Abstract
Introduction:
Percutaneous nephrolithotomy (PCNL) has undergone significant changes in recent years in the quest for improving efficacy and reducing morbidity. Newer minimally-invasive modalities of PCNL such as mini-PCNL, ultra-mini PCNL, and micro-PCNL have evolved with advancement in optics and technology. However, with these newer advancements, migration of small fragments produced with laser lithotripsy remains a concern, which may result in incomplete stone clearance. We describe a new technique of PCNL termed “Superperc”, that utilizes suction to remove all the fragments and maintain one-way flow.
Methods:
This was a prospective observational study involving 52 consecutive patients who underwent PCNL with the Superperc technique from April 2014 to June 2015. Surgery was performed using a pediatric ureteroscope used as a nephroscope and a specially designed sheath with a suction attachment. The Superperc uses a 10/12 F tract size, specially designed Superperc sheath (Shah Sheath) with suction mechanism and a pediatric ureteroscope (4.5/6 Fr, Richard Wolf) as nephroscope.
Results:
The mean age of the group was 41.8 years (range 6–84) with 33 males and 19 females. Mean stone size was 19.11 mm (range 10–37 mm) and mean operative time was 40.9 min (range 26–92 min). Twenty-seven renal units had upper calyceal puncture, whereas 12 had middle, 8 lower calyceal and 5 had two punctures. DJ stent was placed in 20 patients, whereas 32 patients were totally tubeless. Only three patients required a nephrostomy tube. The mean hemoglobin drop was 0.32 g with no blood transfusion. Postoperatively, three patients had a mild fever and one had transient hematuria. The stone clearance rate in our study was 96.15% and the mean hospital stay was 31.5 h (range 22–76 h).
Conclusion:
Superperc is a new technique of minimally-invasive PCNL and can be successfully done with minimal modification in armamentarium, with the potential advantage of good stone clearance.
INTRODUCTION
Urolithiasis is a common problem with an increasing incidence worldwide.[1] It leads to significant loss of work hours due to the morbidity and has a huge socioeconomic impact on the population.[2] There are multiple minimally-invasive modalities for treatment of renal stones, namely, shock wave lithotripsy (SWL), flexible ureterorenoscopy (f-URS), and percutaneous nephrolithotomy (PCNL).[3]
The ideal management in renal stones is complete stone clearance in a single sitting, which is not always achieved despite the advancements in optics, technology, and lasers. The tract size has decreased considerably in the newer minimally-invasive modalities of PCNL such as mini-PCNL,[4] ultra-mini PCNL (UMP),[5] and micro-PCNL,[6] but concerns remain about small fragments produced with laser lithotripsy migrating to other parts of the pelvi-calyceal system. Keeping this in mind, we have devised a new technique of PCNL termed “Superperc” utilizing suction to remove all the fragments and maintaining low intrapelvic pressure and keeping one-way flow. This method utilizes a specially designed sheath with suction attachment. Except this sheath, this technique does not require any special equipment and is performed using a pediatric ureteroscope (4.5/6.0 F, Richard Wolf, Germany) as the nephroscope. Here, we describe the technique in detail and assess its feasibility as a new entrant in the present armamentarium for minimally-invasive PCNL.
METHODS
This was a prospective observational study involving 52 consecutive patients who underwent PCNL with the Superperc technique from April 2014 to June 2015. The inclusion criteria were unilateral renal stones in adults (age >18) with no bleeding diathesis. Any patient with a urinary tract infection was treated before the procedure with intravenous antibiotics till urine culture was sterile. Preoperative investigations included blood counts, renal function tests, electrolytes, bleeding parameters, and urine culture. Stone burden was evaluated using a multi-slice helical computed tomography (CT) scan. All patients provided written, informed consent before the procedure. Demography, operative parameters, and outcomes were analyzed in the study. All patients had postoperative plain X-ray before discharge from the hospital, and follow-up ultrasound examination/NCCT at follow-up visit at 1 month.
Surgical technique
Superperc works on the principle of maintaining a one-way flow of fluid and utilizing suction to remove small fragments produced during laser fragmentation. Superperc uses a 10/12 F, specially designed sheath (Shah sheath) with suction mechanism and a pediatric ureteroscope (4.5/6 Fr, Richard Wolf) as nephroscope.
The Shah sheath has three components, the cannula, suction master, and the obturator [Figure 1]. The cannula has an inner diameter of 10 F and outer diameter of 12 F. It is available in different lengths ranging from 8 to 20 cm. Suction master has a large outlet to which suction cannula is attached [Figure 2]. There is a provision to control the suction in the system. The main port has a silicon valve mechanism to make it water and air tight, through which the telescope enters, without changing the negative pressure inside the suction master. A 10 F obturator cum dilator is used to place the sheath assembly after an initial puncture is obtained.
Figure 1.
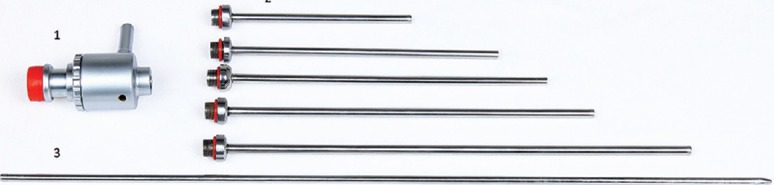
Shah Sheath with different length cannulas
Figure 2.

Shah Sheath with suction attached
The procedure was performed under general anesthesia. Initially, the patient was placed in lithotomy position and a 6 Fr ureteric catheter with multiple side holes in the terminal 10 cm was positioned in the pelvi-calyceal system under cystoscopic and fluoroscopic guidance. The distal end of the ureteric catheter was connected to normal saline solution for a continuous inflow of saline. A 14/16 Fr Foley's catheter was placed for bladder drainage and the patient was turned prone.
The initial puncture was obtained using USG/fluoroscopic guidance by a standard bull's eye technique over the desired calyx and a guidewire was introduced. Tract dilation was done with a single-step screw dilator and the corresponding Shah Sheath was introduced into the desired calyx. The suction master was then attached to the cannula and the telescope was introduced [Figure 3]. The stone was fragmented completely with holmium laser (Lumenis, USA) with a 365 micron end-firing laser fiber at power setting ranging between 12 and 50 W (0.8–1.5 Joules, 15–40 Hz). The fragments were aspirated out through the suction master as the flow in the PCS was from the ureteric catheter towards the sheath, thereby pushing all fragments toward the sheath. Once the stone was cleared, the clearance was confirmed with direct nephroscopy and fluoroscopy. A DJ stent was placed or the ureteric catheter left overnight for drainage. Nephrostomy tube was not routinely placed.
Figure 3.

Whole assembly of Superperc with nephroscope inserted into the Sheath
RESULTS
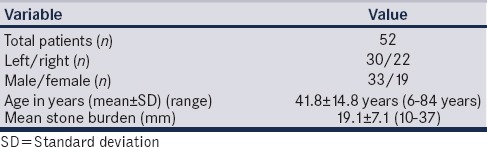
A total of 52 patients underwent Superperc from April 2014 to June 2015, including 33 male (63.4%) and 19 female (36.5%) patients. Mean age was 41.8 ± 14.8 years (range 6–84 years). 30 were left-sided and 22 were right-sided renal units. Thirty-three renal units (63.4%) had single stone, whereas 19 renal units (36.5%) had multiple calculi. The mean stone burden was 19.1 ± 7.1 mm (range 10–37 mm) [Table 1].
Table 1.
Demographic variables
Twenty-seven renal units had upper calyceal puncture, whereas 12 had middle, and 8 lower calyceal punctures. Only five patients required a secondary puncture, whereas two cases required conversion to a larger tract size. All stones were fragmented using laser. Double-J stent was placed in 20 patients (38.4%), whereas in 32 patients (61.5%), only the ureteric catheter was left indwelling overnight. Only 3 patients required nephrostomy tube due to bleeding at the termination of the procedure.
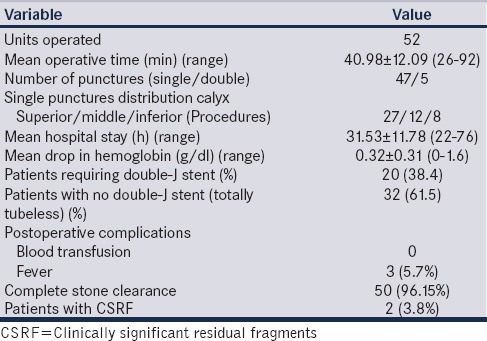
The stone clearance rate in our study was 96.15%. Mean operative time was 40.98 ± 12.09 min (range 26–92 min). Mean hemoglobin (Hb) drop was 0.32 ± 0.31 g/dl (range 0–1.6 g/dl). None of the patients required blood transfusion. Mean hospital stay was 31.53 ± 11.78 h (range 22–76 h) [Table 2]. 3 patients developed fever and one had significant hematuria and all of them were managed conservatively. At minimum follow-up of 6 months, all the patients were doing well without any significant complications.
Table 2.
Operative and postoperative outcomes
DISCUSSION
The best therapeutic approach for 1–2 cm renal stones is still under debate. The European Association of Urology guidelines recommend different treatment strategies for renal calculi in different sizes and locations.[3] While endourological procedures such as PCNL and retrograde intrarenal surgery (RIRS) are accepted as the first-line treatment modality for stones larger than 2 cm in diameter, SWL is preferred for smaller renal stones. The objectives of high stone clearance, minimal invasiveness, short treatment time, and reduced costs are of great interest in determining the treatment strategy, especially in populations with limited resources.
PCNL is a better treatment modality than SWL in terms of stone clearance and is not affected by anatomical factors. Albala et al. compared outcomes of PNL and SWL in lower calyx stones. The stone-free rate was reported to be 90% and 59%, respectively.[7] Similarly in another randomized study by Lingeman et al., comparing SWL and PNL for renal calculi ≤3 cm, success rates of PNL for lower calyx stones were significantly higher than with SWL.[8]
RIRS with the new generation flexible ureterorenoscopes has emerged as a preferred management option for low-volume renal stones in recent years. However, like SWL, the success of f-URS significantly decreases in cases of unfavorable anatomical factors such as a long, lower calyx infundibulum and acute infundibulopelvic angle (<30°).[9] The success of f-URS is reported to be higher than for SWL but lower than for PCNL.[10,11] Regardless of the high stone-free rate, PNL has a statistically higher complication rate than RIRS and SWL for medium sized renal stones (13.19%, 5.26%, and 3.16%, respectively; P < 0.05).[11]
A study comparing UMP with f-URS found no significant differences in operating times (UMP vs. f-URS: 121/102 min), hospital length of stay (2.3/2.0 days), SFR (84/87%), and complications (7/7%). However, the costs for disposable materials and endoscopes were less with UMP than with f-URS.[12]
With the advent of newer technology in optics and lasers, plenty of options in the form of mini PCNL (MIP),[4] UMP[5] and micro PCNL[6] have come up. These have achieved good success rates with lower complication rates as compared to conventional PCNL owing to the size of the tract. Mini-PCNL performed through 20 Fr tract was introduced by Jackman et al.[13] and Helal et al.[14] especially for pediatric cases. In Mini-PCNL the stone fragments are washed out by the turbulence of irrigation fluid, the so-called “eddy-current” effect, and the intra-pelvic pressure is expected to remain low due to open-ended Amplatz sheath. However, Superperc offers the same benefits by assisting removal of stone fragments by suction during and after laser lithotripsy. In this study with Superperc we achieved a stone-free rate of 96.15% and a complication rate of 5.7% only.
The study by Desai and Solanki on UMP[5] on 62 patients achieved a stone-free rate of 86.6% which was comparable to our stone-free rate of 96.1%. The mean Hb drop in UMP study was 1.4 g which was more than 0.3 g reported in our study. The mean hospital stay was comparable in both the studies (1.2 day vs. 31.5 h). Our technique of Superperc is closest to UMP technique in terms of puncture, dilatation, tract size, and fragmentation. However, the mode of stone fragments removal in the form of suction in Superperc is different from the dependence on eddy currents in UMP. We feel the suction technique give a more efficient and complete stone clearance.
The microperc technique developed by Desai et al.[6] utilizes an all-seeing needle for initial puncture and stone fragmentation with laser. The tract size is 4.8 Fr and there is no tract dilatation. The advantages offered are a negligible chance of blood loss. However, limitations include the possibility of rise in intra-pelvic pressure as there is no outflow tract except for ureteric catheter and the likelihood of stone fragments settling down in the PCS. In a study reporting outcomes of microperc for lower calyceal stones of mean size 17.8 mm,[15] the stone-free rate achieved was 85.7%, whereas complications rate was 9.5%. The limitations observed in the study were the inability to remove fragments, the risk of increased intrarenal pressure, low optic resolution, and a fine-needle shaft that hinders excessive torque.
We have termed this new technique “Superperc” as we consider it a superior version of PCNL as it consists of a relatively closed system with an added suction mechanism. The suction mechanism is outside the telescope, thereby allowing use of the working channel continuously for laser fragmentation. The advantage of the multi-hole ureteric catheter with continuous inflow is that there is no reduced flow and no compromise in visibility whenever the working channel is occupied. In a conventional PCNL, the irrigation fluid goes in via the working channel which can get compromised while using a grasper or laser fiber, whereas there is no such limitation in “Superperc.”
The limitations of our study include the relatively small sample size and a single case series without any comparison group. We need to compare Superperc with other minimally invasive techniques such as microperc and UMP on one hand and with flexible ureteroscopy on the other hand in prospective randomized studies to draw proper conclusion regarding the right place of this new technique in the vast armamentarium available now for treatment of small and medium-sized renal stones.
CONCLUSION
Superperc is a new technique of Minimally-Invasive PCNL and can be successfully performed with minimal modification in armamentarium, with the potential advantage of good stone clearance. The initial results are promising, but it requires further comparison in a prospective controlled manner to understand its proper place.
Footnotes
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
REFERENCES
- 1.Romero V, Akpinar H, Assimos DG. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12:e86–96. [PMC free article] [PubMed] [Google Scholar]
- 2.Clark JY, Thompson IM, Optenberg SA. Economic impact of urolithiasis in the United States. J Urol. 1995;154:2020–4. [PubMed] [Google Scholar]
- 3.Türk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Guidelines on Urolithiasis. Uroweb; 2013. [Last cited on 2016 Jan 10; Last accessed on 2016 Jan 10]. Available from: http://www.uroweb.org/gls/pdf/21_Urolithiasis_LR.pdf . [Google Scholar]
- 4.Abdelhafez MF, Bedke J, Amend B, ElGanainy E, Aboulella H, Elakkad M, et al. Minimally invasive percutaneous nephrolitholapaxy (PCNL) as an effective and safe procedure for large renal stones. BJU Int. 2012;110(11 Pt C):E1022–6. doi: 10.1111/j.1464-410X.2012.11191.x. [DOI] [PubMed] [Google Scholar]
- 5.Desai J, Solanki R. Ultra-mini percutaneous nephrolithotomy (UMP): One more armamentarium. BJU Int. 2013;112:1046–9. doi: 10.1111/bju.12193. [DOI] [PubMed] [Google Scholar]
- 6.Desai MR, Sharma R, Mishra S, Sabnis RB, Stief C, Bader M. Single-step percutaneous nephrolithotomy (microperc): The initial clinical report. J Urol. 2011;186:140–5. doi: 10.1016/j.juro.2011.03.029. [DOI] [PubMed] [Google Scholar]
- 7.Albala DM, Assimos DG, Clayman RV, Denstedt JD, Grasso M, Gutierrez-Aceves J, et al. Lower pole I: A prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol. 2001;166:2072–80. doi: 10.1016/s0022-5347(05)65508-5. [DOI] [PubMed] [Google Scholar]
- 8.Lingeman JE, Siegel YI, Steele B, Nyhuis AW, Woods JR. Management of lower pole nephrolithiasis: A critical analysis. J Urol. 1994;151:663–7. doi: 10.1016/s0022-5347(17)35042-5. [DOI] [PubMed] [Google Scholar]
- 9.Elbahnasy AM, Shalhav AL, Hoenig DM, Elashry OM, Smith DS, McDougall EM, et al. Lower caliceal stone clearance after shock wave lithotripsy or ureteroscopy: The impact of lower pole radiographic anatomy. J Urol. 1998;159:676–82. [PubMed] [Google Scholar]
- 10.Pearle MS, Lingeman JE, Leveillee R, Kuo R, Preminger GM, Nadler RB, et al. Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol. 2005;173:2005–9. doi: 10.1097/01.ju.0000158458.51706.56. [DOI] [PubMed] [Google Scholar]
- 11.Ozturk U, Sener NC, Goktug HN, Nalbant I, Gucuk A, Imamoglu MA. Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10-20 mm. Urol Int. 2013;91:345–9. doi: 10.1159/000351136. [DOI] [PubMed] [Google Scholar]
- 12.Schoenthaler M, Wilhelm K, Hein S, Adams F, Schlager D, Wetterauer U, et al. Ultra-mini PCNL versus flexible ureteroscopy: A matched analysis of treatment costs (endoscopes and disposables) in patients with renal stones 10-20 mm. World J Urol. 2015;33:1601–5. doi: 10.1007/s00345-015-1489-4. [DOI] [PubMed] [Google Scholar]
- 13.Jackman SV, Hedican SP, Peters CA, Docimo SG. Percutaneous nephrolithotomy in infants and preschool age children: Experience with a new technique. Urology. 1998;52:697–701. doi: 10.1016/s0090-4295(98)00315-x. [DOI] [PubMed] [Google Scholar]
- 14.Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: Alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997;11:171–2. doi: 10.1089/end.1997.11.171. [DOI] [PubMed] [Google Scholar]
- 15.Tepeler A, Armagan A, Sancaktutar AA, Silay MS, Penbegul N, Akman T, et al. The role of microperc in the treatment of symptomatic lower pole renal calculi. J Endourol. 2013;27:13–8. doi: 10.1089/end.2012.0422. [DOI] [PubMed] [Google Scholar]


