Abstract
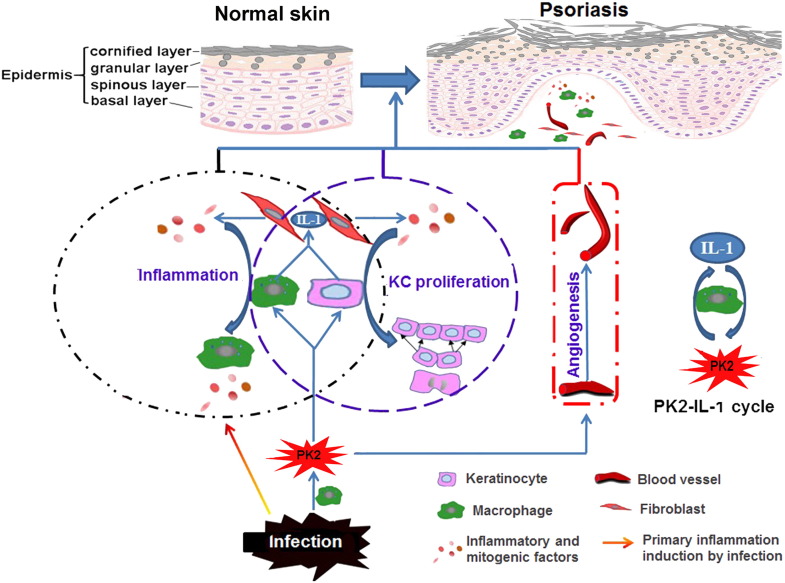
Psoriasis is histologically characterized by keratinocytes (KC) hyperproliferation, inflammation, and increased angiogenesis, but the pathological factor responsible for these symptoms is unknown. Here, a neuroendocrine peptide (prokineticin 2, PK2), is highly expressed in human and mouse psoriatic skins but no significant change in other autoimmune diseases, suggesting that PK2 is a psoriasis-specific factor. Bacterial products significantly up-regulated PK2, implying that infection induces PK2 over-expression. PK2 promoted KC and macrophage to produce interleukin-1 (IL-1), the central player of inflammation and psoriasis, which acts on adjacent fibroblast to induce inflammatory cascades and KC hyperproliferation. IL-1 feeds back on macrophages to induce PK2 production to perpetuate PK2-IL-1 positive feedback loop. PK2 also promoted angiogenesis, another psoriatic symptom. In mouse models, PK2 over-expression aggravated psoriasis while its knock-down inhibited pathological development. The results indicate that PK2 over-production perpetuates psoriatic symptoms by creating PK-2-IL-1 vicious loop. PK2 is a central player in psoriasis and a promising psoriasis-specific target.
Keywords: Prokineticin2, Psoriasis, Interleukin-1, Angiogenesis, Inflammation, Cell proliferation
Highlights
-
•
High level of PK2 is found in psoriasis but not in other autoimmunity diseases.
-
•
Bacterial products induce PK2 over-expression to promote IL-1 signal.
-
•
IL-1 induces PK2 secretion to create a PK2-IL-1 circle to perpetuate symptoms.
-
•
PK2 is a central player in psoriasis and may be a psoriasis-specific target.
Psoriasis is a common autoimmune disease whose pathogenesis remains poorly understood. We found that PK2 was highly expressed in psoriasis but not in other autoimmune diseases. To investigate the role of PK2 in psoriasis, the effect of PK2 on keratinocyte proliferation, inflammation and angiogenesis were analyzed. PK2 expression mediated by virus in psoriasis was applied. The results demonstrated that PK2 promoted psoriasis development. PK2 over-expression in mouse model aggravates psoriasis while knock-down of PK2 improves the disease. PK2 plays a pivotal role in psoriasis.
1. Introduction
Prokineticin2 (PK2), also named Bv8, is a small 8 kDa protein first found in skin secretions of the frog Bombina variegate (Mollay et al., 1999). It belongs to the PK protein family, which has a conserved N-terminal sequence of AVITGA and 10 cysteines. In mammals, the PK protein family is involved in a number of biological activities such as ingestive behaviours, circadian rhythms, angiogenesis, inflammation and inflammatory pain. Two closely related G protein-coupled receptors (PKR1 and PKR2)mediate signal transduction of PKs (Negri et al., 2004, Shojaei et al., 2008). Psoriasis, a chronic cutaneous disorder with a spectrum of clinical phenotypes including red, scaly and well-demarcated skin lesions formed by hyperproliferation of epidermal keratinocytes (KC), affects approximately 1–3% of the worldwide population (Baliwag et al., 2015, Di Meglio et al., 2014, Gottlieb, 2005, Nestle et al., 2009). Besides causing ecological burdens, psoriasis produces a severe psychosocial burden such as anxiety, depression, and perceived stress, therefore significantly impairs the quality of patients' life (Gupta et al., 2015, Tohid et al., 2016, Villasenor-Park et al., 2012). A new emerging concept of psoriasis is that psoriasis is a chronic and disabling disease characterized by an immune-mediated inflammatory background involving skin, joints or both, often associated with several metabolic and non-metabolic comorbid diseases (Coates et al., 2016, Gupta et al., 2015, Menter, 2016). Given that psoriasis is a chronic disabling disease, the long-term safety is the major critical determinant driving the choice of treatment (Campanati et al., 2016). However, understanding of psoriasis has evolved over the years from an epidermal KC disease to an autoimmune disease to a systemic inflammatory disease (Bachelez, 2005, Nestle et al., 2009); its pathogenesis is still poorly understood. The mainstay of treatment is topical therapy, but systemic therapy is considered for the patients with moderate-to-severe disease who do not respond to topical treatments. The current available conventional systemic treatments are associated with several side effects over a long time (Asahina et al., 2016, Guerra et al., 2016). Numerous inflammatory cytokines, such as IL-17, TNF-а and IL-23, are over-produced in psoriatic skin, with their levels correlated with the severity of psoriasis disease (Baliwag et al., 2015, Kofoed et al., 2015). To target these cytokines in psoriatic disease, some anti-cytokine biologic drugs are emerging (Di Meglio et al., 2014; Eberle et al., 2016). However, as disease biomarkers, none of these cytokines has so far met the sensitivity, specificity, and accuracy criteria that would allow their translation into clinical use (Villanova et al., 2013). Psoriasis-specific pathogenesis has not been identified although inflammatory disorders play important roles in this disease as in other autoimmune diseases (Ryan et al., 2014). The cause and mechanism underlying histological symptoms in psoriasis skin remain unknown. Especially, several crucial questions for psoriasis pathogenesis remain to be elucidated including: 1) What is the initiator of psoriasis and how to initiate it? 2) Why and how do KCs abnormally proliferate and differentiate? 3) What is the mechanism triggering processing of IL-1 identified as a key player in psoriasis pathogenesis? 4) What is and how to be responsible for abnormal angiogenesis, such as dilated and contorted blood vessels in psoriatic lesions? 5) How to perpetuate inflammatory and angiogenesis disorder? Here we show that PK2, a multifunctional peptide known to promote inflammation and angiogenesis, plays a key role in psoriatic cell signaling.
2. Materials and Methods
2.1. Collection of Human Samples and Study Approval
Biopsies of psoriasis skin were obtained from the limbs of 3 different patients with moderate to severe plaque psoriasis, in which 2 were females with psoriatic plaque on arms and legs, 1 was a male with psoriatic plaque on limbs and torso. The Psoriasis Area and Severity Index (PASI) scores were 19.2, 21.6 and 27.6 respectively. Normal samples were obtained from limbs of human with no characteristic of any skin diseases. The 10 samples for IHC were skin tissues embedded in paraffin blocks and stored for < 2 years. All the samples were obtained from the patients with PASI > 12. The blood samples of healthy controls were obtained from 60 volunteers. Psoriatic blood samples were obtained from 52 psoriatic patients aged 24–62 years with PASI > 12, of which 24 were females and 28 were males. For each disease, 50 blood samples were taken from patients diagnosed with Crohn's disease, ulcerative colitis, atherosclerosis and type 1 diabetes mellitus. Human samples were from the first affiliated hospital of Kunming Medical University and the affiliated hospital of Jiangnan University Wuxi 4th People's Hospital. The use of human samples for research was approved by the ethical committees of the local hospitals. In all cases, informed patients consent was obtained. All the experiments were reviewed and approved by the internal review board of Kunming Institute of Zoology, Chinese Academy of Sciences (SMKX2016017).
2.2. Animals
K14-VEGF transgenic mice were from State Key Laboratory of Biotherapy, Cancer Center, Western China Hospital, Sichuan University. Kunming mice and C57BL/6 mice were purchased from Kunming Medical University. All the experiments complied with national legislation and were approved by the Committee on the Ethics of Animal Experiments of Kunming Institute of Zoology, Chinese Academy of Sciences (SYDW2013019).
2.3. Peptide and Antibodies
PK2 was purchased from PeproTech, Inc. (USA). Antibodies of PK2, CD3, CD31, CD4, CD8, E-selectin and PPARβ were purchased from Santa Cruz Biotechnology, Inc. (USA); Antibodies of extracellular regulated kinase (ERK), phosphorylated ERK (P-ERK), p38 mitogen-activated protein kinase (p38 MAPK), P-p38, Jun. N-terminal kinase (JNK), P-JNK, and β-actin were purchased from Cell Signaling Technology, Inc. (USA); Antibodies of caspase-1 was purchased from Merck Millipore (USA); Antibodies of α-smooth muscle actin (α-SMA), absent in melanoma 2 (AIM2) were purchased from Abcam (Cambridge, MA, USA). Other chemicals or antibodies without special illustration were purchased from Sigma-Aldrich (USA).
2.4. Analysis of Skin Extracts by RP-HPLC
Human skin of normal and psoriasis were homogenized by continuously grinding in a cold (4 °C) 1:1 distilled water/ethanol 96% (v/v) mixture acidified to pH 3 by the addition of citric acid. Then the suspensions were centrifuged for 30 min at 4 °C with 6000g and the supernatants were filtered using an Amicon Ultracel-30 membrane to cut-off size over 30 kDa (Lande et al., 2007). The filtrate was applied onto a C8 reversed-phase high-performance liquid chromatography column (RP-HPLC, Hypersil 5 μm C8, 4.6 × 300 mm) and eluted by acetonitrile gradient. Compared to normal skin, some additional eluted peaks were observed in the extracts of psoriatic skins and analyzed by quadrupole time-of-flight mass spectrometer (Q-TOF2 mass spectrometer; Waters Micromass) to identify peptides according to the mass. Sequences of peptides were confirmed by MS/MS analyses of Lys-C digests with nano-electrospray ionization.
2.5. Histological Analysis
After fixation by 4% formalin, tissues were dehydrated by an increasing concentration of alcohol, embedded in paraffin and then sectioned into 5 μm slices using a histocut (Leica, RM2235, Germany). All sections were deparaffinized and rehydrated for Hematoxylin and Eeosin (H&E) staining and immunohistochemistry (IHC) analysis. For IHC analysis, sections were incubated with antibodies against PK2, CD3, CD31, CD4, CD8, α-SMA and E-selectin, respectively. Immunoreactivities were visualized with a horseradish peroxidase-conjugated secondary antibody.
2.6. PK2 Quantitation
IHC was used to investigate the differential expression of PK2 in skins of psoriasis patients and healthy human, as well as in mouse skin. PK2 expression in skin of imiquimod–induced psoriasis mouse model was analyzed by western blot. PK2 concentration in skin and blood was determined by ELISA (CUSABIO, China), and the procedure was performed according to the manufacturer's instructions.
2.7. Effects of Bacterial Products and IL-1 on PK2 Production
Raw 264.7 murine macrophage cells were cultured in Dulbecco's modified Eagle's medium (DMEM, GIBCO, USA) supplemented with 10% fetal bovine serum, 100 units/ml of penicillin, and 100 μg/ml of streptomycin in a humidified 5% CO2 atmosphere at 37 °C. 2 × 104 Raw 264.7 murine macrophage cells/well were plated into a 96-well plate. After overnight incubation, the cells were adhered to the plate. Then the medium was changed into DMEM supplemented with 1% fetal bovine serum to starve the cells for 16 h. Bacterial products including DNA and lipopolysaccharide (LPS) or IL-1β were added to the wells for 24 h of incubation, using the same volume of PBS as blank control. At the end of incubation, the supernatants were collected for PK2 detection by ELISA (CUSABIO, China), and the procedure was performed according to the manufacturer's instructions.
2.8. Isolation of Fibroblasts (FB) and Keratinocytes (KC) From Newborn Mice
FB and KC were isolated from newborn mice skins according to previous method (Lichti et al., 2008). Kunming newborn mice (1–2-day-old) were sacrificed by deep CO2 narcosis and sterilized. The skins were removed immediately, and spread out completely and floated on cold trypsin (0.25%, w/v, Sigma-Aldrich, without EDTA) with dermis side down at 4 °C overnight. After trypsin treatment, the skins were transferred to dry culture dishes with the epidermis side down and spread gently to make the epidermis be in contact with the plastic at various points around the edges. The dermis was lifted up straight above the epidermis. Dermis was transferred into culture dishes containing DMEM (GIBCO, USA) supplemented with 10% FBS, 200 units/ml of penicillin and 200 μg/ml of streptomycin (GIBCO, USA) for the preparation of FB. Epidermis was transferred into culture dishes containing Minimum Essential Medium (S-MEM, GIBCO, USA) supplemented with 0.2 mM Ca2 +, 8% FBS (v/v) chelated with chelex-100 resin (Bio-Rad, USA), 200 units/ml of penicillin and 200 μg/ml of streptomycin for the preparation of KC. The suspension of dermis and epidermis were filtered through a 100-μm cell strainer (BD, USA) at 1000 g for 5 min after they were minced and triturated sufficiently. FB and KC were resuspended in DMEM and S-MEM (0.2 mM Ca2 +), then transferred into culture bottles, respectively. After incubation for 24 h, the culture medium was aspirated and the cells were washed with PBS to discard unattached cells and debris. Enough medium was added to the cells before cultured in a humidified 5% CO2 atmosphere at 37 °C (Lichti et al., 2008).
2.9. Cell Proliferation Assay
Cells were seeded in 96-well plates at a density of 1 × 104 cells/well. For KC and FB co-culture, an in vitro co-culture system of millicell culture inserts (0.4 μm pore Millipore, USA) was used, with FB in the bottom of the 24-well plates and KC within the inserts. Cell viability was studied using 3-(4, 5-dimethyl-2-thiazolyl)-2, 5-diphenyl tetrazolium bromide (MTT) assay. At the end of the incubation, 10% volume of 5 mg/ml MTT was added to each well for additional 4 h incubation. Then the millicells were transferred to new 24-well plates, and cells were dissolved in dimethyl sulfoxide (DMSO). The absorbance at 570 nm was measured on a microplate reader (Epoch Etock, BioTek, USA). The relative viability of the cells compared to the control was determined using the following formula:
Cell viability produced by concentrations of PK2 which greater than control was used for the cell proliferation assay.
2.10. Effects of PK2 on Production of Cytokines
Raw 264.7 murine macrophage, KC and FB cells (2 × 105) were seeded in 96-well plates and treated with PK2 for 48 h. In the system of KC or FB co-cultured with Raw 264.7 murine macrophage cells, Raw 264.7 murine macrophage cells were seeded in 24-well plates while KC or FB was seeded in inserts. In the system of KC co-cultured with FB, FB was seeded in 24-well plates and KC was seeded in inserts. Cytokines' expression was measured by ELISA and/or quantitative real-time PCR. To investigate the function of MAPK signal pathway to IL-1 secretion, cells were treated with 10 μM of the inhibitors of ERK (U0126), P38 (SB203580), JNK(SP600125) (Sigma-Aldrich, USA) for 30 min before treated with PK2 or LPS, then the release of IL-1β was measured by ELISA kit (Dakewei, China).
2.11. Quantitative Real-time PCR (qPCR)
RNA was extracted using RNAprep pure cell kit (Tiangen, China) and the first strand cDNA was synthesized using first strand cDNA synthesis kit (TaKaRa, China). qPCR was carried out on the platform of the iQ2 system (BioRad Laboratories, Hercules, CA, USA) with SYBR Premix Ex Taq II kit (TaKaRa, DRR081A) using primers listed in Table S1.
2.12. Western Blot Analysis
Cells were washed twice with ice-cold phosphate-buffered saline (PBS, 8 g/l NaCl, 0.2 g/l KCl, 0.2 g/l KH2PO4, 3.47 g/l Na2HPO4, pH 7.4) and collected by centrifugation at 1000 g for 5 min. The washed cell pellets were resuspended in 100 μl of extraction lysis buffer (50 mM Tris-HCl, pH 7.4, 1% Nonidet P-40, 0.25% sodium deoxycholate, 150 mM NaCl, 1 mM EDTA, 1 mM Phenylmethanesulfonyl fluoride (PMSF), 1 μg/ml each of aprotinin, leupeptin, and pepstatin, 1 mM sodium orthovanadate, and 1 mM NaF) and incubated for 30 min at 4 °C. The cell lysate was centrifuged at 12,000 g for 10 min to remove cell debris, followed by quick storage at − 70 °C for western blot analysis. Protein concentration was determined by BCA protein assay kit (Thermo, USA). A total of 40 μg of protein was subjected to SDS-polyacrylamide gel electrophoresis (SDS-PAGE) on a gel concentration of 12% and electro-transferred onto a polyvinylidenedifluoride (PVDF) membrane (Roche Diagnostics GmbH, Germany). The immunoblot PVDF membrane was blocked with 5% non-fat dried milk (BD, USA) dissolved in Tris-buffered saline tween-20 (TBST, 2.42 g/l Tris base, 8 g/l NaCl, 0.1% Tween 20, pH 7.6) at room temperature for 2 h. The PVDF membrane was washed three times with TBST and was incubated overnight with primary antibodies at 4 °C, and then it was incubated with the secondary antibody for 1 h at room temperature. After washing with TBST, membranes were developed with enhanced chemiluminescence kit (TIANGEN, China) in a dark room.
For KC and Raw 264.7 cells, the cells were treated with different concentrations of PK2 for 15 min after treated with or without LPS for 2 h in serum – free medium. Then EKR, JNK, P38 and their phosphorylated proteins were analyzed by western blot as described above. For THP-1 cells, cells were treated with different concentrations of PK2 for 30 min after starved by 2% medium for 16 h. Then AIM2 and caspase-1 activation were analyzed by western blot.
2.13. Effect of PK2 on Angiogenesis
In vitro angiogenesis formation was evaluated in human umbilical vein endothelial cells (HUVECs). The cells were cultured in M200 medium (GIBCO, USA) supplemented 1 × low serum growth supplement (LSGS; GIBCO, USA) and 10% fetal bovine serum (FBS) at 37 °C in a humidified 5% CO2 atmosphere. After detaching by trypsinization, HUVECs were washed and resuspended in serum-free M200 medium containing 1 × LSGS, and then the cells (1 × 105) were seeded into the 96-well plate pretreated with Matrigel matrix. Cells were incubated with vehicle (PBS), PK2, or basic fibroblast growth factor (b-FGF) for 6 h. Tubes were photographed using a microscope (Olympus, Tokyo, Japan).
In vivo angiogenesis formation in the chicken chorioallantoic membrane (CAM) was performed as described (Mousa et al., 2006). Fertilized eggs were incubated at 37 °C and 60% relative humidity in a forced draught incubator. At day 6, a window opening was punctured in the shell at the air sac of each egg, and then the sterile filter disks preincubated with test samples were placed on the CAM. The control eggs received PBS only. The window opening of eggs was closed with parafilm, and the eggs were maintained in the incubator for another 72 h. After that, the eggs were opened and CAM vasculatures were photographed using a digital camera (Canon, EOS 60D). The angiogenic response was evaluated by counting the vessel density using Photoshop CS6.
2.14. Differentiation Assay of HaCaT KC
HaCaT (human keratinocyte cell line) cells were from Kunming Cell Bank, Kunming Institute of Zoology, Chinese Academy of Science. The cells were cultured in DMEM supplemented with 10% FBS. To differentiate to the basal phenotype, HaCaTs were cultured in M154CF medium (GIBCO, USA) containing 8% fetal bovine serum (chelated with chelex-100 resin), 100 units/ml penicillin, 100 μg/ml streptomycin, and 0.04 mM Ca2 + for 5 days and kept the confluency of cultures below 75–80%. After that, cells were treated with or without 0.2 nM PK2 for 72 h, keratin 1 (K1), keratin 5 (K5), and involucrin were detected by qPCR.
2.15. Full-thickness Wound Mouse Model
According to our previous method (Mu et al., 2014), after anesthetizing with 1% pentobarbital sodium (0.1 ml/20 g body weight), dorsal hairs were removed and dorsal skin was cleansed with betadine in male Kunming mice (age 6–8 week). Two full-thickness skin wounds were created on the back of each mouse using an 8-mm-diameter biopsy punch and each mouse was caged individually. Ten micro liters of vehicle (0.9% NaCl solution), PK2 (100 μg/ml) or recombinant murine EGF (100 μg/ml, PeproTech Inc., USA, positive control) was applied directly to the wound site twice daily for seven days (day 1–day 7). Wound healing was monitored by using IPLab imaging software (BD Biosciences, Bedford, MA, USA). Mice were sacrificed on day 3, 5 and 7 post-wounded and biopsy specimens involving the central part of the wounds were obtained for light microscopy. Skin sections were prepared for histological and IHC analysis as mentioned above.
2.16. Imiquimod-induced Psoriasis-like Dermatitis in Mice
Twenty C57BL/6 mice were randomly divided into two groups. Control mice in group 1 were left untreated. Backs of mice in group 2 were shaved and given a daily topically treatment of imiquimod cream (5%) (iNova Pharmaceuticals Australia Pty Limited) for 7 days. A blinded procedure was used to monitor psoriasis-like skin inflammation. Clinical scoring of psoriasis based on the human clinical Psoriasis Area and Severity Index (PASI) was performed. Three variables were evaluated - erythema, scaling, and thickening. Each of them scored independently on a scale ranging from 0 to 4: 0, none; 1, slight; 2, moderate; 3, marked; 4, very marked. The cumulative score was a total of the three parameter scores ranging from 0 to 12 and the cumulative score of the mouse between 8 and 12 was used.
2.17. Plasmids Vector Construction
The coding region of mouse PK2 was amplified from mouse testis cDNA by standard PCR and cloned into the EcoRI and BamHI site of PLVX-puro vector (Clontech Laboratories, Inc., USA). The empty PLVX-puro vector was used as blank control. The oligonucleotides of shRNA sequence targeting PK2 (sh-PK2) and its negative control scrambled shRNA (sh-Scr) sequence were synthesized by Sangon Biotech Ltd. (Shanghai, China). The sequence of sh-PK2 is: CAUAAGGAUCUGCACACCUAUCUCGAGAUAGGUGUGCAGAUCCUUAUGUUUU (Cheng et al., 2012) while that of sh-Scr is: AGUACUGCUUACGAUACGGUUCAAGCGACCGUAUCGUAUUAGCAGUACUUUU. The oligonucleotides of sh-PK2 and sh-Scr including the digested site of BamHI and EcoRI were annealed with their complementary sequences and inserted into the BamHI and EcoRI site of the RNAi-Ready pSIREN-RetroQ Vector (Clontech Laboratories, Inc., USA) to form retroviral vectors of psh-PK2 and psh-Scr, respectively. The transfection procedure was performed according to the manufacturer's instructions.
2.18. Virus Production
The lentiviral vector of PLVX-puro vector and retroviral vector RNAi-Ready pSIREN-RetroQ vector were used as PK2 over-expression and knockdown system in this study, respectively. The two vectors were respectively packed with HEK 293T cells and EcoPack™ 2–293 cells. For each virus preparation, 1.5 × 107 HEK 293T cells or EcoPack™ 2–293 cells were plated in T175 flask for 24 h before transfection. PLVX-puro empty vector (7 μg) or with PK2 gene and the packaging plasmids including pMDlg/PRRE (5.4 μg), Prsv-REV (2.8 μg), and pMD2.G (3.5 μg) were co-transfected into HEK 293T cells by Fugene 6 (Promega, USA). Each flask of EcoPack™2–293 cells were transfected with 5 μg psh-PK2 or psh-Scr in 1.5 μl xfect polymer (Clontech, USA) as transfection reagent. The transfection procedure was according to manufacturer's manual. Eight hours later, the medium containing transfection reagent and plasmids was changed with fresh medium. After 48 h from the first transfection, the supernatants containing virus were harvested and the cells were re-fed with new fresh medium and incubated for another 24 h. Then the second round of the supernatants was collected and combined together with that from the first round, and concentrated by ultracentrifugation using P28S rotor at 25,000 rpm for 2.5 h at 4 °C.
2.19. Effect of PK2 Expression on Mouse Model of Psoriasis
K14-VEGF male mice (two-month old) were housed under a 12:12 h light: dark cycle with food and water available ad libitum. Mice were divided into 5 groups: the blank control group (C), PK2 over-expression group (P), negative control of over-expression group (NP), PK2 knockdown group (S), and negative control of PK2 knockdown group (NS). NaCl (0.9%) solution, the lentivirus of PK2-PLVX-puro and empty PLVX-puro, the retrovirus of psh-PK2 and psh-Scr was delivered into above five groups mice respectively by tail vein injection. Effects of virus on PK2 expression in mice were examined by skin IHC and blood ELISA. A series of psoriasis indexes (levels of cytokines, redness, thickness, weight, and swelling of ear, and weight of lymph nodes) were measured in mice. The levels of cytokines in serum sampled from eye blood on day 0, 10, 20, and 30 were determined by ELISA. IHC analysis was used to detect some immune indexes including CD3, CD4, CD8, CD31, and E-selectin of the mouse ear.
2.20. Statistics
For statistical analysis, data obtained from three independent experiments were presented as mean ± SD. All statistical analyses were two-tailed, with 95% confidence intervals (CI) and conducted using GraphPad prism 5. Results were analyzed using an unpaired t-test. Differences were considered significant when P < 0.05.
3. Results
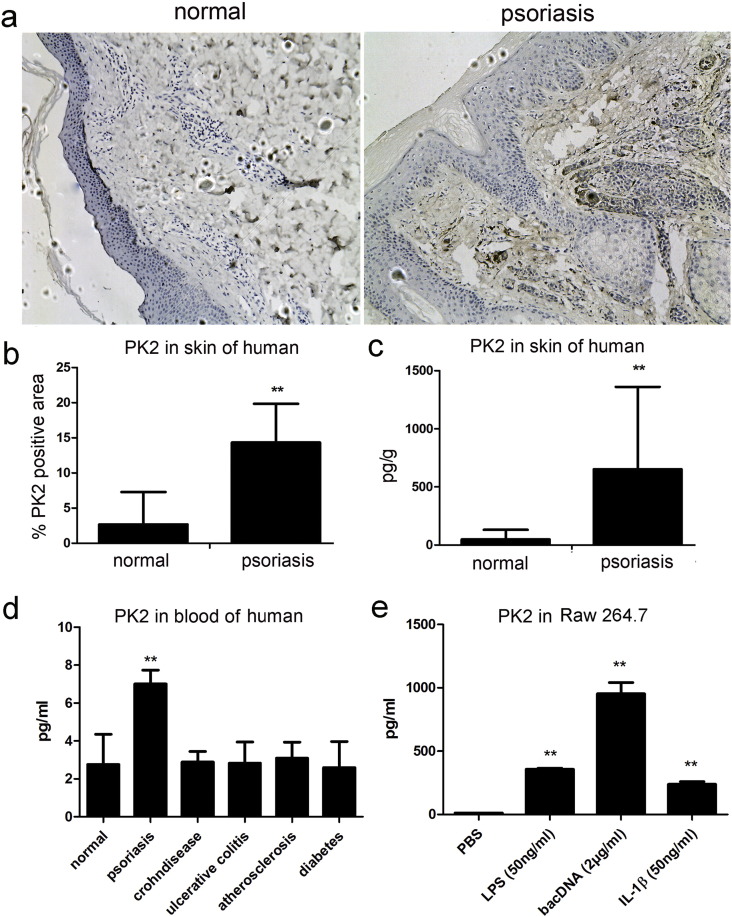
3.1. PK2 Level Is Abnormally High in Human Psoriatic Skin and Blood
To explore the psoriasis-triggering factor(s), extracts of healthy human and psoriatic skins were compared. Among the additional eluted peaks observed in psoriatic skin extract (Fig. S1), we identified those representing psoriasin and an endogenous cathelicidin antimicrobial peptide LL-37, two peptides already known to be associated with the disease (Lande et al., 2007). PK2 was identified as another prominent disease biomarker (indicated by an arrow in Fig. S1b). Indeed, IHC staining (Fig. 1a & b) revealed that there are much more PK2-positive cells in psoriatic skin than that in healthy skin. Enzyme-linked immune sorbent assay (ELISA) showed that PK2 level was dramatically increased in both the skin and blood of psoriasis patients (Fig. 1c & d). Particularly, the expression of PK2 in psoriatic skin (~ 650 pg/g) was ~ 12 times higher than that in normal skin (~ 50 pg/g) (Fig. 1c). The expression of PK2 in skin is normally very low (Negri and Lattanzi, 2011). No significant change was found in patient serum of other autoimmune diseases including inflammatory bowel diseases (IBDs, including Crohn's disease and ulcerative colitis), atherosclerosis, and diabetes (Fig. 1d). Profound and specific over-production of PK2 in psoriasis patients indicated that it might be responsible for causing the histopathological symptoms.
Fig. 1.
Elevated PK2 expression in human psoriasis skin and blood. a, b. PK2 expression analyzed by IHC, PK2-positive staining is marked by red arrows. c. ELISA analysis of PK2 in normal and psoriatic skins. d. ELISA analysis of PK2 in normal, psoriasis, atherosclerosis, Crohn's disease, ulcerative colitis, and diabetes blood. e. ELISA analysis of PK2 in Raw 264.7 induced by LPS, bacterial DNA, and IL-1β. All the bars represent the average of three independent experiments ± SD. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01).
3.2. Bacterial Products Promote PK2 Production
To explore the origin of PK2, bacterial products were applied to stimulate Raw 264.7 murine macrophage cell, which is the main cell type to induce inflammation and to secrete PK2. As illustrated in Fig. 1e, normal Raw 264.7 secreted little (~ 12.4 pg/ml) PK2 while LPS (50 ng/ml) and bacterial DNA (2 μg/ml) induced 357 and 953.2 pg/ml PK2 production. IL-1, the central player of inflammatory reactions and psoriatic plaques, also promoted PK2 production. At the concentration of 50 ng/ml, IL-1β induced 238.1 pg/ml PK2 production in Raw 264.7 (Fig. 1e).
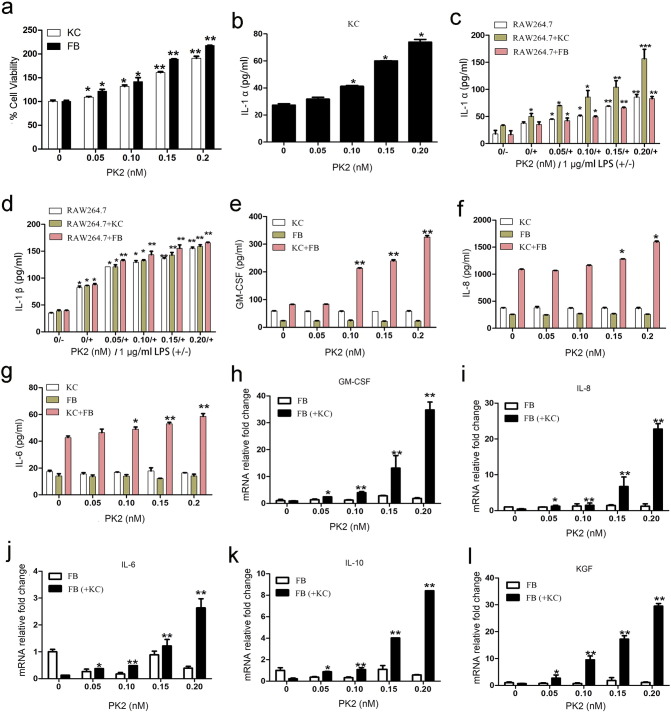
3.3. PK2 Promotes IL-1 Production and Proliferation of Co-cutured KC and FB
Effect of PK2 on proliferation of KC and FB, which are juxtaposing cells in skin both affected by psoriasis, was examined. No proliferation effect was observed when KC or FB was treated with PK2 (Fig. S2a & b), but KC and FB proliferation was induced by PK2 in a concentration-dependent manner when the two types of cells were co-cultured (Fig. 2a & Fig. S2c). KC, but not FB, produces biologically active IL-1, which is able to activate many secondary cytokines in the skin (Kofoed et al., 2015). In addition, IL-1R1, which is expressed in FB, not in KC, mediates all IL-1 biological response (Chong et al., 2009). It was found that IL-1 secretion in KC was promoted by PK2 (Fig. 2b). Considering that IL-1 has a pronounced influence on skin homeostasis (Schroder, 1995), we hypothesized that the proliferation effect of PK2 on KC and FB may be mediated by IL-1. This hypothesis was supported by blockade of IL-1 receptor using IL-1 receptor antagonist (IL-1ra), which resulted in strong inhibition of PK2-induced KC and FB proliferation (Fig. S2c). PK2 also stimulated macrophage, another important epidermal cell type, to secret IL-1 (Fig. 2c & d). Many other mitogenic and proinflammatory factors including keratinocyte growth factor (KGF), granulocyte macrophage colony-stimulating factor (GM-CSF), IL-6, -8, and -10 were induced by PK2 when KC was co-cultured with FB but not when KC or FB was cultured alone (Fig. 2e & l). In particular, KGF is a known potent mitogen for keratinocytes hyperproliferation and has been proposed to account for epidermal hyperplasia associated with psoriasis (Finch et al., 1997, Kovacs et al., 2006, Kovacs et al., 2005). At the concentration of 0.2 nM, PK2 induced an up-to-29-fold elevation of KGF expression in FB when co-cultured with KC (Fig. 2l).
Fig. 2.
Effects of PK2 on FB and KC proliferation and cytokines secretion. a. Effects of PK2 on FB and KC proliferation when they were co-cultured. b. Effects of PK2 on IL-1α production in KC. c, d. Effects of PK2 on IL-1α and IL-1β production in Raw 264.7 alone or co-cultured with FB or KC. e–g. Effects of PK2 on GM-CSF, IL-8, and IL-6 production in KC, FB, and KC co-cultured with FB by ELISA. h–l. Effects of PK2 on mRNA expression of GM-CSF, IL-8, IL-6, IL-10, and KGF in FB alone or FB co-cultured with KC by qPCR. All the bars represent the average of three independent experiments ± SD. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01).
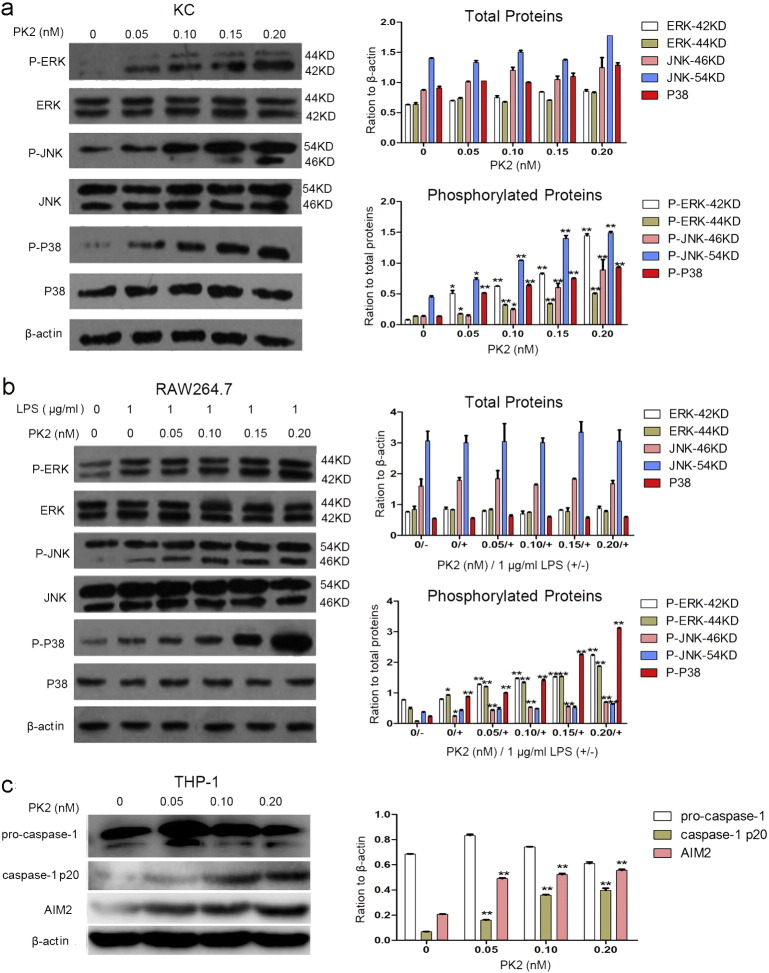
3.4. PK2 Possibly Activates MAPK and AIM2 Signaling Pathways to Promote IL-1 Secretion
As illustrated in Fig. 3a & b, PK2 induced phosphorylation of ERK1/2, JNK and p38 in a concentration-dependent manner in both KC and LPS-activated Raw 264.7 murine macrophage cells. Since MAPK signaling is important for regulation of cell growth, differentiation, and control of cellular responses to pro-inflammatory cytokines (Chang and Karin, 2001), its activation by PK2 may contribute to IL-1 production and cell proliferation in KC and macrophage. IL-1 production induced by PK2 was blunted by inhibitors of MAPK signaling (Fig. S3). Fig. 3c shows that PK2 strongly up-regulated absent in melanoma 2 (AIM2) inflammasome signaling pathway in monocytic THP-1 cells. PK2 also significantly increased the expression of caspase-1, which is engaged by AIM2 to produce active IL-1β by catalyzing proteolytic cleavage of pro-interleukin-1β (pro-IL-1β) (Man and Kanneganti, 2015).
Fig. 3.
Effects of PK2 on MAPK signaling pathway in KC (a) and Raw 264.7 (b) and on AIM2 inflammasome signaling pathway in THP-1 (c). All the bars represent the average of three independent experiments ± SD. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01).
3.5. PK2 Promotes Angiogenesis, Wound Healing and KC and FB Differentiation
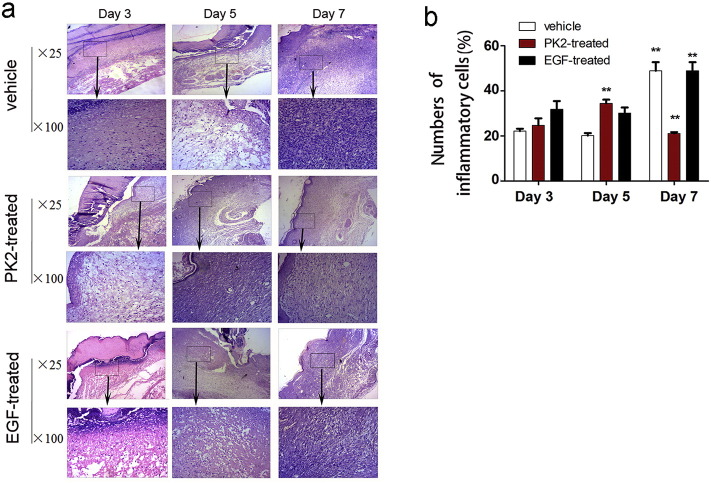
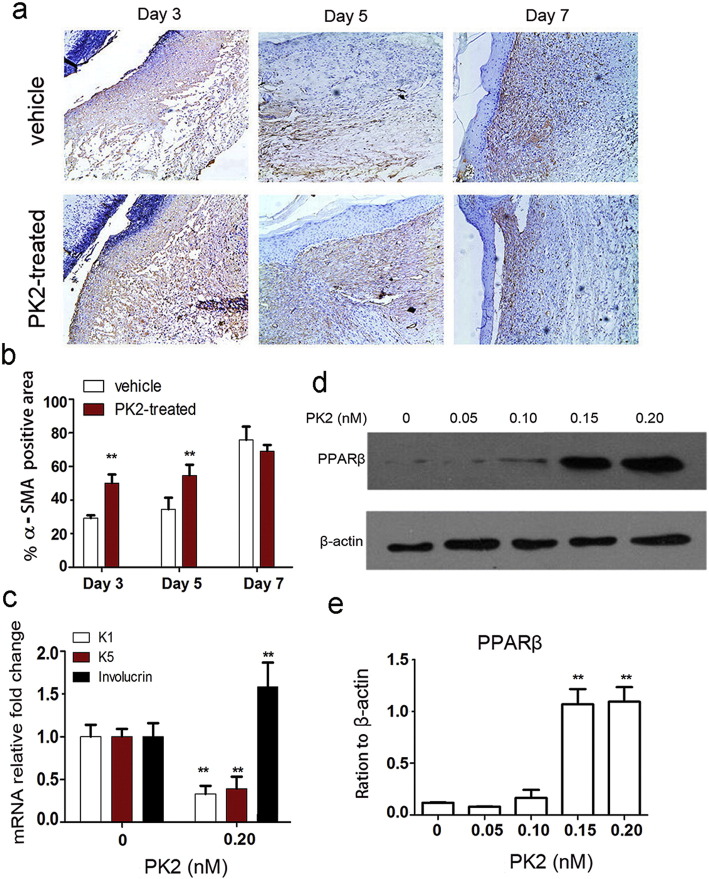
Considering that 1) PK2 promotes the secretion of IL-1 (Fig. 2b–d), a key mediator in the initiation and maintenance of psoriatic plaques (Mee et al., 2006); and 2) Psoriasis shares many features with wound healing and is considered as a model of exaggerated wound healing with contorted blood vessels (Morhenn et al., 2013, Shi et al., 2014), effects of PK2 on angiogenesis and wound healing are investigated. Increased angiogenesis and contorted blood vessels were observed after by PK2 treatment (Fig. S4). PK2 (0.05 nanomolar) increased angiogenesis by 1.5-fold while basic fibroblast growth factor (b-FGF) at the same dose only increased 0.8-fold. As illustrated in Fig. S5, PK2 accelerated the wound closure. At day 3, 5, and 7, 42.8, 21.6, and 7.6% residual wound was observed in PK2 treatment group (2 μg/day/wound), while that in vehicle group was 77.8, 44.6, and 32.1%, respectively. The corresponding residual wound ratio was 77, 20.8, and 9.8% in the group of epidermal growth factor (EGF) treatment, respectively. Wound healing is significantly accelerated in PK2 treatment compared to normal and EGF treatment. Histopathological study showed that PK2 accelerated the initiation and the end of inflammatory phase of wound (Fig. 4a & b). Fibroblast-to-myofibroblast (FTM) transition plays an important role in cutaneous wound healing (Kovacs et al., 2005). The expression of α smooth muscle actin (α-SMA), a marker of smooth muscle cell differentiation and FTM transition (Gabbiani, 2003), was elevated by PK2 in myofibroblasts of the granulation tissue below the wound surface (Fig. 5a & b). After treatment by 0.2 nM PK2, low level of keratin 1 and 5 and high level of involucrin were observed in HaCaT KC, indicting HaCaT KC differentiation induced with PK2 (Fig. 5c). KC differentiation induced by PK2 was further supported by the result that the expression of peroxisome proliferator-activated receptor β (PPAR-β) was elevated in FB by PK2 in a dose-dependent manner (Fig. 5d & e).
Fig. 4.
(a & b) PK2 accelerated inflammatory phase during wound healing. a. Histopathological examination of mice wound treated by PK2/EGF. (25 ×: visual field of magnified 25 times ; 100 ×: visual field of magnified 100 times). b. The statistic of inflammatory cells in wound.
Fig. 5.
PK2 promotes differentiation of FB and KC. a, b. PK2 promoted FB differentiation indicated by up-regulation of α-SMA expression. c. PK2 promoted KC differentiation indicated by down-regulation of K1 and K5 expression and up-regulation of involucrin expression. d, e. PK2 up-regulates PPARβ expression of FB co-cultured with KC. All the bars represent the average of three independent experiments ± SD. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01).
3.6. PK2 Over-expression Aggravated Psoriasis While PK2 Knock-down Inhibited Disease Development
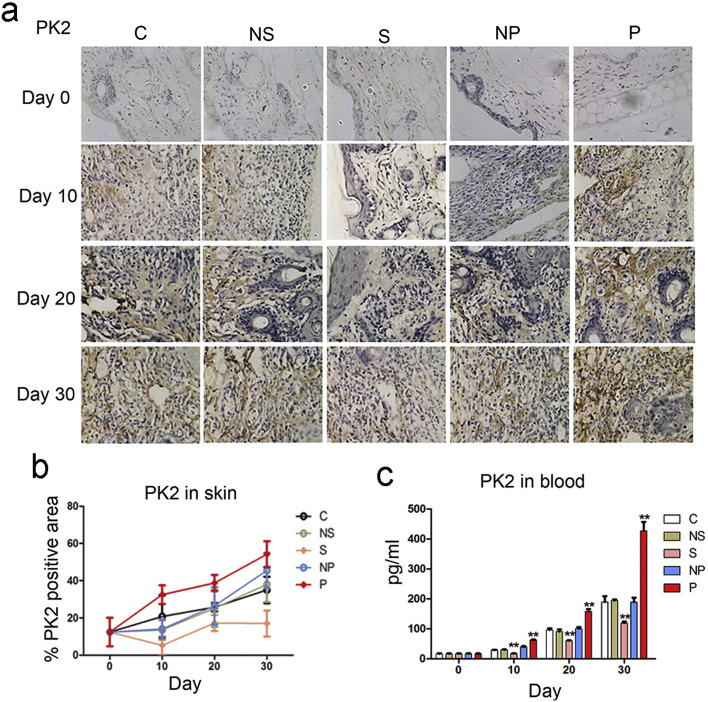
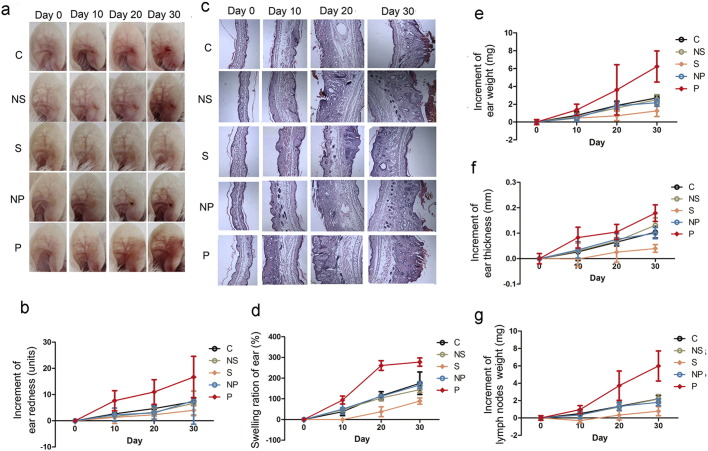
All the results so far demonstrate that high level of PK2 activates IL-1 signaling pathway to produce most of the characteristic features of psoriasis. To evaluate this mechanism in vivo, we used animal models to test effects of PK2 on psoriasis. Keratin 14 (K14)-vascular endothelial growth factor (VEGF) transgenic mouse model precisely matches human psoriasis in all features (Detmar et al., 1998, Xia et al., 2003). As illustrated in Fig. S6, substantial over-expression of PK2 was indeed observed in K14-VEGF psoriasis-like skins as well as in acute imiquimod-induced psoriasis-like skins, confirming our observations from human psoriatic skin (Fig. 1a–c). The level of PK2 in two-month old K14-VEGF mice (n = 20 each) was up-regulated by lentivirus-mediated over-expression of PK2 or down-regulated by retrovirus-mediated PK2-targeting short hairpin RNA (sh-PK2) (Fig. 6a–c). All mice showed psoriasiform features prior to PK2 expression interference, as indicated by erythematous and scaly ear skin (Fig. 7a–d). Psoriasiform symptoms were gradually aggravated by PK2 over-expression, as evaluated by increased ear redness, ear swelling, ear weight, ear thickness, and lymph node weight (Fig. 7a–g). Down-regulation of PK2 expression by sh-PK2, on the other hand, markedly inhibited aggravation of symptom (Fig. 7a–g).
Fig. 6.
The knockdown or overexpression of PK2 was interfered by virus. a, b. IHC analysis of PK2 in K14/VEGF mice skins. c. PK2 levels in blood of K14/VEGF mice. C: control, NaCl (0.9%) solution; NS: negative control of sh-PK2, retrovirus of psh-Scr; S: sh-PK2, retrovirus of psh-PK2; NP: negative control of PLVX-PK2, the lentivirus of empty PLVX-puro; P: PLVX-PK2, the lentivirus of PK2-PLVX-puro. All the bars and line graphs represent the average of three independent experiments ± SD for five mice in each group. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01) versus control at each time point.
C: control, NaCl (0.9%) solution; NS: negative control of sh-PK2, retrovirus of psh-Scr; S: sh-PK2, retrovirus of psh-PK2; NP: negative control of PLVX-PK2, the lentivirus of empty PLVX-puro; P: PLVX-PK2, the lentivirus of PK2-PLVX-puro. All the bars and line graphs represent the average of three independent experiments ± SD for five mice in each group. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01) versus control at each time point.
Fig. 7.
Effects of PK2 knockdown or over-expression on psoriasis symptoms in K14/VEGF transgenic mice. a, b. Change of mouse ear redness. c. Photomicrographs of ear sections stained with H&E. d–g. Changes of ear swelling (d), weight (e), thickness (f), and weight of lymph nodes (g). C: control, NaCl (0.9%) solution; NS: negative control of sh-PK2, retrovirus of psh-Scr; S: sh-PK2, retrovirus of psh-PK2; NP: negative control of PLVX-PK2, the lentivirus of empty PLVX-puro; P: PLVX-PK2, the lentivirus of PK2-PLVX-puro. All the bars and line graphs represent the average of three independent experiments ± SD for five mice in each group. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01) versus control at each time point.
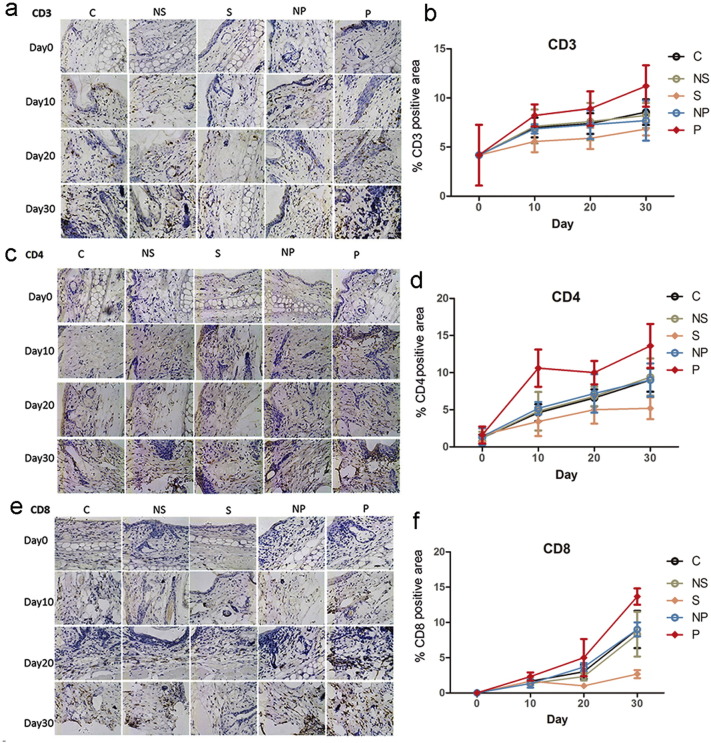
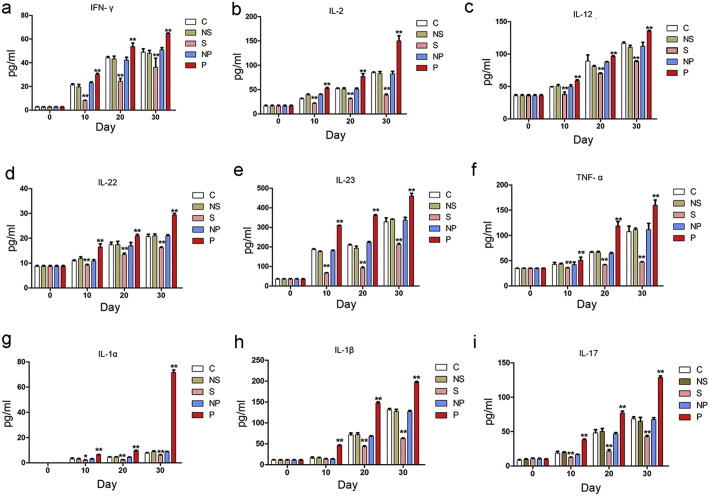
Histological evaluation further supported the role of PK2 in psoriasis progression. Psoriasis-like phenotypes, including epidermal hyperplasia with acanthosis, an absence of the granular layer of epidermis, focal parakeratosis, and the intralesional presence of mononuclear cells, were observed in control K14-VEGF mice (Fig. 7c). These phenotypes were more severe in PK2 over-expression mice but milder in sh-PK2 mice. Staining of CD3, CD4, CD8, CD31 and E-selectin positive cells revealed more inflammatory cells in PK2 over-expression animals and less inflammatory cells in mice treated with sh-PK2, compared to the control animals (Fig. 8a–f & Fig. S7). Inflammation was much milder in sh-PK2 mice than that in other groups. Cytokines levels were chronically elevated in all mice (Fig. 9a–i). Most of these cytokines were quickly elevated in the blood by PK2 over-expression while sh-PK2 markedly inhibited their elevation. Noticeably, the most prominent elevation was observed in IL-1 (IL-1α and IL-1β) and IL-17, key mediators in psoriasis pathogenesis (Fig. 9g–i). After 30 days of PK2 over-expression, the levels of IL-1α and IL-1β were increased by 20 to hundreds folds while sh-PK2 significantly blunted these changes (Fig. 9g & h) (Fig. 10).
Fig. 8.
Effects of PK2 knockdown or over-expression on mouse immunity. Immune indexes and their positive area scores of CD3 (a & b), CD4 (c & d), CD8 (e & f) of mouse ear within 30 days. C: control, NaCl (0.9%) solution; NS: negative control of sh-PK2, retrovirus of psh-Scr; S: sh-PK2, retrovirus of psh-PK2; NP: negative control of PLVX-PK2, the lentivirus of empty PLVX-puro; P: PLVX-PK2, the lentivirus of PK2-PLVX-puro. All the bars and line graphs represent the average of three independent experiments ± SD for five mice in each group. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01) versus control at each time point.
Fig. 9.
Effects of PK2 knockdown or over-expression on cytokines in mouse model. Cytokines of INF-γ (a), IL-2 (b), IL-12 (c), IL-22 (d), IL-23 (e), TNF-α (f), IL-1α (g), IL-1β (h), and IL-17(i) in blood. C: control, NaCl (0.9%) solution; NS: negative control of sh-PK2, retrovirus of psh-Scr; S: sh-PK2, retrovirus of psh-PK2; NP: negative control of PLVX-PK2, the lentivirus of empty PLVX-puro; P: PLVX-PK2, the lentivirus of PK2-PLVX-puro. All the bars and line graphs represent the average of three independent experiments ± SD for five mice in each group. Significant statistics difference indicated by asterisks (*, P < 0.05; **, P < 0.01) versus control at each time point.
Fig. 10.
Schematic illustration of cell signaling network underlying PK2's key role in the process of psoriasis and PK2-IL-1 positive feedback loop. PK2 stimulates KC and macrophages to produce IL-1. The released IL-1 acts on adjacent FB to promote secretion of multiple mitogenic and proinflammatory cytokines that consequently exerted proliferative and differentiating effects on KC and FB. The predominant IL-1 receptor in KC is IL-1R2, which is incapable of participating in IL-1 signaling, while that in FB is IL-1R1, which mediates all IL-1 biological response. The cytokines and chemokines produced by FB, in turn, recruit and activate immunocytes, leading to vicious cycle of inflammation. In addition, PK2 promotes angiogenesis.
4. Discussion
Psoriasis is a chronic systemic inflammatory and an autoimmune skin disease. It is histologically characterized by KC hyperproliferation, inflammation, and increased angiogenesis (Bachelez, 2005, Nestle et al., 2009). Although considerable progress in understanding the complex genetic, environmental, and immunological basis of psoriasis has been achieved, psoriasis pathogenesis remains not fully elucidated. Many biomarker candidates of psoriasis have been found, but none of them has so far met the sensitivity, specificity, and accuracy criteria that would allow their translation into clinical use (Villanova et al., 2013). Especially, limited information is available on psoriasis histopathogenesis related with chronic erythematous plaques, which is considered to be caused by KC hyperproliferation and abnormal angiogenesis. Although over-expression of vascular permeability factor/vascular endothelial growth factor and its receptors is found in psoriasis tissue, the factor responsible for contorted blood vessels in psoriatic lesions remains unknown (Detmar et al., 1994).
PK2 has been recently proposed to participate in numerous important physiological processes including inflammation, neurogenesis, tissue development, angiogenesis, and even nociception (Monnier and Samson, 2010, Negri et al., 2004, Shojaei et al., 2008). It exerts the actions by binding to two G protein-coupled receptors, PKR1 and PKR2 (Cheng et al., 2012, Lattanzi et al., 2001, Negri et al., 2004). PKR1 is exclusively responsible for mediating the modulation of macrophage cytokine production. PK2 is mainly expressed in brain but can also be found in skin, bone marrow, lymphoid organs, granulocytes, dendritic cells, macrophages, etc. (Martucci et al., 2006, Negri et al., 2007). PKRs are distributed in brain and the peripheral organs, including the spleen, and leukocytes, and they are found in most murine immune cell types (Dorsch et al., 2005, Franchi et al., 2008, Martucci et al., 2006). PK2 and its receptors are less expressed in skin but in this study, abnormally high PK2 level was found in human psoriatic skin and blood as well as mouse psoriatic skin and blood, but no significant change in other autoimmune diseases, suggesting that PK2 is a psoriasis-specific factor. PK2 is a multifunctional cytokine possessing abilities to induce epidermal, vascular and inflammatory change (Martucci et al., 2006, Monnier and Samson, 2010) as found in natural psoriasis.
Why and how are PK2 overexpressed in psoriasis? One of the best-characterized psoriasis initiation mechanisms is the antimicrobial peptide LL-37-DNA/RNA complex resulted from infection or physical trauma (Di Meglio et al., 2014), which induces inflammation, but how to initiate and develop psoriasis remains unknown. As illustrated in Fig. 1e, bacterial products including LPS and DNA promoted the production of PK2 besides inflammatory factors, suggesting that infection is a primary inducer of PK2 and inflammation.
Our results suggested that PK2 aggravates psoriasis by promoting KC and FB proliferation and differentiation, inflammation, and angiogenesis. Besides the well-known angiogenesis function of PK2, how did PK2 play the roles in psoriasis? PK2 significantly induced production of IL-1 in KC and macrophage. It is well known that TNF-a, IL-23, IL-17 and some other cytokines play important roles in psoriasis. These cytokines were up-regulated by PK2 in vivo but not obvious in KC or macrophage in our study. IL-1 plays multiple roles in the initiation of an inflammatory response to injury. In psoriasis, dysregulation of IL-1α and IL-1β plays significant roles in orchestrating the immune response (Cooper et al., 1990, Johnston et al., 2011, Perera et al., 2012). IL-1 is a direct chemoattractant to lymphocytes and exerts a further paracrine effect (Chung et al., 2009, Nourshargh et al., 1995). This may be why TNF-a, IL-23, IL-17 and some other cytokines were up-regulated by PK2 in vivo but not in vitro. IL-1 is the most likely initiator of the KC activation cycle (Perera et al., 2012). IL-1 is the inducer of nearly all other proinflammatory cytokines and is able to activate secondary cytokines in the skin (Schroder, 1995). The secreted IL-1 induced by PK2, which acts on adjacent fibroblast (FB), promoted the secretion of mitogenic and proinflammatory factors and consequently exerted proliferative and differentiation effects on KC and FB. Why was the co-culture of KC and FB required for the proliferation effect of PK2 as the result showed? The predominant IL-1 receptor in KC is IL-1R2, which is incapable of participating in IL-1 signaling, while that in FB is IL-1R1, which mediates all IL-1 biological response (Chong et al., 2009). Therefore, IL-1 produced by KC and macrophage likely acted in a paracrine fashion on adjacent FB, triggering the release of other cytokines to regulate proliferation of both KC and FB (Chong et al., 2009, Kovacs et al., 2005). This possibility was supported by observations that many mitogenic and proinflammatory factors including KGF, GM-CSF, IL-6, -8, and -10 were induced by PK2 when KC was co-cultured with FB but not when KC or FB was cultured alone.
In addition to promoting KC and FB proliferation and inflammation, PK2 induced HaCat keratinocyte differentiation. The use of normal human keratinocytes (NHKs) is a primary choice to study molecular mechanisms on the regulation of epidermal differentiation markers, as an easy to handle substitutes for primary human keratinocytes, the immortalized human keratinocyte cell line HaCaT has been widely used in mechanistic and pharmacological studies of potential skin drugs (Seo et al., 2012). Although HaCaT cells displayed some different attributes compared to NHKs, such as it displayed enhanced sensitivity to lethal doses of UV irradiation as compared to NHKs due to mutations leading to the lack of intact p53 alleles and a complete loss of p53 DNA-binding capacity (Pastore et al., 2011). As an alternative system, HaCaT cells maintained normal keratinocyte morphology and epidermal differentiation capacity, remained non-tumorigenic, and underwent, like normal human keratinocytes (Pastore et al., 2011). In this study, HaCat cells were used to study the differentiation function of PK2 on keratinocytes. KC differentiation induced by PK2 was further supported by the result that the expression of PPAR-β, which was found to exert potent pro-differentiating action in KC and possibly involved in psoriasis pathology (Romanowska et al., 2008, Schmuth et al., 2004, Westergaard et al., 2001), was elevated in FB by PK2. In wound healing mouse model, PK2 exerted promoting fibroblast differentiation to myofibroblast and accelerating inflammation. Both in vitro (HUVEC) and in vivo (CAM) angiogenesis assays show that PK2 leaded a markedly distorted, dilated, and contorted vascular phenotype, which is a distinguishing feature of psoriasis (Di Meglio et al., 2014, Perera et al., 2012). The results indicated that PK2 promoted KC and FB proliferation and differentiation, inflammation, and angiogenesis, which are all pathologic features of psoriasis (Shi et al., 2014).
All the results indicated PK2 stimulates IL-1 production, which plays important roles in the pathogenetic process of psoriasis. In addition to activation of MAPK signaling pathways, PK2 is found to up-regulate AIM2 inflammasome signal. The inflammasome is responsible for the synthesis and secretion of proinflammatory cytokine IL-1β (Schroder, 1995). The formation of inflammasome and the synthesis of IL-1β are of paramount importance for the pathogenesis of psoriasis (Schroder, 1995). In turn, IL-1 secretion induced by PK2 promoted PK2 production. The interaction between PK2 and IL-1 makes a PK2-IL-1 vicious circle to possibly sustain inflammation, KC hyperproliferation, and abnormal angiogenesis in psoriasis.
Over-expression of PK2 was observed in both K14-VEGF psoriasis-like skins and acute imiquimod-induced psoriasis-like skins, which is consistent with the results found in the human psoriatic skin. Over-production of PK2 caused most of the psoriatic symptoms including inflammation, angiogenesis, and KC hyperplasia while down-regulation of PK2 inhibited psoriatic development. Our results suggest that pathological increases in the level of PK2, in both human and K14-VEGF psoriatic skins, likely induce perpetuated disease cycle through stimulation of IL-1 production, the release of multiple cytokines and chemokines, and growth of keratinocytes and angiogenesis, as observed in psoriasis. Although many details of molecular events remain to be elucidated, it is clear that PK2 plays a prominent role in this cell signaling network. These findings also provide a molecular explanation for the observation that expression of PK2 increases following inflammation (Negri and Lattanzi, 2011). Therefore, it presents a prominent biomarker for diagnosis as well as a promising novel target for psoriasis therapeutic intervention.
Author Contributions
X.H., C.S. and Q.L. conducted a large part of the experiments including human sample analysis, cell culture, ELISA, IHC, qPCR, animal experiments, and data analysis; J.L. and Y.W. N.L for animal experiments; L.H. and R.B. collected human samples; M.R. and Z.Z helped for plasmid construction; X.H., J.Z., and R.L. participated in data analysis and prepared the manuscript; R.L. conceived and supervised the project.
Competing Financial Interests
The authors declare no competing financial interests.
Acknowledgements
This work was supported by funding from MOST (2013CB911300), NSFC (U1132601, 31200590), CAS (XDB13000000, XDA12020334, KSZD-EW-Z-007) and Yunnan Province (2012BC009).
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.ebiom.2016.10.022.
Contributor Information
Mingqiang Rong, Email: rongmingqiang@mail.kiz.ac.cn.
Ren Lai, Email: rlai@mail.kiz.ac.cn.
Appendix A. Supplementary data
Supplementary material
References
- Asahina A., Torii H., Ohtsuki M., Tokimoto T., Hase H., Tsuchiya T., Shinmura Y., Reyes Servin O., Nakagawa H. Safety and efficacy of adalimumab treatment in Japanese patients with psoriasis: results of SALSA study. J. Dermatol. 2016 doi: 10.1111/1346-8138.13409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachelez H. Immunopathogenesis of psoriasis: recent insights on the role of adaptive and innate immunity. J. Autoimmun. 2005;25:69–73. doi: 10.1016/j.jaut.2005.09.025. (Suppl.) [DOI] [PubMed] [Google Scholar]
- Baliwag J., Barnes D.H., Johnston A. Cytokines in psoriasis. Cytokine. 2015;73:342–350. doi: 10.1016/j.cyto.2014.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campanati A., Ganzetti G., Giuliodori K., Molinelli E., Offidani A. Biologic therapy in psoriasis: safety profile. Curr. Drug Saf. 2016;11:4–11. doi: 10.2174/1574886310666151014115532. [DOI] [PubMed] [Google Scholar]
- Chang L., Karin M. Mammalian MAP kinase signalling cascades. Nature. 2001;410:37–40. doi: 10.1038/35065000. [DOI] [PubMed] [Google Scholar]
- Cheng M.Y., Lee A.G., Culbertson C., Sun G., Talati R.K., Manley N.C., Li X., Zhao H., Lyons D.M., Zhou Q.Y. Prokineticin 2 is an endangering mediator of cerebral ischemic injury. Proc. Natl. Acad. Sci. U. S. A. 2012;109:5475–5480. doi: 10.1073/pnas.1113363109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong H.C., Tan M.J., Philippe V., Tan S.H., Tan C.K., Ku C.W., Goh Y.Y., Wahli W., Michalik L., Tan N.S. Regulation of epithelial-mesenchymal IL-1 signaling by PPAR beta/delta is essential for skin homeostasis and wound healing. J. Cell Biol. 2009;184:817–831. doi: 10.1083/jcb.200809028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung Y., Chang S.H., Martinez G.J., Yang X.O., Nurieva R., Kang H.S., Ma L., Watowich S.S., Jetten A.M., Tian Q. Critical regulation of early Th17 cell differentiation by interleukin-1 signaling. Immunity. 2009;30:576–587. doi: 10.1016/j.immuni.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates L.C., FitzGerald O., Helliwell P.S., Paul C. Psoriasis, psoriatic arthritis, and rheumatoid arthritis: is all inflammation the same? Semin. Arthritis Rheum. 2016 doi: 10.1016/j.semarthrit.2016.05.012. [DOI] [PubMed] [Google Scholar]
- Cooper K.D., Hammerberg C., Baadsgaard O., Elder J.T., Chan L.S., Sauder D.N., Voorhees J.J., Fisher G. IL-1 activity is reduced in psoriatic skin. Decreased IL-1 alpha and increased nonfunctional IL-1 beta. J. Immunol. 1990;144:4593–4603. [PubMed] [Google Scholar]
- Detmar M., Brown L.F., Claffey K.P., Yeo K.T., Kocher O., Jackman R.W., Berse B., Dvorak H.F. Overexpression of vascular permeability factor/vascular endothelial growth factor and its receptors in psoriasis. J. Exp. Med. 1994;180:1141–1146. doi: 10.1084/jem.180.3.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detmar M., Brown L.F., Schon M.P., Elicker B.M., Velasco P., Richard L., Fukumura D., Monsky W., Claffey K.P., Jain R.K. Increased microvascular density and enhanced leukocyte rolling and adhesion in the skin of VEGF transgenic mice. J. Investig. Dermatol. 1998;111:1–6. doi: 10.1046/j.1523-1747.1998.00262.x. [DOI] [PubMed] [Google Scholar]
- Di Meglio P., Villanova F., Nestle F.O. Psoriasis. Cold Spring Harb. Perspect. Med. 2014;4 doi: 10.1101/cshperspect.a015354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsch M., Qiu Y., Soler D., Frank N., Duong T., Goodearl A., O'Neil S., Lora J., Fraser C.C. PK1/EG-VEGF induces monocyte differentiation and activation. J. Leukoc. Biol. 2005;78:426–434. doi: 10.1189/jlb.0205061. [DOI] [PubMed] [Google Scholar]
- Finch P.W., Murphy F., Cardinale I., Krueger J.G. Altered expression of keratinocyte growth factor and its receptor in psoriasis. Am. J. Pathol. 1997;151:1619–1628. [PMC free article] [PubMed] [Google Scholar]
- Franchi S., Giannini E., Lattuada D., Lattanzi R., Tian H., Melchiorri P., Negri L., Panerai A.E., Sacerdote P. The prokineticin receptor agonist Bv8 decreases IL-10 and IL-4 production in mice splenocytes by activating prokineticin receptor-1. BMC Immunol. 2008;9:60. doi: 10.1186/1471-2172-9-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbiani G. The myofibroblast in wound healing and fibrocontractive diseases. J. Pathol. 2003;200:500–503. doi: 10.1002/path.1427. [DOI] [PubMed] [Google Scholar]
- Gottlieb A.B. Psoriasis: emerging therapeutic strategies. Nat. Rev. Drug Discov. 2005;4:19–34. doi: 10.1038/nrd1607. [DOI] [PubMed] [Google Scholar]
- Guerra I., Perez-Jeldres T., Iborra M., Algaba A., Monfort D., Calvet X., Chaparro M., Manosa M., Hinojosa E., Minguez M. Incidence, clinical characteristics, and management of psoriasis induced by anti-TNF therapy in patients with inflammatory bowel disease: a nationwide cohort study. Inflamm. Bowel Dis. 2016;22:894–901. doi: 10.1097/MIB.0000000000000757. [DOI] [PubMed] [Google Scholar]
- Gupta M.A., Simpson F.C., Gupta A.K. Psoriasis and sleep disorders: a systematic review. Sleep Med. Rev. 2015;29:63–75. doi: 10.1016/j.smrv.2015.09.003. [DOI] [PubMed] [Google Scholar]
- Johnston A., Xing X., Guzman A.M., Riblett M., Loyd C.M., Ward N.L., Wohn C., Prens E.P., Wang F., Maier L.E. IL-1F5, -F6, -F8, and -F9: a novel IL-1 family signaling system that is active in psoriasis and promotes keratinocyte antimicrobial peptide expression. J. Immunol. 2011;186:2613–2622. doi: 10.4049/jimmunol.1003162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kofoed K., Skov L., Zachariae C. New drugs and treatment targets in psoriasis. Acta Derm. Venereol. 2015;95:133–139. doi: 10.2340/00015555-1931. [DOI] [PubMed] [Google Scholar]
- Kovacs D., Falchi M., Cardinali G., Raffa S., Carducci M., Cota C., Amantea A., Torrisi M.R., Picardo M. Immunohistochemical analysis of keratinocyte growth factor and fibroblast growth factor 10 expression in psoriasis. Exp. Dermatol. 2005;14:130–137. doi: 10.1111/j.0906-6705.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- Kovacs D., Cota C., Cardinali G., Aspite N., Bolasco G., Amantea A., Torrisi M.R., Picardo M. Expression of keratinocyte growth factor and its receptor in clear cell acanthoma. Exp. Dermatol. 2006;15:762–768. doi: 10.1111/j.1600-0625.2006.00459.x. [DOI] [PubMed] [Google Scholar]
- Lande R., Gregorio J., Facchinetti V., Chatterjee B., Wang Y.H., Homey B., Cao W., Wang Y.H., Su B., Nestle F.O. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 2007;449:564–569. doi: 10.1038/nature06116. [DOI] [PubMed] [Google Scholar]
- Lattanzi R., Giannini E., Melchiorri P., Negri L. Pharmacology of BV8: a new peptide from amphibian skin. Br. J. Pharmacol. 2001;133:U26. [Google Scholar]
- Lichti U., Anders J., Yuspa S.H. Isolation and short-term culture of primary keratinocytes, hair follicle populations and dermal cells from newborn mice and keratinocytes from adult mice for in vitro analysis and for grafting to immunodeficient mice. Nat. Protoc. 2008;3:799–810. doi: 10.1038/nprot.2008.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man S.M., Kanneganti T.D. Regulation of inflammasome activation. Immunol. Rev. 2015;265:6–21. doi: 10.1111/imr.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martucci C., Franchi S., Giannini E., Tian H., Melchiorri P., Negri L., Sacerdote P. Bv8, the amphibian homologue of the mammalian prokineticins, induces a proinflammatory phenotype of mouse macrophages. Br. J. Pharmacol. 2006;147:225–234. doi: 10.1038/sj.bjp.0706467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mee J.B., Cork M.J., di Giovine F.S., Duff G.W., Groves R.W. Interleukin-1: a key inflammatory mediator in psoriasis? Cytokine. 2006;33:72–78. doi: 10.1016/j.cyto.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Menter A. Psoriasis and psoriatic arthritis overview. Am. J. Manag. Care. 2016;22:s216–s224. [PubMed] [Google Scholar]
- Mollay C., Wechselberger C., Mignogna G., Negri L., Melchiorri P., Barra D., Kreil G. Bv8, a small protein from frog skin and its homologue from snake venom induce hyperalgesia in rats. Eur. J. Pharmacol. 1999;374:189–196. doi: 10.1016/s0014-2999(99)00229-0. [DOI] [PubMed] [Google Scholar]
- Monnier J., Samson M. Prokineticins in angiogenesis and cancer. Cancer Lett. 2010;296:144–149. doi: 10.1016/j.canlet.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Morhenn V.B., Nelson T.E., Gruol D.L. The rate of wound healing is increased in psoriasis. J. Dermatol. Sci. 2013;72:87–92. doi: 10.1016/j.jdermsci.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousa S.A., O'Connor L., Davis F.B., Davis P.J. Proangiogenesis action of the thyroid hormone analog 3,5-diiodothyropropionic acid (DITPA) is initiated at the cell surface and is integrin mediated. Endocrinology. 2006;147:1602–1607. doi: 10.1210/en.2005-1390. [DOI] [PubMed] [Google Scholar]
- Mu L., Tang J., Liu H., Shen C., Rong M., Zhang Z., Lai R. A potential wound-healing-promoting peptide from salamander skin. FASEB J. 2014;28:3919–3929. doi: 10.1096/fj.13-248476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negri L., Lattanzi R. Bv8-prokineticins and their receptors: modulators of pain. Curr. Pharm. Biotechnol. 2011;12:1720–1727. doi: 10.2174/138920111798357410. [DOI] [PubMed] [Google Scholar]
- Negri L., Lattanzi R., Giannini E., De Felice M., Colucci A., Melchiorri P. Bv8, the amphibian homologue of the mammalian prokineticins, modulates ingestive behaviour in rats. Br. J. Pharmacol. 2004;142:181–191. doi: 10.1038/sj.bjp.0705686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negri L., Lattanzi R., Giannini E., Melchiorri P. Bv8/prokineticin proteins and their receptors. Life Sci. 2007;81:1103–1116. doi: 10.1016/j.lfs.2007.08.011. [DOI] [PubMed] [Google Scholar]
- Nestle F.O., Kaplan D.H., Barker J. Psoriasis. N. Engl. J. Med. 2009;361:496–509. doi: 10.1056/NEJMra0804595. [DOI] [PubMed] [Google Scholar]
- Nourshargh S., Larkin S.W., Das A., Williams T.J. Interleukin-1-induced leukocyte extravasation across rat mesenteric microvessels is mediated by platelet-activating factor. Blood. 1995;85:2553–2558. [PubMed] [Google Scholar]
- Pastore S., Lulli D., Potapovich A.I., Fidanza P., Kostyuk V.A., Dellambra E., De Luca C., Maurelli R., Korkina L.G. Differential modulation of stress-inflammation responses by plant polyphenols in cultured normal human keratinocytes and immortalized HaCaT cells. J. Dermatol. Sci. 2011;63:104–114. doi: 10.1016/j.jdermsci.2011.04.011. [DOI] [PubMed] [Google Scholar]
- Perera G.K., Di Meglio P., Nestle F.O. Psoriasis. Annu. Rev. Pathol. 2012;7:385–422. doi: 10.1146/annurev-pathol-011811-132448. [DOI] [PubMed] [Google Scholar]
- Romanowska M., al Yacoub N., Seidel H., Donandt S., Gerken H., Phillip S., Haritonova N., Artuc M., Schweiger S., Sterry W. PPARdelta enhances keratinocyte proliferation in psoriasis and induces heparin-binding EGF-like growth factor. J. Invest. Dermatol. 2008;128:110–124. doi: 10.1038/sj.jid.5700943. [DOI] [PubMed] [Google Scholar]
- Ryan C., Korman N.J., Gelfand J.M., Lim H.W., Elmets C.A., Feldman S.R., Gottlieb A.B., Koo J.Y., Lebwohl M., Leonardi C.L. Research gaps in psoriasis: opportunities for future studies. J. Am. Acad. Dermatol. 2014;70:146–167. doi: 10.1016/j.jaad.2013.08.042. [DOI] [PubMed] [Google Scholar]
- Schmuth M., Haqq C.M., Cairns W.J., Holder J.C., Dorsam S., Chang S., Lau P., Fowler A.J., Chuang G., Moser A.H. Peroxisome proliferator-activated receptor (PPAR)-beta/delta stimulates differentiation and lipid accumulation in keratinocytes. J. Invest. Dermatol. 2004;122:971–983. doi: 10.1111/j.0022-202X.2004.22412.x. [DOI] [PubMed] [Google Scholar]
- Schroder J.M. Cytokine networks in the skin. J. Investig. Dermatol. 1995;105:S20–S24. [PubMed] [Google Scholar]
- Seo M.D., Kang T.J., Lee C.H., Lee A.Y., Noh M. HaCaT keratinocytes and primary epidermal keratinocytes have different transcriptional profiles of cornified envelope-associated genes to T helper cell cytokines. Biomol. Ther. (Seoul) 2012;20:171–176. doi: 10.4062/biomolther.2012.20.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi H., Sujeebun M., Song Z. Psoriasis as a model of exaggerated, not dysregulated, wound healing presents potential therapeutic targets for enhanced tissue repair integrity and diminished scaling. Surgery. 2014;156:15–19. doi: 10.1016/j.surg.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Shojaei F., Singh M., Thompson J.D., Ferrara N. Role of Bv8 in neutrophil-dependent angiogenesis in a transgenic model of cancer progression. Proc. Natl. Acad. Sci. U. S. A. 2008;105:2640–2645. doi: 10.1073/pnas.0712185105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tohid H., Aleem D., Jackson C. Major depression and psoriasis: a psychodermatological phenomenon. Skin Pharmacol. Physiol. 2016;29:220–230. doi: 10.1159/000448122. [DOI] [PubMed] [Google Scholar]
- Villanova F., Di Meglio P., Nestle F.O. Biomarkers in psoriasis and psoriatic arthritis. Ann. Rheum. Dis. 2013;72(Suppl. 2):ii104–ii110. doi: 10.1136/annrheumdis-2012-203037. [DOI] [PubMed] [Google Scholar]
- Villasenor-Park J., Wheeler D., Grandinetti L. Psoriasis: evolving treatment for a complex disease. Cleve. Clin. J. Med. 2012;79:413–423. doi: 10.3949/ccjm.79a.11133. [DOI] [PubMed] [Google Scholar]
- Westergaard M., Henningsen J., Svendsen M.L., Johansen C., Jensen U.B., Schroder H.D., Kratchmarova I., Berge R.K., Iversen L., Bolund L. Modulation of keratinocyte gene expression and differentiation by PPAR-selective ligands and tetradecylthioacetic acid. J. Invest. Dermatol. 2001;116:702–712. doi: 10.1046/j.1523-1747.2001.01329.x. [DOI] [PubMed] [Google Scholar]
- Xia Y.P., Li B.S., Hylton D., Detmar M., Yancopoulos G.D., Rudge J.S. Transgenic delivery of VEGF to mouse skin leads to an inflammatory condition resembling human psoriasis. Blood. 2003;102:161–168. doi: 10.1182/blood-2002-12-3793. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material