Abstract
Background
The hip resurfacing concept was developed for young and active patients, especially for femoral bone stock preservation. However, concerns about metal-on-metal bearings with adverse reactions to metal debris have led to a drop off in hip-resurfacing procedures.
Questions/Purposes
The goal of this review is to evaluate our current knowledge of survivorship of second-generation hip resurfacing devices and elaborate international perspectives for product improvement.
Methods
A comprehensive literature search provided information on national joint arthroplasty registers worldwide with a minimum of 3000 reported hip resurfacings. It culminated in the analysis of six registers.
Results
Long-term data showed that available hip resurfacing device survivorship ranged from 95 to 99.7% with 10 years of follow-up, in selected patient populations. The criteria for success were well known, male gender, good bone quality, head component size greater than 48 mm, and cup inclination less than 45°. On the other hand, the recent recall of some hip-resurfacing devices has resulted in huge medico-legal problems and has discredited all implants. It has brought about the recent evolution of hip resurfacing. Femoral fixation is now available for cemented and cementless surfaces. Bearings are still always metal-on-metal, but new types have come on board. Newer designs suggest that ceramic-on-ceramic, cross-linked polyethylene, and oxinium may be applied in this configuration.
Conclusions
In 2015, the evolution of hip resurfacing is ongoing in terms of implant design, alternative bearings, and implant fixation with hopes of improving survivorship.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9511-y) contains supplementary material, which is available to authorized users.
Keywords: hip resurfacing, cementless, cement, bearing
Introduction
The hip-resurfacing concept was first developed for young and active patients, particularly because of femoral bone stock preservation [19]. In recent years, a younger patient population is seeking hip replacement to restore high-impact lifestyles [8]. Hip resurfacing appeals to this younger patient demographic due to the theoretical benefits of femoral bone conservation, restoration of biomechanical hip parameters (leg length, femoral offset, etc.), low rate of dislocation, physiological femoral loading, reduced prevalence of thromboembolic phenomena, and the possibility of returning to sport activities, etc. [10, 17].
Despite these theoretical advantages, hip resurfacing is still surrounded by controversy [2]. The first generation of devices was abandoned during the 1980s due to high wear rates that correlated directly with large-diameter heads in polyethylene bearings [1, 23]. The second generation was designed as metal-on-metal bearings to reduce wear [5], but the use of large femoral heads in resurfacing cups led to adverse reactions to metal debris (ARMD) with the occurrence of pseudo-tumors, aseptic lymphoctye-dominated vasculitis-associated lesions (ALVAL), metallosis, and so on [11].
The present review evaluates current knowledge of the survivorship of second-generation metal-on-metal hip-resurfacing devices and proposes international perspectives for needed improvements.
Methods
A comprehensive literature search of PubMed was undertaken to find national joint arthroplasty registries worldwide, using the key words “hip resurfacing.” To reduce bias of this search for national registers, those without a minimum of 3000 reported hip resurfacings were discarded. This resulted in the analysis of five registries (Australian, Finnish, New Zealand, Canadian, and UK/Wales), the basis of the current review. Revision rates served as the main outcome parameter, but other revision risk factors, such as head component diameter, gender, and cup inclination, were also analyzed.
We propose potential benefits for use of hip resurfacing for the future including component fixation (cement or cementless), metal-on-metal bearing alternatives, and component design.
Results
The Australian register reported 266,645 primary hip arthroplasties (https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013). The revision rate at 10-year follow-up was 6.6% (95% CI 6.4–6.8) for conventional total hip arthroplasty (THA) and 8.8% (95% CI 7.9–9.0) for THA in under 55-year-old patients. The hip-resurfacing revision rates were 7.1% as opposed to 5.9% (95% CI 5.2–6.6) for components with a head diameter greater than or equal to 48 mm. This criterion highlighted the importance of head diameter. Clearly, smaller components were at greater risk of revision than larger ones.
Hip resurfacing component size was the main implant characteristic of all registers analyzed. In the Australian register, after adjusting for age and gender, the risk of revision for femoral components with head size less than 44 mm was more than five times greater than for femoral components larger than 55 mm. The revision risk with components ranging from 45 to 49 mm was three times greater than the revision risk of components larger than 55 mm. Component size was a major revision risk prognosticator and seemed even more important than gender ratio. On the other hand, the threshold below which resurfacing should be not considered was not clearly defined. To many authors, a minimum size of 48 mm should be the lower limit.
Currently, in Finland, 98% of primary hip arthroplasty implantations have been recorded (https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013). Between 2001 and 2009, 48,409 primary hip arthroplasties and 4401 hip resurfacings were performed. This registry compared the revision risks of resurfacing after THA. Median follow-up time was 3.5 (0–9) years for resurfacing and 3.9 (0–9) years for THA. Hip resurfacing was found to have short-term survivorship comparable to THA. Gender appeared to be a very important risk factor, as female patients had twice the risk of revision compared to males.
The Wales registry recorded 539,372 hip arthroplasties (http://www.njrcentre.org.uk/njrcentre/default.aspx). The revision rate at 9 years of follow-up was 6.7% (95% CI 6.4–7) for THA, 8.1% (7.4–8.8) for hip resurfacing (Birmingham Hip Resurfacing BHR©), and 3.2% (CI 95% 2.6–3.9) for resurfacing with head diameter greater than 48 mm.
The New Zealand registry is based on 85,769 hip arthroplasties (http://www.nzoa.org.nz/nz-joint-registry). The revision rate/100 observation years was 0.71 (0.6–0.7) for THA, 1.2 (0.9–1.1) for THA in patients under 55 years old, 0.9 (0.6–1.2) for resurfacing (BHR©), and 0.75 (0.5–1.1) for resurfacing with head diameter greater than 48 mm.
The Canadian registry was based on nine Canadian academic centres and reported 3 years of follow-up; 99.9% of 3432 hip-resurfacing patients experienced no implant failure attributed to metal wear debris [7].
In all registers, implant design had a strong influence on revision rates. The ASR© (DePuy) component had higher revision risk than others. In the Australian registry (https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013), the yearly cumulative percentage of revision of primary total hip-resurfacing replacement was 5.1% (4.6–6.6) for BHR© at 7 years of follow-up. In comparison, revision rates were 23.4 (20.2–26.9) for ASR© and 12.4 (8.7–17.6) for Cormet©.
Another issue noticed in the Finnish register was procedure volume. Low hospital procedure volume worsened hip-resurfacing outcome. A threshold of performance of 100 hip resurfacings separated low-volume from high-volume hospitals (http://www.njrcentre.org.uk/njrcentre/default.aspx).
Another conclusion drawn from the registries concerned THA and ASR© outcomes according to preoperative diagnosis. The yearly cumulative percent survival of patients with primary THA and a primary diagnosis of osteoarthritis in the Australian registry was 96.6% (96–97.2) at 10 years for resurfacing and only 74.5% (73.9–75.1) for THA.
In all six registries, the BHR© was the only implant that had a reduced risk of revision compared to THA. To date, the BHR© has exceeded 170,000 implantations since 1997 and still stands today as the global market leader (considered as the gold standard in resurfacing). Since 2009, with the recognition of the complications associated with the generation of metal debris, competitors have dropped off the map. In the Australian registry (https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013), resurfacings numbered 1547 in 2003 (with 6 different devices), 965 in 2010 (with 8 different designs), and 392 in 2013 (with 4 different devices).
In the European hip-resurfacing market, the BHR© represents 72% of sales (Smith and Nephew data). In the UK registry (http://www.njrcentre.org.uk/njrcentre/default.aspx), temporal percentage changes with each fixation method used in THA dropped off for resurfacing and metal-on-metal bearings. Resurfacing accounted for 10% of primary hip replacements in 2003 and only 0.5% in 2013.
According to the conclusions of previous registries (https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013; http://www.njrcentre.org.uk/njrcentre/default.aspx(http://www.nzoa.org.nz/nz-joint-registry) [7] on head diameter, device type, gender ratio, and learning curve, the French market appears to be experiencing very interesting times. In 2012–2013, the French health authorities (Haute autorité de santé) approved only two implants (BHR© and Conserve Plus©). Only high-volume surgeons (more than 50 cases per year) were allowed to participate, and implant head diameter was required to be greater than 48 mm (http://www.has-sante.fr/portail/upload/docs/evamed/CEPP). As a result, only a few authorized centers persisted, with 97.5% of French hip resurfacings performed in one center (Orthopedic Service, Université Lille). In the French registry, of the 1183 cases treated since 2013 as per Department of Health recommendations, the implant survival rate was 99.1% at 4 years (95% CI 98.8–99.2%) and 99.6% if sepsis was excluded at 4 years (95% CI 99.3–99.7%) [19].
Discussion
Hip resurfacing has evolved with recent trends and new perspectives. To avoid the problem of cement penetration into the femoral head, some authors have developed cementless femoral components. This has led to incomplete femoral seating, abnormal cement mantle thickness, thermal injury, bone necrosis, and femoral head collapse [14]. In fact, cement appears to be a weak link when long-term femoral component fixation is considered [16]. On the other hand, it is a shock absorber at the prosthesis/bone interface, absorbing the stiffness of metal alloys and harmoniously distributing weakness on bone [18].
Two types of cementless femoral devices have been developed according to this concept, the conventional cementless femoral components (Fig. 1) and the BMHR© (Birmingham mid-head resection (Figs. 2 and 3)). The BMHR© is an alternative bone-conserving hip device for young and active patients who are unsuitable for conventional hip resurfacing [22]. For example, conventional resurfacing is not indicated in the presence of femoral head avascular necrosis and/or large femoral cysts. The BMHR© comprises resection through the middle of the head after necrotic bone removal. The remaining femoral bone is cone shaped. An uncemented stem is fitted to the neck and impacted with large metal-on-metal head diameter. Femoral component stability is assumed by the titanium stem with bone ingrowth. In a series of 164 patients (171 hips) performed by designer during 5 years with mean follow-up of 3.5 years, 4 revisions were observed (with 2 femoral failures). Survivorship was 97.4 and 98.7%, respectively, for revision for any reason and femoral failure [22]. Rahman et al. [25] found no failures in 35 consecutive procedures (34 patients) performed by an independent surgeon with mean follow-up of 2.8 years. These authors stated that the BMHR© is an excellent alternative to conventional THA in patients with poor femoral head bone quality who are unsuitable for standard resurfacing [25].
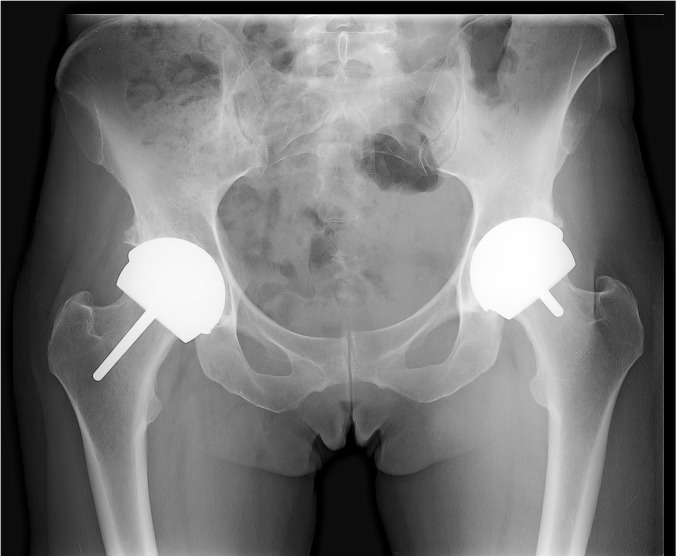
Fig. 1.
Pelvic anteroposterior radiograph of a 38-year-old female marathon runner with bilateral Conserve Plus© hip resurfacing. The femoral component was cemented on the right side and impacted with a cementless fit-and-fill component on the left side. The stem was shorter on the left stem to avoid femoral neck stress shielding.
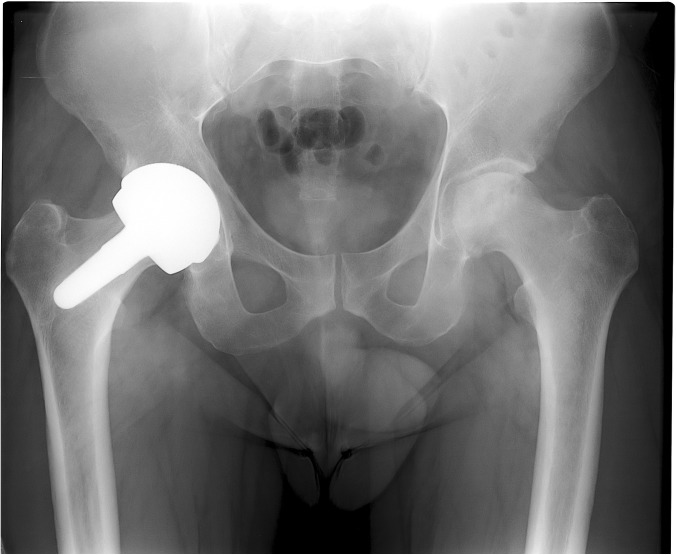
Fig. 2.
Pelvic anteroposterior radiograph of right avascular hip osteonecrosis in a 35-year-old man.
Fig. 3.
BMHR© hip resurfacing required because of head necrosis volume. Fixation was secured into the remaining head and femoral neck.
In another series from an independent center, 49 BMHR© in 47 patients were analyzed with mean follow-up of 6 years [3]. Survivorship was 100% with excellent clinical scores, but 16% of hips presented neck osteolysis, which was strongly associated with pseudo-tumor. No differences in metal ion levels were observed between the osteolysis group and the rest of the cohort. These authors recommended annual clinical and radiological follow-up to avoid the occurrence of large osteolysis [3]. With neck-preserving implants, radiological analysis detected a characteristic pattern of proximal femoral bone loss, with distal cortical hypertrophy, and should be assessed with longer follow-up [26]. On the other hand, Itayem et al. [15] reported excellent stability of the BHMR©. There was no evidence of early migration or loosening of BMHR© components at 2 years compared to cemented femoral components in conventional THA [15].
The second cementless possibility is the implantation of femoral components with porous coating on the under-surface (hydroxy-apatite coating on grit-blasted plasma spray). With Cormet©, Spencer [29] found that survivorship was 95% at 5 years of follow-up and higher than the rate achieved with cemented femoral fixation (91% at 8 years of follow-up). This indicates that femoral fixation is vital for survivorship. Experience with porous-coated Biomet Recap© devices (titanium plasma spray on the femoral component) disclosed similar failure rates (2%) in the uncemented and cemented groups [21].
Other authors reported slightly better survivorship with cementless femoral component resurfacing. In a large series of more than 1000 uncemented Biomet©, Gross and Liu [13] found excellent survivorship (98.5%). Moreover, when they compared cemented femoral components (740 cases) and cementless devices (1300 cases), they noticed better survivorship in the cementless group (99 versus 98% at 2 years) [13]. Experience with the Conserve Plus© cementless device confirmed this conclusion. In a series of 94 cementless Conserve Plus© implants in 90 patients with short follow-up of 13.1 [5, 11] (https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013; http://www.njrcentre.org.uk/njrcentre/default.aspx; http://www.nzoa.org.nz/nz-joint-registry) [7, 27] (http://www.has-sante.fr/portail/upload/docs/evamed/CEPP) [14] months, survivorship was 100% [9]. Cementless “fit and fill” femoral-side fixation should be considered for future resurfacing device production.
In recent years, numerous reports of adverse local tissue reaction have raised doubts in the orthopedic community about the benefits of metal-on-metal implants in resurfacing. To avoid complications with metallic ion release, other bearings must be contemplated. Ceramic-on-ceramic bearings were introduced by some authors [4, 20, 30], but rapid failure occurred, and to date, they do not recommend this particular type of ceramic-on-ceramic bearing for hip resurfacing. Matharu et al. [20] described very early failure of five ceramic-on-ceramic hip resurfacings. The material incorporated in cup inserts was a ceramic composite with 2/3 polyurethane and 1/3 alumina-ceramic. All cases were revised because of dramatically elevated metallic ion levels. This finding was directly correlated with ceramic liner fracture and abnormal wear of ceramic femoral head coating [20].
The situation was similar with a femoral component of cobalt-chrome (Co-Cr) and “ceramicized” coating [30]. The patient rapidly developed soft-tissue masses from metal allergy as ceramic-on-ceramic components were overlaid on metal bases (“ceramicization”) [4]. The risk of squeaking hips with large femoral ceramic heads appears to be too significant to recommend their inclusion [30]. Another bearing for conventional THA also seems to be used for resurfacing, a metallic femoral head with cross-linked polyethylene insert in a cementless cup. The problem of minimal polyethylene insert thickness needs to be addressed by much larger cups (10 mm more than head diameter) and “aggressive acetabular bone growth.” Some authors have, however, undertaken hip resurfacing with small, 4-mm-thick polyethylene implants (<49 mm). Prichett [24] reported 96% survivorship in a series of 160 resurfacings (144 patients with mean follow-up of 11.5 years). Medial acetabular wall thickness averaged 7.3 mm (1.5–14.9). Pritchett found a low rate of femoral head penetration and strongly suggested polyethylene for all femoral head sizes less than 48 mm [24]. Oxinium (oxidized zirconium) was indicated as a suitable alternative bearing [6]. This surface possibly combines the fracture resistance of metal with the wear resistance of ceramics. In vitro studies have demonstrated that oxinium/polyethylene bearings for hip and knee implantation show perfect wear resistance (greater than that of Co-Cr) [12, 28]. Perhaps oxinium-on-oxinium bearings could be developed for hip resurfacing in a few years.
In conclusion, metal-on-metal hip resurfacing is not a new surgical procedure. Devices remaining on the orthopedic market have been followed in many clinical trials and multicenter series for more than 15 years. However, some changes must be made to improve the results, implant design, implant fixation, cup inclination, etc. To date, hip resurfacing is closely linked with metal-on-metal bearings. Thus, the manufacturing quality of these bearings must be precise for clearance, roughness, porous coating, carbide level, alloy resistance, and so on. New bearings have to be developed to minimize the potential side effects of metallic ion release.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Julien Girard, MD, PhD, reports grants from Microport and Smith & Nephew, outside the work.
Human/Animal Rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
The work was performed at Université Lille Nord de France.
References
- 1.Amstutz HC, Beaule PE, Dorey FJ, et al. Metal-on-metal hybrid surface arthroplasty: two- to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. doi: 10.2106/00004623-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Le Duff MJ. Hip resurfacing: a 40-year perspective. HSS J. 2012;8:275–82. doi: 10.1007/s11420-012-9293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asaad A, Hart A, Khoo MM, et al. Frequent femoral neck osteolysis with Birmingham mid-head resection resurfacing arthroplasty in young patients. Clin Orthop Relat Res. 2015;S1:1–9. doi: 10.1007/s11999-015-4348-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atrey A, Waite J, Hart A, et al. Failure of a ceramic-on-ceramic hip resurfacing due to metallosis. JBJS Case Connect. 2014;26 doi: 10.2106/JBJS.CC.M.00128. [DOI] [PubMed] [Google Scholar]
- 5.Beaule PE, Dorey FJ, LeDuff M, et al. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Bourne RB, Barrack R, Rorabeck CH, et al. Arthroplasty options for the young patient: oxinium on cross linked polyethylene. Clin Orthop Relat Res. 2005;441:159–67. doi: 10.1097/01.blo.0000193813.08458.e2. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Hip Resurfacing Group A survey on the prevalence of pseudotumours with MoM hip resurfacings in Canadian academic centres. J Bone Joint Surg Am. 2011;93:118–21. doi: 10.2106/JBJS.J.01848. [DOI] [PubMed] [Google Scholar]
- 8.Fouilleron N, Wavreille G, Endjah N, et al. Running activity after hip resurfacing arthroplasty: a prospective study. Am J Sports Med. 2012;40:889–94. doi: 10.1177/0363546511434564. [DOI] [PubMed] [Google Scholar]
- 9.Girard J. Is it time for cementless hip resurfacing? HSS J. 2012;8:245–50. doi: 10.1007/s11420-012-9295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girard J, Lavigne M, Vendittoli PA, et al. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br. 2006;88:721–6. doi: 10.1302/0301-620X.88B6.17447. [DOI] [PubMed] [Google Scholar]
- 11.Glyn-Jones S, Pandit H, Kwon YM, et al. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br. 2009;91:1566–74. doi: 10.1302/0301-620X.91B12.22287. [DOI] [PubMed] [Google Scholar]
- 12.Good V, Ries M, Barrack RL, et al. Reduced wear with oxidized zirconium femoral heads. J Bone Joint Surg Am. 2003;85-A(Suppl 4):105–10. doi: 10.2106/00004623-200300004-00013. [DOI] [PubMed] [Google Scholar]
- 13.Gross TP, Liu F. Metal-on-metal hip resurfacing with an uncemented femoral component. A seven-year follow-up study. J Bone Joint Surg Am. 2008;90:32–7. doi: 10.2106/JBJS.H.00614. [DOI] [PubMed] [Google Scholar]
- 14.Gross TP, Liu F. The first 100 fully porous-coated femoral components in hip resurfacing. Bull NYU Hosp Jt Dis. 2011;69:S30–5. [PubMed] [Google Scholar]
- 15.Itayem R, Arndt A, Nistor L, et al. Stability of the Birmingham hip resurfacing arthroplasty at two years. A radiostereophotogrammetric analysis study. J Bone Joint Surg Br. 2005;87:158–62. doi: 10.1302/0301-620X.87B2.15394. [DOI] [PubMed] [Google Scholar]
- 16.Katrana P, Crawford JR, Vowler S, et al. Femoral neck resorption after hip resurfacing arthroplasty a comparison of cemented and uncemented prostheses. J Bone Joint Surg Br. 2006;88:S234. doi: 10.2106/00004623-200609001-00008. [DOI] [Google Scholar]
- 17.Kishida Y, Sugano N, Nishii T, et al. Preservation of the bone mineral density of the femur after surface replacement of the hip. J Bone Joint Surg Br. 2004;86:185–9. doi: 10.1302/0301-620X.86B2.14338. [DOI] [PubMed] [Google Scholar]
- 18.Lilikakis AK, Vowler SL, Villar RN. Hydroxyapatite-coated femoral implant in metal-on-metal resurfacing hip arthroplasty: minimum of two years follow-up. Orthop Clin North Am. 2005;36:215–22. doi: 10.1016/j.ocl.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Lons A, Arnould A, Pommepuy T, et al. Excellent short-term results of hip resurfacing in a selected population of young patients. Orthop Traumatil Surg Res. 2015;101(6):661–5. doi: 10.1016/j.otsr.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Matharu GS, Daniel J, Ziaee H, et al. Failure of a novel ceramic-on-ceramic hip resurfacing prosthesis. J Arthroplasty. 2015;30:416–8. doi: 10.1016/j.arth.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 21.Mazzullo S, Paolini M, Verdi C. Numerical simulation of thermal bone necrosis during cementation of femoral prostheses. J Math Biol. 1991;29:475–94. doi: 10.1007/BF00160473. [DOI] [PubMed] [Google Scholar]
- 22.McMinn DJ, Pradhan C, Ziaee H, et al. Is mid-head resection a durable conservative option in the presence of poor femoral bone quality and distorted anatomy? Clin Orthop Relat Res. 2011;469:1589–97. doi: 10.1007/s11999-010-1739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Migaud H, Putman S, Combes A, et al. Metal-on-metal bearing: is this the end of the line? We do not think so. HSS J. 2012;8:262–9. doi: 10.1007/s11420-012-9300-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pritchett J. Highly cross-linked polyethylene for hip resurfacing: results at 10 years in patients under age 50. ISTA (International Society for Technology in Arthroplasty), Vienna, 2015, 11A-6.
- 25.Rahman L, Muirhead-Allwood SK. The Birmingham mid-head resection arthroplasty—minimum two year clinical and radiological follow-up: an independent single surgeon series. Hip Int 2011; 21(3). doi: 10.5301/HIP.2011.8407 [DOI] [PubMed]
- 26.Rajakulendran K, Field RE. Neck-preserving femoral stems. HSS J. 2012;8:295–303. doi: 10.1007/s11420-012-9302-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seppänen M, Mäkelä K, Virolainen P, et al. Hip resurfacing arthroplasty: short-term survivorship of 4,401 hips from the Finnish Arthroplasty Register. Acta Orthop. 2012;83:207–13. doi: 10.3109/17453674.2012.693016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spector BM, Ries MD, Bourne RB, et al. Wear performance of ultra-high molecular weight polyethylene on oxidized zirconium total knee femoral components. J Bone Joint Surg Am. 2001;83:80–6. doi: 10.2106/00004623-200100022-00004. [DOI] [PubMed] [Google Scholar]
- 29.Spencer RF. Evolution in hip resurfacing design and contemporary experience with an uncemented device. J Bone Joint Surg Am. 2011;93:84–8. doi: 10.2106/JBJS.J.01716. [DOI] [PubMed] [Google Scholar]
- 30.Su EP. Ceramic-ceramic bearing: too unpredictable to use it regularly. HSS J. 2012;8:287–90. doi: 10.1007/s11420-012-9289-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)