Abstract
Background
Mucocutaneous leishmaniasis (MCL), a protozoan infectious disease, is very rare in Iran despite the endemicity of both cutaneous and visceral forms. It is transmitted by the Phlebotomus sand fly. The lip is considered one of the extraordinary sites. Lesions usually initiate with erythematous papules, slowly enlarges and then it ulcerates. The diagnosis of MCL encompasses epidemiological, clinical and laboratory aspects. Usually, the combination of some of these elements is necessary for the final diagnosis. So, lip leishmaniasis lesions can be challenging to diagnose.
Case presentation
We presented seven rare cases of lip leishmaniasis. Tissue impression smear, culture, PCR and phylogenetic analysis were carried out for explicit diagnosis. Skin scraping investigation showed several Leishmania spp. amastigotes in the cytoplasm of macrophages. Culture examination was positive for Leishmania spp. PCR was positive for L. major, L. tropica, and L. infantum. Differential diagnosis includes orofacial granulomatosis, basal cell carcinoma, squamous cell carcinoma, and mesenchymal tumors. The cases were treated with systemic meglumine antimoniate (Glucantime®). No relapses were observed during 1 year of follow-up. Early detection of the infection are necessary in order to start effective treatment and prevent more serious complications.
Conclusions
In this paper, we reported seven rare cases of lip leishmaniasis in Iran, emphasized the importance of clinical and diagnostic features of lesions, characterized the phylogenetic kinship of isolated parasites, and reviewed the literature on lip leishmaniasis.
Keywords: Mucosal leishmaniasis, Case report, Lip, PCR, Phylogenetic analysis, Iran
Background
Leishmaniasis is a group of infectious disease, caused by protozoan parasites belonging to the genus Leishmania (order Kinetoplastida). It is transmitted by sand flies of Phlebotomus and Lutzomyia species. Reservoirs are represented by a wide range of mammals, and more rarely, humans [1].
Leishmaniases present a wide spectrum of clinical manifestations including cutaneous (CL), diffuse cutaneous (DCL), mucocutaneous (MCL), and visceral leishmaniasis (VL) [1]. CL is endemic in half of the 31 provinces of Iran, and is a great health problem [2].
From the clinical vista, CL is characterized by skin lesions that vary in presentation from papules to plaques to ulcers. These lesions can cause varying amounts of scarring depending on the number and size of lesions [3]. Although localized lymphadenopathy may be present in the area of the cutaneous lesion, systemic complications from this form of leishmaniasis are rare [3].
MCL is characterized by the scatter of skin ulcers to encompassing tissues, specifically inner nostril wall to larynx and mouth [3]. Moreover, there may be cases in which the MCL would be seen without cutaneous lesions. In fact, in 30% of MCL cases, patients do not recall the presence of a primary cutaneous lesion [3]. Primary mucosal leishmaniasis is very rare in Iran in spite of high prevalence of cutaneous and visceral forms. The lip involvement is very rare and may imitate orofacial granulomatosis such as Crohn’s disease, sarcoidosis, foreign body giant cell granuloma and Melkersson-Rosenthal syndrome [4]. Other differential diagnosis includes basal cell carcinoma, squamous cell carcinoma, mesenchymal tumors, and mycotic infections. Because of its heterogeneous and underestimated clinical presentation [5, 6], MCL is often perplexed and remains a diagnostic challenge for the clinicians and scientists.
The diagnosis of MCL includes epidemiological, clinical and laboratory aspects. Generally, the combination of some of these constituents is necessary for the final diagnosis [7]. Unfortunately, delayed diagnosis and the lack of consensus on optimal treatment can frequently lead to inappropriate management of the disease [8].
In this report, we presented seven rare cases of lip leishmaniasis in Iran, emphasized the importance of clinical and diagnostic features of lesions, characterized the phylogenetic relationship of isolated parasites, and reviewed the literature on oral leishmaniasis. Also, we highlighted the important role of the clinicians in the diagnosis of perioral leishmaniasis lesions, which are unusual and can be confounded with other diseases, especially in individuals living or traveling in certain geographic regions where the parasite is endemic.
Case presentation
Case 1
A 65-year-old woman was referred to the Fajr Health Center. The chief complaint was a lip lesion that began 2 months prior as a slowly enlarging nodule. Patient reported that the lesion began as a small soft mass, which ulcerated later. Clinical examination showed a necrotic ulcer of the left lower lip vermillion. The lip was erythematous and edematous from midline to the left commissure mediolaterally (Fig. 1a). With suspicion of basal cell carcinoma and squamous cell carcinoma, skin scraping, culture, and PCR were accomplished. Touch impression smears and culture were positive and the parasite was characterized by PCR as L. tropica.
Fig. 1.

a An erythematous, calloused, crusted left lower lip ulcerative plaque in patient 1. b A round shiny and red colored nodular lesion with hard consistency in the right inferior lip of patient 2. c An erythematous, edematous, and elliptical ulcerative plaque of the left upper lip with overlying yellow crusting lesion extending to the wet line in patient 3. d Sore swelling, with well-defined edges and scaling, involving the left side of the upper lip in patient 4. e A deep red-colored ulcer covered with mild hemorrhagic crusts and severe swelling of the lower lip in patient 5. f Mild swelling of the superior lip, in addition to ulceration, yellow crusting, scaling and bleeding in patient 6. g A severe swelling cheilitis, with crusting, scaling and fissuring lesion of the right superior lip in patient 7
Case 2
A 75-year-old woman came to the Dermatology Clinic of Saadi Hospital complaining about a lesion on his right lower lip. She reported that the lesion appeared about 3 months before. The clinical examination revealed a round nodular lesion in the right lower lip which was slightly shiny and red colored. Palpation of the lesion revealed a firm consistency (Fig. 1b). The differential diagnosis of a nodular lesion of the lip included: neoplasia (basal cell carcinoma), and tumors from mesenchymal origin (fibroma, lipoma, and neuroma). Giemsa stain and culture were negative. PCR depicted the parasite as L. tropica.
Case 3
A 40-year-old, generally healthy woman complained of persistent lip enlargement and sore that appeared after several days of fever and had been present for 2 months. At clinical examination, the left side of the upper lip appeared erythematous and distended, with overlying yellow crusting lesion extending to the wet line. No lymphadenopathy was associated (Fig. 1c). Giemsa-stained smears and culture were positive (Fig. 2). PCR identified the parasite as L. major.
Fig. 2.
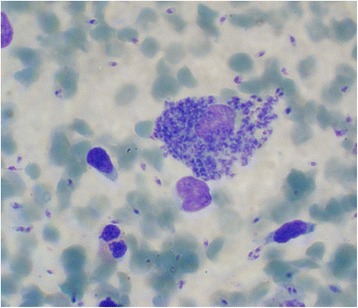
Touch impression smear in patient 3. Numerous intracellular and scattered extracellular amastigotes are present (Giemsa stain; original magnification, ×1000). Kinetoplasts are visible in many amastigotes
Case 4
A 28-year-old man expressed displeasure about a swelling localized to the left side of the upper lip. The patient also stated that the swelling had appeared about 2 months before and that it rapidly enlarged up to the current morphology and size. Clinical examination showed the presence of a swelling which involved the left side of the upper lip. The surface of the swelling was slightly erythematous and irregular, because of the presence of lesion and scaling (Fig. 1d). Consistency was parenchymatous-hard. With suspicion of mycotic infection, laboratory tests were carried out. Slit dermal smears and culture were positive. PCR characterized the parasite as L. tropica.
Case 5
A 10-year-old girl was referred to the Dermatology Clinic of Saadi Hospital. The patient had become infected with CL on the left side of her mentum 3 months before. Three weeks prior to referral, the lesion had spread to the mucosal part of the lower lip. The patient improved diffuse severe swelling of the lower lip. On physical examination, erythema, ulceration, and scaling of the left side of the mentum were detected. There was a diffuse swelling cheilitis of the lower lip extra to ulceration and bleeding of the labial mucosa (Fig. 1e). Giemsa-stained smears and culture were positive. PCR identified the parasite as L. major.
Case 6
An 8-year-old girl presented to the Leishmaniasis research laboratory of the Fajr Health Center with complaint of wound on her upper lip. The lesion started 3 months prior as a small nodule in the center of the upper lip which slowly enlarged over a few weeks and then ulcerated. Clinical examination showed an indurated, crusted, and scaled necrotic ulcer with swelling on the midline of the upper lip, extending to the vermilion. There was purulent discharge from the lesion (Fig. 1 f). With suspicion of cheilitis granulomatosa, slit dermal scraping, culture and PCR were performed. Giemsa-stained smear and culture were positive. PCR portrayed the parasite as L. major.
Case 7
A 4-year-old girl presented with a 2 month history of increasing swelling and painful ulcer on the right upper lip. On clinical examination, an erythematous infiltrated, crusted, scaled and fissured plaque of the upper lip leading to macrocheilitis was observed. Cervical lymph nodes were noticed to be enlarged (Fig. 1g). With suspicion of granulomatous macrocheilitis; slit impression smear, culture and PCR were achieved. Just PCR was positive and characterized the parasite as L. infantum.
The studied patients were examined in the Dermatology Clinic of Saadi Hospital and Fajr Health Center from January 2014 to the end of December 2015. All patients were came from endemic regions of Fars province. A structured questionnaire was used to collect clinical and therapeutic data from all patients.
The margin dermal scrapings were prepared with a no. 15 disposable sterile surgical blade (Unicut, Chicago, USA) to make a slit in the border of the lesion. Dermal tissues were stained with Giemsa (Merck, Darmstadt, Germany), and exhibited amastigotes by light microscope. Employing Giemsa, amastigotes are seen within the cytoplasm of macrophages as pale blue oval bodies with a dark blue nucleus and a small rod-shaped kinetoplast with a specified mitochondrial frame that contains extra-nuclear DNA.
In addition, an aspirate from the active indurated margins of the same lesions was transferred to two tubes of the modified NNN culture medium. Modified NNN medium consists of two phases, horse blood agar base and an overlay Locke’s solution. The specimens were inoculated into the liquid phase of the biphasic medium and incubated. Positive cultures were run in RPMI-1640 medium (Gibco, Frankfurt, Germany) supplemented with 10% heat inactivated FCS (Gibco, Frankfurt, Germany), 100 U/mL penicillin, and 100 μg/mL streptomycin (Gibco, Frankfurt, Germany) for mass cultivation. Promastigotes were harvested and kept at -20 °C until used.
Total genomic DNA was extracted from each clinical sample using the AccuPrep® Genomic DNA Extraction Kit (Bioneer, Daejeon, Korea), according to manufacturer’s instructions. The quantification and quality control of the DNA extraction procedures were performed using a nano spectrophotometer (NanoDrop 1000, Thermo Fisher Scientific, Waltham, Massachusetts, USA). The DNA was stored at −20 °C until being used.
The conserved area of the minicircle kDNA from the Leishmania species was amplified by Semi-Nested PCR. The primers LINR4 (forward) (5’-GGG GTT GGT GTA AAA TAG GG-3’), LIN17 (reverse) (5’-TTT GAA CGG GAT TTC TG-3’), and LIN19 (reverse) (5’-CAG AAC GCC CCT ACC CG-3’) were used for amplification [9]. Standard PCR was carried out with 40 cycles, each consisting of 30 s at 94 °C, 30 s at 52 °C (for LINR4 and LIN17) or 58 °C (for LINR4 and LIN19), 1 min at 72 °C, and a final extension at 72 °C for 10 min in an Eppendorf thermal cycler (Hamburg, Germany). PCR products were visualized by UV after electrophoresis on 1.5% agarose gel using TAE buffer and staining with GelRed (Biotium Inc., Hayward, CA). All primers were synthesized by Macrogen Genomics Laboratories (Macrogen, Seoul, Korea). A 650-bp fragment was amplified for L. major, whereas a 760-bp and 720-bp fragments were amplified for L. tropica and L. infantum, respectively (Fig. 3).
Fig. 3.
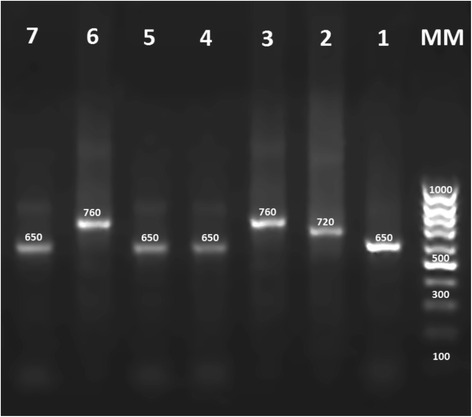
Electrophoresis of PCR products of DNA extracted from positive smears and cultures. The seven lanes contained the products from positive controls of L. tropica (lane 6) and L. major (lane 7), lip lesions due to L. major (lanes 1, 4, 5), L. infantum (lane 2), L. tropica (lane 3), and a molecular size marker (MM)
The PCR products were purified by using QIAquick Gel Extraction Kit (QIAGEN, Hilden, Germany) and sequenced through the sequencing service of Macrogen Genomics Laboratories (Seoul, Korea). The resulting sequences were aligned and compared with those of existing sequences related to Leishmania in GenBank. A Maximum Likelihood (ML) tree was constructed using the MEGA-7 program [10], and genetic distances were calculated with the Maximum Composite Likelihood method. The sequences of three patients of L. tropica showed 100% identity to the published isolate IranJWtrop (AB678350). Also, these three isolates showed 99% identity to the published isolates from UK, Egypt, and Iran (AF308689, X84845, and KM491168) (Fig. 4a). The sequences of three patients of L. major showed 100% identity to the published isolate IranJWmaj (AB678349), In addition, the three L. major showed 99%, 99% and 98% identity to the published isolates from UK and Iran (AF308685, KM555292, and KM555295) respectively (Fig. 4b). The sequence of L. infantum showed 99% identity to the published isolate IranJWinf (AB678348). Plus, this isolate showed 98% identity to the published isolate from Spain (EU437407) (Fig. 4c).
Fig. 4.
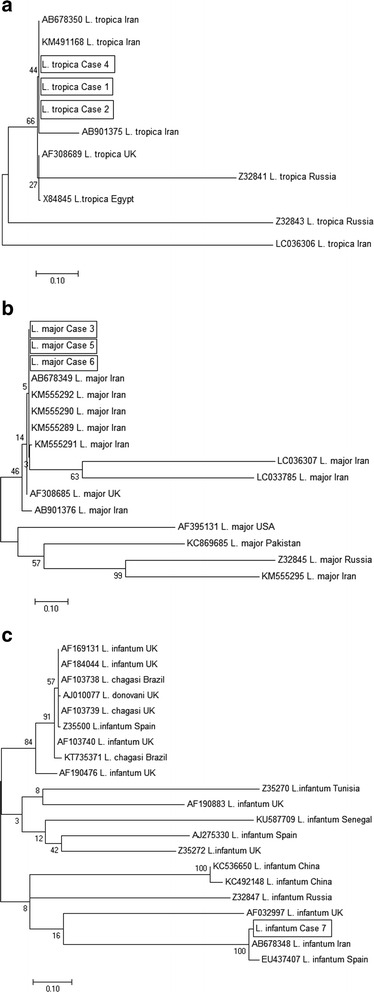
a, b, c Phylogenetic relationship among various Leishmania species to each other as inferred by Maximum Likelihood tree based on minicircle kDNA gene. Numbers on branches are percentage bootstrap values of 1,000 replicates. All positions with less than 95% site coverage were eliminated. The evolutionary distances between sequences were computed using the Maximum Composite Likelihood method and are in the units of the number of base substitutions per site. The scale bar indicates an evolutionary distance of 0.10 nucleotides per position in the sequence. The reference sequences accession numbers are inserted. Evolutionary analyses were conducted in MEGA-7
The patients received intramuscular injections of Meglumine antimoniate (Glucantime®; Sanofi-Aventis, Paris, France), 20 mg/kg/day over a 3-week period with good results [7, 8]. All lesions resolved after 3 weeks of therapy. After 1 year of follow up, the patients were completely normal and no relapses were observed.
Discussion
Cutaneous leishmaniasis is a protozoan-induced disease known to affect people in 98 tropical, subtropical, and Mediterranean countries [1]. The incubation period of CL ranges from 2 weeks up to several months, and a wide spectrum of clinical presentations arranging from cutaneous ulceration to various degrees of mucosal involvement [3]. CL is the most prevalent and is characterized by the presence of ulcers with a well-defined erythematous border and a central crust that is often hemorrhagic and located in exposed areas of the body [3, 7].
In recent years, there has been an intensifying in the number of reports for rare variants of CL in Old World [11]. MCL most usually influences the upper respiratory tract with lesions principally in the oral and nasal mucosa and occasionally in the laryngeal and pharyngeal mucosa [12–18]. These lesions are ordinarily associated with nasal congestion, pain, erythema, edema, halitosis, bleeding, serous rhinorrhea, epistaxis, dysphagia, and dysphonia [19]. The importance of the MCL is in the possibility of having presentations that may determine destructive, disfiguring and disabling injuries, with major repercussions in psychosocial aspect of the individual [19].
The first commitment and sole mucosal involvement of the lip region is very uncommon. Lip leishmaniasis is characterized clinically by the gradual and proceeding expansion of one or both lips and macrocheilitis is the final presentation [20–23]. A papule, nodule or plaque often demonstrate within the swelling undergoes an ulceration which may be covered by crusts and scaling [20–23]. The consistency of the entire lesion is parenchymatous-hard [22, 23]. Lip involvement in leishmaniasis may result from direct extension of nearby skin lesions, as occurred in case 5, or from hematogenous or lymphatic dissemination of Leishmania amastigotes from the skin [19]. Patients with lip leishmaniasis are in good general health, however, case 7 in our study was noticed to have cervical lymphadenopathy. This is in accordance with a previous report of localized leishmaniasis of the larynx [24]. It has been hypothesized that L. infantum strains involved in isolated ML, have developed different resistance to high/low temperature, attaining the capability to live electively in mucous membranes [6]. In case 5, nodular crusted plaque localized on the left side of the mentum was representative for CL and it was the clue for us that lip lesion could also be a Leishmania lesion.
In MCL, the clinical demonstration at the perioral site is atypical and can be deceiving. Accordingly, clinical diagnosis of lip leishmaniasis is frequently a challenge with a significantly delayed diagnosis or even an erroneous clinical diagnosis of malignancy [12, 19, 25]. The most important diseases that must be taken into account in differential diagnosis are herpes labialis [26], syphilitic chancre [27], Melkersson-Rosenthal syndrome [28], orofacial granulomatosis [28], cheilitis granulomatosa [29, 30], Wegener granulomatosis [12, 19, 25], oral Crohn’s disease [31], sarcoidosis [32, 33], skin tuberculosis [34], discoid lupus erythematosus [34], lymphoma [34], foreign body giant cell granuloma [12, 19, 25, 28], leprosy [35], mycotic infection [36], fibroma, lipoma, and neuroma [37], basal cell carcinoma [38], and squamous cell carcinoma [34, 39]. The diagnosis is easier to make if typical CL lesions are present elsewhere on the skin. However, this was observed in only case 5.
Identification of leishmania parasites in dermal macrophages by skin biopsy or dermal scraping can confirm the diagnosis. When performing the slit smear, it is important to scrape tissue from the inside of the lesion and from the edges of the cut. However, in chronic lesions, parasites may be scarce. Therefore, failure to visualize amastigotes on histopathology does not exclude the diagnosis of MCL. In this context, culture, IFA and PCR can be amongst significant diagnostic techniques [7].
Detection of the kDNA of Leishmania spp. by semi-nested PCR in the oral mucosal specimen and clinical course of the disease verified the diagnosis of MCL. PCR is now the diagnostic method of choice for molecular confirmation of cases of MCL [40]. In this study, L. tropica, L. major, and L. infantum were the identified species in this case series.
Involvement of the lip can be treated with intralesional injections, systemic treatment, or their combination depending on the clinical manifestation and infective species. Intralesional injections are associated with burning sensation, pain, inflammation, and vasovagal reaction [41]. Systemic treatment is usually more effective than local, although less tolerated because of increased toxicity. The widely used therapeutics for treatment of mucosal leishmaniasis are: pentavalent antimony compounds (Pentostam® and Glucantime®), liposomal amphotericin B (Ambisome®), pentamidine, oral azole compounds, and miltefosine [7, 8, 41]. Recommended follow-up times vary, although 12 months has been suggested for CL and MCL [12].
Conclusion
In conclusion, we highlight a case series of lip leishmaniasis which are rare and can be confused with other diseases. In addition, the present report emphasizes the importance of a multidisciplinary approach in the diagnosis and treatment of lip leishmaniasis. These unusual clinical presentations of leishmaniasis should be considered in differential diagnosis of rebellious lip lesions by physicians practiced both in endemic and non-endemic regions, since MCL is ascending in these areas due to increasing rate of traveling, as tourists or military personnel, to endemic regions. Clinician should kept in mind leishmaniasis in the differential diagnosis of orofacial granulomatosis and other inflammatory and neoplastic diseases.
Acknowledgements
The results described in this paper were a part of Ph.D. thesis of Iraj Mohammadpour. The study was financially supported by the office of vice-chancellor for research of Shiraz University of Medical Sciences (Grant No. 94-7548).
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Authors’ contributions
IM collected data, performed the molecular and phylogenetic analyses, and drafted the manuscript. FH treated and managed the patients at the clinical site and gave advice in drafting. IM, MHM and GRH participated in interpretation and discussion. IM, MHM and GRH finally approved the article. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consents were obtained from the patients or the parents of child patients for publication of this case reports and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shiraz University of Medical Sciences and performed in accordance with the Declaration of Helsinki (code: IR.SUMS.REC.1394.S282).
Financial support
The study was financially supported by the office of vice-chancellor for research of Shiraz University of Medical Sciences (Grant No. 94-7548).
Abbreviations
- CL
Cutaneous leishmaniasis
- DCL
Diffuse cutaneous leishmaniasis
- MCL
Mucocutaneous leishmaniasis
- VL
Visceral leishmaniasis
Contributor Information
Iraj Mohammadpour, Email: iraj2106@yahoo.com.
Mohammad Hossein Motazedian, Phone: +98-71-32305291, Email: motazedm@sums.ac.ir.
Farhad Handjani, Email: hanjanif@yahoo.com.
Gholam Reza Hatam, Email: hatam908@yahoo.com.
References
- 1.Alvar J, Velez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M. Leishmaniasis worldwide and global estimates of its incidence. PLoS One. 2012;7:e35671. doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davami MH, Motazedian MH, Kalantari M, Asgari Q, Badzohre A, Mohammadpour I. First microscopical and molecular-based characterization of Leishmania major within naturally infected Phlebotomus salehi (Diptera; Psychodidae) in Fars province, southern Iran. Ann Trop Med Parasitol. 2011;105:485–491. doi: 10.1179/1364859411Y.0000000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.David CV, Craft N. Cutaneous and mucocutaneous leishmaniasis. Dermatolog Ther. 2009;22:491–502. doi: 10.1111/j.1529-8019.2009.01272.x. [DOI] [PubMed] [Google Scholar]
- 4.Grave B, McCullough M, Wiesenfeld D. Orofacial granulomatosis: a 20-year review. Oral Dis. 2009;15:46–51. doi: 10.1111/j.1601-0825.2008.01500.x. [DOI] [PubMed] [Google Scholar]
- 5.De Paulo LF, Rocha GF, Luisi CM, Jr, Rosa RR, Durighetto AF., Jr Mucocutaneous leishmaniasis: mucosal manifestations in an endemic country. Int J Infect Dis. 2013;17:1088–1089. doi: 10.1016/j.ijid.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Alessio Strazzulla, Salvatore Cocuzza, Marilia Rita Pinzone, Maria Concetta Postorino, Stefano Cosentino, Agostino Serra, Bruno Cacopardo, Giuseppe Nunnari. Mucosal Leishmaniasis: An Underestimated Presentation of a Neglected Disease. BioMed Research International. 2013;1–7. [DOI] [PMC free article] [PubMed]
- 7.Goto H, Lindoso JAL. Current diagnosis and treatment of cutaneous and mucocutaneous leishmaniasis. Expert Rev Anti Infect Ther. 2010;8:419–433. doi: 10.1586/eri.10.19. [DOI] [PubMed] [Google Scholar]
- 8.Amato VS, Tuon FF, Bacha HA, Neto VA, Nicodemo AC. Mucosal leishmaniasis: current scenario and prospects for treatment. Acta Trop. 2008;105:1–9. doi: 10.1016/j.actatropica.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Aransay AM, Scoulica E, Tselentis Y. Detection and identification of Leishmania DNA within naturally infected sand flies by seminested PCR on minicircle kinetoplastic DNA. Appl Environ Microbiol. 2000;66:1933–1938. doi: 10.1128/AEM.66.5.1933-1938.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sudhir Kumar, Glen Stecher, Koichiro Tamura. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Molecular Biology and Evolution. 2016;33(7):1870–1874. [DOI] [PMC free article] [PubMed]
- 11.Akilov OE, Khachemoune A, Hasan T. Clinical manifestations and classification of old world cutaneous leishmaniasis. Int J Dermatol. 2007;46:132–142. doi: 10.1111/j.1365-4632.2007.03154.x. [DOI] [PubMed] [Google Scholar]
- 12.Nadler C, Enk CD, Leon GT, Samuni Y, Maly A, Czerninski R. Diagnosis and management of oral leishmaniasis: case series and literature review. J Oral Maxillofac Surg. 2014;72:927–934. doi: 10.1016/j.joms.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 13.Marra F, Chiappetta MC, Vincenti V. Ear, nose and throat manifestations of mucocutaneous leishmaniasis: a literature review. Acta Biomed. 2014;85:3–7. [PubMed] [Google Scholar]
- 14.Palmeiro MR, Rosalino CM, Quintella LP, Morgado FN, Da Costa Martins AC, Moreira J, De Oliveira SA, Conceicao-Silva F. Gingival leishmaniasis in an HIV-negative patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e12–e16. doi: 10.1016/j.tripleo.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Teemul TA, Giles-Lima M, Williams J, Lester SE. Laryngeal leishmaniasis: case report of a rare infection. Head Neck. 2013;35:E277–E279. doi: 10.1002/hed.23141. [DOI] [PubMed] [Google Scholar]
- 16.Salvatore Cocuzza, Alessio Strazzulla, Marilia Rita Pinzone, Stefano Cosentino, Agostino Serra, Rosario Caltabiano, Salvatore Lanzafame, Bruno Cacopardo, Giuseppe Nunnari. Isolated Laryngeal Leishmaniasis in Immunocompetent Patients: An Underdiagnosed Disease. Case Reports in Infectious Diseases. 2013;1–7. [DOI] [PMC free article] [PubMed]
- 17.Di Lella F, Vincenti V, Zennaro D, Afeltra A, Baldi A, Giordano D, Pasanisi E, Bacciu A, Bacciu S, Di Lella G. Mucocutaneous leishmaniasis: report of a case with massive involvement of nasal, pharyngeal and laryngeal mucosa. J Oral Maxillofac Surg. 2006;35:870–872. doi: 10.1016/j.ijom.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 18.Shirian S, Oryan A, Hatam GR, Daneshbod Y. Three Leishmania/L. species–L. infantum, L. major, L. tropica–as causative agents of mucosal leishmaniasis in Iran. Pathog Glob Health. 2013;107:267–272. doi: 10.1179/2047773213Y.0000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Motta ACF, Lopes MA, Ito FA, Carlos-Bregni R, De Almeida OP, Roselino AM. Oral leishmaniasis: a clinicopathological study of 11 cases. Oral Dis. 2007;13:335–340. doi: 10.1111/j.1601-0825.2006.01296.x. [DOI] [PubMed] [Google Scholar]
- 20.Roundy S, Almony J, Zislis T. Cutaneous Leishmaniasis of the lower Lip in a united states soldier. J Oral Maxillofac Surg. 2008;66:1513–1515. doi: 10.1016/j.joms.2007.12.045. [DOI] [PubMed] [Google Scholar]
- 21.Ferreli C, Atzori L, Zucca M, Pistis P, Aste N. Leishmaniasis of the lip in a patient with Down’s syndrome. J Eur Acad Dermatol Venereol. 2004;18:599–602. doi: 10.1111/j.1468-3083.2004.00987.x. [DOI] [PubMed] [Google Scholar]
- 22.Veraldi S, Rigoni C, Gianotti R. Leishmaniasis of the lip. Acta Derm Venereol. 2002;82:469–470. doi: 10.1080/000155502762064674. [DOI] [PubMed] [Google Scholar]
- 23.Veraldi S, Bottini S, Persico MC. Case report: leishmaniasis of the upper lip. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:659–661. doi: 10.1016/j.tripleo.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Rongioletti F, Cannata GE, Parodi A. Leishmaniasis due to L. infantum presenting as macrocheilitis and responding to liposomal amphotericin B. Eur J Dermatol. 2009;19:281–282. doi: 10.1684/ejd.2009.0652. [DOI] [PubMed] [Google Scholar]
- 25.Mignogna MD, Celentano A, Leuci S, Cascone M, Adamo D, Ruoppo E, Favia G. Mucosal leishmaniasis with primary oral involvement: a case series and a review of the literature. Oral Dis. 2014;21:e70–e78. doi: 10.1111/odi.12268. [DOI] [PubMed] [Google Scholar]
- 26.Esmann J. The many challenges of facial herpes simplex virus infection. J Antimicrob Chemother. 2001;47:17–27. doi: 10.1093/jac/47.suppl_1.17. [DOI] [PubMed] [Google Scholar]
- 27.Paz A, Potasman I. Oral lesions as the sole presenting symptom of secondary syphilis. Travel Med Infect Dis. 2004;2:37–39. doi: 10.1016/j.tmaid.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Boukhris I, Azzabi S, Cherif E, Kechaou I. Orofacial granulomatosis: do not forget leishmaniasis. BMJ Case Rep. 2015. doi: 10.1136/211919. [DOI] [PMC free article] [PubMed]
- 29.Critchlow WA, Chang D. Cheilitis granulomatosa: a review. Head Neck Pathol. 2014;8:209–213. doi: 10.1007/s12105-013-0488-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Serarslan G, Aksakal M. Cutaneous leishmaniasis mimicking granulomatous cheilitis and treated successfully with oral fluconazole in a boy. Ann Parasitol. 2015;61:197–199. doi: 10.17420/ap6103.08. [DOI] [PubMed] [Google Scholar]
- 31.Padmavathi BN, Sharma S, Astekar M, Rajan Y, Sowmya GV. Oral Crohn’s disease. J Oral Maxillofac Pathol. 2014;18:S139–S142. doi: 10.4103/0973-029X.141369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tchernev G, Patterson JW, Nenoff P, Horn LC. Sarcoidosis of the skin–a dermatological puzzle: important differential diagnostic aspects and guidelines for clinical and histopathological recognition. J Eur Acad Dermatol Venereol. 2010;24:125–137. doi: 10.1111/j.1468-3083.2009.03396.x. [DOI] [PubMed] [Google Scholar]
- 33.Moravvej H, Vesal P, Abolhasani E, Nahidi S, Mahboudi F. Comorbidity of Leishmania major with cutaneous sarcoidosis. Indian J Dermatol. 2014;59:316. doi: 10.4103/0019-5154.131453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saab J, Fedda F, Khattab R, Yahya L, Loya A, Satt M, Kibbi AG, Houreih MA, Raslan W, El-Sabban M, Khalifeh I. Cutaneous leishmaniasis mimicking inflammatory and neoplastic processes: a clinical, histopathological and molecular study of 57 cases. J Cutan Pathol. 2012;39:251–262. doi: 10.1111/j.1600-0560.2011.01844.x. [DOI] [PubMed] [Google Scholar]
- 35.Dassoni F, Abebe Z, Naafs B, Morrone A. Cutaneous and mucocutaneous Leishmaniasis resembling borderline-tuberculoid leprosy: a new clinical presentation? Acta Derm Venereol. 2013;93:74–77. doi: 10.2340/00015555-1338. [DOI] [PubMed] [Google Scholar]
- 36.Linss G, Richter C, Janda J, Gantenberg R. Leishmaniasis of the lips mimicking a mycotic infection. Mycoses. 1998;41:78–80. doi: 10.1111/j.1439-0507.1998.tb00608.x. [DOI] [PubMed] [Google Scholar]
- 37.Voisin C, Bianchi F, Dominique P, Evrard L. Leishmaniasis of the lip: report of a case. Bull Group Int Rech Sci Stomatol Odontol. 2011;50:6–10. [PubMed] [Google Scholar]
- 38.Silapunt S, Peterson SR, Goldberg LH, Friedman PM, Alam M. Basal cell carcinoma on the vermilion lip: a study of 18 cases. J Am Acad Dermatol. 2004;50:384–387. doi: 10.1016/j.jaad.2003.08.027. [DOI] [PubMed] [Google Scholar]
- 39.Ramos A, Munez E, Garcia-Dominguez J, Martinez-Ruiz R, Chicharro C, Banos I, Suarez-Massa D, Cuervas-Mons V. Mucosal leishmaniasis mimicking squamous cell carcinoma in a liver transplant recipient. Transpl Infect Dis. 2015;17:488–492. doi: 10.1111/tid.12380. [DOI] [PubMed] [Google Scholar]
- 40.Oliveira JG, Novais FO, de Oliveira CI, da Cruz Junior AC, Campos LF, da Rocha AV, Boaventura V, Noronha A, Costa JM, Barral A. Polymerase chain reaction (PCR) is highly sensitive for diagnosis of mucosal leishmaniasis. Acta Trop. 2005;94:55–59. doi: 10.1016/j.actatropica.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 41.Monge-Maillo B, Lopez-Velez R. Therapeutic options for old world cutaneous leishmaniasis and new world cutaneous and mucocutaneous Leishmaniasis. Drugs. 2013;73:1889–1920. doi: 10.1007/s40265-013-0132-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.


