Abstract
Objectives
There remains limited consensus regarding the definition and conceptual basis of exercise addiction. An understanding of the factors motivating maintenance of addictive exercise behavior is important for appropriately targeting intervention. The aims of this study were twofold: first, to establish consensus on features of an exercise addiction using Delphi methodology and second, to identify whether these features are congruous with a conceptual model of exercise addiction adapted from the Work Craving Model.
Methods
A three-round Delphi process explored the views of participants regarding the features of an exercise addiction. The participants were selected from sport and exercise relevant domains, including physicians, physiotherapists, coaches, trainers, and athletes. Suggestions meeting consensus were considered with regard to the proposed conceptual model.
Results and discussion
Sixty-three items reached consensus. There was concordance of opinion that exercising excessively is an addiction, and therefore it was appropriate to consider the suggestions in light of the addiction-based conceptual model. Statements reaching consensus were consistent with all three components of the model: learned (negative perfectionism), behavioral (obsessive–compulsive drive), and hedonic (self-worth compensation and reduction of negative affect and withdrawal).
Conclusions
Delphi methodology allowed consensus to be reached regarding the features of an exercise addiction, and these features were consistent with our hypothesized conceptual model of exercise addiction. This study is the first to have applied Delphi methodology to the exercise addiction field, and therefore introduces a novel approach to exercise addiction research that can be used as a template to stimulate future examination using this technique.
Keywords: exercise addiction, work craving, Delphi technique, perfectionism, obsessive–compulsive
Introduction
Regular exercise engagement has important implications for both physical and psychological health outcomes (Bauman, 2004; Fox, 1999), and with global increases in physical inactivity and sedentary behavior (Kohl et al., 2012), improving exercise participation and adherence is a critical focus for healthcare practitioners and policy makers alike. However, for a small percentage of the population, exercise engagement can be excessive (Monok et al., 2012; Sussman, Lisha, & Griffiths, 2011) and in some instances this can also lead to physical, psychological, and social distress.
In recent years, excessive exercise has not been described with regard to the absolute volume of exercise engaged in, but rather, the extent to which the exercise impairs functioning across other valuable life domains (e.g., in occupational and family settings) and is maintained regardless of negative consequences (Terry, Szabo, & Griffiths, 2004; Veale, 1995). While there is an agreement in the conceptualization of excessive exercise engagement as a negative behavior, there is less consensus regarding more nuanced definitions of an exercise problem. Although the existing conceptual frameworks are not entirely discrepant and describe a number of similar features, each of them approach and subsequently label the excessive exercise construct differently. Labels include obligatory exercise (Pasman & Thompson, 1988), compulsive exercise (Taranis, Touyz, & Meyer, 2011), exercise dependence (Hausenblas & Symons Downs, 2002), and exercise addiction (Terry et al., 2004).
The two terms that have been most commonly adopted are those of exercise dependence and exercise addiction, which are measured, respectively, by the Exercise Dependence Scale (EDS; Hausenblas & Symons Downs, 2002) and the Exercise Addiction Inventory (EAI; Terry et al., 2004). The EDS is based on the DSM-IV criteria for substance dependence, with scale items reflecting each of seven substance dependence criteria modified as appropriate for exercise behavior. The EAI, in contrast, is based on a modification of Brown’s (1993) components of behavioral addiction (see also Griffiths, 1996, 2005). These components share a reasonable degree of overlap with those of Hausenblas and Symons Downs (2002), and concurrent validity has been demonstrated between the two scales (Monok et al., 2012; Terry et al., 2004). However, in comparison to the multidimensionality of the construct in the former, the items of the EAI represent one addiction factor (Terry et al., 2004). Similar to the EDS, the EAI also identifies at-risk, symptomatic, and asymptomatic individuals according to the prescribed cutoff scores.
While the EDS and the EAI describe features of the problematic behavior and define exercise addiction as the presence of symptoms across components, these conceptual frameworks and their associated scales do not address, explicitly, the hypothesized factors that are operating in the maintenance of the disorder and the way in which these factors interact. Understanding which underlying factors are motivating continued engagement in destructive exercise behavior is an important key to appropriately targeting intervention. Therefore, validating an alternative measure based on a conceptual maintenance model may be a valuable addition to the existing instruments, which serve as aids for diagnosing those at-risk. Indeed, this approach has been taken by Taranis et al. (2011) in their development of the Compulsive Exercise Test (CET) to assess the core maintaining factors in compulsive exercise behavior for eating disordered populations. The CET has five subscales: (a) avoidance and rule driven behavior; (b) weight control exercise; (c) mood improvement; (d) lack of exercise enjoyment; and (e) exercise rigidity. Taranis et al. (2011) suggested that therapeutic focus on avoiding affective withdrawal and the following of exercise rules might be effective in treating compulsive exercise behaviors.
Similar to the EAI and propositions of other authors (see Berczik et al., 2012), excessive or problematic exercise may be better understood as an addictive process, and as a part of a large body of research we are, therefore, proposing an alternative hypothesis for framing problematic exercise within an addiction paradigm. In our review of behavioral addictions, we noted similarity between the work addiction or workaholism and exercise addiction fields, and particularly, that the recently developed Work Craving Model (WCM; Wojdylo, Baumann, Buczny, Owens, & Kuhl, 2013) might be suitably adapted for addictive exercise behavior. The WCM proposes that there are three core dimensions that interact in the maintenance of work addiction, labeled as work craving, that are aligned with three psychological factors that operate in the subjective experience of reward (Berridge, Robinson, & Aldridge, 2009; Wojdylo et al., 2013), and for which there is evidence of neurobiological dissociability (Berridge et al., 2009). These have been termed as “liking,” “wanting,” and “learning” (Berridge et al., 2009) and may alternatively be labeled as hedonic, compulsive, and learned or cognitive components. In the WCM, Wojdylo et al. (2013) outline an interaction between neurotic perfectionism (learned), an obsessive–compulsive drive (compulsive) and reduction of negative affect or withdrawal symptoms, and positive self-worth compensation (hedonic) in the maintenance of unhealthy work behavior.
With regard to exercise addiction, inclusion of neurotic or negative perfectionism and obsessive–compulsive behavior as central to its maintenance may be important considerations, in addition to the individual seeking to avoid negative withdrawal consequences. Both perfectionism (in its maladaptive form) and obsessive–compulsive tendencies have been frequently associated with excessive exercise behavior, including when the exercise is viewed as a primary phenomenon or when it is associated with disordered eating, for example, in hyperactive forms of anorexia nervosa (Davis & Kaptein, 2006; Davis et al., 1995; Goodwin, Haycraft, Willis, & Meyer, 2011; Gulker, Laskis, & Kuba, 2001; Hagan & Hausenblas, 2003; Shroff et al., 2006; Symons Downs, Hausenblas, & Nigg, 2004). Moreover, perfectionism and obsessive–compulsiveness are commonly implicated in other psychopathologies such as anxiety and depression (Egan, Wade, & Shafran, 2011; LaSalle et al., 2004). Further empirical and conceptual support for the inclusion of negative perfectionism, obsessive–compulsive drive, and affective components as central in our hypothesized model is beyond the scope of this paper, for which the primary objective is to present the results of a Delphi study. However, discussion of the research hypothesis is necessary for understanding the way in which these results have been presented.
Delphi methodology is a technique used to establish consensus between individuals who are informed within a particular subject area on a topic in which there has previously been little or no agreement (Dalkey & Helmer, 1963; Hasson, Keeney, & McKenna, 2000; Hsu & Sandford, 2007; Linstone & Turoff, 1975). It is now widely used across a number of domains, particularly those concerning decisions regarding policy or healthcare (Hasson et al., 2000; Hsu & Sandford, 2007; McKenna, 1994), and has recently been used in the field of substance misuse (Nutt, King, Saulsbury, & Blakemore, 2007). Given the differences in conceptualization of exercise addiction and the lack of consensus regarding the features of the problem, it may be an appropriate method to apply to questions in the exercise addiction field. To our knowledge, this study is the first to have done so, and therefore introduces a novel approach. The main objective was to establish agreement within a group of exercise practitioners and athletes on the features of an exercise problem, and second to compare these results with our hypothesized model of exercise addiction. It was predicted that the results would show agreement with the components of the model: learned (perfectionism), compulsive, and hedonic.
Methods
Study structure
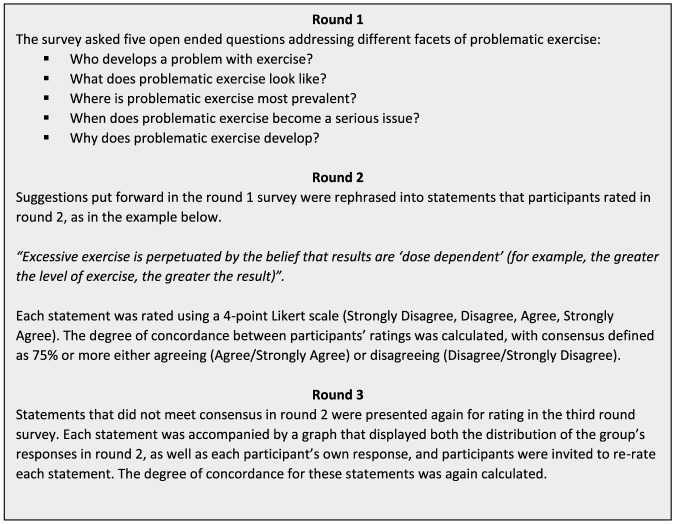
In this study, a three-round Delphi process was used (see Figure 1). In the first round, participants were asked open-ended questions designed to elicit a wide range of alternative responses and opinions. These responses were then collated by the researcher and used to generate a second round questionnaire, which comprised a series of statements that participants were asked to rank or rate according to their level of agreement. In the third round, participants were given individualized feedback showing their own responses to the statements in round 2, and the distribution of the group’s responses. At each stage, participants were free to change their opinions if they wish. The suggestions meeting consensus at the end of the third round were considered with regard to the WCM.
Figure 1.
Overview of the Delphi process
Participant selection
Panel characteristics
The representation of “expertise” is most commonly stressed in selection of participant panels for Delphi studies. However, there are no universal guidelines as to the definition of an expert (Hsu & Sandford, 2007; Keeney, Hasson, & McKenna, 2006), who are chosen dependent on the priorities of the study, and there is further contention as to whether “expertise” is truly necessary. A critical examination of the method by Goodman (1987, p. 732) states that “it would therefore seem to be more appropriate to recruit individuals who have knowledge of a particular topic and who are consequently willing to engage in discussion upon it without the potentially misleading title of “expert.” The results would then represent that particular group’s opinions at a given point in time.”
In this study, we wished to represent the opinions of a group of participants who are involved in daily practice across various domains in sport and exercise, including physicians, physiotherapists, coaches, trainers, and exercisers/athletes themselves, and who were willing to discuss the topic. Given that these individuals see many and varied exercisers, and often establish relationships with exercisers across time, we assumed that this would render them capable of discerning differences in the exercisers they see and detecting features they believed to differentiate “normal” and “problematic” patterns of exercise, despite a lack of nominal specialty or “expertise” in exercise addiction. Some heterogeneity in the panel was desired both to reflect the multifaceted nature of an exercise addiction, and due to suggestion that panel members with different perspectives may produce a higher quality result (Delbecq, Van de Ven, & Gustafson, 1975; Powell, 2003).
Selection criteria for participants identified in practitioner roles were to be currently practicing in a sport- and exercise-related field, and to have a minimum of 10 years’ experience in a sport and exercise position. No criteria was applied to athletes other than regular training and/or competition, as representing exercise from both a high performance and recreational perspective was desired.
Panel size and recruitment
Size of the participant panel for Delphi studies is also highly variable. While the greater the number of participants in the group the greater the assumed reliability of the judgments made by that group, there is little empirical evidence available on the effect participant number actually has on the reliability or validity of the process (Murphy et al., 1998). Moreover, large group numbers can introduce difficulties in data collection and management (Hasson et al., 2000; Hsu & Sandford, 2007). Hasson et al. (2000) describe studies as having employed from 15 to over 60 participants, and Clayton (1997) suggests that, as a rule of thumb, homogeneous panels should include 15–30 participants and heterogeneous panels 5–10 participants.
Nineteen individuals were approached and invited to take part in the study via email (physiotherapists, 5; sports psychologists, 2; sports physicians, 5; personal trainers, 3; high performance coaches, 2; and athletes, 3). One participant was both a physiotherapist and personal trainer, and has been recorded under the numbers for both types of role. Prospective participants were sent a brief introductory email and participant information sheet with an invitation to participate to the email addresses supplied with their public profiles. Twelve responses were received in total; two practitioners declined to take part on the basis of work and travel commitments (two physiotherapists), and the other 10 agreed to participate in the study. Participant demographics are shown in Table 1.
Table 1.
Participant demographics
| Participants (n = 10) | |
| Age, mean (range) | 41.8 years (23–64) |
| Gender | |
| Male | 5 |
| Female | 5 |
| Rolea | |
| Sports physician | 2 |
| Physiotherapist | 2 |
| Coach | 2 |
| Personal trainer | 2 |
| Athlete | 3 |
| Time in sports- and exercise-related field (professional roles), mean (range) | 21.9 years (10–41) |
| Time in current role (professional roles), mean (range) | 11.4 years (11 months–40 years) |
| Time in current sport (athletes), mean (range) | 5.1 years (1–13) |
Note that the total number of participants by role is 11, as one participant was both a physiotherapist and a personal trainer.
Data collection and analysis
Qualtrics survey software was used for the design and distribution of all questionnaires online, and all participants were given a code that made their answers identifiable to the researcher across questionnaire rounds. Participants were asked to complete each questionnaire within 2 weeks.
Round 1 questionnaire
In the first round questionnaire, five open-ended questions addressing different facets of the issue were posed. At the end of the five questions, a blank space was provided for any further comments or information participants wished to put forward.
All answers received by participants in the first round were coded according to their explicit content, and similar suggestions were collapsed into one statement that retained the intended meaning. Where there was any uncertainty about whether the comments were referring to the same thing, or there was a subtle difference, comments were kept as separate statements. As far as possible, participants’ own wording was preserved in the statements; wording was changed only if sentences had been incomplete or it was necessary to rewrite for semantic clarity for the other participants.
Round 2 questionnaire
The second round questionnaire comprised 70 statements generated from the answers and comments provided by the participants in the first round. Space was also provided below each statement for any further comments participants wished to make. Participant ratings were entered into SPSS data analysis software and the frequency of each level of rating for each statement was calculated.
Round 3 questionnaire
The third round questionnaire comprised 13 statements that had not met consensus in the second round. Consensus was defined as either agreement (agree or strongly agree) or disagreement (disagree or strongly disagree) by 75% of participants.
There is no set level for consensus in Delphi studies, with the level selected by the researcher depending on the number of participants and the priorities of the study (Hasson et al., 2000; Keeney et al., 2006). In this study, 75% was chosen to reflect the smaller overall number of participants, and the desire to represent the panel’s views as accurately as possible. Because two participants dropped out of the study between the first and second rounds (prior to any rating of their agreement), 75% accounted for six of the eight remaining participants.
For each of the 13 statements, a graph was prepared that displayed the distribution of the group’s responses for that statement in the previous round. Each participant received an individualized questionnaire with the 13 statements repeated, accompanied by the graph for that statement that had their own previous answer highlighted. This visual display was chosen so that participants could easily see how they answered in relation to others in the group. Comments that had been made regarding each of these statements in the second round were also presented beneath the graph.
Participants were asked to consider their previous answers in light of the group’s responses and the comments that had been made, and again rate their level of agreement with the statements. If they wished to, they could change their answers and make any further comments. When the third round questionnaires were received, participants’ ratings for each of the 13 statements were again entered into SPSS and the frequency of each response calculated to identify any that had now reached consensus.
Ethics
The ethical approval for the study was granted by the University of Auckland Human Participants Ethics Committee (014119). All participants received information about the study and provided their consent.
Results
Round 1 results
Ten participants completed the first round questionnaire, responding to the five open-ended questions put forward. Table 2 summarizes the suggestions made. Suggestions were categorized into weight and eating; age; external pressure, advice and information; self-related; mood and mental health; physical health and rest; and other. The responses produced 70 statements that were rated in the second round.
Table 2.
Summary of suggestions made in round 1
| Mood/mental health | Weight and eating | Age | External | Physical health | Self-related | Other |
| An addiction | Exist without concurrent eating disorder | Children multiple sports at high level | Coaches – performance ahead of health | Inability to take rest days when necessary | Belief results dose dependent | More prevalent bigger cities |
| Upset if miss/rearrange a workout | Lose/control weight | Changes in physical capabilities with age | Non-adherence prescribed exercise | Relative energy deficiency/low EA | “One size fits all” approach | Most common high performance sport |
| Rigidity – exercise plans | Accompanied by eating issues | Puberty time of risk | Inadequate support for those in field | Physical ill health – illness/injury | Identity | Strength/skill not sufficient for demand level |
| Fear circumstances that prevent training | Pressure to meet weight category | Middle age time of risk | Focus on immediate not long-term development | Burnout | Unrealistic self-expectations | More common in girls/women than in boys/men |
| Predisposition to obsessive behavior | Low body fat, skinny/unhealthy | Common in young teenage athletes | Pressure – parents and coaches | Not completing rehab | Strongly goal focused | Use of PEDs |
| Obsessive thinking – training and/or diet | Men/muscle mass at gym | Self-prescribed exercise regimes | Returning before injury healed | Compensation – fear of not trying hard enough | Fewer talents in non-physical activities | |
| Anxiety if unable to exercise | Not listening to professional advice | Preconceived idea – “right” level of exercise | ||||
| Guilt if miss/change planned workout | Extreme trends, e.g., Crossfit | Increase self-worth | ||||
| Satisfy exercise need/craving | Unrealistic expectations from others | Perfectionists | ||||
| Addicted to training effect | Current gym/fitness culture | Think not fit enough | ||||
| Difficult mood without workout | Weight loss pressure, e.g., doctor | High achievers other areas, e.g., academic | ||||
| Think persistently about next exercise session | Difficult to identify | Highly competitive individuals | ||||
| Withdrawal symptoms | Lack of adequate information/consultation | |||||
| Trained hard in the past, e.g., former athletes | ||||||
| No longer enjoyable | ||||||
| Mood changes | ||||||
| Poor body image | ||||||
| Maintain positive reinforcement | ||||||
| Push hard to feel satisfied | ||||||
| Lose control – volume, frequency, intensity | ||||||
| Depression | ||||||
| Develops from habit |
Note. EA: energy availability, PED: performance enhancing drug.
Round 2 results
Eight of the ten participants completed the second round questionnaire at an attrition rate of 20%. Of the 70 statements, 57 (81%) reached consensus, with 75% or more of the participants showing either agreement or disagreement. The 13 statements that did not reach consensus were rated again in the third round.
Round 3 results
All eight participants who had completed the second round also completed the third round questionnaire. A further 6 of the 13 statements reached consensus at this point, to give consensus overall on 63 of the 70 original statements (90%). Table 3 summarizes the overall concordance levels for all 70 statements at the end of the third and final rounds.
Table 3.
Overall concordance on all statements after final round 3 rating
| Non-consensus (<75% concordance) | Consensus (≥75% concordance) | ||||||
| % Agree/Disagree | % Disagree (strongly)a | % Agree (strongly)a | |||||
| Common in young teenage athletes | 62.5/37.5 | More prevalent bigger cities | 75.0 (33.3) | Inability to take rest days when necessary | 100.0 (50.0) | Compensation – fear of not trying hard enough | 87.5 (14.3) |
| More common in girls/women than in boys/men | 37.5/62.5 | Most common high performance sport | 75.0 (33.3) | Belief results dose dependent | 100.0 (50.0) | Poor body image | 87.5 (0.0) |
| Use of PEDs | 50.0/50.0 | Not completing rehab | 75.0 (0.0) | “One size fits all” approach | 100.0 (50.0) | Mood changes | 87.5 (0.0) |
| Fewer talents in non-physical activities | 50.0/50.0 | Returning before injury healed | 75.0 (0.0) | An addiction | 100.0 (37.5) | Maintain positive reinforcement | 87.5 (0.0) |
| Highly competitive individuals | 50.0/50.0 | Weight loss pressure, e.g., doctor | 75.0 (0.0) | Upset if miss/rearrange workout | 100.0 (37.5) | Difficult to identify | 87.5 (0.0) |
| Low body fat, skinny/unhealthy | 50.0/50.0 | Rigidity – exercise plans | 100.0 (37.5) | Inadequate support for those in field | 87.5 (0.0) | ||
| Men, muscle mass at gym | 50.0/50.0 | Fear circumstances that prevent training | 100.0 (37.5) | Focus on immediate not long term development | 75.0 (66.7) | ||
| Identity | 100.0 (37.5) | Burnout | 75.0 (50.0) | ||||
| Predisposition to obsessive behavior | 100.0 (25.0) | Preconceived idea – “right” level of exercise | 75.0 (50.0) | ||||
| Obsessive thinking – training and/or diet | 100.0 (25.0) | Increase self-worth | 75.0 (50.0) | ||||
| Relative energy deficiency/low EA | 100.0 (25.0) | Push hard to feel satisfied | 75.0 (50.0) | ||||
| Anxiety if unable to exercise | 100.0 (12.5) | Not listening to professional advice | 75.0 (33.3) | ||||
| Physical ill health – illness/injury | 87.5 (71.4) | Self-prescribed exercise regimes | 75.0 (33.3) | ||||
| Guilt if miss/change planned workout | 87.5 (57.1) | Pressure – parents and coaches | 75.0 (33.3) | ||||
| Unrealistic self-expectations | 87.5 (57.1) | Children multiple sports at high level | 75.0 (33.3) | ||||
| Exist without concurrent eating disorder | 87.5 (42.9) | Accompanied by eating issues | 75.0 (33.3) | ||||
| Strongly goal-focused | 87.5 (42.9) | Extreme trends, e.g., Crossfit | 75.0 (16.7) | ||||
| Satisfy exercise need/craving | 87.5 (28.6) | Unrealistic expectations from others | 75.0 (16.7) | ||||
| Addicted to training effect | 87.5 (28.6) | Trained hard in past, e.g., former athletes | 75.0 (16.7) | ||||
| Difficult mood without workout | 87.5 (28.6) | No longer enjoyable | 75.0 (16.7) | ||||
| Lose/control weight | 87.5 (28.6) | Depression | 75.0 (16.7) | ||||
| Think persistently about next exercise session | 87.5 (14.3) | Lack of adequate information/consultation | 75.0 (16.7) | ||||
| Withdrawal symptoms | 87.5 (14.3) | Changes in physical capabilities with age | 75.0 (16.7) | ||||
| Lose control – volume, frequency, intensity | 87.5 (14.3) | Puberty time of risk | 75.0 (16.7) | ||||
| Coaches – performance ahead of health | 87.5 (14.3) | Perfectionists | 75.0 (16.7) | ||||
| High achievers other areas, e.g., academic | 87.5 (14.3) | Strength/skill level not sufficient for demand level | 75.0 (16.7) | ||||
| Non-adherence prescribed exercise | 87.5 (14.3) | Current gym/fitness culture | 75.0 (0.0) | ||||
| Middle age time of risk | 75.0 (0.0) | ||||||
| Think not fit enough | 75.0 (0.0) | ||||||
| Develops from habit | 75.0 (0.0) | ||||||
| Pressure to meet weight category | 75.0 (0.0) | ||||||
Note. EA: energy availability, PED: performance enhancing drug.
Overall degree of concordance (percentage of the consensus strongly disagreeing/strongly agreeing).
Discussion
The Delphi process allowed consensus to be reached between experienced sports and exercise practitioners and athletes regarding the features of an exercise addiction. Our main hypothesis was that the features identified by participants in the study would be congruous with components of the WCM, which we are proposing as suitable for adaptation as a conceptual model of the factors maintaining exercise addiction. The results lent support to this hypothesis across all components of the model (learned, behavioral, and hedonic) and are discussed in relation to these components below.
Terminology and definition have been the major points of discrepancy regarding the excessive exercise construct. Therefore, the complete concordance of participants’ opinion that excessive exercise is an addiction, and accordingly that it is appropriate to conceptualize it in this way, was an important finding prior to considering the results in light of the WCM, which adheres to an addiction paradigm.
Learned (cognitive) component: Negative perfectionism
Participants identified perfectionism as being one of the characteristics of individuals who exercise excessively, and further identified thoughts and behavior that most closely describe a neurotic or negative form of perfectionism. Negative perfectionistic behavior is that which is maintained by negative reinforcement and is pathological in nature (Slade & Owens, 1998). Comments regarding unrealistic self-expectations, a strong goal focus, and compensation for a fear of not trying hard enough or being dedicated enough to a chosen sport or exercise goal resemble this type of behavioral motivation. Furthermore, it is possible that perceived pressure from coaches and parents, and the implied desire to avoid the disapproval that comes from not meeting the expectations of others, also correspond to a (socially oriented) negative perfectionistic behavioral style. Because perfectionistic excess may be more likely in those activities that have some intrinsic social value, this manifestation may make sense in light of the current fitness culture.
Behavioral component: Obsessive–compulsive drive
A number of statements for which there was concordance were also consistent with an underlying compulsivity or obsessive–compulsive drive. These included an inability to take rest days even when rest was demanded, being unable to give up the effects of training or needing exercise to “feel right” (e.g., as a former athlete), needing to satisfy a craving for exercise, showing rigidity around exercise plans, exercise no longer being enjoyable, and excessive exercise as a habitual behavior. There was also agreement that individuals who develop an exercise addiction may have a predisposition toward obsessive behavior. Compulsivity has been well documented in relation to excessive exercise (e.g., Davis et al., 1995; Gulker et al., 2001) and indeed, these comments are not dissimilar to the compulsivity described by Taranis et al. (2011) as one of the maintaining factors of excessive exercise in eating disordered populations. The comments are also consistent with the documentation of compulsivity within the workaholism literature (e.g., Schaufeli, Shimazu, & Taris, 2009; Wojdylo et al., 2013), suggesting that although not sufficient alone as a description for the motivation underlying behavioral addiction, compulsivity is a necessary feature of a robust conceptual framework.
Hedonic component: Self-worth compensation and reduction of negative affect and withdrawal
The hedonic component of the WCM includes both the anticipation of compensation for feelings of low self-worth, and the minimization of negative affect and withdrawal that results from not engaging in the behavior. Participants agreed that excessive exercise is related to a desire to increase feelings of self-worth, and that excessive exercise behavior may be attributed in part to maintaining positive reinforcement that has resulted from exercise in the past (e.g., feeling good about the results or attention). That is, the results support the idea that excessive exercisers may be validating their self-worth through the positive response received for exercise derived results. Negative affect and withdrawal symptoms when unable to exercise featured predominantly in participants’ suggestions. These included having a fear of circumstances that prevent training, feeling upset, guilty, and anxious when having to miss or change planned exercise sessions, and changes in mood such as a difficult mood prior to completing daily workouts. It is reasonable to assume, therefore, that the continued pattern of exercise is, at least in part, to alleviate the anticipated affective withdrawal symptoms.
Additional findings
There was a strong consensus that excessive exercise can exist without a concurrent eating disorder; that is, that it can be a primary phenomenon (De Coverley Veale, 1987; Veale, 1995). However, there was also consensus regarding eating- and weight-related suggestions (e.g., that excessive exercise is used as a means to lose or control weight, and accompanied by eating-related issues such as restricted caloric intake). Much debate has centered on the primary/secondary distinction, and some authors (e.g., Bamber, Cockerill, & Carroll, 2000) have highlighted the lack of empirical evidence for excessive exercise in the absence of eating psychopathology. We agree that more empirical evidence is needed before conclusions can be drawn regarding excessive exercise as an independent phenomenon, and there is likely a considerable degree of overlap between eating and exercise pathology. There is, however, evidence suggesting that high levels of physical activity may precede the development of eating disorder symptoms (see Davis, Blackmore, Katzman, & Fox, 2005). As such, a comprehensive model of the motivation for exercise addiction may have utility irrespective of whether the two can be teased apart, and it is possible that the underlying motivational bases for exercise and eating symptoms are not discrepant.
Participant selection
There are different groups of people who may be appropriate to consult in a Delphi process that explores the features of an exercise addiction. Although perhaps a less considered group, exercise-related practitioners have informative and valid insights to offer because these practitioners establish relationships with a wide variety of exercisers on a consistent basis, and those who have a “problem” do not necessarily present for specialist treatment (Veale, 1995). In fact, denial or lack of recognition or acknowledgment of an issue may be common, especially if the excessive exercise behavior holds some value for the individual. However, excessive exercisers may be likely to seek treatment for related issues (whether biomechanical or medical), to engage the services of a specialist trainer, or have a coach monitoring their performance, and as such practitioners in these positions are ideally situated for identifying differences in patterns of exercise behavior. In this sense, they may be viewed as an important interface between scholarship and practice.
Limitations
Delphi methodology is time intensive on behalf of the participants, and therefore both initial recruitment and participation maintenance can be challenging. The sample size in this study was small, and it would be of benefit in future studies to recruit a larger number of individuals to ensure depth and any diversity arising in their responses. However, it has been suggested that sample size may not be the major concern in Delphi studies, and that comparable reliability may be obtained for both fewer and larger numbers of participants (Murphy et al., 1998). Moreover, too many participants may introduce additional difficulties in group interaction and data collection and management (Hasson et al., 2000; Hsu & Sandford, 2007; Murphy et al., 1998).
Selection of the “expert” panel is also a key aspect of Delphi methodology, and there are some limitations inherent in the sample that we selected. Exercise professionals were defined as those who had a minimum of 10 years’ experience in the sport and exercise field across their respective domains. They were not, however, specialists in exercise addiction per se. Exercise addiction is a multifaceted issue; and the participants were chosen across domains in which symptomatic individuals may present for different reasons. Nevertheless, it is possible that their explicit familiarity and involvement with the problem were not sufficient. There are alternative ways by more specific expertise in exercise addiction could be obtained: by sampling academics who are actively researching and publishing in the area, or by sampling professionals who are specialists in the treatment of the problem or similar problems (e.g., a clinical psychologist who specializes in disordered eating and exercise). Both approaches would be worthwhile for future studies, and there may be some overlap in the participants for these two types of panels. However, as discussed regarding the participant selection above, there is also utility in repetition of the study with a participant panel similar to the one used here, to confirm whether these results are generalizable beyond the present scope. A further alternative would be to employ Delphi methodology in a sample that includes all of the aforementioned participants in the expert panel: (a) academics; (b) practicing psychologists, and across-domain exercise practitioners; and (c) to systematically compare and contrast any group differences in opinion.
The terminology we used may also have resulted in some confusion. “Problematic exercise” rather than “exercise addiction” was initially used to avoid any assumptions of addiction prior to the participants’ own explicit statement of this idea. However, it may have led to different interpretations of the intended construct, and future studies may be better to use the term addiction and pose a working definition, against which opinion can be elicited.
Despite these limitations, and acknowledgment that the conclusions can pertain only to our particular participant group; to our knowledge, this study is the first to employ Delphi methodology in this field. Therefore, it provides a valuable template to stimulate further research using a similar approach.
Conclusions
The Delphi process showed the features of an addictive exercise pattern that are salient for sports and exercise practitioners and athletes, and these features aligned well with our hypothesized conceptual model of exercise addiction. Delphi methodology is appropriate for use in areas where agreement has been limited, and prior to this study had not yet been applied to the exercise addiction field. Therefore, the study introduces a novel approach to the examination of exercise addiction, and provides a template to stimulate future research using the technique.
Authors’ contribution
LM: Study concept and design, analysis and interpretation of data, and manuscript preparation; GO: Study concept and design and manuscript preparation; BdPC: Manuscript preparation. All authors have reviewed and approved the submitted version of the manuscript. The first author only had full access to the data and takes responsibility for the integrity of the data and data analysis.
Conflict of interest
The authors declare no conflict of interest.
Funding Statement
Funding sources: No financial support was received for this study.
References
- Bamber D., Cockerill I. M., Carroll D. (2000). The pathological status of exercise dependence. British Journal of Sports Medicine, 34(2), 125–132. doi:10.1136/bjsm.34.2.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman A. E. (2004). Updating the evidence that physical activity is good for health: An epidemiological review 2000–2003. Journal of Science and Medicine in Sport, 7(1), 6–19. doi:10.1016/S1440-2440(04)80273-1 [DOI] [PubMed] [Google Scholar]
- Berczik K., Szabo A., Griffiths M. D., Kurimay T., Kun B., Urban R., Demetrovics Z. (2012). Exercise addiction: Symptoms, diagnosis, epidemiology, and etiology. Substance Use and Misuse, 47, 403–417. doi:10.3109/10826084.2011.639120 [DOI] [PubMed] [Google Scholar]
- Berridge K. C., Robinson T. E., Aldridge J. W. (2009). Dissecting components of reward: ‘Liking’, ‘wanting’ and learning. Current Opinion in Pharmacology, 9(1), 65–73. doi:10.1016/j.coph.2008.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. I. F. (1993). Some contributions of the study of gambling to the study of other addictions In Eadington W. R., Cornelius J. (Eds.), Gambling behaviour and problem gambling (pp. 241–272). Reno, NV: University of Nevada Press. [Google Scholar]
- Clayton M. J. (1997). Delphi: A technique to harness expert opinion for critical decision-making tasks in education. Educational Psychology, 17(4), 373–386. doi:10.1080/0144341970170401 [Google Scholar]
- Dalkey N., Helmer O. (1963). An experimental application of the Delphi method to the use of experts. Management Science, 9(3), 458–467. doi:10.1287/mnsc.9.3.458 [Google Scholar]
- Davis C., Blackmore E., Katzman D. K., Fox J. (2005). Female adolescents with anorexia nervosa and their parents: A case-control study of exercise attitudes and behaviours. Psychological Medicine, 35, 377–386. doi:10.1017/S0033291704003447 [DOI] [PubMed] [Google Scholar]
- Davis C., Kaptein S. (2006). Anorexia nervosa with excessive exercise: A phenotype with close links to obsessive-compulsive disorder. Psychiatry Research, 142, 209–217. doi:10.1016/j.psychres.2005.11.006 [DOI] [PubMed] [Google Scholar]
- Davis C., Kennedy S. H., Ralevski E., Dionne M., Brewer H., Neitzert C., Ratusny D. (1995). Obsessive compulsiveness and physical activity in anorexia nervosa and high-level exercising. Journal of Psychosomatic Research, 39(8), 967–976. doi:10.1016/0022-3999(95)00064-X [DOI] [PubMed] [Google Scholar]
- De Coverley Veale D. M. W. (1987). Exercise dependence. British Journal of Addiction, 82, 735–740. doi:10.1111/j.1360-0443.1987.tb01539.x [DOI] [PubMed] [Google Scholar]
- Delbecq A. L., Van de Ven A. H., Gustafson D. H. (1975). Group techniques for program planning: A guide to nominal group and Delphi processes. Glenview, IL: Scott Foresman. [Google Scholar]
- Egan S. J., Wade T. D., Shafran R. (2011). Perfectionism as a transdiagnostic process: A clinical review. Clinical Psychology Review, 31, 203–212. doi:10.1016/j.cpr.2010.04.009 [DOI] [PubMed] [Google Scholar]
- Fox K. R. (1999). The influence of physical activity on mental well-being. Public Health Nutrition, 2(3a), 411–418. doi:10.1017/S1368980099000567 [DOI] [PubMed] [Google Scholar]
- Goodman C. M. (1987). The Delphi technique: A critique. Journal of Advanced Nursing, 12, 729–734. doi:10.1111/j.1365-2648.1987.tb01376.x [DOI] [PubMed] [Google Scholar]
- Goodwin H., Haycraft E., Willis A., Meyer C. (2011). Compulsive exercise: The role of personality, psychological morbidity, and disordered eating. International Journal of Eating Disorders, 44, 655–660. doi:10.1002/eat.20902 [DOI] [PubMed] [Google Scholar]
- Griffiths M. (1996). Behavioural addiction: An issue for everybody? Employee Counselling Today, 8(3), 19–25. doi:10.1108/13665629610116872 [Google Scholar]
- Griffiths M. (2005). A ‘components’ model of addiction within a biopsychosocial framework. Journal of Substance Use, 10(4), 191–197. doi:10.1080/14659890500114359 [Google Scholar]
- Gulker M. G., Laskis T. A., Kuba S. A. (2001). Do excessive exercisers have a higher rate of obsessive-compulsive symptomatology? Psychology, Health and Medicine, 6(4), 387–398. doi:10.1080/13548500126535 [Google Scholar]
- Hagan A. L., Hausenblas H. A. (2003). The relationship between exercise dependence symptoms and perfectionism. American Journal of Health Studies, 18(2–3), 133–137. [Google Scholar]
- Hasson F., Keeney S., McKenna H. (2000). Research guidelines for the Delphi survey technique. Advanced Journal of Nursing, 32(4), 1008–1015. doi:10.1046/j.1365-2648.2000.t01-1-01567.x [PubMed] [Google Scholar]
- Hausenblas H. A., Symons Downs D. (2002). How much is too much? The development and validation of the exercise dependence scale. Psychology and Health, 17(4), 387–404. doi:10.1080/0887044022000004894 [Google Scholar]
- Hsu C.-C., Sandford B. A. (2007). The Delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation, 12(10), 1–8. [Google Scholar]
- Keeney S., Hasson F., McKenna H. (2006). Consulting the oracle: Ten lessons from using the Delphi technique in nursing research. Journal of Advanced Nursing, 53(2), 205–212. doi:10.1111/jan.2006.53.issue-2 [DOI] [PubMed] [Google Scholar]
- Kohl H. W., Craig C. L., Lambert E. V., Inoue S., Alkandari J. R., Leetongin G., Kahlmeier S. (2012). The pandemic of physical inactivity: Global action for public health. The Lancet, 380, 294–305. doi:10.1016/S0140-6736(12)60898-8 [DOI] [PubMed] [Google Scholar]
- LaSalle V. H., Cromer K. R., Nelson K. N., Kazuba D., Justement L., Murphy D. L. (2005). Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive-compulsive disorder. Depression and Anxiety, 19, 163–173. doi:10.1002/da.20009 [DOI] [PubMed] [Google Scholar]
- Linstone H. A., Turoff M. (1975). The Delphi method: Techniques and applications. Reading, MA: Addison-Wesley. [Google Scholar]
- McKenna H. P. (1994). The Delphi technique: A worthwhile research approach for nursing? Journal of Advanced Nursing, 19, 1221–1225. doi:10.1111/j.1365-2648.1994.tb01207.x [DOI] [PubMed] [Google Scholar]
- Monok K., Berczik K., Urban R., Szabo A., Griffiths M. D., Farkas J., Magi A., Eisinger A., Kurimay T., Kökönyei G., Kun B. (2012). Psychometric properties and concurrent validity of two exercise addiction measures: A population wide study. Psychology of Sport and Exercise, 13, 739–746. doi: 10.1016/j.psychsport.2012.06.003 [Google Scholar]
- Murphy M. K., Black N., Lamping D. L., McKee C. M., Sanderson C. F. B., Askham J. (1998). Consensus development methods and their use in clinical guideline development. Health Technology Assessment, 2(3), 31–38. doi:10.3310/hta2030 [PubMed] [Google Scholar]
- Nutt D., King L. A., Saulsbury W., Blakemore C. (2007). Development of a rational scale to assess the harm of drugs of potential misuse. The Lancet, 369, 1047–1053. doi:10.1016/S0140-6736(07)60464-4 [DOI] [PubMed] [Google Scholar]
- Pasman L., Thompson J. K. (1988). Body image and eating disturbance in obligatory runners, obligatory weight lifters, and sedentary individuals. International Journal of Eating Disorders, 7(6), 759–769. doi:10.1002/1098-108X(198811)7:6<759::AID-EAT2260070605>3.0.CO;2-G [Google Scholar]
- Powell C. (2003). The Delphi technique: Myths and realities. Journal of Advanced Nursing, 41(4), 376–382. doi:10.1046/j.1365-2648.2003.02537.x [DOI] [PubMed] [Google Scholar]
- Schaufeli W. B., Shimazu A., Taris T. W. (2009). Being driven to work excessively hard. The evaluation of a two-factor measure of workaholism in the Netherlands and Japan. Cross Cultural Research, 43, 320–348. doi:10.1177/1069397109337239 [Google Scholar]
- Shroff H., Reba L., Thornton L. M., Tozzi F., Klump K. L., Berrettini W. H., Brandt H., Crawford S., Crow S., Fichter M. M., Goldman D., Halmi K. A., Johnson C., Kaplan A. S., Keel P., LaVia M., Mitchell J., Rotondo A., Strober M., Treasure J., Woodside D. B., Kaye W. H., Bulik C. M. (2006). Features associated with excessive exercise in women with eating disorders. International Journal of Eating Disorders, 39, 454–461. doi:10.1002/eat.20247 [DOI] [PubMed] [Google Scholar]
- Slade P. D., Owens R. G. (1998). A dual process model of perfectionism based on reinforcement theory. Behaviour Modification, 22(3), 372–390. doi:10.1177/01454455980223010 [DOI] [PubMed] [Google Scholar]
- Sussman S., Lisha N., Griffiths M. (2011). Prevalence of the addictions: A problem of the majority or the minority? Evaluation and the Health Professions, 34(1), 3–56. doi:10.1177/0163278710380124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symons Downs D., Hausenblas H. A., Nigg C. R. (2004). Factorial validity and psychometric examination of the exercise dependence scale-revised. Measurement in Physical Education and Exercise Science, 8(4), 183–201. doi:10.1207/s15327841mpee0804_1 [Google Scholar]
- Taranis L., Touyz S., Meyer C. (2011). Disordered eating and exercise: Development and preliminary validation of the compulsive exercise test (CET). European Eating Disorders Review, 19, 256–268. doi:10.1002/erv.1108 [DOI] [PubMed] [Google Scholar]
- Terry A., Szabo A., Griffiths M. (2004). The exercise addiction inventory: A new brief screening tool. Addiction Research and Theory, 12(5), 489–499. doi:10.1080/16066350310001637363 [Google Scholar]
- Veale D. (1995). Does primary exercise dependence really exist? In Annett J., Cripps B., Steinberg H. (Eds.), Exercise addiction: Motivation for participation in sport and exercise (pp. 1–5). Leicester, UK: British Psychological Society. [Google Scholar]
- Wojdylo K., Baumann N., Buczny J., Owens G., Kuhl J. (2013). Work craving: A conceptualisation and measurement. Basic and Applied Social Psychology, 35(6), 547–568. doi:10.1080/01973533.2013.840631 [Google Scholar]