Abstract
Tyrosine kinase inhibitors sunitinib and pazopanib are used as first-line agents in the treatment of metastatic renal cell carcinoma. Treatment-related toxicities have been described with both these drugs. This report describes a patient with metastatic renal carcinoma who developed trismus while being treated with these agents and is, to the best of our knowledge, the first such case to be reported.
INTRODUCTION
The small molecule tyrosine kinase inhibitors (TKIs) sunitinib and pazopanib are used as first-line agents in the treatment of metastatic renal cell carcinoma. Despite proven efficacy, their use can be limited by treatment-related toxicities. We report a patient with metastatic renal carcinoma who developed trismus while being treated with these agents and is, to the best of our knowledge, the first such case to be reported.
CASE REPORT
A 77-year-old male underwent radical nephrectomy for a 7 cm T2 Fuhrman grade two left-sided clear cell renal carcinoma. Eleven years postresection, a surveillance X-ray computed tomography (CT) scan revealed two pancreatic lesions, consistent with disease relapse. On the appearance of malignant lymphadenopathy on further imaging, the patient commenced treatment with oral sunitinib. A dose reduction was required at cycle three due to mucositis, but otherwise the treatment was generally well tolerated with minimal toxicity. Serial CT scans showed evidence of objective disease response and subsequent disease stabilization [Figure 1].
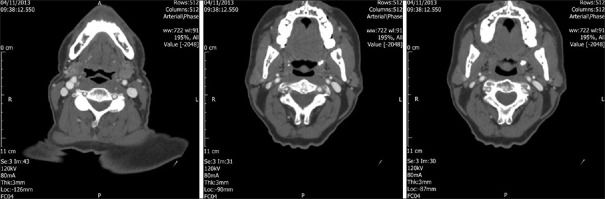
Figure 1.
CT scan to confirm no evidence of cerebral metastasis and no skull metastasis. Also confirms no evidence of soft tissue metastasis, no bone metastasis and no metastasis within the mandible. Within the inferior pole of the right lobe of the thyroid gland there is a well defined 12 mm nodule which is likely to be benign but needs further characterisation
Five years after commencing sunitinib, the patient developed stiffness of the jaw and difficulty opening his mouth, which worsened over the subsequent 2 weeks. Eventually, his symptoms were so severe that he was only able to open his mouth wide enough to use a straw for drinking. Speech and swallowing were unaffected, and there was no evidence of mucositis in the oral cavity. No other neuromuscular symptoms, muscle stiffness spasm were present. The patient had no history of jaw or dental problems and was not taking any other regular medication. Head and neck imaging was unremarkable with no evidence of metastatic disease or other pathology. The patient initially continued with sunitinib treatment, but when he commenced his scheduled 2-week treatment break, his symptoms spontaneously resolved. On commencing the next cycle 2 weeks later, the same symptoms recurred, and once again resolved spontaneously on stopping treatment. A further staging CT scan revealed only a new adrenal metastasis, which was resected. Several months later, on further disease progression, pazopanib was commenced. Within a week, the trismus symptoms recurred, and once again resolved with cessation of the drug. No other TKIs were used in the further management of this patient's disease, and the trismus did not occur again.
DISCUSSION
Sunitinib and pazopanib act by antagonizing several growth factor receptors commonly found on the endothelial cells of tumor vasculature, including vascular endothelial growth factor receptor (VEGFR) and platelet-derived growth factor receptor. Their mechanism of action is competitive inhibition at the ATP-binding domain, preventing phosphorylation at key tyrosine residues and thus blocking receptor activation.[1] The effect, largely mediated through VEGFR2, is inhibition of angiogenesis, one of the core processes required for cancer cell survival and proliferation. Although when initially developed, toxicity secondary to these agents was predicted to be low or nonexistent, as 99% of endothelial cells in an adult remain quiescent at any 1 time and only proliferate during wound healing or the menstrual cycle,[1] a well-defined toxicity profile now exists for this group of drugs. This includes gastrointestinal toxicity, mucocutaneous effects including hand-foot syndrome and mucositis, hematological abnormalities (anemia, leucopenia, and thrombocytopenia), hepatic enzyme elevation, and hypertension. Contrary to previous assumptions, it is now clear that VEGFR is not unique to the proliferating endothelial cell, and is present on many other cell types throughout the body. Its involvement has been described in several hematological processes including coagulation and hematopoeiesis, and in organs including the thyroid gland, kidney, and bone.[1] Most of the treatment toxicities noted therefore appear to be “on target” effects, secondary to the presence of VEGFR at these sites. The precise mechanism of mucocutaneous toxicity is not completely understood but is likely a combination of impaired wound healing, microhemorrhage and impaired endothelial cell proliferation, secondary to the presence of VEGFR on the endothelial cells of dermal capillaries.[1]
Trismus or “lockjaw” can be defined as progressive tonic contraction of the muscles of mastication that results in decreased mouth opening. Common causes include trauma, infections, disorders of the temporomandibular joint such as arthritis, submucosal fibrosis, dental treatment, and in the oncology patient, direct invasion of the temporomandibular joint or muscles of mastication by tumors and head and neck radiotherapy. In addition, several drugs have been associated with the condition, including tricyclic antidepressants, phenothiazines, and succinylcholine. There have been no previous reports of trismus secondary to antiangiogenic TKIs. Other antiangiogenic agents, including the monoclonal antibody bevacizumab which also targets VEGFR, are similarly not commonly associated with trismus. There has been only one study which described seven patients on bevacizumab who developed tetany-like symptoms, one of whom presented with jaw stiffness.[2] However, both sunitinib and bevacizumab are associated with osteonecrosis of the jaw in patients with renal cell carcinoma, both in conjunction with but also independent of simultaneous bisphosphonate therapy.[3] This indicates that these agents can penetrate bone tissue and that the mandible appears to be particularly susceptible to their effects, as osteonecrosis in other bony sites secondary to TKI use is rare. The mechanism suggested is reduced vascularity, leading to ischemia-induced osteonecrosis.[4] In addition, VEGF has other roles within the bone in addition to affecting vascularity, including osteoblast differentiation and enhancement of osteoclast-mediated bone resorption[5] and therefore it is conceivable that the trismus experienced by this patient was a result of VEGF blockade with the body of the mandible or within the temporomandibular joint.
Our patient developed trismus as a complication of sunitinib therapy 5 years after commencing treatment for metastatic renal cell carcinoma. This unusual symptom was related to drug exposure and also recurred when changing sunitinib to another TKI pazopanib. The trismus resolved completely upon pazopanib cessation and did not recur. This is the first report of trismus as a direct toxicity of any TKI agent for any indication.
Footnotes
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
REFERENCES
- 1.Verheul HM, Pinedo HM. Possible molecular mechanisms involved in the toxicity of angiogenesis inhibition. Nat Rev Cancer. 2007;7:475–85. doi: 10.1038/nrc2152. [DOI] [PubMed] [Google Scholar]
- 2.Anwikar SR, Bandekar MS, Patel TK, Patel PB, Kshirsagar NA. Tetany: Possible adverse effect of bevacizumab. Indian J Cancer. 2011;48:31–3. doi: 10.4103/0019-509X.75819. [DOI] [PubMed] [Google Scholar]
- 3.Fleissig Y, Regev E, Lehman H. Sunitinib related osteonecrosis of jaw: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:e1–3. doi: 10.1016/j.tripleo.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Gotink KJ, Verheul HM. Anti-angiogenic tyrosine kinase inhibitors: What is their mechanism of action? Angiogenesis. 2010;13:1–14. doi: 10.1007/s10456-009-9160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chim SM, Tickner J, Chow ST, Kuek V, Guo B, Zhang G, et al. Angiogenic factors in bone local environment. Cytokine Growth Factor Rev. 2013;24:297–310. doi: 10.1016/j.cytogfr.2013.03.008. [DOI] [PubMed] [Google Scholar]