Abstract
Context:
Volitional preemptive abdominal contraction (VPAC) during dynamic activities may alter trunk motion, but the role of the core musculature in positioning the trunk during landing tasks is unclear.
Objective:
To determine whether volitional core-muscle activation incorporated during a drop vertical jump alters lower extremity kinematics and kinetics, as well as trunk and lower extremity muscle activity at different landing heights.
Design:
Controlled laboratory study.
Setting:
Clinical biomechanics laboratory.
Patients or Other Participants:
Thirty-two young healthy adults, consisting of 17 men (age = 25.24 ± 2.88 years, height = 1.85 ± 0.06 m, mass = 89.68 ± 16.80 kg) and 15 women (age = 23.93 ± 1.33 years, height = 1.67 ± 0.08 m, mass = 89.68 ± 5.28 kg).
Intervention(s):
Core-muscle activation using VPAC.
Main Outcome Measure(s):
We collected 3-dimensional ankle, knee, and hip motions, moments, and powers; ground reaction forces; and trunk and lower extremity muscle activity during 0.30- and 0.50-m drop vertical-jump landings.
Results:
During landing from a 0.30-m height, VPAC performance increased external oblique and semitendinosis activity, knee flexion, and knee internal rotation and decreased knee-abduction moment and knee-energy absorption. During the 0.50-m landing, the VPAC increased external oblique and semitendinosis activity, knee flexion, and hip flexion and decreased ankle inversion and hip-energy absorption.
Conclusions:
The VPAC performance during landing may protect the anterior cruciate ligament during different landing phases from different heights, creating a protective advantage just before ground contact and after the impact phase. Incorporating VPAC during high injury-risk activities may enhance pelvic stability, improve lower extremity positioning and sensorimotor control, and reduce anterior cruciate ligament injury risk while protecting the lumbar spine.
Key Words: clinical biomechanics, core stabilization, rehabilitation
Anterior cruciate ligament (ACL) injuries sustained during landing, deceleration, or directional change1 result in considerable consequences to the athlete and society.2,3 The overall ACL injury rate in men's and women's National Collegiate Athletic Association athletics is 0.15 per 1000 athlete-exposures and appears to be influenced by multiple factors, including sport-specific aspects.4,5 Reduced knee flexion (between 0° and 30°) at initial contact in landing produces large joint-compression forces and shear forces that result in anterior tibial translation.1,6 Through cadaveric,6,7 in vivo,8 and computer-simulation9 studies of ACL strain and force, researchers have found that reduced flexion represents the most vulnerable knee position for ACL tears.
In addition to sagittal-plane knee angle, the positions of other lower extremity joints at landing contribute to ACL injury mechanisms.10,11 Injury risk appears to be further increased when transverse-plane rotation, particularly internal rotation,12 is added to this landing position. Moreover, different position combinations, including knee valgus combined with hip internal rotation and tibial external rotation or a fully extended knee combined with tibial internal rotation, appear to be more frequently associated with ACL injury.1
Alterations in trunk and lower extremity muscle-activation patterns may increase ACL injury risk.13 For example, diminished hamstrings muscle activation during landing reduces dynamic joint stability,14 impairing the muscles' ability to reduce anterior tibial shear forces at the knee.15 This reduced hamstrings activity may be accompanied by increased quadriceps activation, which leads to increased tibiofemoral joint compression and anterior tibial displacement that increases ACL strain.15 Conversely, optimizing hamstrings muscle activity and quadriceps-hamstrings cocontraction may stabilize the tibia, resulting in decreased anterior shear and ACL strain.6,16 Muscle activity proximal to the knee joint may influence knee-motion control.13,17−19 Weakness and poor control of the hip abductors and external rotators reduce pelvic stability, which may lead to excessive dynamic knee valgus.20 In response, heightened pelvic-stability control may affect the outcomes of knee-control measures by enhancing normal kinematic responses during landing activities. The trunk muscles can influence pelvic stability via their attachments to the pelvis; therefore, activating these muscles may create a more stable pelvic base for hip-muscle activation.
Volitional preemptive abdominal contraction (VPAC) is often used to increase trunk-muscle activity, improve lumbar spine stability, and reduce pelvic motion.21,22 A commonly used VPAC strategy is the abdominal-bracing maneuver (ABM), which produces a global trunk-muscle contraction.21,23 This VPAC strategy may alter lower extremity neuromuscular control and improve pelvic stability by affecting hip-abductor and external-rotator control, thereby affecting dynamic knee valgus and pelvic stability.24,25
The role of trunk-muscle activation in modifying pelvic responses and influencing lower extremity control has not been fully examined, but preliminary evidence has suggested that trunk stabilization may improve lower extremity control. For example, investigators26 have demonstrated that preventive sensorimotor control programs that include lumbar-stabilization exercises reduce ACL injury risk in athletes. In addition, Shirey et al27 found that a nonquantified VPAC activity decreased bilateral frontal-plane hip displacement and increased stance-limb knee flexion during a 6-in (15.24-cm) step descent. Furthermore, transversus abdominis activation increased gluteus maximus (GM) and medial hamstrings muscle activity and decreased anterior pelvic tilt during prone active hip extension.24
Researchers21,28,29 have reported that increased trunk lateral flexion during landing activities can also influence lower extremity mechanics. Trunk-muscle activation during these activities could potentially alter this motion, but it is unclear what role the core musculature plays in positioning the trunk during landing tasks. A better understanding of the core musculature's influence on pelvic stability, lower extremity muscle activity, and trunk positioning during the landing sequence might lead to enhanced training strategies for landing tasks, improving their effectiveness in reducing injury risk at the ACL and other lower extremity sites. Therefore, the influence of spine-stabilization strategies on lower extremity control during higher-risk activities, such as landing, requires further investigation.
The primary purpose of our study was to determine whether VPAC incorporated into a drop vertical jump altered lower extremity kinematics and kinetics, as well as trunk and lower extremity muscle activity, during different landing phases. The secondary purpose of our study was to examine possible differences in these variables when landing from 0.50- and 0.30-m heights. Whereas investigators26,30 have used a 0.30-m landing height to represent low- to midlevel athletic and recreational performance, greater heights, such as 0.50 m, may be better suited for human sport performance and elite athletic measures.31,32 Thus, this comparison may better reflect responses to sport performance.32 We hypothesized that VPAC would improve neuromuscular and biomechanical measures that may be related to ACL injury during a drop vertical jump. Moreover, we hypothesized that lower extremity electromyography (EMG) and kinematic and kinetic variables would differ between landing heights. If VPAC improves landing technique, incorporating this maneuver during athletic and industrial tasks that increase the risk for lower extremity injury may help reduce that risk.
METHODS
Participants
Seventeen men (age = 25.24 ± 2.88 years, height = 1.85 ± 0.06 m, mass = 89.68 ± 16.80 kg) and 15 women (age = 23.93 ± 1.33 years, height = 1.67 ± 0.08 m, mass = 89.68 ± 5.28 kg) completed the study. The sample size needed to approach 80% statistical power was estimated from the data of a previous study in which VPAC was examined.27 An effect size index of f = 0.50 was estimated. With a desired power of 80% (1 − β = 0.80) and an α level of .05, this effect size index required a minimum sample size of 28.33
All participants were between the ages of 18 and 35 years and scored between 4 and 8 on a physical activity level scale developed by Noyes et al34 and published in Wojtys et al.35 The mean activity levels were 5.6 for women and 6.5 for men. Volunteers were excluded if they self-reported a history of knee pain or low back pain (LBP) in the 2 years before the study, history of knee or lumbar spine surgery, an active abdominal or gastrointestinal condition, or pregnancy. In addition, participants were excluded if they had engaged in training through a jump-landing program. All participants provided written informed consent, and the study was approved by the Texas Tech University Health Sciences Center Institutional Review Board for the Protection of Human Subjects.
Procedures
Participants wore their own T-shirts and shorts and a pair of standard athletic shoes, which we provided. Before data collection, participants received instruction on VPAC and performed drop vertical-jump training. Investigators13,14 have used drop vertical-jump–landing sequences to represent lower extremity control during both landing and ballistic responses in the closed chain. For VPAC instruction, participants were taught the ABM. They were instructed to place the first webspace of each hand over the respective iliac crest. After placement, participants were instructed to prepare themselves to be punched in the stomach while continuing with diaphragmatic respiration.21 The investigator (R.H.) visually verified the contractile states of the abdominal muscles by reviewing the recorded EMG data from the internal oblique (IO) and external oblique (EO) muscles during each trial. To familiarize themselves with the drop vertical-jump task, participants performed jump trials with and without superimposed VPAC until they were comfortable with the task. For the drop vertical jump, participants stood with their toes at the edge of 0.30- and 0.50-m boxes. The 0.30-m landing height represents a midlevel load for recreationally active individuals, and the 0.50-m box represents a dynamic, higher-performance load. The drop vertical-jump trial was initiated when participants stepped forward with the dominant foot, which was defined as the kicking foot, and dropped down off the box, simultaneously landing on a separate force platform with each foot. The landing was immediately followed by a maximal vertical jump during which participants reached with both upper extremities overhead to a maximal achievable height.
Key Points
Using a volitional preemptive abdominal contraction strategy during 0.30- and 0.50-m drop vertical-jump landings may decrease exposure to biomechanical factors contributing to anterior cruciate ligament injury.
Selected benefits were greater during the 0.30-m than during the 0.50-m drop vertical jump, possibly due to increased external loads associated with the greater height.
Individuals can be trained to incorporate volitional preemptive abdominal contraction during functional, closed chain activities in a controlled laboratory setting to enhance pelvic stability, improve lower extremity sensorimotor control and positioning, and reduce biomechanical factors associated with anterior cruciate ligament injury while protecting the lumbar spine.
After drop vertical-jump practice, participants warmed up on a treadmill for 5 minutes and performed several practice trials before data collection. Next, they performed a series of six 0.30-m and six 0.50-m drop vertical-jump trials in random order, performing 3 trials with no VPAC and 3 trials with VPAC from each height. The contractile condition and box-height order were randomized for each participant.
Using locations and procedures from Vaughan et al,36 we attached 15 reflective markers, each with a 2.5-cm diameter, to the participant to collect 3-dimensional kinematics (Vicon Peak Motus 9.1.0; Peak Performance, Inc, Englewood, CO) at a sampling rate of 120 Hz (Figure 1). Three markers on each segment were used to define a local axis system and to calculate joint centers. The local axis system and joint centers were used to calculate an anatomic axis system.36 Raw 3-dimensional coordinates were smoothed using a fourth-order, no-phase-shift, low-pass Butterworth digital filter with a cutoff of 6 Hz before data were exported for further analysis. The ground reaction force (GRF) data were collected at 1200 Hz using 2 parallel force plates (model 4060-10-2000; Bertec Corporation, Columbus, OH) oriented side by side. Muscle activities of the IO,37 EO,37 erector spinae (ES),37 GM,38 semitendinosis (ST),38 biceps femoris,38 vastus medialis,38 and vastus lateralis38 were collected on the right side using self-adhesive Ag-AgCl bipolar differential electrodes (model 272; Noraxon USA, Scottsdale, AZ) with a 1-cm diameter and a 2-cm interelectrode distance. A common reference electrode was placed on the right tibial tubercle. The skin was cleaned with alcohol, shaved if necessary, and lightly abraded to reduce impedance. The EMG data were wirelessly transmitted and collected at 1200 Hz using an 8-channel transmitter (model Telemyo 900; Noraxon USA), which was firmly strapped across the upper back. The transmitter system bandwidth was 10 to 500 Hz with a signal-to-noise ratio of 1 μV root mean square baseline noise. The signal was amplified 2000 times with an impedance of 10 MΩ and a common-mode rejection ratio of 130 dB.
Figure 1.

Vaughan et al36 lower extremity marker set.
Data Reduction
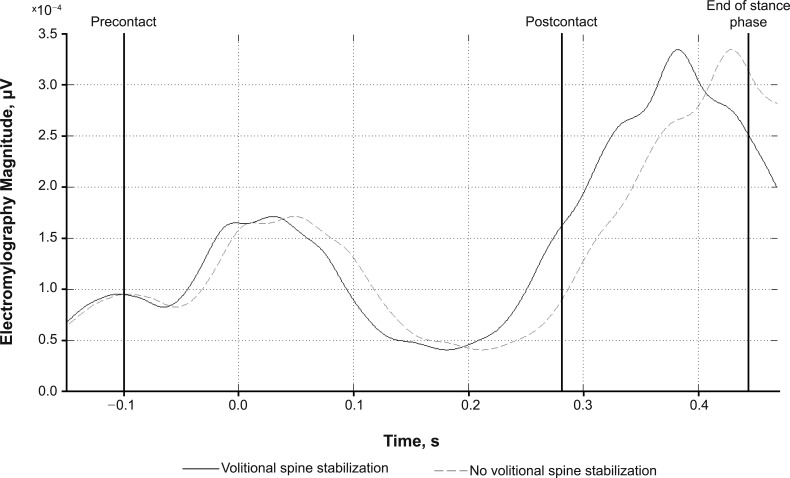
We assessed 16 kinematic, 10 kinetic, and 16 EMG dependent variables. Kinematic dependent variables were sagittal-, frontal-, and transverse-plane angles of the ankle and knee and sagittal- and frontal-plane angles of the hip. All angles were analyzed for their positions at initial contact and their ranges of motion during the postcontact landing phase. The postcontact landing phase was defined as the period from the instant of initial foot contact with the force platform until maximum knee flexion (Figure 2). Kinetic dependent variables were peak vertical GRF; internal sagittal- and frontal-plane moments of the ankle, knee, and hip; and sagittal-plane powers of the ankle, knee, and hip. Joint moments were calculated from the distal to the proximal segment using an inverse-dynamics solution derived from the Newton-Euler approach.39 All joint kinetic variables were analyzed for their mean maximum values during the eccentric landing phase. Electromyography-dependent variables were magnitudes of the IO, EO, ES, GM, ST, biceps femoris, vastus medialis, and vastus lateralis muscles during 2 phases: (1) the precontact phase, which was defined as the period from 100 milliseconds before initial contact to initial contact, and (2) the postcontact landing phase, as described earlier.
Figure 2.
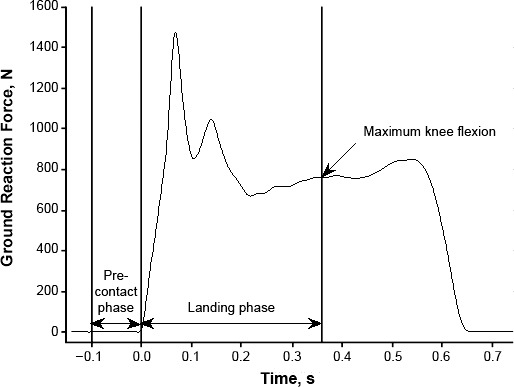
Example of ground reaction force for 1 individual during landing with no volitional preemptive abdominal contraction. Time zero is initial contact (IC). The precontact phase is from 100 milliseconds precontact to IC. The postcontact landing phase is from IC to maximum knee flexion.
All raw data were exported from the Vicon Motus system and imported into a custom Matlab program (version 7.10.0; The MathWorks, Inc, Natick, MA) for processing. The EMG data were bandpass filtered between 20 and 450 Hz using a fourth-order, no-phase-shift, low-pass Butterworth digital filter and were full-wave rectified.40 The filtered EMG data were analyzed to determine precontact and postcontact muscle amplitudes. The root mean square amplitude was calculated for each muscle for the precontact and postcontact phases of each trial.
Statistical Analyses
All dependent variables were assessed for normality of distribution using the Shapiro-Wilk test. The EMG data were not normally distributed, so we applied a log10 transformation, which resulted in normal distributions for all EMG variables. All subsequent EMG analyses incorporated these transformed variables.
Differences between VPAC and height conditions for each kinematic and kinetic dependent variable were assessed using 2 (abdominal contractile state) × 2 (landing height) within-subject analyses of variance. In addition, repeated-measures analyses of variance were used to compare all EMG muscle-activation differences from precontact to postcontact landing phases with and without VPAC performance. All statistical tests were conducted in an exploratory analysis comparing VPAC conditions with an α level of .05. Statistical analyses were conducted using SPSS software (version 21.0; IBM Corp, Armonk, NY).
RESULTS
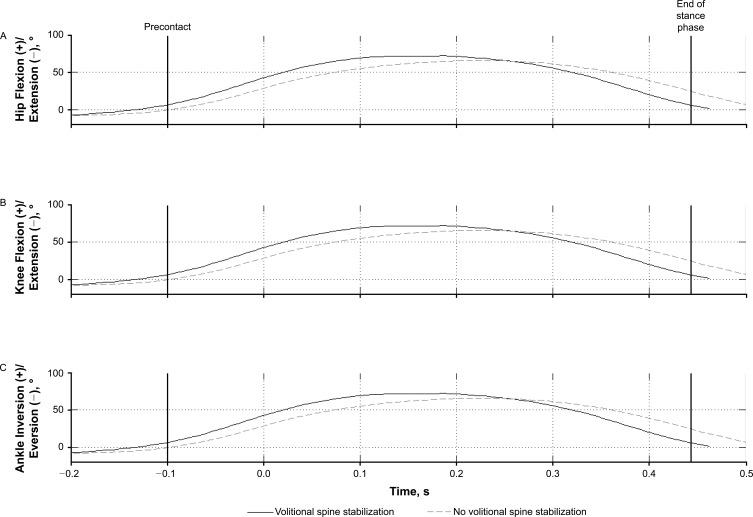
Performing the VPAC altered joint kinematics at the hip, knee, and ankle (Figure 3; Tables 1 through 3) during 0.30- and 0.50-m drop vertical jumps. We observed 2-way interaction effects between VPAC and height for knee flexion (P = .01, ηp2 = 0.201), hip flexion (P = .02, ηp2 = 0.167), and ankle-rotation angles at contact (P = .04, ηp2 = 0.139; Table 1). No other dependent variables exhibited a 2-way interaction effect. We observed several main effects for height and VPAC performance, indicating differences between VPAC conditions during the 0.30- and 0.50-m landings (Tables 1 through 3).
Figure 3.
Kinematic differences for the right lower extremity on the 0.50-m drop vertical jump from a representative participant. A, Hip flexion-extension. B, Knee flexion-extension. C, Ankle inversion-eversion. Angles were analyzed for their position at initial contact (time zero) and during the eccentric landing phase (maximum knee flexion). The end-of-stance phase is represented by the right vertical line.
Table 1.
Kinematic Variables for the Right Lower Extremity and Trunk (Mean ± SD)
| Kinematic Variable, ° |
Height |
|||
| 0.30 m |
0.50 m |
|||
| No VPAC |
VPAC |
No VPAC |
VPAC |
|
| Ankle plantar flexion | 11.6 ± 7.9 | 11.6 ± 9.3 | 40.0 ± 9.8 | 41.1 ± 8.3 |
| Ankle inversiona | 10.4 ± 11.3 | 8.5 ± 6.8 | 7.2 ± 12.3 | 3.2 ± 14.5 |
| Ankle rotation | 22.2 ± 12.8 | 23.9 ± 16.1 | 24.3 ± 11.3 | 23.3 ± 11.7 |
| Knee flexionb | 40.9 ± 12.5 | 44.9 ± 13.7 | 46.8 ± 26.5 | 40.4 ± 15.7 |
| Knee abduction | 4.4 ± 3.4 | 4.4 ± 2.9 | 8.7 ± 5.4 | 6.4 ± 14.4 |
| Knee rotationb | 31.0 ± 10.9 | 33.7 ± 13.6 | 31.6 ± 11.2 | 32.1 ± 9.9 |
| Hip flexion | 9.2 ± 4.91 | 9.4 ± 4.4 | 29.3 ± 13.9 | 25.4 ± 28.3 |
| Hip abduction | 2.2 ± 1.5 | 2.4 ± 1.5 | 12.8 ± 39.9 | 10.0 ± 38.1 |
| Ankle plantar flexion at contact | −7.0 ± 16.7 | −7.4 ± 16.3 | 13.1 ± 23.9 | 15.4 ± 11.2 |
| Ankle inversion at contact | −4.2 ± 19.8 | −4.0 ± 19.7 | 11.7 ± 20.7 | 8.4 ± 14.7 |
| Ankle rotation at contactc | −9.1 ± 7.0 | −9.7 ± 7.0 | −14.1 ± 8.1 | −9.9 ± 8.9 |
| Knee flexion at contacta,c | 18.6 ± 21.4 | 18.5 ± 20.4 | 9.4 ± 9.6 | 11.9 ± 9.5 |
| Knee abduction at contact | −6.7 ± 18.6 | −6.1 ± 19.4 | −3.8 ± 6.7 | −3.5 ± 5.2 |
| Knee rotation at contact | −4.7 ± 10.9 | −4.8 ± 11.7 | −0.1 ± 16.9 | −1.9 ± 10.9 |
| Hip flexion at contacta,c | 28.1 ± 8.2 | 28.5 ± 7.7 | 25.4 ± 7.2 | 27.2 ± 6.8 |
| Hip abduction at contact | 1.4 ± 9.6 | 1.3 ± 9.2 | 7.1 ± 4.9 | 6.7 ± 6.0 |
Abbreviation: VPAC, preemptive abdominal contraction.
VPAC effect for the 0.50-m height (P < .05).
VPAC effect for the 0.30-m height (P < .05).
Interaction between VPAC and height (P < .05).
Table 3.
Electromyography Variables for the Right Lower Extremity and Trunk (Mean ± SD)
| Electromyography Variable, μV |
Height |
|||
| 0.30 m |
0.50 m |
|||
| No VPAC |
VPAC |
No VPAC |
VPAC |
|
| Precontact | ||||
| Internal oblique | 0.236 ± 0.22 | 0.239 ± 0.21 | 0.206 ± 0.16 | 0.173 ± 0.17 |
| External obliquea,b | 0.165 ± 0.10 | 0.201 ± 0.11 | 0.197 ± 0.10 | 0.231 ± 0.12 |
| Erector spinae | 0.083 ± 0.11 | 0.094 ± 0.14 | 0.105 ± 0.14 | 0.107 ± 0.10 |
| Gluteus maximus | 0.078 ± 0.13 | 0.108 ± 0.18 | 0.076 ± 0.12 | 0.086 ± 0.18 |
| Semitendinosisb | 0.148 ± 0.11 | 0.163 ± 0.14 | 0.164 ± 0.10 | 0.219 ± 0.20 |
| Biceps femoris | 0.095 ± 0.14 | 0.098 ± 0.14 | 0.075 ± 0.11 | 0.067 ± 0.11 |
| Vastus medialis | 0.149 ± 0.15 | 0.160 ± 0.17 | 0.214 ± 0.13 | 0.189 ± 0.18 |
| Vastus lateralis | 0.111 ± 0.19 | 0.119 ± 0.14 | 0.242 ± 0.15 | 0.203 ± 0.19 |
| Postcontact | ||||
| Internal oblique | 0.312 ± 0.31 | 0.327 ± 0.39 | 0.240 ± 0.17 | 0.242 ± 0.19 |
| External obliquea,b | 0.169 ± 0.12 | 0.199 ± 0.30 | 0.209 ± 0.16 | 0.177 ± 0.14 |
| Erector spinae | 0.391 ± 0.31 | 0.388 ± 0.31 | 0.346 ± 0.14 | 0.263 ± 0.15 |
| Gluteus maximus | 0.342 ± 0.22 | 0.355 ± 0.31 | 0.252 ± 0.12 | 0.192 ± 0.15 |
| Semitendinosisa | 0.343 ± 0.26 | 0.392 ± 0.30 | 0.381 ± 0.10 | 0.417 ± 0.11 |
| Biceps femoris | 0.236 ± 0.20 | 0.239 ± 0.26 | 0.206 ± 0.14 | 0.173 ± 0.19 |
| Vastus medialis | 0.165 ± 0.10 | 0.201 ± 0.17 | 0.197 ± 0.19 | 0.231 ± 0.14 |
| Vastus lateralis | 0.083 ± 0.10 | 0.094 ± 0.17 | 0.105 ± 0.15 | 0.107 ± 0.11 |
Abbreviation: VPAC, preemptive abdominal contraction.
VPAC effect for the 0.30-m height (P < .05).
VPAC effect for the 0.50-m height (P < .05).
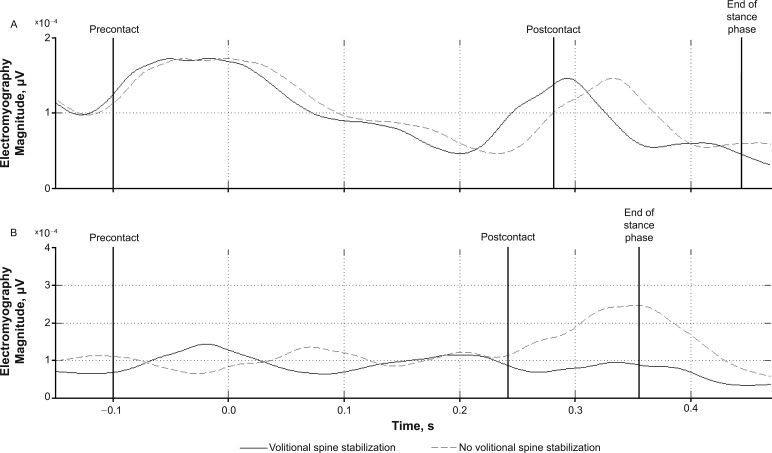
A main effect was observed during the 0.30-m drop vertical-jump–landing condition. External oblique activity increased by 21.8% (0.036 μV) during the VPAC condition versus the no-VPAC condition in the precontact phase (F1,29 = 6.03, P = .02) and by 17.8% (0.030 μV) during the postcontact phase (F1,29 = 6.94, P = .02; Figure 4; Table 3). In the postcontact phase, ST activity was 14.3% (0.049 μV) greater during the VPAC condition (F1,29 = 6.14, P = .02; Figure 5; Table 3). The VPAC produced a 4.0° (9.8%) increase in the total range of knee flexion (F1,29 = 4.78, P = .04) and a 2.7° (8.8%) increase in the total range of knee internal rotation (F1,29 = 4.86, P = .050; Table 1). In addition, the VPAC condition produced a 19.2-Nm (52.2%) decrease in internal knee-abduction moment (F1,7 = 6.070, P = .043) and a 7.6-W (25.6%) decrease in sagittal-plane energy absorption at the knee (F1,29 = 4.354, P = .046; Table 2).
Figure 4.
Linear envelope of external oblique activity of the 0.50-m drop vertical jump from a representative participant. Electromyography variables were evaluated for root mean square amplitude from 0.1 seconds before initial contact (IC; precontact) to IC (time zero) and from IC to the end of the eccentric landing phase (postcontact). Linear envelope processing was used for graphic presentation only.
Figure 5.
Linear envelope of semitendinosis activity of the, A, 0.50-m and, B, 0.30-m drop vertical jumps from a representative participant. Electromyography variables were evaluated for root mean square amplitude from 0.1 seconds before initial contact (IC; precontact) to IC (time zero) and from IC to the end of the eccentric landing phase (postcontact). Linear envelope processing was used for graphic presentation only.
Table 2.
Kinetic Variables for the Right Lower Extremity and Trunk (Mean ± SD)
| Kinetic Variable |
Height |
|||
| 0.30 m |
0.50 m |
|||
| No VPAC |
VPAC |
No VPAC |
VPAC |
|
| Vertical ground reaction force, N | 1352.2 ± 471.9 | 1283.6 ± 379.2 | 1745.2 ± 568.4 | 1623.9 ± 485.7 |
| Ankle-flexion moment, Nm | 59.5 ± 31.5 | 51.6 ± 40.3 | 68.2 ± 42.8 | 69.5 ± 34.3 |
| Ankle-inversion moment, Nm | 11.9 ± 21.8 | 11.7 ± 20.3 | 15.5 ± 28.1 | 11.6 ± 15.8 |
| Knee-flexion moment, Nm | 38.2 ± 38.9 | 38.7 ± 37.8 | −67.9 ± 38.3 | −68.7 ± 46.6 |
| Knee-abduction moment, Nma | −40.2 ± 6.6 | −21.0 ± 6.4 | 46.4 ± 46.6 | 40.5 ± 34.3 |
| Hip-flexion moment, Nm | 143.8 ± 83.5 | 133.1 ± 61.9 | 208.2 ± 86.8 | 200.2 ± 87.3 |
| Hip-abduction moment, Nm | 100.5 ± 215.4 | 54.6 ± 116.1 | 71.7 ± 135.4 | −78.2 ± 189.6 |
| Ankle-energy absorption, W | −13.9 ± 44.7 | −19.8 ± 42.9 | 157.8 ± 274.5 | 94.8 ± 160.0 |
| Knee-energy absorption, Wa | −29.7 ± 64.1 | −37.3 ± 69.0 | 373.1 ± 300.9 | 481.1 ± 286.7 |
| Hip-energy absorption, Wb | −8.8 ± 15.7 | −13.8 ± 20.2 | 301.6 ± 254.3 | 277.6 ± 253.6 |
Abbreviation: VPAC, preemptive abdominal contraction.
VPAC effect for the 0.30-m height (P < .05).
VPAC effect for the 0.50-m height (P < .05).
We observed several main effects during the 0.50-m drop vertical jump-landing condition. External oblique activity increased by 17.3% (0.034 μV) during the VPAC condition compared with the no-VPAC condition in the precontact phase (F1,29 = 6.03, P = .03) but decreased by 15.3% (0.032 μV) during the postcontact phase (F1,29 = 6.94, P = .02; Figure 4; Table 3). In the precontact phase, ST activity was 33.5% (0.055 μV) greater during the VPAC condition than during the no-VPAC condition (F1,29 = 6.14, P = .01; Table 3). The VPAC condition produced a 2.5° (26.8%) increase in knee flexion at contact (F1,29 = 9.41, P = .005; Table 1). In addition, the VPAC condition produced a 1.8° (7.1%) increase in hip-flexion angle at contact (F1,29 = 6.64, P = .02) during the 0.50-m landing. Furthermore, the VPAC produced a 4.0° (55.6%) decrease in the total range of ankle-inversion motion (F1,29 = 4.86, P = .04; Table 1). Finally, the VPAC condition produced a 24.0-W (8.0%) decrease in sagittal-plane energy absorption at the hip (F1,18 = 4.730, P = .045) during the 0.50-m landing phase (Table 2).
DISCUSSION
The purpose of our study was to determine whether a VPAC strategy using the ABM during a drop vertical-jump task altered lower extremity kinematics and kinetics, as well as trunk and lower extremity muscle activity. In addition, we examined differences in these measures between drop vertical-jump activities from 0.30- and 0.50-m heights. Our results partially supported our hypothesis that VPAC would improve neuromuscular and biomechanical measures related to ACL injury and add to the growing body of evidence26,27 that increased proximal stability induced by a VPAC strategy potentially improves the neuromuscular control of more distal segments during dynamic activities. In addition, our prediction that lower extremity EMG and kinematic and kinetic variables would differ between landing heights was supported. The disparities between the 2 drop vertical-jump heights suggest that the system responded differently to the loads encountered during those experiences.
The trunk muscles must be recruited during the landing sequence to control trunk momentum and increase intra-abdominal pressure to improve spine stability.30,41 Abdominal muscle activity increases during the precontact phase of landing and decreases immediately postcontact.21,29,41 This increased activity stiffens the trunk in preparation for impact. Kulas et al41 found that IO activity was greater than EO activity 150 milliseconds before landing. Therefore, IO precontact activation likely did not change with the VPAC maneuver because of the expected increase in activity.41 However, EO precontact activation was higher with VPAC, suggesting a volitional preparatory protective response exceeding the expected automatic precontact elevated activity.21,29,41 Moreover, researchers23 have found that, during the ABM, the EO was consistently more involved than the IO, further supporting the obvious disparity between the muscles' preparatory response during prelanding. Whereas EO postcontact activity remained elevated during the VPAC-condition landings at 0.30 m, the muscle demonstrated less activity during the VPAC condition than the no-VPAC condition postcontact during the 0.50-m landings. This indicates that volitional trunk muscle activation during the increased external load from a 0.50-m drop vertical jump may have been superseded by the system's automatic trunk-muscle responses to increased loads that were governed by motor programming. When landing from this great height, participants may have needed to automatically attend to other functions on cognitive and control levels to maintain control during a more demanding landing sequence. Therefore, they may not have been able to volitionally attend to a heightened volitional abdominal contraction response during that demand, and the system may have defaulted to a motor program, which is typically refined through previous repeated exposure to the stability demands of lower extremity loading and stress.42 These findings suggest that the previously reported changes in landing kinematic and EMG responses during the VPAC conditions may more likely be linked to heightened abdominal activity precontact during the landing sequence, which may have set up the system for enhanced control during the actual loading response. Future investigators should focus on the influence of cognitive and movement distractions on landing responses from various heights.
Finally, the VPAC goal is to increase activation of both the trunk flexors and extensors. However, ES activation levels did not differ between the 2 conditions. This may have been related to the role the ES plays in eccentrically controlling the forward flexion of the trunk during landing, particularly after initial contact.30 Therefore, participants may not be able to further increase ES activation in response to VPAC due to the already high level of activity during the no-VPAC condition.
Activity of the remaining 6 tested muscles increased from precontact to postcontact during both VPAC and no-VPAC conditions, which is consistent with previous research.30 Eccentric contractions of the hip and knee extensors that follow landing dissipate vertical GRF and absorb kinetic energy transferred to the lower limbs.43 The VPAC condition changed the activation level of only 1 lower limb muscle during the 0.50-m drop vertical jump: ST activity increased during the precontact phase of the drop vertical jump. This increase was not sustained during the postcontact phase. In contrast, VPAC up-regulated ST activity postcontact during the 0.30-m drop vertical jump (Figure 5). Therefore, VPAC performance during landing may protect the ACL during different landing phases from different heights because the hamstrings help restrain anterior tibial translation during a landing sequence.15 To further explore this behavior, researchers should examine these variables during a landing response from different angles and when proceeded by different functional activities.
Several lower extremity kinematic changes occurred during the VPAC landing trials, and these were more numerous during the 0.50-m landings. Hip- and knee-flexion angles at contact were greater during landings with a superimposed VPAC only at 0.50 m. Adding the VPAC during the 0.50-m drop vertical jump increased knee and hip flexion at contact by 2.5° and 1.8°, respectively. Reduced hip and knee flexion during landing is linked to ACL injury40; therefore, these results suggest that VPAC use may protect the lower extremity when landing from 0.50 m. This outcome agrees with the results of Shirey et al,27 who found that knee-flexion range of motion increased during a single-legged step-down squat accompanied by a superimposed VPAC. Hip- and knee-flexion angles with VPAC may have been greater only during the 0.50-m landings due to the increased landing height, which requires greater force attenuation created by changes in neuromuscular control. Increased knee flexion precontact may result from VPAC triggering increased ST activity during the precontact phase of the landing sequence, creating a flexion torque on the tibia and increased knee-flexion angle at contact. Whereas the changes in our study were small, any increase in hip-flexion or knee-flexion angle during a landing sequence could increase shock absorption and decrease injury risk, especially when the changes occur during the terminal knee-extension range where injuries are more likely. Similarly, whereas we observed no changes in ankle rotation between VPAC conditions at 0.30 m, we observed appreciable changes in the same variable at 0.50 m. The ankle was less inverted during the VPAC trials at this height, where the VPAC may have enhanced a shock-absorbing response in the ankle region during the landing sequence.
Whereas VPAC performance did not change initial contact angles at 0.30 m, total knee-flexion and rotation range of motion did increase during VPAC trials. This finding may be due to the increased ST activity during jumps with VPAC, which would create a greater flexion torque on the tibia. Moreover, when performing VPAC during the 0.50-m drop vertical jump, individuals exhibited decreased ankle inversion. Along with the increased knee flexion mentioned previously, this places the lower extremity in a more neutral stance position and promotes force attenuation in the lower extremity, potentially reducing injury risk.44
Fewer kinetic changes were observed at either height, but knee-adduction moment and energy absorption decreased with VPAC performance during the 0.30-m landings. Increased valgus force appears to reflect an increased potential for knee injury. For example, Hewett et al45 found that the peak external knee-abduction moment, which is analogous to internal knee-adduction moment in our study, was 26.9 Nm greater in females with ACL injury than in those without ACL injury. The 19.2-Nm decrease in internal knee-adduction moment observed during landing with the ABM may provide protection during a drop vertical-jump sequence. In addition, hip-energy absorption decreased during the 0.50-m landings. This decreased energy absorption may correspond with the previously described decrease in EO activation observed postcontact, further supporting the supersession by automatic programming when landing from increased heights.42
Hip- and trunk-muscle activation influences knee-motion control.13,17−19 For example, weakness and poor control of the hip abductors and external rotators reduce pelvic stabilization, leading to excessive dynamic knee valgus.20,46 In response, controlling pelvic stabilization may influence knee-control measure outcomes. A VPAC activity, such as the ABM, may increase pelvic stability and, thus, improve lower extremity biomechanical responses.24,25 Therefore, VPAC performance may reduce the potential for lower extremity injury by changing control measures at the knee and hip. Moreover, a link appears to exist between LBP and lower extremity injury risk, including ACL injury.47 Given that VPAC performance appears to improve spinal and pelvic stability,23 this type of volitional control response may be especially important during activities such as landing for those with LBP.
We acknowledge limitations associated with inverse-dynamic modeling using the marker set, including skin movement, an anthropometric model, system-tracking errors, and data-smoothing errors. Our participants were given a limited time to learn the VPAC. Hall et al48 found that a single session of VPAC training did not improve EMG amplitudes of the IO, EO, and ES during rapid arm movement or walking in participants with recurrent LBP. Whereas our participants did not have LBP, 1 training session may not have been sufficient to optimize their VPAC performance. However, the increased EO activity during the VPAC condition suggests that they increased trunk-muscle activity when attempting such a strategy, superseding any disadvantage.
Our study was performed in a controlled laboratory environment. Future research is needed to determine whether individuals can maintain this contraction and its beneficial effects in a more open, distractive setting. In addition, focusing on VPAC maintenance in a distractive setting could impair movement outcomes, so researchers should determine the effect of VPAC maintenance on various dynamic performance variables. Finally, investigators should examine the influence of VPAC use on actual injury risk and incidence during various functional activities and whether these findings are influenced by the presence of LBP. Meanwhile, coaches and clinicians can be encouraged to apply this information when teaching athletes or clients to volitionally increase spinal stability. Such instruction could optimize lower extremity performance through core-muscle activation during functional activity to reduce exposure to adverse biomechanical factors associated with lower extremity injury. Researchers should examine the effect of VPAC training on planned landing activity from a height (eg, box jumps) or during competitive encounters, such as returning from a rebound. Through this evaluation, they assess both the role of VPAC on formerly described physical and mechanical measures as discussed and the influence of VPAC on a performer's vigilance toward stabilizing the trunk during dynamic skills.
CONCLUSIONS
Our study represents a novel approach to using core-muscle activation to change important kinematic, kinetic, and neuromuscular control responses during a dynamic vertical-jump sequence. The results provide preliminary evidence that a VPAC strategy during a landing sequence may decrease exposure to biomechanical factors that can contribute to ACL injury when landing from 0.30- and 0.50-m heights using a drop vertical jump. Selected benefits were observed during the 0.50-m drop vertical jump but they were fewer than during the jump from 0.30 m. Such outcomes may have occurred in response to the increased external loads associated with the 0.50-m height. Our data suggest that individuals can be trained to incorporate a VPAC during functional, closed chain activities in a controlled laboratory environment to enhance pelvic stability, improve sensorimotor control and positioning of the lower extremity, and reduce biomechanical factors associated with ACL injury while protecting the lumbar spine.
REFERENCES
- 1. Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. . Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000; 23 6: 573– 578. [DOI] [PubMed] [Google Scholar]
- 2. Arendt E, Dick R. . Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med. 1995; 23 6: 694– 701. [DOI] [PubMed] [Google Scholar]
- 3. Agel J, Klossner D. . Epidemiologic review of collegiate ACL injury rates across 14 sports: National Collegiate Athletic Association Injury Surveillance System data 2004−05 through 2011–12 [abstract]. Br J Sports Med. 2014; 48 7: 560. [Google Scholar]
- 4. Whiting WC, Zernicke RF. . Biomechanics of Musculoskeletal Injury. 2nd ed. Champaign, IL: Human Kinetics; 2008: 149– 156. [Google Scholar]
- 5. Hootman JM, Dick R, Agel J. . Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007; 42 2: 311– 319. [PMC free article] [PubMed] [Google Scholar]
- 6. Withrow TJ, Huston LJ, Wojtys EM, Ashton-Miller JA. . Effect of varying hamstring tension on anterior cruciate ligament strain during in vitro impulsive knee flexion and compression loading. J Bone Joint Surg Am. 2008; 90 4: 815– 823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Markolf KL, O'Neill G, Jackson SR, McAllister DR. . Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004; 32 5: 1144– 1149. [DOI] [PubMed] [Google Scholar]
- 8. Heijne A, Fleming BC, Renstrom PA, Peura GD, Beynnon BD, Werner S. . Strain on the anterior cruciate ligament during closed kinetic chain exercises. Med Sci Sports Exerc. 2004; 36 6: 935– 941. [DOI] [PubMed] [Google Scholar]
- 9. Pflum MA, Shelburne KB, Torry MR, Decker MJ, Pandy MG. . Model prediction of anterior cruciate ligament force during drop-landings. Med Sci Sports Exerc. 2004; 36 11: 1949– 1958. [DOI] [PubMed] [Google Scholar]
- 10. Boden BP, Torg JS, Knowles SB, Hewett TE. . Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009; 37 2: 252– 259. [DOI] [PubMed] [Google Scholar]
- 11. Krosshaug T, Nakamae A, Boden BP, et al. . Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007; 35 3: 359– 367. [DOI] [PubMed] [Google Scholar]
- 12. Levine JW, Kiapour AM, Quatman CE, et al. . Clinically relevant injury patterns after an anterior cruciate ligament injury provide insight into injury mechanisms. Am J Sports Med. 2013; 41 2: 385– 395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hewett TE, Myer GD. . The mechanistic connection between the trunk, knee, and ACL injury. Exerc Sport Sci Rev. 2011; 39 4: 161– 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Myer GD, Ford KR, Hewett TE. . The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J Electromyogr Kinesiol. 2005; 15 2: 181– 189. [DOI] [PubMed] [Google Scholar]
- 15. Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL. . The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999; 32 4: 395– 400. [DOI] [PubMed] [Google Scholar]
- 16. Ebben WP, Fauth ML, Petushek EJ, et al. . Gender-based analysis of hamstring and quadriceps muscle activation during jump landings and cutting. J Strength Cond Res. 2010; 24 2: 408– 415. [DOI] [PubMed] [Google Scholar]
- 17. Hammill RR, Beazell JR, Hart JM. . Neuromuscular consequences of low back pain and core dysfunction. Clin Sports Med. 2008; 27 3: 449– 462, ix. [DOI] [PubMed] [Google Scholar]
- 18. Willson JD, Dougherty CP, Ireland ML, Davis IM. . Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005; 13 5: 316– 325. [DOI] [PubMed] [Google Scholar]
- 19. Zazulak B, Cholewicki J, Reeves NP. . Neuromuscular control of trunk stability: clinical implications for sports injury prevention. J Am Acad Orthop Surg. 2008; 16 9: 497– 505. [PubMed] [Google Scholar]
- 20. Powers CM. . The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40 2: 42– 51. [DOI] [PubMed] [Google Scholar]
- 21. Haddas R, Sawyer SF, Sizer PS Jr, Brooks T, Chyu MC, James CR. . Effects of volitional spine stabilization and lower extremity fatigue on trunk control during landing in individuals with recurrent low back pain. J Orthop Sports Phys Ther. 2016; 46 2: 71– 78. [DOI] [PubMed] [Google Scholar]
- 22. McGill S. . Core training: evidence translating to better performance and injury prevention. Strength Cond J. 2010; 32 3: 33– 46. [Google Scholar]
- 23. Grenier SG, McGill SM. . Quantification of lumbar stability by using 2 different abdominal activation strategies. Arch Phys Med Rehabil. 2007; 88 1: 54– 62. [DOI] [PubMed] [Google Scholar]
- 24. Oh JS, Cynn HS, Won JH, Kwon OY, Yi CH. . Effects of performing an abdominal drawing-in maneuver during prone hip extension exercises on hip and back extensor muscle activity and amount of anterior pelvic tilt. J Orthop Sports Phys Ther. 2007; 37 6: 320– 324. [DOI] [PubMed] [Google Scholar]
- 25. Park KN, Cynn HS, Kwon OY, et al. . Effects of the abdominal drawing-in maneuver on muscle activity, pelvic motions, and knee flexion during active prone knee flexion in patients with lumbar extension rotation syndrome. Arch Phys Med Rehabil. 2011; 92 9: 1477– 1483. [DOI] [PubMed] [Google Scholar]
- 26. Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. . The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999; 27 6: 699– 706. [DOI] [PubMed] [Google Scholar]
- 27. Shirey M, Hurlbutt M, Johansen N, King GW, Wilkinson SG, Hoover DL. . The influence of core musculature engagement on hip and knee kinematics in women during a single leg squat. Int J Sports Phys Ther. 2012; 7 1: 1– 12. [PMC free article] [PubMed] [Google Scholar]
- 28. Hewett TE, Torg JS, Boden BP. . Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009; 43 6: 417– 422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haddas R, James CR, Hooper TL. . Lower extremity fatigue, sex, and landing performance in a population with recurrent low back pain. J Athl Train. 2015; 50 4: 378– 384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Iida Y, Kanehisa H, Inaba Y, Nakazawa K. . Activity modulations of trunk and lower limb muscles during impact-absorbing landing. J Electromyogr Kinesiol. 2011; 21 4: 602– 609. [DOI] [PubMed] [Google Scholar]
- 31. Kulas A, Zalewski P, Hortobagyi T, DeVita P. . Effects of added trunk load and corresponding trunk position adaptations on lower extremity biomechanics during drop-landings. J Biomech. 2008; 41 1: 180– 185. [DOI] [PubMed] [Google Scholar]
- 32. James CR, Dufek JS, Bates BT. . Effects of stretch shortening cycle exercise fatigue on stress fracture injury risk during landing. Res Q Exerc Sport. 2006; 77 1: 1– 13. [DOI] [PubMed] [Google Scholar]
- 33. Portney LG, Watkins MP. . Foundation of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, NJ: Julie Levin Alexander; 2009. [Google Scholar]
- 34. Noyes FR, Barber SD, Mangine RE. . Bone-patellar ligament-bone and fascia lata allografts for reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1990; 72 8: 1125– 1136. [PubMed] [Google Scholar]
- 35. Wojtys EM, Wylie BB, Huston LJ. . The effects of muscle fatigue on neuromuscular function and anterior tibial translation in healthy knees. Am J Sports Med. 1996; 24 5: 615– 622. [DOI] [PubMed] [Google Scholar]
- 36. Vaughan CL, Davis BL, O'Conner JC. . Dynamics of Human Gait . 2nd ed. Cape Town, . South Africa: Kiboho Publishers; 1999: 22–29. [Google Scholar]
- 37. Butler HL, Hubley-Kozey CL, Kozey JW. . Electromyographic assessment of trunk muscle activation amplitudes during a simulated lifting task using pattern recognition techniques. J Electromyogr Kinesiol. 2009; 19 6: E505– E512. [DOI] [PubMed] [Google Scholar]
- 38. Rainoldi A, Melchiorri G, Caruso I. . A method for positioning electrodes during surface EMG recordings in lower limb muscles. J Neurosci Methods. 2004; 134 1: 37– 43. [DOI] [PubMed] [Google Scholar]
- 39. Robertson GE, Caldwell GE, Hamill J, Kamen G, Whittlesey SN. . Research Methods in Biomechanics. Champaign, IL: Human Kinetics; 2004: 109– 129, 152– 167. [Google Scholar]
- 40. Winter DA. . Biomechanics and Motor Control of Human Movement. 4th ed. New York, NY: Wiley; 2009: 257– 272. [Google Scholar]
- 41. Kulas AS, Schmitz RJ, Shultz SJ, Henning JM, Perrin DH. . Sex-specific abdominal activation strategies during landing. J Athl Train. 2006; 41 4: 381– 386. [PMC free article] [PubMed] [Google Scholar]
- 42. Schmidt RA, Lee TD. . Motor Control and Learning: A Behavioral Emphasis. 5th ed. Champaign, IL: Human Kinetics; 2011. [Google Scholar]
- 43. Norcross MF, Blackburn JT, Goerger BM, Padua DA. . The association between lower extremity energy absorption and biomechanical factors related to anterior cruciate ligament injury. Clin Biomech (Bristol, Avon). 2010; 25 10: 1031– 1036. [DOI] [PubMed] [Google Scholar]
- 44. Zhang SN, Bates BT, Dufek JS. . Contributions of lower extremity joints to energy dissipation during landings. Med Sci Sports Exerc. 2000; 32 4: 812– 819. [DOI] [PubMed] [Google Scholar]
- 45. Hewett TE, Myer GD, Ford KR, et al. . Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005; 33 4: 492– 501. [DOI] [PubMed] [Google Scholar]
- 46. Imwalle LE, Myer GD, Ford KR, Hewett TE. . Relationship between hip and knee kinematics in athletic women during cutting maneuvers: a possible link to noncontact anterior cruciate ligament injury and prevention. J Strength Cond Res. 2009; 23 8: 2223– 2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wilkerson GB, Colston MA. . A refined prediction model for core and lower extremity sprains and strains among collegiate football players. J Athl Train. 2015; 50 6: 643– 650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hall L, Tsao H, MacDonald D, Coppieters M, Hodges PW. . Immediate effects of co-contraction training on motor control of the trunk muscles in people with recurrent low back pain. J Electromyogr Kinesiol. 2009; 19 5: 763– 773. [DOI] [PubMed] [Google Scholar]