover, the inclusion of community SES has largely been used as a proxy for patient SES. Some studies report no racial disparities after controlling for sociodemographic and medical characteristics (Fiscella et al. 2005; Metersky et al. 2011), whereas other studies show higher rates of postsurgical complications among black patients compared with non‐Hispanic white patients while accounting for socioeconomic characteristics (in varying ways) (Coffey, Andrews, and Moy 2005; Brooks Carthon et al. 2013).
Several critical gaps exist in the literature that may help identify the sources of racial disparities in postsurgical complications. Little is known about the underlying multilevel characteristics (i.e., patient, hospital, and community) that may contribute to observed racial and ethnic disparities in outcomes. Specifically, very few studies have explicitly examined how the patient's residential community may influence such differences in postsurgical complications. Although a few studies have included measures of community SES (Coffey, Andrews, and Moy 2005; Gaskin et al. 2011; Brooks Carthon et al. 2013), there is insufficient evidence to definitively quantify the role of socioeconomic characteristics in racial and ethnic differences in postsurgical complications.
There are several potential pathways by which the patient's residential community SES along with patient and hospital factors could impact the risk for surgical complications and thereby help in understanding disparities. Community SES may be associated with cultural, health literacy, and language‐related factors; the in‐hospital treatment of patients from low SES communities; and the availability of health care resources such as the number and quality of surgeons.
To address these gaps in the literature and to determine the most salient characteristics that contributed to postsurgical complications, the present study examined (1) whether in‐hospital postsurgical complications varied by patient race and ethnicity and (2) the role of patient‐, hospital‐, and community‐level characteristics. In addition to examining these multiple characteristics, this study advances the research on disparities in patient safety by incorporating the present on admission (POA) data element (critical for identifying complications that began in the hospital), using all‐payer data from most states in the nation. This study draws upon multiple data sources and accounts for other multilevel characteristics through multivariable analyses.
Methods
Data Sources
Data were from the 2011 Healthcare Cost and Utilization Project (HCUP) all‐payer State Inpatient Databases (SID) (http://www.hcup-us.ahrq.gov/). HCUP SID include discharge summary records that contain demographic and clinical information for all inpatient discharges in nearly all hospitals from participating states. We included supplemental data from the American Hospital Association (AHA) Annual Survey of Hospitals, Area Health Resources Files (AHRF), and the Centers for Medicare & Medicaid Services (CMS) Hospital Compare database.
Study Population
We targeted adults aged 18 years and older who were undergoing surgical procedures during inpatient admissions at community, nonrehabilitation hospitals. For inclusion in this study, discharge records needed to indicate both a surgical diagnosis‐related group (DRG) and an operating room (OR) procedure. To distinguish complications arising during the hospitalization from those already present before admission, we only included data from states with POA indicators in the SID. A total of 35 states contributed inpatient discharge data with POA flags for each diagnosis in the SID in 2011, totaling 7,339,712 adult surgical discharges.
From this population, we sequentially applied exclusion criteria to produce the final study sample (Figure 1). We first excluded discharges from hospitals exempt from CMS reporting of POA, hospitals without reliable POA reporting (e.g., hospitals only reporting POA on Medicare discharges or POA not reported on the majority of diagnoses), and discharges with missing POA indicators (N = 399,036 discharges; 5.4 percent). We then excluded hospitals without racial/ethnic data and those with racial/ethnic data that had poor quality (N = 383,647 discharges; 5.2 percent). We defined poor‐quality racial/ethnic data in a manner consistent with the methods used in support of the National Healthcare Disparities Report (Coffey et al. 2012). Next, we excluded hospitals in remote rural counties (counties that were not in Core‐Based Statistical Areas) (N = 52,805 discharges; 0.7 percent). Most hospitals in non‐Core‐Based Statistical Area counties had already been excluded, as they were generally Critical Access Hospitals and therefore exempt from CMS reporting of POA. We excluded these hospitals to maintain the homogeneity of the hospital sample. Finally, we excluded discharges when key data elements (e.g., AHA data, Hospital Compare data, primary expected payer, quartile of median household income in the patient's ZIP Code) were missing (N = 1,030,157 discharges; 14.0 percent). The final sample consisted of 5,474,067 discharges, or 74.6 percent of the initial adult surgical discharge population. This sample includes discharges from 1,703 hospitals in 30 states.
Figure 1.
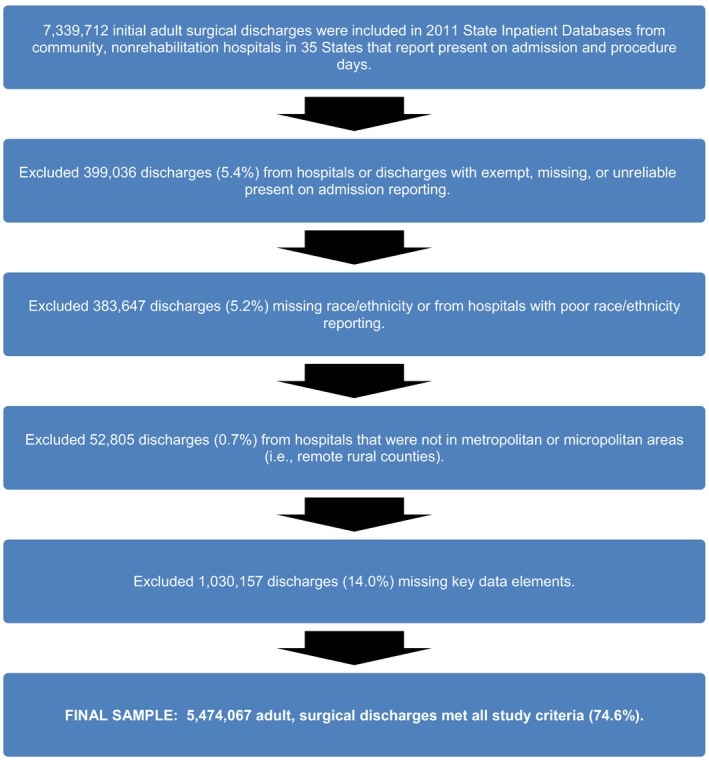
Sample Selection Criteria
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases (2011).
Variables
Dependent Variable: In‐Hospital Postsurgical Complications
The dependent variable was a measure of postsurgical complications occurring in the hospital. We identified eight Agency for Healthcare Quality and Research (AHRQ) Patient Safety Indicators (PSIs) as measures with documented disparities in surgical complications, based on examination of tables from the National Healthcare Quality Report and the National Healthcare Disparities Report (AHRQ 2014b). Specifically, we selected PSIs 06 (Adult Iatrogenic Pneumothorax Rate), 07 (Adult Central Venous Catheter‐Related Bloodstream Infections Rate), 09 (Adult Postoperative Hemorrhage or Hematoma Rate), 10 (Adult Postoperative Physiologic and Metabolic Derangement Rate), 11 (Adult Postoperative Respiratory Failure Rate), 12 (Adult Postoperative Pulmonary Embolism or Deep Vein Thrombosis Rate), 13 (Adult Postoperative Sepsis Rate), and 15 (Adult Accidental Puncture or Laceration Rate). We operationalized the PSIs into a measure of postsurgical complication as a binary variable indicating the presence of any one of the eight complications from surgery. Many of the PSIs were very rare and therefore had a low frequency of the event. Therefore, the PSIs were combined into a dichotomized variable for these analyses.
Primary Independent Variable: Race/Ethnicity
Race and ethnicity served as the predictor variables of interest. We measured race and ethnicity as reported in the SID. To attain sufficient power for analysis, we used four categories: black (non‐Hispanic), white (non‐Hispanic), other (non‐Hispanic), and Hispanic. We included additional covariates in the analysis to isolate the effects of race/ethnicity on postsurgical complications. These can be categorized into three distinct levels: patient, hospital, and community characteristics.
Patient Characteristics
We included primary expected payer for the hospital admission (Medicare, Medicaid, private insurance, uninsured, or other) as a patient‐level covariate. Payer types are derived from the expected payment source at time of admission or discharge. We defined uninsured populations as patients with an expected payment source of “self‐pay” or “no charge.” In addition, we included a clinical risk adjustment score as an offset variable based on PSI methodology (AHRQ 2012). The risk adjustment score incorporated patient age, sex, comorbidities identified on the discharge record, the specific surgical procedure, and a measure of clinical risk defined through the modified DRGs. The risk adjustment score was an externally derived standard (or benchmark) based on a large, multistate database to control for risk of surgical complication due to age, sex, DRG, and comorbidities appearing on the discharge record. Specifically, we used the PSI risk adjustment models (i.e., we applied the risk adjustment coefficients specific to each PSI) to calculate the score (AHRQ 2012).
Hospital Characteristics
We obtained hospital characteristics using data from the AHA Annual Survey of Hospitals. The characteristics included bed size (less than 100 beds, 100–299 beds, 300–499 beds, or 500 or more beds); teaching status (teaching or nonteaching); hospital ownership (government, private nonprofit, or private for‐profit); hospital urban or rural location based on the 2006 NCHS Urban‐Rural Classification Scheme for Counties (Ingram and Franco 2012) (large metropolitan, small metropolitan, or micropolitan); region (Northeast, Midwest, South, or West); and nurse staffing (number of registered nurses per 1,000 inpatient days). Finally, we estimated the hospital's level of technological sophistication with the Saidin index of available technologies in a hospital weighted by the relative rarity of that technology across all hospitals. The hospital services included in our index are described in the Technical Appendix, and the methodology is described in published literature (Spetz and Baker 1999).
We used available measures from the CMS Hospital Compare data to construct an additional hospital‐level factor quantifying hospital surgical quality. These measures were originally developed for the Hospital Inpatient Quality Reporting program and are currently being used by the Hospital Value‐Based Purchasing (HVBP) program. HVBP data contain a Total Performance Score, which includes clinical and patient‐experience measures. The surgical quality composite measure uses seven Inpatient Quality Reporting measures related to surgical quality, which is a subset of the clinical care measures used by HVBP. The measures from Hospital Compare included in the derivation of the surgical quality composite measure came from two sets of data. The first set was the Surgical Care Improvement Project (SCIP) health care‐associated infections (Inf) data labeled SCIP‐Inf‐1, Prophylactic Antibiotic Received within 1 hour Prior to Surgical Incision; SCIP‐Inf‐2, Prophylactic Antibiotic Selection for Surgical Patients; SCIP‐Inf‐3, Prophylactic Antibiotics Discontinued within 24 hours after Surgery End Time; and SCIP‐Inf‐4, Cardiac Surgery Patients with Controlled 6:00 a.m. Postoperative Serum Glucose. The second set was cardiology (Card) data labeled SCIP‐Card‐2, Surgery Patients on a Beta Blocker Prior to Arrival that Received a Beta Blocker during the Perioperative Period and venous thromboembolism (VTE) data labeled SCIP‐VTE‐1, Surgery Patients with Recommended VTE Prophylaxis Ordered and SCIP‐VTE‐2, Surgery Patients Who Received Appropriate VTE Prophylaxis within 24 hours prior to Surgery to 24 hours after Surgery. See the Technical Appendix for additional details about the surgical quality composite measure.
Community Characteristics
We included three variables to account for SES within the patient's community. The HCUP SID contain discharge‐level median household income of the patient's ZIP Code, categorized in population‐weighted quartiles, which we used as one measure of community SES. We also used AHRF data to measure county‐level educational attainment (percentage of adults aged 25 years and older with a high school diploma or a college degree) and county‐level employment (the unemployment rate for individuals aged 16 years and older). We also studied community health characteristics such as the County Health Rankings for Health Behaviors and Community Care that were ultimately deemed highly correlated with the measures above and insignificantly associated with in‐hospital surgical complications. All community‐level characteristics corresponded to the patient's community of residence rather than the location of the hospital.
Statistical Approach
Given the multilevel nature of the data, we adopted a nonlinear hierarchical modeling approach. This approach accounted for multiple sources of variation and appropriately assessed the statistical significance of patient‐, hospital‐, and community‐level effects. We clustered patients (level 1) within both hospitals and communities (level 2). However, because the community‐level characteristics corresponded to patient residence and not hospital location, hospitals were not strictly nested within communities. This data structure is described as a cross‐classified, multilevel model (Fielding and Goldstein 2006). We performed five progressive hierarchical logistic regression models. A base model estimated the unadjusted effect of race/ethnicity on in‐hospital postsurgical complications. The second model added the patient‐level clinical risk adjustment, and the third model the patient‐level expected primary payer. The fourth and fifth models added hospital and community‐level characteristics, respectively.
We included the clinical risk adjustment score as an offset variable in Models 2 through 5 of the regression analyses. The goal was to determine whether deviations from this standard can be explained by community, hospital, and patient characteristics other than characteristics used to derive the standard. Therefore, we implemented a hierarchical logistic regression, with the dependent variable equal to the difference between (1) the log‐odds of a complication in our study data and (2) the “expected” log‐odds of a complication predicted from the standard. We accomplished this by entering the expected log‐odds of a complication as an offset variable in the regression. Consequently, the “odds ratios” estimated for each of the independent variables in the regressions can be interpreted as the multiple of the ratio (predicted odds)/(expected odds) estimated for a one‐unit change in the independent variable.
Results
Bivariate Analysis
Table 1 shows the bivariate results of patient‐, hospital‐ and community‐level characteristics by in‐hospital, postsurgical complication status (yes or no). We found 231,823 inpatient surgeries that resulted in a complication, representing 4.2 percent of 5.47 million inpatient surgical discharges among the study population. On average, patients who experienced postsurgical complications had a longer length of stay in the hospital compared with those who did not experience a complication (16.7 vs. 4.6, respectively; p < .01). Patients who experienced a postsurgical complication were more likely to be older and male, have a larger risk adjustment score, more comorbidities, and be insured through Medicare. By race/ethnicity, those who experienced a postsurgical complication were more likely to be black (non‐Hispanic) and less likely to be Hispanic than those who did not experience a complication. Differences in the rate of postsurgical complications by hospital characteristics were statistically significant but substantively smaller. Postsurgical complications were more likely if patients were treated at a teaching hospital, a hospital with a larger number of beds, one with higher nurse staffing levels, or one that was government owned or located in the Midwest or in a large metropolitan area. Hospitals characterized as having a higher level of technology or lower surgical quality were also associated with larger percentages of patients with postsurgical complications. Patients who experienced complications were more likely to live in communities where there were higher percentages of adults with a high school diploma or college degree, there was a higher rate of unemployment, and residents had low income.
Table 1.
Select Patient, Hospital, and Community Characteristics, by In‐Hospital Surgical Complication Status
| Characteristic | No Inpatient Surgical Complications | Inpatient Surgical Complications | p‐Value for Pairwise Comparison |
|---|---|---|---|
| Discharges, n | 5,242,244 | 231,823 | |
| Length of stay, mean | 4.62 | 16.74 | <.0001 |
| Patient characteristics | |||
| Race/ethnicity, %a | |||
| White (non‐Hispanic) | 71.00 | 71.42 | <.0001 |
| Black (non‐Hispanic) | 11.05 | 13.21 | <.0001 |
| Other (non‐Hispanic) | 6.05 | 5.89 | 0.0023 |
| Hispanic | 11.90 | 9.47 | <.0001 |
| Age, mean | 55.19 | 62.42 | <.0001 |
| Sex, %a,b | |||
| Female | 60.71 | 49.65 | <.0001 |
| Male | 39.29 | 50.35 | <.0001 |
| Risk adjustment score based on PSI methodology, mean | –3.67 | –1.93 | <.0001 |
| Sum of comorbidities, mean | 1.88 | 3.54 | <.0001 |
| Primary expected payer, %a | |||
| Medicare | 37.99 | 52.34 | <.0001 |
| Medicaid | 13.43 | 10.73 | <.0001 |
| Private insurance | 39.89 | 28.38 | <.0001 |
| Uninsured | 5.25 | 5.73 | <.0001 |
| Other | 3.44 | 2.82 | <.0001 |
| Hospital characteristics | |||
| Teaching status, %a,b | |||
| Teaching | 54.99 | 61.93 | <.0001 |
| Nonteaching | 45.01 | 38.07 | <.0001 |
| Bed size, mean | 437.32 | 481.00 | <.0001 |
| Bed size, %a | |||
| <100 beds | 5.24 | 3.14 | <.0001 |
| 101–200 beds | 15.59 | 12.48 | <.0001 |
| 201–349 beds | 27.53 | 25.38 | <.0001 |
| ≥350 beds | 51.63 | 59.00 | <.0001 |
| Ownership status, %a | |||
| Government | 10.62 | 12.61 | <.0001 |
| Private, for‐profit | 13.00 | 11.15 | <.0001 |
| Private, nonprofit | 76.39 | 76.24 | 0.1163 |
| Hospital region, %a | |||
| Northeast | 24.07 | 23.57 | <.0001 |
| Midwest | 16.76 | 17.65 | <.0001 |
| South | 34.96 | 34.97 | 0.9292 |
| West | 24.21 | 23.81 | <.0001 |
| Hospital location, %a | |||
| Large metropolitan | 61.20 | 63.05 | <.0001 |
| Small metropolitan | 33.74 | 33.05 | <.0001 |
| Micropolitan | 5.06 | 3.91 | <.0001 |
| Saidin index of hospital technology, mean | 9.87 | 10.38 | <.0001 |
| Number of full‐time‐equivalent RNs per 1,000 inpatient days, mean | 4.48 | 4.53 | <.0001 |
| Surgical quality composite measure, mean | 56.24 | 55.20 | <.0001 |
| Community characteristics | |||
| Individuals aged 25+ years with high school diploma or more, % in county | 15.30 | 15.39 | <.0001 |
| Rate of unemployed aged 16 years or older, mean | 9.33 | 9.39 | <.0001 |
| Median household income in patient's ZIP code, %a | |||
| Quartile 1 (lowest) | 24.27 | 26.73 | <.0001 |
| Quartile 2 | 23.88 | 24.43 | <.0001 |
| Quartile 3 | 26.85 | 26.13 | <.0001 |
| Quartile 4 (highest) | 24.99 | 22.72 | <.0001 |
Percentages are column percentages.
Statistically significant differences by group.
IHS, Indian Health Service; PSI, Patient Safety Indicators, RN, registered nurse.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases (2011).
Figure 2 shows the observed in‐hospital postsurgical complication rates per 1,000 discharges by patient race and ethnicity. The overall mean rate of postsurgical complications was 42.3 per 1,000 surgery discharges. Black (non‐Hispanic) patients had the highest postsurgical complication rate, with a rate of 50.2 per 1,000 surgical discharges. The complication rates for white (non‐Hispanic) and other (non‐Hispanic) patients were 42.6 and 41.3, respectively. Hispanic patients had the lowest rate of surgical complications, at 34.0 per 1,000 surgical discharges.
Figure 2.
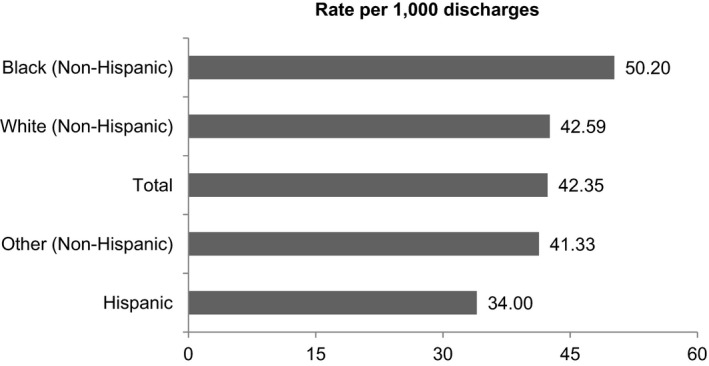
In‐Hospital Surgical Complication Rate (Observed), by Patient Race and Ethnicity
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases (2011).
Multivariable Analyses
To further evaluate the effect of race and ethnicity on in‐hospital surgical complications, we performed progressive multivariable hierarchical logistic regressions (Table 2). The base (unadjusted) model (Model 1) showed that black (non‐Hispanic) patients were 8.8 percent more likely to experience a complication compared with white (non‐Hispanic) patients (odds ratio [OR], 1.088; 95 percent confidence interval [CI], 1.073–1.104). Hispanic patients were less likely to experience a complication compared with white patients (Hispanic OR, 0.746; 95 percent CI, 0.734–0.759). Model 2 included a measure of clinical risk as an offset. The odds ratios for race and ethnicity were attenuated for black (non‐Hispanic) patients (OR, 1.033; 95 percent CI, 1.017–1.049) and Hispanic patients (OR, 0.889; 95 percent CI, 0.874–0.906). Model 3 added expected primary payer. The odds ratios for race were further attenuated for black (non‐Hispanic) patients (OR, 1.025; 95 percent CI, 1.009–1.041). The inclusion of hospital characteristics did not significantly change the point estimates for race or ethnicity (Model 4). When community characteristics were included in the model of complications (Model 5), the effect of being black (non‐Hispanic) was eliminated and no longer statistically significant (OR, 1.004; 95 percent CI, 0.988–1.020). In the final model, Hispanic patients remained significantly less likely to experience an in‐hospital surgical complication (OR, 0.866; 95 percent CI, 0.850–0.882).
Table 2.
Multivariable Hierarchical Logistic Regression (Clustering for Hospital and Patient County) Showing the Odds of In‐Hospital Surgical Complications at the Discharge Level
| Characteristic | Model 1 | Model 2a | Model 3a | Model 4a | Model 5a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio | Lower CI | Upper CI | Odds Ratio | Lower CI | Upper CI | Odds Ratio | Lower CI | Upper CI | Odds Ratio | Lower CI | Upper CI | Odds Ratio | Lower CI | Upper CI | |
| Patient characteristics | |||||||||||||||
| Patient race/ethnicity | |||||||||||||||
| White (non‐Hispanic) (ref) | |||||||||||||||
| Black (non‐Hispanic) | 1.088 | 1.073 | 1.104 | 1.033 | 1.017 | 1.049 | 1.025 | 1.009 | 1.041 | 1.022 | 1.007 | 1.038 | 1.004 | 0.988 | 1.020 |
| Other (non‐Hispanic) | 0.920 | 0.903 | 0.938 | 1.010 | 0.989 | 1.031 | 1.015 | 0.994 | 1.036 | 1.013 | 0.992 | 1.034 | 1.009 | 0.988 | 1.030 |
| Hispanic | 0.746 | 0.734 | 0.759 | 0.889 | 0.874 | 0.906 | 0.881 | 0.865 | 0.897 | 0.879 | 0.864 | 0.895 | 0.866 | 0.850 | 0.882 |
| Primary payer | |||||||||||||||
| Medicare | 1.426 | 1.411 | 1.441 | 1.426 | 1.411 | 1.441 | 1.419 | 1.404 | 1.435 | ||||||
| Medicaid | 1.508 | 1.483 | 1.534 | 1.510 | 1.484 | 1.535 | 1.493 | 1.468 | 1.519 | ||||||
| Private insurance (ref) | |||||||||||||||
| Uninsured | 1.321 | 1.293 | 1.35 | 1.321 | 1.292 | 1.350 | 1.311 | 1.282 | 1.339 | ||||||
| Other | 1.357 | 1.318 | 1.397 | 1.358 | 1.319 | 1.397 | 1.353 | 1.315 | 1.393 | ||||||
| Hospital characteristics | |||||||||||||||
| Teaching | 1.069 | 1.022 | 1.118 | 1.066 | 1.019 | 1.115 | |||||||||
| Bed size | |||||||||||||||
| <100 beds (ref) | |||||||||||||||
| 101–200 beds | 1.132 | 1.067 | 1.202 | 1.132 | 1.066 | 1.202 | |||||||||
| 201–349 beds | 1.165 | 1.088 | 1.249 | 1.161 | 1.084 | 1.245 | |||||||||
| ≥350 beds | 1.240 | 1.139 | 1.348 | 1.232 | 1.132 | 1.340 | |||||||||
| Ownership status | |||||||||||||||
| Government | 1.037 | 0.965 | 1.115 | 1.042 | 0.970 | 1.120 | |||||||||
| Private not‐for‐profit | 0.938 | 0.891 | 0.988 | 0.944 | 0.897 | 0.994 | |||||||||
| Private for‐profit (ref) | |||||||||||||||
| Hospital region | |||||||||||||||
| Northeast (ref) | |||||||||||||||
| Midwest | 1.017 | 0.958 | 1.081 | 1.013 | 0.954 | 1.076 | |||||||||
| South | 1.051 | 0.996 | 1.110 | 1.029 | 0.974 | 1.088 | |||||||||
| West | 1.017 | 0.957 | 1.081 | 1.025 | 0.963 | 1.091 | |||||||||
| Hospital location | |||||||||||||||
| Large metropolitan (ref) | |||||||||||||||
| Small metropolitan | 0.960 | 0.922 | 1.000 | 0.940 | 0.902 | 0.979 | |||||||||
| Micropolitan | 0.817 | 0.768 | 0.869 | 0.787 | 0.740 | 0.838 | |||||||||
| Saidin Index of hospital technology | 1.023 | 1.015 | 1.032 | 1.024 | 1.015 | 1.032 | |||||||||
| Number of full‐time‐ equivalent RN's per 1,000 inpatient days, mean of hospitals | 0.982 | 0.971 | 0.994 | 0.983 | 0.971 | 0.994 | |||||||||
| Surgical quality composite measure | 0.999 | 0.998 | 1.000 | 0.999 | 0.998 | 1.000 | |||||||||
| Community characteristics | |||||||||||||||
| Percentage of people 25+ with high school diploma or more | 1.002 | 1.000 | 1.004 | ||||||||||||
| Rate of unemployed aged 16 or older, mean | 0.994 | 0.989 | 0.999 | ||||||||||||
| Median household income in patient's ZIP Code | |||||||||||||||
| Quartile 1 (lowest) | 1.116 | 1.097 | 1.136 | ||||||||||||
| Quartile 2 | 1.084 | 1.066 | 1.102 | ||||||||||||
| Quartile 3 | 1.053 | 1.038 | 1.069 | ||||||||||||
| Quartile 4 (highest) (ref) | |||||||||||||||
Notes. Model 1 estimates the effect of race/ethnicity on any in‐hospital, postsurgical complications. Model 2 adds a measure of clinical risk. Model 3 adds other patient attributes. Model 4 adds hospital characteristics. Model 5 adds community characteristics.
Model uses severity score as an offset.
AOR, adjusted odds ratio; CI, 95% confidence interval; ref, reference group.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases (2011).
The final, fully adjusted multivariable model (Model 5) shows all measured determinants of the occurrence of in‐hospital postsurgical complications and their relative strength. The patient's expected primary payer of care was the strongest determinant of complications. Patients covered by Medicare (OR, 1.419; 95 percent CI, 1.404–1.435), Medicaid (OR, 1.493; 95 percent CI, 1.468–1.519), some other nonprivate form of insurance (OR, 1.353; 95 percent CI, 1.315–1.393), or those who were uninsured (OR, 1.311; 95 percent CI, 1.282–1.339) were significantly more likely to experience a complication following surgery, compared with their privately insured counterparts. Several hospital characteristics were also statistically associated with increased odds of in‐hospital surgical complications. Patients who were treated at teaching hospitals were 6.6 percent more likely to experience a complication. Patients who were treated at hospitals with a larger bed size and a higher level of technological sophistication were more likely to have a complication. Patients were less likely to have a postsurgical complication if they were treated at hospitals that were private not‐for‐profit or were located in small metropolitan or micropolitan areas. Patients in hospitals with higher nurse‐to‐patient ratios experienced fewer complications (OR, 0.983; CI, 0.971–0.994 for an increase of one nurse per 1,000 inpatient days). Adding one nurse per 1,000 patient days was associated with a 1.7 percent lower likelihood of a surgical complication. Of the community characteristics, the median household income in the patient's ZIP code was significantly related to the occurrence of complications (OR, 1.116; CI, 1.097–1.136), whereas the unemployment rate was associated with fewer complications.
Discussion
This study examined the characteristics associated with in‐hospital postsurgical complications for a variety of hospital‐based surgical procedures. Specifically, we examined (1) whether in‐hospital, postsurgical complications varied by patient race and ethnicity and (2) if and to what extent patient‐, hospital‐, and community‐level characteristics attenuated this relationship. These results allowed us to determine the most salient characteristics that are associated with complications. The findings have important implications for research, clinical practice, and health policy.
Our unadjusted findings revealed that black (non‐Hispanic) patients were more likely to experience inpatient postsurgical complications; the size of this effect was modest but statistically significant. Moreover, in the multivariable model, there were no significant differences in the odds of experiencing complications by race. Although this study showed that Hispanic patients were 13 percent less likely to experience complications than white (non‐Hispanic) patients after including patient‐, hospital‐, and community‐level characteristics, other unmeasured or residual confounders may explain this finding. For example, family or social structures that are more prevalent in Hispanic populations (Sabogal et al. 1987) may contribute to fewer complications because of familial support and outlook about recovery. Alternatively, the Hispanic patients may have had a higher prevalence of low‐risk surgical procedures, or they may have been in better health prior to the surgery than the white (non‐Hispanic) patients, which would not be detected with administrative data (Abraido‐Lanza, Chao, and Florez 2005; Ruiz, Steffen, and Smith 2013).
Our findings suggest that other patient‐ and community‐level characteristics attenuate estimates of the relationship between race and postsurgical complications. Several mechanisms may help explain the pathways by which low community‐level SES affects the relationship between race and complications. First, the socioeconomic context of neighborhoods has been shown to be related to patient health status (Malmstrom, Sundquist, and Johansson 1999; Cubbin, Hadden, and Winkleby 2001; Shohaimi et al. 2003), and the community context is independent of the patient's SES (Haan, Kaplan, and Camacho 1987). Second, low community‐level SES may reflect worse quality of care or fewer community‐wide resources to support health. Among the studies of postsurgical complications, most controlled for patient or hospital SES, either as income at the ZIP Code level (Coffey, Andrews, and Moy 2005) or county level (Gaskin et al. 2011) or as an index measure (Brooks et al. 2013). Of note, Carthon et al. (2012) provides an earlier example of community SES attenuating racial disparities in postsurgical mortality (Carthon et al. 2012). Our study further expands upon this research to show that community SES may help explain racial disparities and attenuate ethnic disparities in postsurgical inpatient hospitalizations.
Our final multivariable results showed that several patient‐, hospital‐, and community‐level characteristics were significantly associated with in‐hospital postsurgical complications. First, patient payer type had the strongest independent association with the likelihood of complications. Patients who were uninsured, publicly insured, or covered by insurance other than private insurance were 30 to almost 50 percent more likely to experience a complication following surgery compared with patients covered by private insurance. One explanation for this finding is that insurance status may reflect unmeasured patient clinical severity. We controlled for age, sex, DRG, and comorbidities in a clinical risk adjustment score in the final adjusted model. Nevertheless, it is possible that our findings may be a result of residual confounding such that patients without private insurance may differ with respect to unmeasured clinical variables. For example, we were not able to include information about the functional status or frailty of the patient, quality of ambulatory care prior to admission for an in‐hospital surgery, or skill level of the surgeon that performed the procedure. Administrative data are limited in these dimensions. Identifying the underlying mechanisms that drive the effect of having private insurance on the occurrence of surgical complications is worthy of investigation.
Second, we also demonstrate that several institutional characteristics were associated with the likelihood of developing a complication after an in‐hospital surgery. Patients were less likely to have postsurgical complication if they were treated at private, not‐for‐profit hospitals or hospitals located in small metropolitan or micropolitan areas. In addition, although they were modest effects, our study shows that patients in hospitals with higher nurse‐to‐patient ratios experienced fewer complications. This finding is consistent with other studies of nurse staffing and surgical complications (Kovner and Gergen 1998; Dimick et al. 2001; Pronovost et al. 2001). Increasing surgical nurse staffing in hospitals is a modifiable factor that stands to reduce the incidence of surgical complications.
Third, we demonstrated that postsurgical patient safety outcomes differ based on community income level. Patients residing in the lowest income communities were 12 percent more likely to experience a postoperative complication than patients residing in the highest income communities. People in lower income areas often have less access to needed care and/or availability to high surgical volume and to specialty surgeons, which may help explain such income disparities (Schrag et al. 2002; Chowdhury, Dagash, and Pierro 2007; Kalbasi et al. 2014). Findings from this study suggest that focusing solely on patient‐ and hospital‐level characteristics may not be sufficient to prevent or reduce disparities in postsurgical complications.
This research has important implications for health and health care policy. Health insurance type had the strongest association with the risk for postsurgical complications. As such, health insurers, government programs, health care providers, and patients should ensure that high‐quality inpatient surgical care is equal and fair across all‐payer types. In addition, measured community‐level SES may be a proxy for other factors affecting surgical complications. Low‐community‐level SES is often associated with lower patient health status (Cubbin, Hadden, and Winkleby 2001; Shohaimi et al. 2003) and worse health care quality and outcomes (Bikdeli et al. 2014; Agarwal, Menon, and Jaber 2015). Even though we performed risk‐adjusted analyses on both patient health and surgical quality, our measure of community income may be capturing unmeasured poor health status and health care quality of patients living in low‐income areas. Therefore, if our measure is a proxy for such factors, then improving the health and quality of health care in low‐income communities may help in reducing complications.
Finally, the root causes of surgical complications are likely multifactorial and therefore a population‐based approach may be needed to understand the role of the community characteristics as they relate to hospital patient safety (Wholey et al. 2004; Zhang, Ayanian, and Zaslavsky 2007). Future research should include improved measurement of community‐based factors that would allow for a better examination of the specific mechanisms by which the community context influences patient safety. Public health and/or community‐level clinical care efforts may be needed to improve the health of communities, to ensure that the populations living in these contexts can optimize their health and maximize their benefit from the health care system. We are unaware of any such community‐level efforts in the peer reviewed literature that focus on patient safety.
Our study has several strengths. First, we included all‐payer data from 30 states. This is a notable improvement from previous studies that have focused solely on the occurrence of complications among all‐payer, among the elderly, or exclusively on Medicare‐insured patients (Silber et al. 2009; Metersky et al. 2011; Brooks Carthon et al. 2013). Second, we used the POA indicator of the patients' health conditions at the time of admission to the hospital for surgery. Including this variable improves patient safety measures and may partially explain why our unadjusted estimates of the effect of race and ethnicity are modest compared with previous studies. For example, Coffey, Andrews, and Moy (2005) reported odds ratios of 1.25–1.50 for postoperative sepsis, respiratory failure, and pulmonary embolism or deep vein thrombosis when comparing black (non‐Hispanic) with white (non‐Hispanic) patients. Finally, this study incorporates population‐based or community‐level measures in determining in‐hospital postsurgical complications.
Several potential limitations should be considered when interpreting the results from this study. First, we excluded discharges from hospitals without POA reporting or with limited POA data. These exclusions targeted general patterns of reporting POA and did not address the accuracy of the coding of POA. The quality of POA coding is sometimes inaccurate and could impact our results in an unknown direction. Second, we used a composite measure to indicate whether a patient experienced a complication, and this does create the possibility that the predictors are influencing each of the PSI indicators differently. The eight individual PSIs that comprise the composite represent very different complications, and our results may differ depending on the type of surgery performed. Third, our dependent variable was limited to postsurgical complications occurring in the hospital, and our results may have varied if we could have included complications that occurred after discharge. Fourth, there may have been variation in how hospitals code the complications making up the PSIs that could have led to misclassification and biased our results in an unknown direction. Fifth, the final sample that was used in this study was subject to many exclusion criteria, so our results are not generalizable to the U.S. population. The exclusion of remote rural (non‐CBSA) hospitals may have some effect on the level of racial disparities estimated in our study relative to the literature, and therefore our results may not be generalizable to such hospitals. Moreover, we also excluded discharges that had missing or inadequate POA, race and ethnicity, or hospital quality data. Excluding these discharges from our sample may also limit the generalizability of our results, as those hospitals or states may be different from entities that collect such data. Lastly, our study used administrative data, which lack detailed clinical information such as laboratory results and physiological measures; this may have underadjusted for clinical risk.
Race does not appear to be an important determinant of in‐hospital postsurgical complications, all else being equal. We find relatively small initial effect sizes on the odds of postsurgical complications by patient race and ethnicity. The effect of race and ethnicity was mitigated with the addition of patient and hospital characteristics, and it became statistically insignificant for all but Hispanic patients after the addition of community‐level SES to the model. However, patients without private insurance or those who lived in low‐income communities were more likely to experience a complication. These findings suggest that community‐level socioeconomic characteristics should be considered when examining in‐hospital postsurgical complications. In addition, a population‐based approach—one that includes improving the health status and health care for individuals regardless of SES or type of insurance—may help in reducing or eliminating disparities in these outcomes.
Supporting information
Appendix SA1: Author Matrix.
Data S1. Technical Appendix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors thank Robert L. Houchens, Timothy Kenney, and Minya Sheng for their methodological contributions to this paper and Linda Lee for her editorial comments on the paper. We also acknowledge the following HCUP Partner organizations for contributing data to the HCUP State Inpatient Databases used in this study: Arizona Department of Health Services, Arkansas Department of Health, California Office of Statewide Health Planning and Development, Colorado Hospital Association, Florida Agency for Health Care Administration, Georgia Hospital Association, Hawaii Health Information Corporation, Illinois Department of Public Health, Indiana Hospital Association, Iowa Hospital Association, Kansas Hospital Association, Kentucky Cabinet for Health and Family Services, Maine Health Data Organization, Massachusetts Center for Health Information and Analysis, Michigan Health & Hospital Association, Nevada Department of Health and Human Services, New Jersey Department of Health, New Mexico Department of Health, New York State Department of Health, Oregon Association of Hospitals and Health Systems, Pennsylvania Health Care Cost Containment Council, Rhode Island Department of Health, South Carolina Revenue and Fiscal Affairs Office, South Dakota Association of Healthcare Organizations, Tennessee Hospital Association, Texas Department of State Health Services, Vermont Association of Hospitals and Health Systems, Virginia Health Information, Washington State Department of Health, and Wisconsin Department of Health Services. A full list of HCUP Data Partners can be found at https://www.hcup-us.ahrq.gov/db/hcupdatapartners.jsp. This study was funded by the Agency for Healthcare Research and Quality under contract HHSA‐290‐2013‐00002‐C (Contract PI: Gary Pickens). The views expressed herein are those of the authors and do not necessarily reflect those of the Agency for Healthcare Research and Quality of the U.S. Department of Department of Health and Human Services.
Disclosures: None.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect those of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
References
- Abraido‐Lanza, A. F. , Chao M. T., and Florez K. R.. 2005. “Do Healthy Behaviors Decline with Greater Acculturation? Implications for the Latino Mortality Paradox.” Social Science and Medicine 61 (6): 1243–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal, S. , Menon V., and Jaber W. A.. 2015. “Residential Zip Code Influences Outcomes Following Hospitalization for Acute Pulmonary Embolism in the United States.” Vascular Medicine 20 (5): 439–46. [DOI] [PubMed] [Google Scholar]
- AHRQ . 2012. Patient Safety Indicators: Technical Specifications, AHQR Quality Indicators, Version 4.4 SAS. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- AHRQ . 2014a. 2014 Annual Progress Report to Congress: National Strategy for Quality Improvement in Health Care, pp. 1–27. Rockville, MD: The Agency for Healthcare Research and Quality. [Google Scholar]
- AHRQ . 2014b. National Healthcare Disparities Report, 2013, pp. 1–271. Rockville, MD: The Agency for Healthcare Research and Quality. [Google Scholar]
- Bikdeli, B. , Wayda B., Bao H., Ross J. S., Xu X., Chaudhry S. I., Spertus J. A., Bernheim S. M., Lindenauer P. K., and Krumholz H. M.. 2014. “Place of Residence and Outcomes of Patients with Heart Failure: Analysis from the Telemonitoring to Improve Heart Failure Outcomes Trial.” Circulation: Cardiovascular Quality and Outcomes 7 (5): 749–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks Carthon, J. M. , Jarrin O., Sloane D., and Kutney‐Lee A.. 2013. “Variations in Postoperative Complications According to Race, Ethnicity, and Sex in Older Adults.” Journal of the American Geriatrics Society 61 (9): 1499–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carthon, J. M. , Kutney‐Lee A., Jarrin O., Sloane D., and Aiken L. H.. 2012. “Nurse Staffing and Postsurgical Outcomes in Black Adults.” Journal of the American Geriatrics Society 60 (6): 1078–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury, M. M. , Dagash H., and Pierro A.. 2007. “A Systematic Review of the Impact of Volume of Surgery and Specialization on Patient Outcome.” British Journal of Surgery 94 (2): 145–61. [DOI] [PubMed] [Google Scholar]
- Coffey, R. M. , Andrews R. M., and Moy E.. 2005. “Racial, Ethnic, and Socioeconomic Disparities in Estimates of AHRQ Patient Safety Indicators.” Medical Care 43 (3 Suppl): I48–57. [DOI] [PubMed] [Google Scholar]
- Coffey, R. , Barrett M., Houchens R., Moy E., Andrews R., Moles E., and Coenen N.. 2012. Methods Applying AHRQ Quality Indicators to Healthcare Cost and Utilization Project (HCUP) Data for the Tenth (2012) NHQR and NHDR. HCUP Method Series Report. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Cubbin, C. , Hadden W. C., and Winkleby M. A.. 2001. “Neighborhood Context and Cardiovascular Disease Risk Factors: The Contribution of Material Deprivation.” Ethnicity and Disease 11 (4): 687–700. [PubMed] [Google Scholar]
- Dehal, A. , Abbas A., and Johna S.. 2013. “Racial Disparities in Clinical Presentation, Surgical Treatment and In‐Hospital Outcomes of Women with Breast Cancer: Analysis of Nationwide Inpatient Sample Database.” Breast Cancer Research and Treatment 139 (2): 561–9. [DOI] [PubMed] [Google Scholar]
- Dimick, J. B. , Swoboda S. M., Pronovost P. J., and Lipsett P. A.. 2001. “Effect of Nurse‐to‐Patient Ratio in the Intensive Care Unit on Pulmonary Complications and Resource Use after Hepatectomy.” American Journal of Critical Care 10 (6): 376–82. [PubMed] [Google Scholar]
- Fielding, A. , and Goldstein H.. 2006. Cross‐Classified and Multiple Membership Structures in Multilevel Models: An Introduction and Review. Nottingham, UK: DfES Publications, University of Birmingham. [Google Scholar]
- Fiscella, K. , Franks P., Meldrum S., and Barnett S.. 2005. “Racial Disparity in Surgical Complications in New York State.” Annals of Surgery 242 (2): 151–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin, D. J. , Spencer C. S., Richard P., Anderson G. F., Powe N. R., and Laveist T. A.. 2008. “Do Hospitals Provide Lower‐Quality Care to Minorities Than to Whites?” Health Affairs (Millwood) 27 (2): 518–27. [DOI] [PubMed] [Google Scholar]
- Gaskin, D. J. , Spencer C. S., Richard P., Anderson G., Powe N. R., and LaVeist T. A.. 2011. “Do Minority Patients Use Lower Quality Hospitals?” Inquiry 48 (3): 209–20. [DOI] [PubMed] [Google Scholar]
- Haan, M. , Kaplan G. A., and Camacho T.. 1987. “Poverty and Health. Prospective Evidence from the Alameda County Study.” American Journal of Epidemiology 125 (6): 989–98. [DOI] [PubMed] [Google Scholar]
- Ingram, D. D. , and Franco S. J.. 2012. “NCHS Urban‐Rural Classification Scheme for Counties.” Vital Health Statistics 2 (154): 1–65. [PubMed] [Google Scholar]
- Kalbasi, A. , Swisher‐McClure S., Mitra N., Sunderland R., Smaldone M. C., Uzzo R. G., and Bekelman J. E.. 2014. “Low Rates of Adjuvant Radiation in Patients with Nonmetastatic Prostate Cancer with High‐Risk Pathologic Features.” Cancer 120 (19): 3089–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovner, C. , and Gergen P. J.. 1998. “Nurse Staffing Levels and Adverse Events Following Surgery in U.S. Hospitals.” Image—The Journal of Nursing Scholarship 30 (4): 315–21. [PubMed] [Google Scholar]
- Ly, D. P. , Lopez L., Isaac T., and Jha A. K.. 2010. “How Do Black‐Serving Hospitals Perform on Patient Safety Indicators? Implications for National Public Reporting and Pay‐for‐Performance.” Medical Care 48 (12): 1133–7. [DOI] [PubMed] [Google Scholar]
- Malmstrom, M. , Sundquist J., and Johansson S. E.. 1999. “Neighborhood Environment and Self‐Reported Health Status: A Multilevel Analysis.” American Journal of Public Health 89 (8): 1181–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metersky, M. L. , Hunt D. R., Kliman R., Wang Y., Curry M., Verzier N., Lyder C. H., and Moy E.. 2011. “Racial Disparities in the Frequency of Patient Safety Events: Results from the National Medicare Patient Safety Monitoring System.” Medical Care 49 (5): 504–10. [DOI] [PubMed] [Google Scholar]
- Pronovost, P. J. , Dang D., Dorman T., Lipsett P. A., Garrett E., Jenckes M., and Bass E. B.. 2001. “Intensive Care Unit Nurse Staffing and the Risk for Complications after Abdominal Aortic Surgery.” Eff Clin Pract 4 (5): 199–206. [PubMed] [Google Scholar]
- Ruiz, J. M. , Steffen P., and Smith T. B.. 2013. “Hispanic Mortality Paradox: A Systematic Review and Meta‐Analysis of the Longitudinal Literature.” American Journal of Public Health 103 (3): e52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabogal, F. , Otero‐Sabogal R., Marín B., and Perez‐Stable E. J.. 1987. “Hispanic Familism and Acculturation: What Changes and What Doesn't?” Hispanic Journal of Behavioral Sciences 9 (4): 397–412. [Google Scholar]
- Schrag, D. , Panageas K. S., Riedel E., Cramer L. D., Guillem J. G., Bach P. B., and Begg C. B.. 2002. “Hospital and Surgeon Procedure Volume as Predictors of Outcome Following Rectal Cancer Resection.” Annals of Surgery 236 (5): 583–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shohaimi, S. , Luben R., Wareham N., Day N., Bingham S., Welch A., Oakes S., and Khaw K. T.. 2003. “Residential Area Deprivation Predicts Smoking Habit Independently of Individual Educational Level and Occupational Social Class: A Cross Sectional Study in the Norfolk Cohort of the European Investigation into Cancer (EPIC‐Norfolk).” Journal of Epidemiology and Community Health 57 (4): 270–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silber, J. H. , Rosenbaum P. R., Romano P. S., Rosen A. K., Wang Y., Teng Y., Halenar M. J., Even‐Shoshan O., and Volpp K. G.. 2009. “Hospital Teaching Intensity, Patient Race, and Surgical Outcomes.” Archives of Surgery 144 (2): 113–20; discussion 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley, B. , Stith A., and Nelson A.. 2003. Unequal Treatment Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Spetz, J. , and Baker L.. 1999. Has Managed Care Affected the Availability of Medical Technology?. San Francisco, CA: Public Policy Institute of California. [Google Scholar]
- Wholey, D. , Moscovice I., Hietpas T., and Holtzman J.. 2004. “The Environmental Context of Patient Safety and Medical Errors.” Journal of Rural Health 20 (4): 304–13. [DOI] [PubMed] [Google Scholar]
- Zhang, W. , Ayanian J. Z., and Zaslavsky A. M.. 2007. “Patient Characteristics and Hospital Quality for Colorectal Cancer Surgery.” International Journal for Quality in Health Care 19 (1): 11–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Data S1. Technical Appendix.


