Abstract
BACKGROUND:
Inappropriate use of antimicrobial agents is the major cause for the development of resistance. Thus, it is important to include outpatient clinics in the development of antibiotic stewardship program.
METHODS:
We report a multifaceted approach to decrease inappropriate antibiotic use in upper respiratory tract infections (URTIs) in an outpatient pediatric clinic. The interventions included educational grand round, academic detailing, and prospective audit and feedback and peer comparison.
RESULTS:
During the study period, a total of 3677 outpatient clinic visits for URTIs were evaluated. Of all the included patients, 12% were <1 year of age, 42% were 1–5 years, and 46% were >5 years of age. Of the total patients, 684 (17.6%) received appropriate antibiotics, 2812 (76.4%) appropriately did not receive antibiotics, and 217 (6%) inappropriately received antibiotics. The monthly rate of prescription of inappropriate antibiotics significantly decreased from 12.3% at the beginning of the study to 3.8% at the end of the study (P < 0.0001). Antibiotic prescription among those who had rapid streptococcal antigen test (RSAT) was 40% compared with 78% among those who did not have RSAT (P < 0.0001).
CONCLUSIONS:
The combination of education and academic detailing is important to improve antibiotic use.
Key words: Antibiotic, antimicrobial stewardship, rapid streptococcal antigen, upper respiratory tract infection
Use, misuse, and abuse of antimicrobial agents are the major causes for the development of resistance. Antimicrobial resistance is a major concern due to the limited availability of newer antibiotics.[1] One area for antimicrobial misuse is upper respiratory tract infections (URTIs).[2,3,4,5,6,7,8] There is a global concern of emerging resistance among respiratory pathogens. In Saudi Arabia, Haemophilus influenzae resistance to ampicillin was 13.2%.[9] In addition, Streptococcus pneumoniae showed 59% resistance to penicillin, of which 15% were highly resistant.[10] The resistance rate was higher in children <10 years of age.[10] In a study, S. pneumoniae from pediatric patients showed 28.8% intermediate susceptibility and 13.7% high resistance rates to penicillin.[11]
Different methodologies were used to limit the use of antibiotics in children with URTIs, including delayed antibiotic prescribing, education, and the use of laboratory tests.[12,13,14,15,16] Delayed prescription may result in >50% reduction in antibiotic use.[12] However, adding education to delayed prescribing strategy resulted in a significant reduction in antibiotic use.[17,18,19]
Recently, there had been a call to include outpatients in the development of antibiotic stewardship program.[20] In this study, we report our experience with a multifaceted approach to decrease inappropriate antibiotic usage in an outpatient pediatric clinic targeting patients with URTIs.
Methods
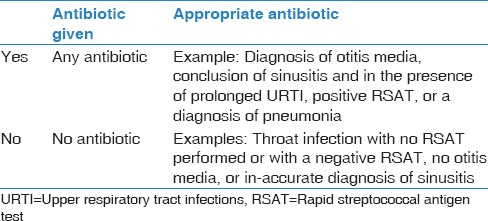
During the study period of December 2012–December 2013, we collected all the charts for pediatric patients <13 years of age who presented to the outpatient clinic at Dhahran health center with a chief complaint of any respiratory symptom (cough, cold, congestion, sore throat, or sneezing). Paper and electronic medical records were reviewed by an experienced physician and used the Centers for Disease Control and Prevention Pediatric Treatment Recommendations of Upper Respiratory Tract infection.[21] The following information were recorded: The date, age, gender, chief complaint, diagnosis, rapid streptococcal antigen test (RSAT), and treatment choice. For treatment choice, we recorded whether antibiotics were given or not, the type of the antibiotic, and whether the treatment choice was appropriate or not [Table 1].
Table 1.
A summary of data collection in relation to antibiotics
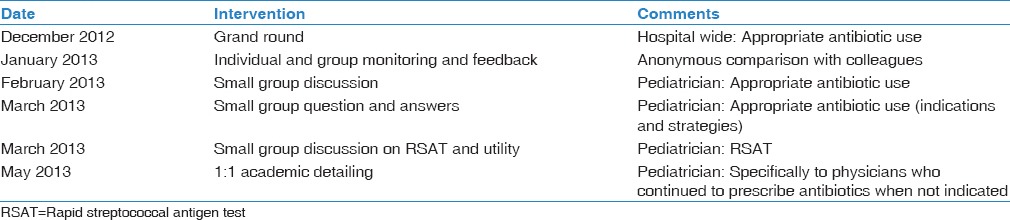
The multifaceted interventions included an initial grand round about judicious antibiotic use, followed by multiple other interventions as summarized in Table 2. Academic detailing is a concept of adult learning and behavior change. This principle relies on probing baseline knowledge of an individual physician, using evidence-based resources highlighting essential messages on appropriate antibiotic use and providing positive feedback.[22]
Table 2.
A summary of multifaceted approach to reduce inappropriate antibiotic use in children with upper respiratory tract infections
The use of RSAT was also introduced to help in the differentiation of streptococcal pharyngitis. RSAT was introduced for testing in children with a streptococcal score of ≥5 as described previously.[23,24]
The study was approved by the Institutional Review Board and informed consent was not required.
Results
During the study period, a total of 3677 outpatient clinic visits for URTI were evaluated. Of all the included patients, 441 (12%) were <1 year of age, 1544 (42%) were 1–5 years, and 1692 (46%) were >5 years of age. Of the total patients, 56% were male. The initial diagnosis of the patients is summarized in Figure 1.
Figure 1.

Initial diagnosis in the included pediatric patients, numbers represent percentage of the total patients. URTI=Upper respiratory tract infections
Of the included patients, 684 (17.6%) received appropriate antibiotic, 2812 (76.4%) appropriately did not receive antibiotic, and 217 (6%) received antibiotic inappropriately. Of those who received antibiotic appropriately, 42 patients (6.5%) had streptococcal pharyngitis. The most frequently prescribed antibiotics were amoxicillin (42%) and azithromycin (25%) [Figure 2]. The monthly inappropriate antibiotic prescription decreased from 12.3% at the beginning of the study to 3.8% at the end of the study (P < 0.0001) [Figure 3].
Figure 2.
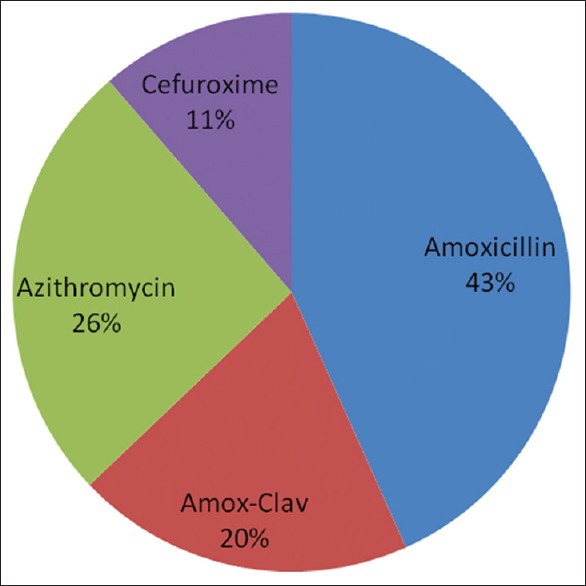
Most frequently prescribed antibiotics (numbers represent percentage of the total prescribed antibiotics)
Figure 3.
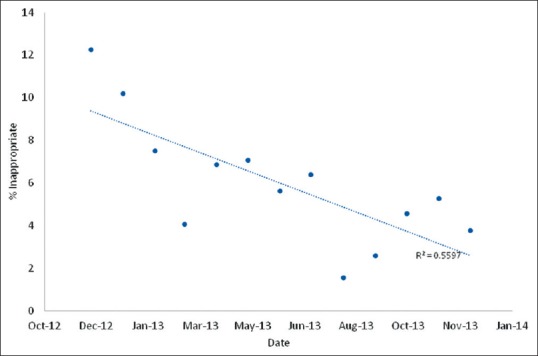
A scattered diagram showing monthly inappropriate antibiotic usage as a percentage
Among 317 patients with a diagnosis of pharyngitis, 162 (51%) patients had RSAT was antibiotic prescription among those who had RSAT was 65 (40%) compared with 121 (78%) among those who did not have RSAT (P < 0.0001).
Discussion
This study showed that a multifaceted approach is useful for the reduction of antibiotic use in pediatric patients with URTIs. Education and academic detailing were important parts of the interventions as well as the use of RSAT.
One important finding of this study is the lower rate of antibiotic prescribing for pediatric patients with URTIs and the achievement of even a lower rate with a multifaceted approach. In Saudi Arabia, antibiotics were prescribed for 87% of URTI patients[25] and account for 43.8% of all prescriptions.[26] In the United States of America, 75% of the antibiotic prescriptions in the outpatient settings are for acute URTIs.[27]
In this study, we utilized multiple interventions to improve antibiotic use focused on physicians. A multifaceted approach was cited as the best intervention to reduce antibiotic usage in patients with URTIs.[28,29,30]
Individual prescriber and small group education play a role in the reduction of inappropriate antibiotic use.[22,31,32,33,34] We specifically included academic detailing in the intervention. Academic detailing is an important component of an individual educational perspective.[22,35,36] In one study, academic detailing showed better compliance in relation to the choice of antibiotics but did not result in reduction in total prescription rates.[37] One method to facilitate academic detailing is the use of clinical vignette.[38,39]
Although Group A beta-hemolytic Streptococcus accounts for 15%-30% of acute pharyngitis in children, this condition is overdiagnosed and overtreated.[40] In the current study, the use of RSAT resulted in 50% reduction in antibiotic use (40% vs. 78%). Similarly in previous studies, RSAT was associated with 22.4% antibiotic prescription for children with pharyngitis compared to 41.4% for those who did not have RSAT.[40,41] RSAT is an easy and sensitive test that is available at the point-of-care testing and could be utilized to decrease inappropriate antibiotic use.[42,43]
Conclusions
The combination of education, academic detailing, and focus education of physicians is an important intervention to improve antibiotic utilization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Livermore DM. Bacterial resistance: Origins, epidemiology, and impact. Clin Infect Dis. 2003;36(Suppl 1):S11–23. doi: 10.1086/344654. [DOI] [PubMed] [Google Scholar]
- 2.Smucny J, Fahey T, Becker L, Glazier R. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2004 Oct 18;4:CD000245. doi: 10.1002/14651858.CD000245.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Kenealy T, Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev. 2013 Jun 4;6:CD000247. doi: 10.1002/14651858.CD000247.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zoorob R, Sidani MA, Fremont RD, Kihlberg C. Antibiotic use in acute upper respiratory tract infections. Am Fam Physician. 2012;86:817–22. [PubMed] [Google Scholar]
- 5.van Dijk L, de Jong JD, Westert GP, de Bakker DH. Variation in formulary adherence in general practice over time (2003-2007) Fam Pract. 2011;28:624–31. doi: 10.1093/fampra/cmr043. [DOI] [PubMed] [Google Scholar]
- 6.Marc C, Vrignaud B, Levieux K, Robine A, Gras-Le Guen C, Launay E. Inappropriate prescription of antibiotics in pediatric practice: Analysis of the prescriptions in primary care. J Child Health Care. 2016:pii: 1367493516643421. doi: 10.1177/1367493516643421. [DOI] [PubMed] [Google Scholar]
- 7.Ivanovska V, Hek K, Mantel Teeuwisse AK, Leufkens HG, Nielen MM, van Dijk L. Antibiotic prescribing for children in primary care and adherence to treatment guidelines. J Antimicrob Chemother. 2016;71:1707–14. doi: 10.1093/jac/dkw030. [DOI] [PubMed] [Google Scholar]
- 8.Thompson PL, Spyridis N, Sharland M, Gilbert RE, Saxena S, Long PF, et al. Changes in clinical indications for community antibiotic prescribing for children in the UK from 1996 to 2006: Will the new NICE prescribing guidance on upper respiratory tract infections just be ignored? Arch Dis Child. 2009;94:337–40. doi: 10.1136/adc.2008.147579. [DOI] [PubMed] [Google Scholar]
- 9.Abdel-Rahman EM, Ismael NA, Dixon RA. Antibiotic resistance and prevalence of beta-lactamase in Haemophilus influenzae isolates-a surveillance study of patients with respiratory infection in Saudi Arabia. Diagn Microbiol Infect Dis. 2000;36:203–8. doi: 10.1016/s0732-8893(99)00142-x. [DOI] [PubMed] [Google Scholar]
- 10.Memish ZA, Balkhy HH, Shibl AM, Barrozo CP, Gray GC. Streptococcus pneumoniae in Saudi Arabia: Antibiotic resistance and serotypes of recent clinical isolates. Int J Antimicrob Agents. 2004;23:32–8. doi: 10.1016/j.ijantimicag.2003.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Al-Tawfiq JA. Antibiotic resistance of pediatric isolates of Streptococcus pneumoniae in a Saudi Arabian hospital from 1999 to 2004. Med Sci Monit. 2006;12:CR471–5. [PubMed] [Google Scholar]
- 12.Andrews T, Thompson M, Buckley DI, Heneghan C, Deyo R, Redmond N, et al. Interventions to influence consulting and antibiotic use for acute respiratory tract infections in children: A systematic review and meta-analysis. PLoS One. 2012;7:e30334. doi: 10.1371/journal.pone.0030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: Cluster randomised trial. BMJ. 2009;338:b1374. doi: 10.1136/bmj.b1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmonth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ. 1997;314:722–7. doi: 10.1136/bmj.314.7082.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arroll B, Kenealy T, Kerse N. Do delayed prescriptions reduce antibiotic use in respiratory tract infections? A systematic review. Br J Gen Pract. 2003;53:871–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Spurling GK, Del Mar CB, Dooley L, Foxlee R, Farley R. Delayed antibiotics for respiratory infections. Cochrane Database Syst Rev. 2013 Apr 30;4:CD004417. doi: 10.1002/14651858.CD004417.pub4. [DOI] [PubMed] [Google Scholar]
- 17.Chao JH, Kunkov S, Reyes LB, Lichten S, Crain EF. Comparison of two approaches to observation therapy for acute otitis media in the emergency department. Pediatrics. 2008;121:e1352–6. doi: 10.1542/peds.2007-2278. [DOI] [PubMed] [Google Scholar]
- 18.Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ. 2001;322:336–42. doi: 10.1136/bmj.322.7282.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spiro DM, Tay KY, Arnold DH, Dziura JD, Baker MD, Shapiro ED. Wait-and-see prescription for the treatment of acute otitis media: A randomized controlled trial. JAMA. 2006;296:1235–41. doi: 10.1001/jama.296.10.1235. [DOI] [PubMed] [Google Scholar]
- 20.Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62:e51–77. doi: 10.1093/cid/ciw118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Get Smart about Antibiotics-Pediatric Treatment Recommendations|CDC. [Last accessed on 2016 Sep 06]. Available from: http://www.cdc.gov/getsmart/community/for-hcp/outpatient-hcp/pediatric-treatment-rec.html.
- 22.Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263:549–56. [PubMed] [Google Scholar]
- 23.Wald ER, Green MD, Schwartz B, Barbadora K. A streptococcal score card revisited. Pediatr Emerg Care. 1998;14:109–11. doi: 10.1097/00006565-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Edmonson MB, Farwell KR. Relationship between the clinical likelihood of group a streptococcal pharyngitis and the sensitivity of a rapid antigen-detection test in a pediatric practice. Pediatrics. 2005;115:280–5. doi: 10.1542/peds.2004-0907. [DOI] [PubMed] [Google Scholar]
- 25.el-Gilany AH. Acute respiratory infections in primary health care centres in Northern Saudi Arabia. East Mediterr Health J. 2000;6:955–60. [PubMed] [Google Scholar]
- 26.Irshaid YM, Al-Homrany MA, Hamdi AA, Adjepon-Yamoah KK, Mahfouz AA. A pharmacoepidemiological study of prescription pattern in outpatient clinics in Southwestern Saudi Arabia. Saudi Med J. 2004;25:1864–70. [PubMed] [Google Scholar]
- 27.McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002;287:3096–102. doi: 10.1001/jama.287.23.3096. [DOI] [PubMed] [Google Scholar]
- 28.Welschen I, Kuyvenhoven MM, Hoes AW, Verheij TJ. Effectiveness of a multiple intervention to reduce antibiotic prescribing for respiratory tract symptoms in primary care: Randomised controlled trial. BMJ. 2004;329:431. doi: 10.1136/bmj.38182.591238.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Butler CC, Simpson SA, Dunstan F, Rollnick S, Cohen D, Gillespie D, et al. Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: Practice based randomised controlled trial. BMJ. 2012;344:d8173. doi: 10.1136/bmj.d8173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2005 Oct 19;4:CD003539. doi: 10.1002/14651858.CD003539.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schaffner W, Ray WA, Federspiel CF, Miller WO. Improving antibiotic prescribing in office practice. A controlled trial of three educational methods. JAMA. 1983;250:1728–32. [PubMed] [Google Scholar]
- 32.Avorn J, Soumerai SB. Improving drug-therapy decisions through educational outreach. A randomized controlled trial of academically based “detailing”. N Engl J Med. 1983;308:1457–63. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- 33.De Santis G, Harvey KJ, Howard D, Mashford ML, Moulds RF. Improving the quality of antibiotic prescription patterns in general practice. The role of educational intervention. Med J Aust. 1994;160:502–5. [PubMed] [Google Scholar]
- 34.Ekedahl A, Andersson SI, Hovelius B, Mölstad S, Liedholm H, Melander A. Drug prescription attitudes and behaviour of general practitioners. Effects of a problem-oriented educational programme. Eur J Clin Pharmacol. 1995;47:381–7. doi: 10.1007/BF00196849. [DOI] [PubMed] [Google Scholar]
- 35.Belongia EA, Schwartz B. Strategies for promoting judicious use of antibiotics by doctors and patients. BMJ. 1998;317:668–71. doi: 10.1136/bmj.317.7159.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gjelstad S, Høye S, Straand J, Brekke M, Dalen I, Lindbæk M. Improving antibiotic prescribing in acute respiratory tract infections: Cluster randomised trial from Norwegian general practice (prescription peer academic detailing (Rx-PAD) study) BMJ. 2013;347:f4403. doi: 10.1136/bmj.f4403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dyrkorn R, Gjelstad S, Espnes KA, Lindbæk M. Peer academic detailing on use of antibiotics in acute respiratory tract infections. A controlled study in an urban Norwegian out-of-hours service. Scand J Prim Health Care. 2016;34:180–5. doi: 10.3109/02813432.2016.1163035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gidengil CA, Linder JA, Beach S, Setodji CM, Hunter G, Mehrotra A. Using clinical vignettes to assess quality of care for acute respiratory infections. Inquiry. 2016;53:pii: 0046958016636531. doi: 10.1177/0046958016636531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Magin PJ, Morgan S, Tapley A, Davis JS, McArthur L, Henderson KM, et al. Reducing general practice trainees' antibiotic prescribing for respiratory tract infections: An evaluation of a combined face-to-face workshop and online educational intervention. Educ Prim Care. 2016;27:98–105. doi: 10.1080/14739879.2015.1106085. [DOI] [PubMed] [Google Scholar]
- 40.Ayanruoh S, Waseem M, Quee F, Humphrey A, Reynolds T. Impact of rapid streptococcal test on antibiotic use in a pediatric emergency department. Pediatr Emerg Care. 2009;25:748–50. doi: 10.1097/PEC.0b013e3181bec88c. [DOI] [PubMed] [Google Scholar]
- 41.Kose E, Sirin Kose S, Akca D, Yildiz K, Elmas C, Baris M, et al. The effect of rapid antigen detection test on antibiotic prescription decision of clinicians and reducing antibiotic costs in children with acute pharyngitis. J Trop Pediatr. 2016;62:308–15. doi: 10.1093/tropej/fmw014. [DOI] [PubMed] [Google Scholar]
- 42.Gazzano V, Berger A, Benito Y, Freydiere AM, Tristan A, Boisset S, et al. Reassessment of the role of rapid antigen detection tests in diagnosis of invasive group A streptococcal infections. J Clin Microbiol. 2016;54:994–9. doi: 10.1128/JCM.02516-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Windfuhr JP, Toepfner N, Steffen G, Waldfahrer F, Berner R. Clinical practice guideline: Tonsillitis I. Diagnostics and nonsurgical management. Eur Arch Otorhinolaryngol. 2016;273:973–87. doi: 10.1007/s00405-015-3872-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


