Abstract
Insertional and non-insertional Achilles tendinopathy is usually treated conservatively. Surgery is indicated if conservative treatment fails to relieve the pain. Endoscopic surgery has the advantages of less morbidity, a shorter operating time, reduced postoperative pain, and a lower rate of wound and soft-tissue healing problems. Patients will have a short recovery time and quickly resume work and sports because of less soft-tissue disruption. Moreover, the pathology can be better differentiated and precisely treated. Achilles tendoscopy is classically performed with the patient in the prone position, whereas endoscopic calcaneoplasty can be performed with the patient in the prone or supine position. This technical note describes the technique of Achilles tendoscopy and endoscopic calcaneoplasty with the patient in the supine position. This has the advantages of more ergonomic hand motion for the Achilles tendon debridement, easier access to the ventral surface of the Achilles tendon, and better orientation of the inside structures; moreover, concomitant chondral lesions of the ankle can be dealt with arthroscopically.
Achilles tendinopathy is caused by repeated microtrauma to the Achilles tendon together with a failed healing response of the tendon. The main symptom is pain at the tendon, and it most commonly occurs at the midportion of the tendon.1, 2 The source of pain in tendinopathy could be related to the neurovascular ingrowth associated with the neovascularization that is seen in the tendon's response to injury.1 Conservative treatment is the mainstay of management of Achilles tendinopathy.1 However, conservative management is unsuccessful and surgery has to be considered in 24% to 45.5% of patients with Achilles tendinopathy.2 The objective of open surgery is to excise fibrotic adhesions, remove degenerate nodules, and make longitudinal incisions in the tendon so as to detect and remove intratendinous lesions and restore vascularity.1, 2 It requires extensive incisions and soft-tissue dissection and prolonged postoperative rehabilitation.1 The technique of Achilles tendoscopy was published by van Dijk et al.3 in 1997. It is a safe minimally invasive technique that yields excellent results for tendinopathy and paratendinopathy of the Achilles tendon.4 The fibrous adhesions and neovasculature of the Achilles tendon are resected endoscopically.3, 5, 6, 7, 8, 9, 10 The technique is usually performed with the patient in the prone position.3, 5, 6, 7, 8, 9, 10 Limitations of the procedure are extensive intratendinous pathologies and alterations of tendon insertion sites.11
Haglund syndrome is a triad of posterosuperior calcaneal prominence (Haglund deformity), retrocalcaneal bursitis, and insertional Achilles tendinopathy.12 This is a common cause of pain in the posterosuperior portion of the calcaneus.13 Surgery is indicated if conservative treatment fails to relieve the pain. The inflamed bursa and posterosuperior surface of the calcaneus are removed until there is no impingement on the Achilles tendon with ankle dorsiflexion. Endoscopic calcaneoplasty appears to be a safe and effective surgical procedure for the treatment of Haglund syndrome.14 The endoscopic exposure has the advantages of less morbidity, a shorter operating time, reduced postoperative pain, and a lower rate of wound and soft-tissue healing problems. Patients will have a short recovery time and quickly resume work and sports because of less soft-tissue disruption.12, 15, 16 Moreover, the pathology can be better differentiated.17 Endoscopy can facilitate more precise local decompression and avoid bone over-resection. This can reduce the risk of injury to the Achilles tendon insertion or iatrogenic calcaneal fracture.4 The technique can be performed with the patient in the prone or supine position.12, 13, 14, 15, 16, 17, 18, 19
In this technical note, we report the technique of Achilles tendoscopy and endoscopic calcaneoplasty with the patient in the supine position. This is indicated for non-insertional Achilles tendinopathy or paratendinopathy and/or Haglund syndrome. It is especially suitable if there is a concomitant chondral lesion of the ankle joint that requires anterior ankle arthroscopy. The technique is contraindicated if there is extensive bone formation within the distal Achilles tendon insertion that requires open resection.16 Painful insertional Achilles tendinopathy requiring endoscopic detachment of the tendon insertion for debridement is a relative contraindication. In this case, endoscopic calcaneoplasty in the prone position makes subsequent reattachment of the tendon to the calcaneus easier.20 This approach is also contraindicated in extensive non-insertional Achilles tendinopathy in which augmentation by endoscopic flexor hallux longus transfer is needed.21 It is also better performed with the patient in the prone position if there are concomitant pathologies that require zone 2 flexor hallucis longus tendoscopy22, 23, 24 or endoscopic adhesiolysis of the flexor hallucis longus muscle25 (Table 1).
Table 1.
Pearls and Pitfalls of Endoscopic Calcaneoplasty and Achilles Tendoscopy With Patient in Supine Position
| Pearls |
| The operated leg is lifted up from the operation table by a towel roll or triangular supporting frame under the calf during Achilles tendoscopy. |
| The triangular supporting frame is put under the knee during endoscopic calcaneoplasty. |
| The ankle is allowed to undergo plantar flexion by gravity. |
| Pitfalls |
| The technique is contraindicated if there is extensive bone formation within the distal Achilles tendon insertion that requires open resection. |
| Painful insertional Achilles tendinopathy requiring endoscopic detachment of the tendon insertion for debridement is a relative contraindication. |
| The technique is contraindicated in extensive non-insertional Achilles tendinopathy in which augmentation by endoscopic flexor hallux longus transfer is needed. |
| The technique is contraindicated if there are concomitant pathologies that require zone 2 flexor hallucis longus tendoscopy or endoscopic adhesiolysis of the flexor hallucis longus muscle. |
Technique
Preoperative Assessment and Patient Positioning
Preoperative clinical examination of the ankle, hindfoot, and Achilles tendon is important to delineate the extent of the clinical problem. Radiographs and magnetic resonance imaging can be useful to confirm the diagnosis and assess the extent of tendinopathy, although clinical outcomes are independent of changes on imaging.1
The patient is put in the supine position with the legs spread. A thigh tourniquet is applied to provide a bloodless operative field. The operated leg is lifted up from the operation table by a towel roll or triangular supporting frame (Innomed, Savannah, GA) under the calf. The ankle is allowed to undergo plantar flexion by gravity. The fluid inflow is by gravity, and no arthro-pump is used. A 4.0-mm 30° arthroscope (Dyonics; Smith & Nephew, Andover, MA) is used for this procedure. The arthroscopic video system (Dyonics; Smith & Nephew) is at the head side of the patient.
Portal Placement
Posteromedial and posterolateral portals at the medial and lateral sides of the Achilles tendon are used for this procedure. The portals are at the level of the posterosuperior corner of the posterior calcaneal tubercle (Fig 1).19 A 5-mm incision is made at the posteromedial portal. The subcutaneous tissue is bluntly dissected with a hemostat, and the investing fascia is perforated by the tip of the hemostat. The hemostat should point toward the posterolateral portal and deep to the Achilles tendon. Similarly, a 5-mm incision is made at the posterolateral portal, the subcutaneous tissue is bluntly dissected with a hemostat, and the investing fascia is perforated by the tip of the hemostat. The hemostat should point toward the posteromedial portal and deep to the Achilles tendon. The portals are interchangeable as the viewing and working portals. During debridement of the lateral half of the Achilles tendon and posterior calcaneal tubercle, the posterolateral portal is the working portal and the posteromedial portal is the viewing portal. During debridement of the medial half of the Achilles tendon and posterior calcaneal tubercle, the posteromedial portal is the working portal and the posterolateral portal is the viewing portal.
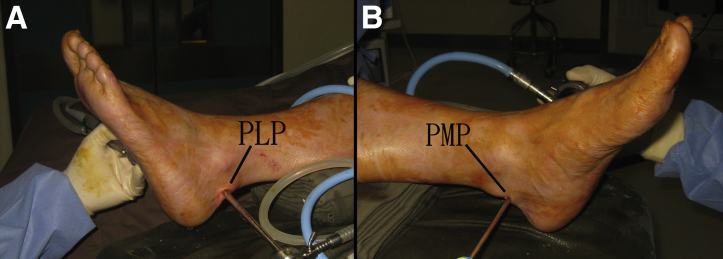
Fig 1.
Endoscopic calcaneoplasty and Achilles tendoscopy of the left leg. (A) The posterolateral portal (PLP) is located at the lateral side of the Achilles tendon. (B) The posteromedial portal (PMP) is located at the medial side of the Achilles tendon. The portals are at the level of the posterosuperior corner of the posterior calcaneal tubercle.
Achilles Tendoscopy
The arthroscope is inserted to the level of the ventral surface of the Achilles tendon through the posterolateral portal, and an arthroscopic shaver (Dyonics; Smith & Nephew) is inserted through the posteromedial portal. The posteromedial and posterolateral portals are coaxial portals, and the arthroscope and the shaver can meet at the level of the portals. Arthroscopic debridement starts at the level and progresses proximally. The medial half of the ventral surface of the tendon is debrided for any fibrous adhesions and neo-vasculature (Fig 2). The debridement should extend proximally until normal tendinous tissue is seen. After completion of debridement of the medial half of the tendon, the arthroscope is switched to the posteromedial portal. The lateral half of the ventral surface of the Achilles tendon is debrided by the arthroscopic shaver through the posterolateral portal. The whole ventral surface of the Achilles tendon should be examined again through the 2 portals for any residual fibrous adhesions.
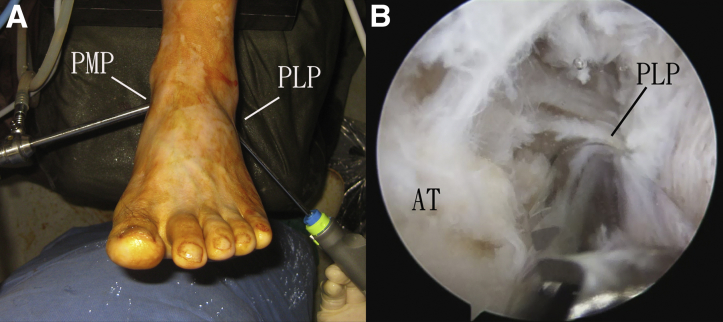
Fig 2.
Achilles tendoscopy of the left leg. (A) Achilles tendoscopy is performed with the posteromedial portal (PMP) and posterolateral portal (PLP). (B) The posteromedial portal is the viewing portal. The ventral surface of the Achilles tendon (AT) is debrided by an arthroscopic shaver through the PLP.
Endoscopic Calcaneoplasty
The posteromedial portal is the viewing portal. The inflamed retrocalcaneal bursa is resected. The lateral half of the posterosuperior corner of the posterior calcaneal tubercle is resected by an arthroscopic acromionizer (Dyonics; Smith & Nephew) through the posterolateral portal. The portals can be switched to allow resection of the medial half of the posterosuperior corner of the posterior calcaneal tubercle. The plantar-flexed position of the ankle will relax the Achilles tendon and open up the angle between the tendon and the posterior calcaneal tubercle. This allows the calcaneal insertion of the Achilles tendon to be easily reached by the acromionizer (Fig 3). The bone resection can be started at this point, moving anteriorly and proximally toward the dorsum of the posterior calcaneal tubercle. This can ensure adequate decompression of the Achilles tendon without the risk of iatrogenic injury to the tendon and its insertion (Fig 4, Video 1). The triangular frame can be put under the knee instead of the calf. This will flex the knee and hip, put the foot onto the operation table, and keep the ankle in a position of plantar flexion. This can stabilize the foot during the bone resection. The hand motion may be more ergonomic if the leg is positioned in this way. The whole posterosuperior corner of the posterior calcaneal tubercle should be examined again through the 2 portals to confirm complete resection down to the Achilles insertion, including the medial and lateral edges of the posterosuperior calcaneal tubercle.
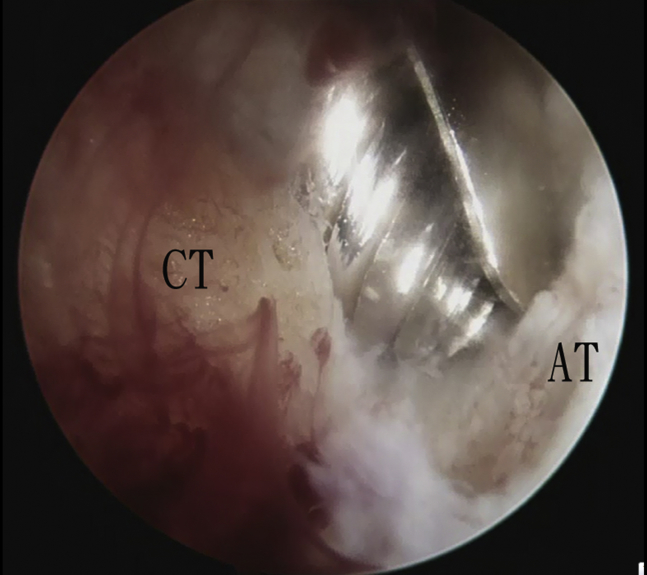
Fig 3.
Endoscopic calcaneoplasty of the left leg. The posterolateral portal is the viewing portal. The plantar-flexed position of the ankle will relax the Achilles tendon (AT) and open up the angle between the tendon and the posterior calcaneal tubercle (CT). This allows the calcaneal insertion of the Achilles tendon to be easily reached by the acromionizer.
Fig 4.
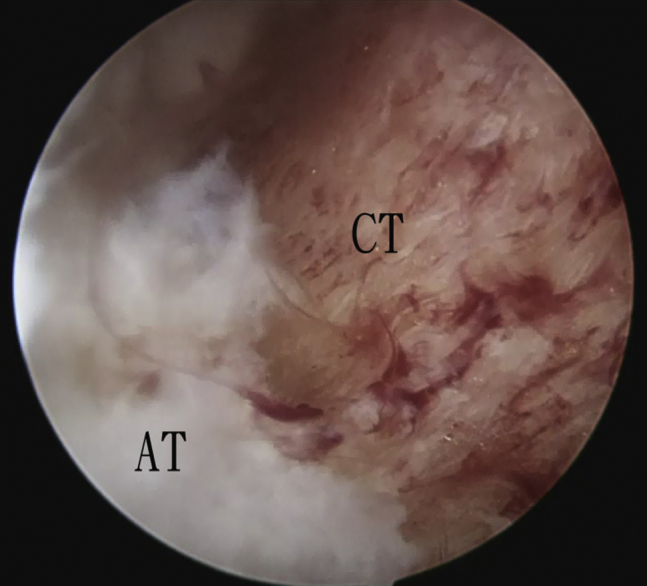
Endoscopic calcaneoplasty of the left leg. The posteromedial portal is the viewing portal. Adequate decompression of the Achilles tendon (AT) down to its insertion is shown. (CT, posterior calcaneal tubercle.)
Discussion
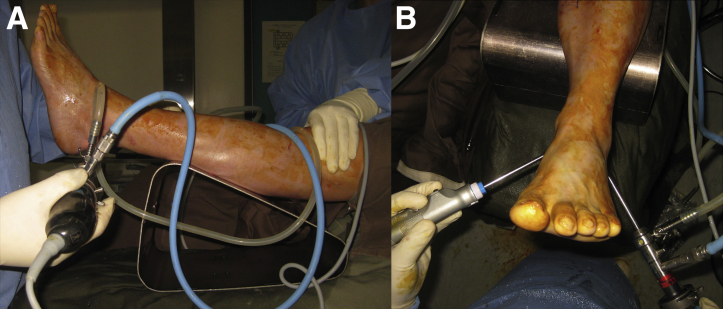
Achilles tendoscopy with the patient in the supine position allows a more logical view on the monitor and more ergonomic hand motion for the Achilles tendon debridement, especially with the hip flexed, knee extended, and leg elevated by the triangular frame (Fig 5). Plantar flexion of the ankle by gravity will relax the triceps surae and Achilles tendon. This can allow easier access to the ventral surface of the Achilles tendon. Moreover, the angle between the Achilles tendon and the posterior calcaneal tubercle will be opened up. This facilitates bone resection and debridement of the Achilles tendon down to its insertion. However, the hand position will be less ergonomic when performing endoscopic calcaneoplasty in this position than in the prone position.12 This can be solved by putting the triangular frame under the knee to flex the knee and hip. The foot will be placed on the operation table with the ankle positioned in plantar flexion. This positioning allows easier handling of the instruments because the foot is stabilized on the table. Moreover, it provides a better orientation of the inside structures for surgical beginners because the leg is closer to its anatomic position.7, 16, 18
Fig 5.
Achilles tendoscopy of the left leg. (A, B) Achilles tendoscopy with the hip flexed, knee extended, and leg elevated by the triangular frame allows a more ergonomic hand motion for the Achilles tendon debridement.
Anterior and posterior ankle arthroscopies can be performed in the supine position to treat associated anterior and posterior ankle impingement or chondral lesions of the ankle.26, 27 Endoscopic gastrocnemius recession can also be performed in the supine position to reduce tension of the Achilles tendon.28, 29
The advantages of the described minimally invasive technique compared with an endoscopic approach with the patient in the prone position are more ergonomic hand motion for the Achilles tendon debridement, easier access to the ventral surface of the Achilles tendon, and better orientation of the inside structures; moreover, concomitant chondral lesions of the ankle can be dealt with arthroscopically. The potential risks of this procedure include injury to the sural nerve, calcaneal branch of the tibial nerve, and Achilles tendon insertion (Table 2).
Table 2.
Advantages and Risks of Endoscopic Calcaneoplasty and Achilles Tendoscopy With Patient in Supine Position
| Advantages |
| More ergonomic hand motion for Achilles tendon debridement |
| Easier access to ventral surface of Achilles tendon |
| Better orientation of inside structures |
| Concomitant chondral lesions of ankle can be dealt with arthroscopically |
| Risks |
| Injury to sural nerve |
| Injury to calcaneal branch of tibial nerve |
| Injury to Achilles tendon insertion |
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Endoscopic calcaneoplasty and Achilles tendoscopy of the left leg. The posteromedial and posterolateral portals are interchangeable as the viewing and working portals. Achilles tendoscopy is performed with debridement of the ventral surface of the Achilles tendon. Endoscopic calcaneoplasty is performed with an arthroscopic acromionizer. The posterosuperior surface of the calcaneus is resected down to the calcaneal insertion of the Achilles tendon. After completion of the resection, there should not be any impingement on the Achilles tendon during ankle dorsiflexion.
References
- 1.Alfredson H., Cook J. A treatment algorithm for managing Achilles tendinopathy: New treatment options. Br J Sports Med. 2007;41:211–216. doi: 10.1136/bjsm.2007.035543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maffulli N., Sharma P., Luscombe K.L. Achilles tendinopathy: Aetiology and management. J R Soc Med. 2004;97:472–476. doi: 10.1258/jrsm.97.10.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Dijk C.N., Scholten P.E., Kort N.P. Tendoscopy (tendon sheath endoscopy) for overuse tendon injuries. Oper Tech Sports Med. 1997;5:170–178. [Google Scholar]
- 4.Roth K.E., Mueller R., Schwand E. Open versus endoscopic bone resection of the dorsolateral calcaneal edge: A cadaveric analysis comparing three dimensional CT scans. J Foot Ankle Res. 2014;7:56. doi: 10.1186/s13047-014-0056-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steenstra F., van Dijk C.N. Achilles tendoscopy. Foot Ankle Clin. 2006;11:429–438. doi: 10.1016/j.fcl.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Phisitkul P. Endoscopic surgery of the Achilles tendon. Curr Rev Musculoskelet Med. 2012;5:156–163. doi: 10.1007/s12178-012-9115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carreira D., Ballard A. Achilles tendoscopy. Foot Ankle Clin. 2015;20:27–40. doi: 10.1016/j.fcl.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H. Endoscopic Achilles tenolysis for management of heel cord pain after repair of acute rupture of Achilles tendon. J Foot Ankle Surg. 2013;52:125–127. doi: 10.1053/j.jfas.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Lui T.H. A case of heel cord pain after repair of acute Achilles tendon rupture: Treated by endoscopic adhesiolysis of the Achilles tendon. Foot Ankle Spec. 2016;9:448–451. doi: 10.1177/1938640015620636. [DOI] [PubMed] [Google Scholar]
- 10.Lui T.H. Endoscopic management of heel cord pain after repair of acute Achilles tendon rupture. J Third Mil Med Univ. 2015;37:187–192. [Google Scholar]
- 11.Kriegelstein S., Altenberger S., Roser A., Walther M. Tendoscopy of the Achilles tendon: Indications, technique and results. Unfallchirurg. 2016;119:120–124. doi: 10.1007/s00113-015-0141-5. [in German] [DOI] [PubMed] [Google Scholar]
- 12.Labib S.A., Pendleton A.M. Endoscopic calcaneoplasty: An improved technique. J Surg Orthop Adv. 2012;21:176–180. doi: 10.3113/jsoa.2012.0176. [DOI] [PubMed] [Google Scholar]
- 13.Jerosch J., Nasef N.M. Endoscopic calcaneoplasty—Rationale, surgical technique, and early results: A preliminary report. Knee Surg Sports Traumatol Arthrosc. 2003;11:190–195. doi: 10.1007/s00167-003-0365-8. [DOI] [PubMed] [Google Scholar]
- 14.Kaynak G., Ogut T., Yontar N.S., Botanlioglu H., Can A., Unlu M.C. Endoscopic calcaneoplasty: 5-Year results. Acta Orthop Traumatol Turc. 2013;47:261–265. doi: 10.3944/aott.2013.3003. [DOI] [PubMed] [Google Scholar]
- 15.van Dijk C.N., van Dyk G.E., Scholten P.E., Kort N.P. Endoscopic calcaneoplasty. Am J Sports Med. 2001;29:185–189. doi: 10.1177/03635465010290021101. [DOI] [PubMed] [Google Scholar]
- 16.Jerosch J., Schunck J., Sokkar S.H. Endoscopic calcaneoplasty (ECP) as a surgical treatment of Haglund's syndrome. Knee Surg Sports Traumatol Arthrosc. 2007;15:927–934. doi: 10.1007/s00167-006-0279-3. [DOI] [PubMed] [Google Scholar]
- 17.Jerosch J., Sokkar S., Ducker M., Donner A. Endoscopic calcaneoplasty (ECP) in Haglund's syndrome. Indication, surgical technique, surgical findings and results. Z Orthop Unfall. 2012;150:250–256. doi: 10.1055/s-0031-1280344. [in German] [DOI] [PubMed] [Google Scholar]
- 18.van Dijk C.N., van Dyk C.E., Scholten P.E., Kort N.P. Endoscopic calcaneoplasty. Foot Ankle Clin. 2006;10:439–446. doi: 10.1016/j.fcl.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 19.van Sterkenburg M.N., Groot M., Sierevelt I.N., Spennacchio P.A., Kerkhoffs G.M., van Dijk C.N. Optimization of portal placement for endoscopic calcaneoplasty. Arthroscopy. 2011;27:1110–1117. doi: 10.1016/j.arthro.2011.02.030. [DOI] [PubMed] [Google Scholar]
- 20.Lui T.H. Reattachment of Achilles tendon after endoscopic calcaneoplasty. Foot Ankle Int. 2007;28:742–745. doi: 10.3113/FAI.2007.0742. [DOI] [PubMed] [Google Scholar]
- 21.Lui T.H. Treatment of chronic non-insertional Achilles tendinopathy with endoscopic Achilles tendon debridement and flexor hallucis longus transfer. Foot Ankle Spec. 2012;5:195–200. doi: 10.1177/1938640011434508. [DOI] [PubMed] [Google Scholar]
- 22.Lui T.H. Flexor hallucis longus tendoscopy: A technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17:107–110. doi: 10.1007/s00167-008-0623-x. [DOI] [PubMed] [Google Scholar]
- 23.Lui T.H. Arthroscopic synovectomy for zone 2 flexor hallucis longus tenosynovitis. Arthrosc Tech. 2015;4:e403–e405. doi: 10.1016/j.eats.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lui T.H. Endoscopic loose body removal from zone 2 flexor hallucis longus tendon sheath. Arthrosc Tech. 2016;5:e465–e469. doi: 10.1016/j.eats.2016.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lui T.H. Endoscopic adhesiolysis of the flexor hallucis longus muscle. Foot Ankle Spec. 2014;7:492–494. doi: 10.1177/1938640014546859. [DOI] [PubMed] [Google Scholar]
- 26.Lui T.H., Chan L.K. The safety of the posterior ankle arthroscopy in management of posterior ankle impingement: A cadaveric study. Foot. 2015;27:4–9. doi: 10.1016/j.foot.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Lui T.H. Arthroscopic treatment of posterior ankle impingement in the supine position using coaxial posterior portals. Foot Ankle Int. 2014;35:834–837. doi: 10.1177/1071100714534218. [DOI] [PubMed] [Google Scholar]
- 28.Lui T.H. Modified endoscopic release of gastrocnemius aponeurosis. J Foot Ankle Surg. 2015;54:140–142. doi: 10.1053/j.jfas.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 29.Lui T.H. Endoscopic gastrocnemius intramuscular aponeurotic recession. Arthrosc Tech. 2015;4:e615–e618. doi: 10.1016/j.eats.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic calcaneoplasty and Achilles tendoscopy of the left leg. The posteromedial and posterolateral portals are interchangeable as the viewing and working portals. Achilles tendoscopy is performed with debridement of the ventral surface of the Achilles tendon. Endoscopic calcaneoplasty is performed with an arthroscopic acromionizer. The posterosuperior surface of the calcaneus is resected down to the calcaneal insertion of the Achilles tendon. After completion of the resection, there should not be any impingement on the Achilles tendon during ankle dorsiflexion.