Abstract
Plantar fascia (PF) disorders commonly cause heel pain and disability in the general population. Imaging is often required to confirm diagnosis. This review article aims to provide simple and systematic guidelines for imaging assessment of PF disease, focussing on key findings detectable on plain radiography, ultrasound and magnetic resonance imaging (MRI). Sonographic characteristics of plantar fasciitis include PF thickening, loss of fibrillar structure, perifascial collections, calcifications and hyperaemia on Doppler imaging. Thickening and signal changes in the PF as well as oedema of adjacent soft tissues and bone marrow can be assessed on MRI. Radiographic findings of plantar fasciitis include PF thickening, cortical irregularities and abnormalities in the fat pad located deep below the PF. Plantar fibromatosis appears as well-demarcated, nodular thickenings that are iso-hypoechoic on ultrasound and show low-signal intensity on MRI. PF tears present with partial or complete fibre interruption on both ultrasound and MRI. Imaging description of further PF disorders, including xanthoma, diabetic fascial disease, foreign-body reactions and plantar infections, is detailed in the main text. Ultrasound and MRI should be considered as first- and second-line modalities for assessment of PF disorders, respectively. Indirect findings of PF disease can be ruled out on plain radiography.
Teaching Points
• PF disorders commonly cause heel pain and disability in the general population.
• Imaging is often required to confirm diagnosis or reveal concomitant injuries.
• Ultrasound and MRI respectively represent the first- and second-line modalities for diagnosis.
• Indirect findings of PF disease can be ruled out on plain radiography.
Keywords: Plantar fascia, Fasciitis, Fibromatosis, Tear, Imaging
Introduction
Plantar fascia (PF) disorders are common in the adult population [1]. They cause pain and disability and may curtail the performance of athletic activities, work-related duties or routine tasks [2]. Imaging is of great help for achieving correct diagnosis, prompting appropriate treatment and aiding in the determination of prognosis. Awareness of the normal and pathological imaging appearance of the PF is thus required. This review article aims to provide radiologists and clinicians with simple and systematic guidelines for the evaluation of PF disorders, specifically focussing on key features suggestive of PF disease that have to be detected on conventional radiograph, ultrasound and magnetic resonance imaging (MRI). These guidelines are generated from our centres’ experience in combination, as indicated by the references in the text, with a thorough analysis of the last 20 years’ literature (1996–2016). A systematic search of the literature was carried out in PubMed using the keywords “plantar fascia” or “plantar aponeurosis” combined with “radiography”, “X-ray”, “ultrasound”, “sonography”, “magnetic resonance imaging” or “imaging”, even combined with “fasciitis”, “fibromatosis”, “tear”, “rupture”, “xanthoma”, “diabetes mellitus”, “infection” or “foreign body”. Additionally, the references of identified publications were checked. Original studies and review articles in English dealing with imaging description of PF and related disorders were included. Case reports and case series were selected according to clinical relevance.
Anatomy and function of the PF
The PF (Fig. 1), also called the plantar aponeurosis, is a strong connective tissue structure that helps maintain the longitudinal arch of the foot [3, 4]. The PF consists of three bundles: central, lateral and medial. The central component is proximally thick and distally thin and is the thickest of the three. It arises from the medial tubercle of the calcaneus and extends distally becoming broader and covering the plantar surface of the flexor digitorum brevis muscle. Distally, it divides into five digitations that insert into the metatarsophalangeal joints. The lateral portion is also proximally thick and distally thin. It arises from the lateral margin of the medial calcaneal tubercle, covers the plantar surface of the abductor digiti minimi muscle and inserts into the fifth metatarsal joint capsule. The medial portion is thinner than the others. It arises from the midportion of the central bundle, covers the plantar surface of the abductor hallucis muscle and inserts into the first metatarsal joint capsule [5]. The mean maximal thickness of the PF has been reported as 4.0 mm in its central bundle, 2.3 mm in its lateral bundle and 0.6 mm in its medial bundle [6]. Overall, PF thickness is greater in men than in women [6]. Histologically, the PF is mostly composed of type I collagen fibres forming bundles arranged in a proximal-distal direction, with a few transverse and vertical collagen fibres. These large fibrous bundles are embedded within a matrix of loose connective tissue containing type III collagen and a few elastic fibres [5].
Fig. 1.
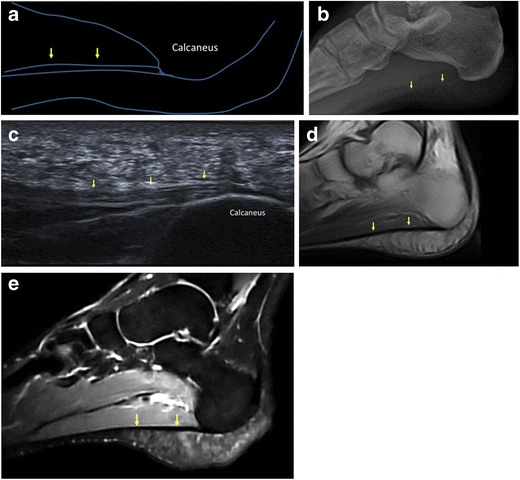
Normal plantar fascia. A schematic representation (a) and lateral plain radiograph (b) show the normal PF (arrows). On sagittal ultrasound scan, the normal PF (arrows) appears as a fibrillar ligamentous structure (c). On MRI, the normal PF (arrows) is seen as a thin band of low signal intensity on both T1-weighted (d) and fluid-sensitive (e) images
General features of PF disorders
Plantar fasciitis (Figs. 2, 3, and 4) is the most common injury of the PF and is estimated to induce more than 1 million patients to seek treatment annually [7]. Despite its name, plantar fasciitis has a degenerative rather than inflammatory nature and is related to overuse trauma leading to microtears [8]; thus, the term “plantar fasciopathy” is often preferred. The proximal third of the central bundle of the PF is classically involved; however, distal plantar fasciitis has recently been recognised as a cause of recalcitrant heel pain [9]. The aetiology of plantar fasciitis is multifactorial. Biomechanical risk factors include those causing repetitive stress on the PF, such as foot deformities, improper footwear, increased body mass index and activities that involve prolonged walking, running or standing [10–12]. Among the medical conditions associated with plantar fasciitis, the most notable are seronegative spondyloarthropathies and rheumatoid arthritis [13–16]. Plantar calcaneal spurs, also known as calcaneal enthesophytes, have been investigated in great detail as a possible cause of plantar fasciitis [17–20], but they are not specific and also occur in asymptomatic individuals. The diagnosis of plantar fasciitis generally relies on clinical history and physical examination. The main symptoms include pain and stiffness in the morning, or pain at the beginning of activity after rest. Physical examination reveals tenderness at the origin of the PF and impaired dorsiflexion of the ankle and extension of the toes [21–24]. Although generally self-limiting, plantar fasciitis may result in physical inactivity and impact quality of life. Imaging can aid in the diagnosis, particularly in recalcitrant cases or may rule out other heel pathology [9, 22].
Fig. 2.
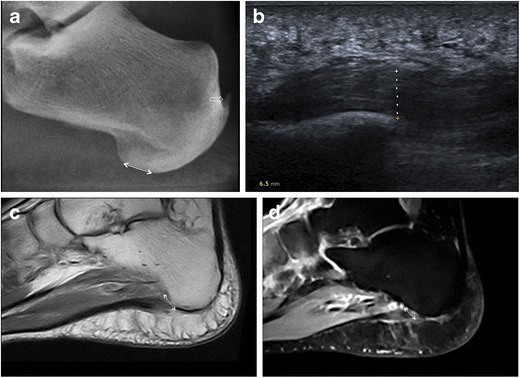
Plantar fasciitis. Lateral plain radiograph highlights an increase in the distance between subcutaneous fat and intrinsic muscles of the foot at the calcaneal insertion of the PF as an indirect sign of plantar fasciitis (double-head arrow); calcific enthesopathy of the Achilles tendon is also seen (open arrow) (a). On ultrasound, plantar fasciitis presents with PF thickening (dashed line, 6.5 mm), a hypoechoic appearance and loss of fibrillar pattern (b). MRI confirms thickening of the PF at its calcaneal origin (double-head arrow) with intrasubstance areas of intermediate and high signal intensity on T1-weighted (c) and fluid-sensitive (d) images, respectively
Fig. 3.
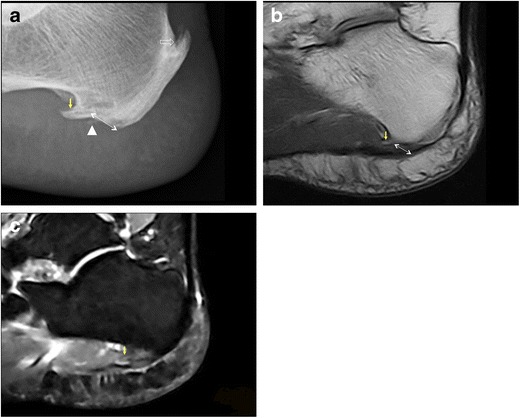
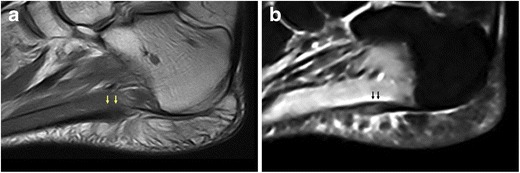
Plantar fasciitis. Lateral plain radiograph shows PF thickening (double-head arrow) and fine calcifications at the calcaneal insertion of the PF (arrowhead); a plantar calcaneal spur at the origin of intrinsic muscles of the foot (arrow) and calcific enthesopathy of the Achilles tendon (open arrow) are also evident (a). MRI confirms the presence of a calcaneal spur (arrow) and PF thickening at its calcaneal attachment (double-head arrow) (b). Bone marrow oedema in the calcaneal spur (arrow) is demonstrated on the fluid-sensitive image (c)
Fig. 4.
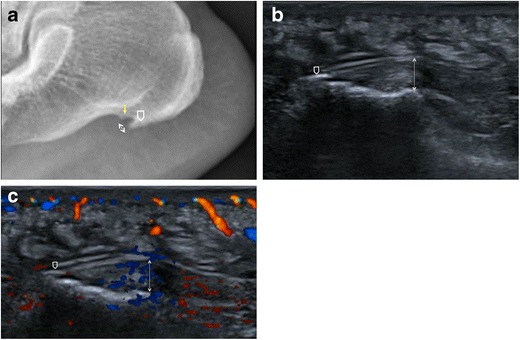
Plantar fasciitis. Lateral plain radiograph shows PF thickening (double-head arrow), a calcaneal spur located within the PF (open arrow) and another spur at the origin of intrinsic muscles of the foot (arrow); cortical irregularities of the calcaneus with sclerotic changes are also seen (a). On ultrasound, the PF is thickened and hypoechoic (double-head arrow) with a minute calcification (open arrow) at its insertion into the calcaneus (b). On colour-Doppler ultrasound, hypervascularisation of the PF and adjacent soft tissues is demonstrated (c)
Plantar fibromatosis or Ledderhose disease (Fig. 5) is a benign nodular formation due to fibroblastic proliferation in the PF. It tends to involve the distal two thirds of the PF, usually in its central bundle, although proximal nodules are not uncommon. Nodular lesions may be multiple and bilateral and typically measure less than 3 cm in diameter [25–27]. Plantar fibromatosis is frequently seen as an isolated disease, but an association with Dupuytren’s disease has been noted [28]. Clinically, plantar fibroma appears as a firm thickening or a single nodule, generally localised in the medial portion of the sole, which is occasionally painful [25–27].
Fig. 5.
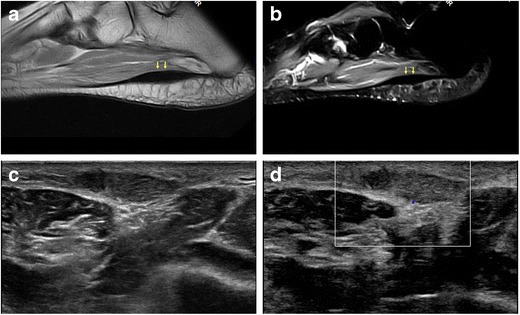
Ledderhose disease. MRI shows a fusiform thickening (arrows) in the distal portion of the PF with low signal intensity on both T1-weighted (a) and fluid-sensitive images (b). On ultrasound, a well-demarcated, hypoechoic nodule is demonstrated (c) with no increased internal vascularity (d)
Tears of the PF (Fig. 6) are uncommon and can be partial or complete. Traumatic tears are often related to forcible plantar flexion of the foot in competitive athletes, mostly runners and jumpers; these are typically distal to calcaneal insertion of the PF and chronic overuse is considered an aetiological factor [29–32]. Spontaneous ruptures may occur at the calcaneal attachment of the PF in patients with previous history of plantar fasciitis and local treatment with steroid injections [33–35]. Clinical presentation includes acute pain, usually accompanied by a “snap” noise, and local swelling [36].
Fig. 6.
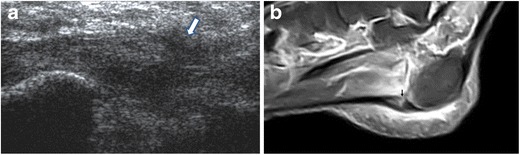
Plantar fascia rupture. On ultrasound, a tear in the PF (arrow) is shown; the PF is hypoechoic and thickened as a result of previous plantar fasciitis treated with local injections (a). MRI confirms PF rupture (arrow) and highlights marked oedema of soft tissues (b)
Peculiar lesions of the PF should be kept in mind as differential diagnoses of the main PF disorders and include xanthoma, diabetic fascial disease, foreign-body reactions and plantar infections. Xanthomas (Fig. 7) are described in many hyperlipidaemia states; they typically involve tendons and are occasionally located within the PF. They are usually asymptomatic and tend to recur after surgical removal [3]. Some studies have found that the thickness and stiffness of the PF and Achilles tendon are increased in patients with type I and type II diabetes mellitus [37, 38]. PF thickness is considered a predictor of the development of late complications in type I diabetes mellitus [38, 39]. Moreover, a relationship between PF thickening in type II diabetes mellitus and body mass index values has also been demonstrated [37]. Occasionally, foreign material is present within or adjacent to the PF and presents with symptoms of plantar fasciitis. It derives from penetrating injuries even though history of trauma or puncture is not always reported [3]. Infectious fasciitis (Fig. 8) may occur as a result of spread from a contiguous source of infection, penetrating wounds due to iatrogenic (surgical procedures) and accidental causes (foreign body, punctures), or in diabetics’ feet [2, 40]; atypical infections may result from haematic diffusion of microorganisms, particularly in immunosuppressed patients [41]. As fascial inflammation can cause destruction of mechanical barriers, infection may spread and affect perifascial structures including soft tissues, bone and muscles [42].
Fig. 7.
Plantar xanthoma. On both sagittal T1-weighted (a) and fluid-sensitive (b) images, xanthoma (arrows) appears as fusiform enlargement of the PF and shows heterogeneous signal intensity
Fig. 8.
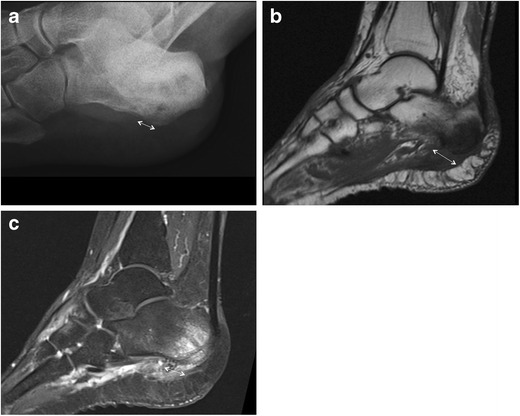
Heel osteomyelitis. Lateral plain radiograph shows marked morphological alteration of the heel with irregular lytic areas and concomitant PF thickening (double-head arrow) due to spreading of the infection (a). MRI confirms morphological alterations of the heel and PF (double-head arrow) on both T1-weighted (b) and fluid-sensitive (c) images
Plain radiography
Plain radiography is widespread, cost-effective and panoramic, thus often representing the imaging modality of first choice for the evaluation of painful heel.
Several findings suggestive of plantar fasciitis can be detected on conventional radiographs. Despite this, plain radiography should not be used to make a diagnosis of plantar fasciitis without knowledge of clinical history or physical examination findings [19]. PF thickness can be measured with accuracy on lateral plain radiographs of the ankle and foot [3, 4, 19]. PF mean thickness at its calcaneal origin, in the central fascicle, is 4.0 mm [6]. Increased thickness of the PF measuring more than 4–5 mm within 5 mm of its calcaneal attachment is evident on lateral plain radiographs of individuals with plantar fasciitis (Figs. 2, 3 and 4) and represents a reliable sign of plantar fasciitis [19]. Deep below the PF, at its calcaneal origin, a fat pad is seen and usually has a triangular shape on lateral non-weight-bearing plain radiographs. This fat pad becomes narrowed or is absent in individuals with plantar fasciitis, maybe owing to both mechanical and inflammatory mechanisms, thus representing a further sign of plantar fasciitis [19]. The combination of thickened PF and fat pad abnormalities on lateral plain radiography has a sensitivity of 85% and specificity of 95% for plantar fasciitis [19]. Changes in the cortex of the calcaneus at the attachment of the PF, with or without spur formation, have been correlated with plantar fasciitis (Fig. 4). These are cortical irregularities presenting with loss of the smooth contour of the bone and both cortical lucency and sclerosis [19].
Plantar calcaneal spurs and calcifications within the PF are uncommon occurrences in patients with plantar fasciitis [19, 20]. The significance of calcaneal spurs as a cause of plantar fasciitis has received considerable attention in the literature [17–20], and currently their importance in terms of the diagnosis and prognosis of plantar fasciitis is debatable. Calcaneal spurs associated with plantar fasciitis include those located within the plantar fascia (Fig. 4) [20]. These are however very uncommon, as the most common site of plantar calcaneal spurs is in the abductor hallucis and flexor digitorum brevis origins, deep below the PF (Figs. 3 and 4) [18, 20]. Thus, evidence of calcaneal spurs on conventional radiographs is not a pathognomonic sign of plantar fasciitis.
Apart from highlighting indirect signs of plantar fasciitis and calcaneal spurs, conventional radiography is useful in overviewing anatomical and pathological changes of the bone and soft tissues. Radiopaque foreign material, such as metals, may be easily revealed [43]. In the case of infectious fasciitis, plain radiography shows soft-tissue swelling and blurring of soft-tissue planes. Concomitant osteomyelitic changes in bone morphology can also be detected and mainly include lytic lesions, osteopenia, loss of trabecular architecture, new bone apposition and periosteal thickening (Fig. 8) [40]. Finally, stress fractures may be associated with PF injuries and should be ruled out [44].
Ultrasound
On ultrasound, similarly to ligaments, PF shows a fibrillar pattern due to the hyperechoic appearance of type I collagen fibre bundles embedded within a background of hypoechoic matrix [45, 46].
Sonographic characteristics of plantar fasciitis include loss of fibrillar structure, increased thickness over 4 mm, perifascial collections and calcifications within the PF (Figs. 2 and 4) [16, 47–57]. Hyperaemia is a well-known feature of tendinopathy due to neurovascular growth and may contribute to pain. It can be assessed using Doppler ultrasound. Similarly, Doppler ultrasound can identify hyperaemia in the PF, near its proximal insertion and in the perifascial soft tissue, in patients with plantar fasciitis (Fig. 4); hyperaemia can also correlate with treatment [58–61]. As an additional finding, in patients with plantar fasciitis the PF is less elastic under real-time sonoelastography, and this might increase the accuracy of ultrasound [62, 63].
The sonographic presentation of plantar fibromatosis (Ledderhose disease) includes typically single, rarely multiple iso-hypoechoic, well-demarcated, nodular thickenings of the PF, with no calcifications or fluid collection. Doppler ultrasound generally shows no vascular flow inside the lesion (Fig. 5) [64].
Sonographic findings of PF rupture include complete or partial interruption of the PF, with hypoechoic tissue at the site of rupture related to local haemorrhage and inflammation (Fig. 6) [3].
Among other disorders of the PF, plantar xanthomas appear as nodules with a speckled pattern [3]. Increased thickness of the PF can be sonographically detected in the early stages of diabetes mellitus [37–39]. Ultrasound can aid in the diagnosis of foreign body reaction by identifying echoic extraneous material within or adjacent to the PF. Sometimes posterior acoustic shadowing and, in cases of metal objects, comet tail reverberation artefacts may also be seen [65]. Ultrasound is useful in the assessment of musculoskeletal infections, particularly in distinguishing acute or chronic infections from tumours or non-infective conditions. In the case of infectious fasciitis, the PF is increased in volume with loss of fibrillar pattern and perifascial oedema and is hyperaemic on Doppler evaluation [40].
Magnetic resonance imaging
In healthy individuals, the PF is homogeneously hypointense on both T1-weighted and fluid-sensitive sequences [6].
MRI findings of plantar fasciitis include: thickening of the PF, most commonly at its calcaneal origin; intrasubstance areas of intermediate signal on T1-weighted sequences and increased signal on fluid-sensitive sequences; oedema in the adjacent soft tissue; bone marrow oedema of the calcaneal attachment of the PF suggestive of enthesopathy (Figs. 2 and 3) [2, 4].
In plantar fibromatosis (Ledderhose disease), the common MRI appearance of plantar fibroma is a lobulated mass of low signal intensity on both T1- and T2-weighted sequences due to its fibrous nature (Fig. 5). In some instances, plantar fibroma may show high signal on fluid-sensitive sequences [4].
MRI findings of acute PF tear are complete or partial interruption of the low signal of the PF and signal changes at the site of lesion including high signal on fluid-sensitive sequences and intermediate signal on T1-weighted sequences. High-signal intensity may be an additional finding on fluid-sensitive sequences in the soft tissues surrounding the site of rupture (Fig. 6); this reflects local haemorrhage, inflammation and oedema [2, 66, 67].
Among other lesions of the PF, xanthomas appear as fusiform enlargement of the PF showing heterogeneous signal intensity on both T1- and T2-weighted sequences (Fig. 7) [66]. In the case of foreign body reaction, MRI appearance is variable: low signal intensity on T1-weighted images is frequently noted, while surrounding granulation tissue often has high signal intensity on T2-weighted images [3]. In the case of plantar infection, MR imaging allows identification, localisation and assessment of the extent of the inflammatory process. On MRI, the PF, perifascial soft tissues and adjacent bone show abnormal high signal intensity on fluid-sensitive sequences, low signal intensity on T1-weighted sequences and significant contrast enhancement (Fig. 8) [2, 67].
Discussion
Based on a systematic review of the last 20 years’ literature and taking advantage of our centres’ experience, this study is able to shed light on key features of PF disorders that can be identified on conventional imaging modalities, such as plain radiography, ultrasound and MRI, thus representing a valuable guide to proper diagnosis of PF disease. Radiographic, sonographic and MRI findings of PF disorders are summarised in Table 1.
Table 1.
Radiographic, sonographic and MRI features of PF disorders
| Plain radiography | Ultrasound | Magnetic resonance imaging | |
|---|---|---|---|
| Plantar fasciitis | PF thickening Narrowed/absent fat pad deep below the PF Cortical changes (sclerosis/lucency and loss of smooth contour) at the PF calcaneal attachment Calcaneal spurs within the PF |
PF thickening Loss of fibrillar structure Perifascial fluid collections Calcifications within the PF Hyperemia in the PF/perifascial soft tissues (Doppler imaging) Reduced PF elasticity (elastosonography) |
PF thickening Intrasubstance areas of intermediate T1/high T2 signal Oedema in the adjacent soft tissues Bone marrow oedema at the PF calcaneal attachment |
| Plantar fibromatosis | Iso-hypoechoic, well-demarcated mass No intralesional flow (Doppler imaging) |
Lobulated low-signal mass on T1w and T2w images | |
| Tear | Complete/partial interruption of the PF Hypoechoic tissue at the site of rupture |
Complete/partial interruption of the PF Intermediate T1/high T2 signal at the site of rupture Oedema in the adjacent soft tissues |
|
| Xanthoma | Nodule with speckled pattern | Fusiform enlargement of the PF Heterogeneous T1 and T2 signal |
|
| Foreign body | Radiopaque material (e.g., metals) | Echoic material Posterior acoustic shadowing Comet tail reverberation (metals) |
Variable signal of the foreign body High T2 signal of the granulation tissue |
| Plantar infection | Soft tissue swelling Blurring of soft tissue planes Bone osteomyelitic changes |
PF thickening Loss of fibrillar structure Perifascial oedema Hyperemia in the PF (Doppler imaging) |
Low T1/high T2 signal and contrast enhancement in the PF, perifascial soft tissues and adjacent bone |
Plantar fasciitis is the most common disorder of the PF and a frequent cause of heel pain in the general population [22]. Plain radiography, ultrasound and MRI all provide valuable information that aids in the diagnosis. Osborne et al. have demonstrated that PF thickening, abnormalities in the fat pad deep below the PF and bone cortical changes in the calcaneus are radiographic findings of plantar fasciitis [19]. A systematic review of articles published between 2000 and 2012 concerning the role of sonography in plantar fasciitis indicates that it is accurate and reliable [53]. Doppler ultrasound is often normal with plantar fasciitis, but various degrees of hyperaemia may be demonstrated [58–61]. Several studies support the role of elastosonography in patients with plantar fasciitis [62, 63, 68–70], even in symptomatic patients with normal B-mode findings [71]; however, some results are controversial [72] and further investigations are thus needed to clarify the diagnostic value of sonoelastography in plantar fasciitis. Even though there is no significant difference between the accuracy of ultrasound and MRI regarding the measurements of the PF thickness [73], MRI is considered as the most sensitive imaging modality for diagnosing plantar fasciitis [74]. It enables determination of the exact location and extent of the inflammatory alterations within the PF as well as detection of signal changes within adjacent soft tissue or bone marrow [2].
In cases of atypical clinical presentation or where imaging findings do not confirm the presence of plantar fasciitis, differential diagnosis includes other causes of PF disease, such as plantar fibromatosis, trauma and infection, but also disorders arising from structures other than the PF. Ultrasound has several advantages over MRI in the assessment of Ledderhose disease or plantar fibromatosis. Plantar fibromas may be small, thus appearing as small hypointense lesions on MRI, and are difficult to differentiate from the low signal intensity of the PF. Small plantar fibromas are more easily detected on ultrasound because of the contrast between their poorly reflective echotexture and fibrillar appearance of the normal PF. Further, both feet may be examined together using ultrasound. Examining both feet together using MRI reduces the in-plane resolution; in contrast, examining both feet separately is time-consuming if compared with ultrasound [4]. A significant overlap exists between the presentation of plantar fasciitis and that of a traumatic partial tear. In our experience, ultrasound is superior to MRI in differentiating true fibre interruption and tearing from oedema. Confirmation of a complete tear is best achieved by proving widening of the gap between the two ends of PF with dynamic manoeuvres [43]. In cases of complete tear, MRI allows precise estimation of PF retraction with prognostic implications for surgical reparability of the lesion [2]. In cases of infectious fasciitis, MRI provides high anatomic detail and an accurate depiction of the extent of the inflammatory process and adjacent soft tissues, even though artefacts arising from metallic foreign material may be present [40].
Several pathologies involving structures other than the PF may mimic PF disease and should be included in the differential diagnosis. Achilles tendinopathy may present with symptoms that are similar to those of plantar fasciitis. This may be related to the close anatomic connection between the PF and the paratenon of the Achilles tendon [5, 75]. Thus, both the Achilles tendon and PF should be carefully evaluated using ultrasound or MRI. Further, if MRI reveals marked bone marrow oedema at the calcaneal origin of the PF in patients with plantar fasciitis, a concomitant enthesopathy of the Achilles tendon should be suspected [4]. The presence of plantar calcaneal spurs should also be assessed. Spur genesis has traditionally been attributed to chronic traction of the PF and repetitive microtrauma, which in turn lead to periostitis and calcification [3]. The role of vertical compression of the heel in spur formation has recently been hypothesised and related to older age, osteoarthritis and obesity [76]. As stated above, calcaneal spurs are not specific for plantar fasciitis and are often identified in asymptomatic individuals; however, a strong association between spurs and chronic plantar heel pain has been demonstrated, specifically in cases of concurrent fat pad abnormalities [77]. Finally, entrapment of the first branch of the lateral plantar nerve (Baxter’s neuropathy) [43], stress fractures of the calcaneus [78], vascular disease [79] and heel fat pad atrophy and necrosis [2] may present with nonspecific heel pain and represent all differential diagnoses of PF disease.
In conclusion, PF disorders are common causes of heel pain and disability in the general population. Imaging is often required to confirm diagnosis or reveal concomitant injuries. As an inexpensive, quick and dynamic imaging technique that also provides high-resolution depiction of the PF and comparison with the contralateral side, ultrasound should be considered the modality of first choice for assessing PF disorders. Several indirect findings of PF disorders can be detected on conventional radiographs and should be identified even in patients examined for other reasons. MRI can reliably delineate both the soft tissue and bone anatomy of the sole of the foot and enables correct diagnosis of PF disorders, but is expensive and should be regarded as a second-line imaging modality.
Compliance with ethical standards
Conflict of interest
None.
Funding source
None.
References
- 1.Thomas MJ, Roddy E, Zhang W, Menz HB, Hannan MT, Peat GM. The population prevalence of foot and ankle pain in middle and old age: a systematic review. Pain. 2011;152(12):2870–2880. doi: 10.1016/j.pain.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 2.Theodorou DJ, Theodorou SJ, Resnick D. MR imaging of abnormalities of the plantar fascia. Semin Musculoskelet Radiol. 2002;6(2):105–118. doi: 10.1055/s-2002-32357. [DOI] [PubMed] [Google Scholar]
- 3.Jeswani T, Morlese J, McNally EG. Getting to the heel of the problem: plantar fascia lesions. Clin Radiol. 2009;64(9):931–939. doi: 10.1016/j.crad.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 4.McNally EG, Shetty S. Plantar fascia: imaging diagnosis and guided treatment. Semin Musculoskelet Radiol. 2010;14(3):334–343. doi: 10.1055/s-0030-1254522. [DOI] [PubMed] [Google Scholar]
- 5.Stecco C, Corradin M, Macchi V, et al. Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. J Anat. 2013;223(6):665–676. doi: 10.1111/joa.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehrmann C, Maier M, Mengiardi B, Pfirrmann CW, Sutter R. Calcaneal attachment of the plantar fascia: MR findings in asymptomatic volunteers. Radiology. 2014;272(3):807–814. doi: 10.1148/radiol.14131410. [DOI] [PubMed] [Google Scholar]
- 7.Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303–310. doi: 10.1177/107110070402500505. [DOI] [PubMed] [Google Scholar]
- 8.Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 9.Ieong E, Afolayan J, Carne A, Solan M. Ultrasound scanning for recalcitrant plantar fasciopathy. Basis of a new classification. Skelet Radiol. 2013;42(3):393–398. doi: 10.1007/s00256-012-1470-x. [DOI] [PubMed] [Google Scholar]
- 10.Huang YC, Wang LY, Wang HC, Chang KL, Leong CP. The relationship between the flexible flatfoot and plantar fasciitis: ultrasonographic evaluation. Chang Gung Med J. 2004;27(6):443–448. [PubMed] [Google Scholar]
- 11.McGonagle D, Marzo-Ortega H, O’Connor P, et al. The role of biomechanical factors and HLA-B27 in magnetic resonance imaging-determined bone changes in plantar fascia enthesopathy. Arthritis Rheum. 2002;46(2):489–493. doi: 10.1002/art.10125. [DOI] [PubMed] [Google Scholar]
- 12.van Leeuwen KD, Rogers J, Winzenberg T, van Middelkoop M. Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: systematic review and meta-analysis of various clinical and imaging risk factors. Br J Sports Med. 2016;50(16):972–981. doi: 10.1136/bjsports-2015-094695. [DOI] [PubMed] [Google Scholar]
- 13.de Miguel E, Cobo T, Munoz-Fernandez S, et al. Validity of enthesis ultrasound assessment in spondyloarthropathy. Ann Rheum Dis. 2009;68(2):169–174. doi: 10.1136/ard.2007.084251. [DOI] [PubMed] [Google Scholar]
- 14.Erdem CZ, Sarikaya S, Erdem LO, Ozdolap S, Gundogdu S. MR imaging features of foot involvement in ankylosing spondylitis. Eur J Radiol. 2005;53(1):110–119. doi: 10.1016/j.ejrad.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Erdem CZ, Tekin NS, Sarikaya S, Erdem LO, Gulec S. MR imaging features of foot involvement in patients with psoriasis. Eur J Radiol. 2008;67(3):521–525. doi: 10.1016/j.ejrad.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Gibbon WW, Long G. Ultrasound of the plantar aponeurosis (fascia) Skelet Radiol. 1999;28(1):21–26. doi: 10.1007/s002560050467. [DOI] [PubMed] [Google Scholar]
- 17.Abreu MR, Chung CB, Mendes L, Mohana-Borges A, Trudell D, Resnick D. Plantar calcaneal enthesophytes: new observations regarding sites of origin based on radiographic, MR imaging, anatomic, and paleopathologic analysis. Skelet Radiol. 2003;32(1):13–21. doi: 10.1007/s00256-002-0585-x. [DOI] [PubMed] [Google Scholar]
- 18.Johal KS, Milner SA (2012) Plantar fasciitis and the calcaneal spur: fact or fiction? Foot Ankle Surg 18(1):39–41 [DOI] [PubMed]
- 19.Osborne HR, Breidahl WH, Allison GT (2006) Critical differences in lateral X-rays with and without a diagnosis of plantar fasciitis. J Sci Med Sport 9(3):231–237 [DOI] [PubMed]
- 20.Zhou B, Zhou Y, Tao X, Yuan C, Tang K (2015) Classification of calcaneal spurs and their relationship with plantar fasciitis. J Foot Ankle Surg 54(4):594–600 [DOI] [PubMed]
- 21.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350(21):2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 22.Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician. 2011;84(6):676–682. [PubMed] [Google Scholar]
- 23.Schwartz EN, Su J. Plantar fasciitis: a concise review. Perm J. 2014;18(1):e105–e107. doi: 10.7812/TPP/13-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas JL, Christensen JC, Kravitz SR et al (2010) The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg 49(3 Suppl):S1–S19 [DOI] [PubMed]
- 25.Adib O, Noizet E, Croue A, Aube C. Ledderhose’s disease: radiologic/pathologic correlation of superficial plantar fibromatosis. Diagn Interv Imaging. 2014;95(9):893–896. doi: 10.1016/j.diii.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 26.Draghi F, Ippolito S, Sosio D, Pietrobono L, Ferrozzi G. Ultrasonography contrast media and “compound” technique in the study of 2 cases of Ledderhose disease. Radiol Med. 2001;101(1–2):91–92. [PubMed] [Google Scholar]
- 27.Lee TH, Wapner KL, Hecht PJ. Plantar fibromatosis. J Bone Joint Surg Am. 1993;75(7):1080–1084. doi: 10.2106/00004623-199307000-00016. [DOI] [PubMed] [Google Scholar]
- 28.Gudmundsson KG, Jonsson T, Arngrimsson R. Association of Morbus Ledderhose with Dupuytren’s contracture. Foot Ankle Int. 2013;34(6):841–845. doi: 10.1177/1071100713475352. [DOI] [PubMed] [Google Scholar]
- 29.Louwers MJ, Sabb B, Pangilinan PH (2010) Ultrasound evaluation of a spontaneous plantar fascia rupture. Am J Phys Med Rehabil 89(11):941–944 [DOI] [PubMed]
- 30.Pascoe SC, Mazzola TJ. Acute medial plantar fascia tear. J Orthop Sports Phys Ther. 2016;46(6):495. doi: 10.2519/jospt.2016.0409. [DOI] [PubMed] [Google Scholar]
- 31.Saxena A, Fullem B. Plantar fascia ruptures in athletes. Am J Sports Med. 2004;32(3):662–665. doi: 10.1177/0363546503261727. [DOI] [PubMed] [Google Scholar]
- 32.Suzue N, Iwame T, Kato K et al (2014) Plantar fascia rupture in a professional soccer player. J Med Investig 61(3–4):413–416 [DOI] [PubMed]
- 33.Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19(2):91–97. doi: 10.1177/107110079801900207. [DOI] [PubMed] [Google Scholar]
- 34.Lee HS, Choi YR, Kim SW, Lee JY, Seo JH, Jeong JJ. Risk factors affecting chronic rupture of the plantar fascia. Foot Ankle Int. 2014;35(3):258–263. doi: 10.1177/1071100713514564. [DOI] [PubMed] [Google Scholar]
- 35.Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15(7):376–381. doi: 10.1177/107110079401500706. [DOI] [PubMed] [Google Scholar]
- 36.Yu JS. Pathologic and post-operative conditions of the plantar fascia: review of MR imaging appearances. Skelet Radiol. 2000;29(9):491–501. doi: 10.1007/s002560000230. [DOI] [PubMed] [Google Scholar]
- 37.Abate M, Schiavone C, Di Carlo L, Salini V. Achilles tendon and plantar fascia in recently diagnosed type II diabetes: role of body mass index. Clin Rheumatol. 2012;31(7):1109–1113. doi: 10.1007/s10067-012-1955-y. [DOI] [PubMed] [Google Scholar]
- 38.Craig ME, Duffin AC, Gallego PH, et al. Plantar fascia thickness, a measure of tissue glycation, predicts the development of complications in adolescents with type 1 diabetes. Diabetes Care. 2008;31(6):1201–1206. doi: 10.2337/dc07-2168. [DOI] [PubMed] [Google Scholar]
- 39.Benitez-Aguirre PZ, Craig ME, Jenkins AJ, et al. Plantar fascia thickness is longitudinally associated with retinopathy and renal dysfunction: a prospective study from adolescence to adulthood. J Diabetes Sci Technol. 2012;6(2):348–355. doi: 10.1177/193229681200600220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009;23(2):80–89. doi: 10.1055/s-0029-1214160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sideras PA, Heiba S, Machac J, Hechtman J, Vatti S. Mycobacterial pseudotumor of the plantar fascia: how common is it? Clin Imaging. 2013;37(4):802–805. doi: 10.1016/j.clinimag.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 42.Goodwin DW, Salonen DC, Yu JS, Brossmann J, Trudell DJ, Resnick DL. Plantar compartments of the foot: MR appearance in cadavers and diabetic patients. Radiology. 1995;196(3):623–630. doi: 10.1148/radiology.196.3.7644621. [DOI] [PubMed] [Google Scholar]
- 43.Hoffman DF, Grothe HL, Bianchi S. Sonographic evaluation of hindfoot disorders. J Ultrasound. 2014;17(2):141–150. doi: 10.1007/s40477-014-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yu JS, Solmen J. Stress fractures associated with plantar fascia disruption: two case reports involving the cuboid. J Comput Assist Tomogr. 2001;25(6):971–974. doi: 10.1097/00004728-200111000-00023. [DOI] [PubMed] [Google Scholar]
- 45.Gitto S, Draghi F (2016) Normal sonographic anatomy of the wrist with emphasis on assessment of tendons, nerves, and ligaments. J Ultrasound Med 35(5):1081–1094 [DOI] [PubMed]
- 46.Precerutti M, Bonardi M, Ferrozzi G, Draghi F. Sonographic anatomy of the ankle. J Ultrasound. 2014;17(2):79–87. doi: 10.1007/s40477-013-0025-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abul K, Ozer D, Sakizlioglu SS, Buyuk AF, Kaygusuz MA. Detection of normal plantar fascia thickness in adults via the ultrasonographic method. J Am Podiatr Med Assoc. 2015;105(1):8–13. doi: 10.7547/8750-7315-105.1.8. [DOI] [PubMed] [Google Scholar]
- 48.Akfirat M, Sen C, Gunes T. Ultrasonographic appearance of the plantar fasciitis. Clin Imaging. 2003;27(5):353–357. doi: 10.1016/S0899-7071(02)00591-0. [DOI] [PubMed] [Google Scholar]
- 49.Cardinal E, Chhem RK, Beauregard CG, Aubin B, Pelletier M. Plantar fasciitis: sonographic evaluation. Radiology. 1996;201(1):257–259. doi: 10.1148/radiology.201.1.8816554. [DOI] [PubMed] [Google Scholar]
- 50.Cheng JW, Tsai WC, Yu TY, Huang KY (2012) Reproducibility of sonographic measurement of thickness and echogenicity of the plantar fascia. J Clin Ultrasound 40(1):14–19 [DOI] [PubMed]
- 51.Kane D, Greaney T, Shanahan M, et al. The role of ultrasonography in the diagnosis and management of idiopathic plantar fasciitis. Rheumatology. 2001;40(9):1002–1008. doi: 10.1093/rheumatology/40.9.1002. [DOI] [PubMed] [Google Scholar]
- 52.Karabay N, Toros T, Hurel C (2007) Ultrasonographic evaluation in plantar fasciitis. J Foot Ankle Surg 46(6):442–446 [DOI] [PubMed]
- 53.Mohseni-Bandpei MA, Nakhaee M, Mousavi ME, Shakourirad A, Safari MR, Vahab Kashani R. Application of ultrasound in the assessment of plantar fascia in patients with plantar fasciitis: a systematic review. Ultrasound Med Biol. 2014;40(8):1737–1754. doi: 10.1016/j.ultrasmedbio.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 54.Ozdemir H, Yilmaz E, Murat A, Karakurt L, Poyraz AK, Ogur E. Sonographic evaluation of plantar fasciitis and relation to body mass index. Eur J Radiol. 2005;54(3):443–447. doi: 10.1016/j.ejrad.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 55.Sabir N, Demirlenk S, Yagci B, Karabulut N, Cubukcu S (2005) Clinical utility of sonography in diagnosing plantar fasciitis. J Ultrasound Med 24(8):1041–1048 [DOI] [PubMed]
- 56.Tsai WC, Chiu MF, Wang CL, Tang FT, Wong MK. Ultrasound evaluation of plantar fasciitis. Scand J Rheumatol. 2000;29(4):255–259. doi: 10.1080/030097400750041415. [DOI] [PubMed] [Google Scholar]
- 57.Vohra PK, Kincaid BR, Japour CJ, Sobel E. Ultrasonographic evaluation of plantar fascia bands. A retrospective study of 211 symptomatic feet. J Am Podiatr Med Assoc. 2002;92(8):444–449. doi: 10.7547/87507315-92-8-444. [DOI] [PubMed] [Google Scholar]
- 58.Chen H, Ho HM, Ying M, Fu SN. Association between plantar fascia vascularity and morphology and foot dysfunction in individuals with chronic plantar fasciitis. J Orthop Sports Phys Ther. 2013;43(10):727–734. doi: 10.2519/jospt.2013.4774. [DOI] [PubMed] [Google Scholar]
- 59.McMillan AM, Landorf KB, Gregg JM, De Luca J, Cotchett MP, Menz HB. Hyperemia in plantar fasciitis determined by power Doppler ultrasound. J Orthop Sports Phys Ther. 2013;43(12):875–880. doi: 10.2519/jospt.2013.4810. [DOI] [PubMed] [Google Scholar]
- 60.Mendonca JA, Provenza JR, Appenzeller S. Positive power Doppler signal in plantar fasciitis. Rheumatol Int. 2013;33(2):507–509. doi: 10.1007/s00296-011-2209-z. [DOI] [PubMed] [Google Scholar]
- 61.Walther M, Radke S, Kirschner S, Ettl V, Gohlke F. Power Doppler findings in plantar fasciitis. Ultrasound Med Biol. 2004;30(4):435–440. doi: 10.1016/j.ultrasmedbio.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 62.Rios-Diaz J, Martinez-Paya JJ, del Bano-Aledo ME, de Groot-Ferrando A, Botia-Castillo P, Fernandez-Rodriguez D. Sonoelastography of plantar fascia: reproducibility and pattern description in healthy subjects and symptomatic subjects. Ultrasound Med Biol. 2015;41(10):2605–2613. doi: 10.1016/j.ultrasmedbio.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 63.Sconfienza LM, Silvestri E, Orlandi D, et al. Real-time sonoelastography of the plantar fascia: comparison between patients with plantar fasciitis and healthy control subjects. Radiology. 2013;267(1):195–200. doi: 10.1148/radiol.12120969. [DOI] [PubMed] [Google Scholar]
- 64.Griffith JF, Wong TY, Wong SM, Wong MW, Metreweli C. Sonography of plantar fibromatosis. AJR Am J Roentgenol. 2002;179(5):1167–1172. doi: 10.2214/ajr.179.5.1791167. [DOI] [PubMed] [Google Scholar]
- 65.Rawool NM, Nazarian LN. Ultrasound of the ankle and foot. Semin Ultrasound CT MR. 2000;21(3):275–284. doi: 10.1016/S0887-2171(00)90046-5. [DOI] [PubMed] [Google Scholar]
- 66.Narvaez JA, Narvaez J, Ortega R, Aguilera C, Sanchez A, Andia E (2000) Painful heel: MR imaging findings. Radiographics 20(2):333–352 [DOI] [PubMed]
- 67.Theodorou DJ, Theodorou SJ, Farooki S, Kakitsubata Y, Resnick D. Disorders of the plantar aponeurosis: a spectrum of MR imaging findings. AJR Am J Roentgenol. 2001;176(1):97–104. doi: 10.2214/ajr.176.1.1760097. [DOI] [PubMed] [Google Scholar]
- 68.Lee SY, Park HJ, Kwag HJ, et al. Ultrasound elastography in the early diagnosis of plantar fasciitis. Clin Imaging. 2014;38(5):715–718. doi: 10.1016/j.clinimag.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 69.Sconfienza LM, Orlandi D, Cimmino MA, Silvestri E. A few considerations on “sonoelastography of the plantar fascia”. Radiology. 2011;261(3):995–996. doi: 10.1148/radiol.11111255. [DOI] [PubMed] [Google Scholar]
- 70.Wu CH, Chang KV, Mio S, Chen WS, Wang TG. Sonoelastography of the plantar fascia. Radiology. 2011;259(2):502–507. doi: 10.1148/radiol.11101665. [DOI] [PubMed] [Google Scholar]
- 71.Wu CH, Chen WS, Wang TG. Plantar fascia softening in plantar fasciitis with normal B-mode sonography. Skelet Radiol. 2015;44(11):1603–1607. doi: 10.1007/s00256-015-2215-4. [DOI] [PubMed] [Google Scholar]
- 72.Wu CH. A few considerations on “Ultrasound elastography in the early diagnosis of plantar fasciitis”. Clin Imaging. 2015;39(1):165. doi: 10.1016/j.clinimag.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 73.Moraes do Carmo CC, Fonseca de Almeida Melao LI, Valle de Lemos Weber MF, Trudell D, Resnick D. Anatomical features of plantar aponeurosis: cadaveric study using ultrasonography and magnetic resonance imaging. Skelet Radiol. 2008;37(10):929–935. doi: 10.1007/s00256-008-0497-5. [DOI] [PubMed] [Google Scholar]
- 74.Chimutengwende-Gordon M, O’Donnell P, Singh D. Magnetic resonance imaging in plantar heel pain. Foot Ankle Int. 2010;31(10):865–870. doi: 10.3113/FAI.2010.0865. [DOI] [PubMed] [Google Scholar]
- 75.Gitto S, Draghi AG, Bortolotto C, Draghi F (2016) Sonography of the Achilles tendon after complete rupture repair: what the radiologist should know. J Ultrasound Med 35(12):2529–2536 [DOI] [PubMed]
- 76.Menz HB, Zammit GV, Landorf KB, Munteanu SE. Plantar calcaneal spurs in older people: longitudinal traction or vertical compression? J Foot Ankle Res. 2008;1(1):7. doi: 10.1186/1757-1146-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2009;2:32. doi: 10.1186/1757-1146-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Berger FH, de Jonge MC, Maas M. Stress fractures in the lower extremity. The importance of increasing awareness amongst radiologists. Eur J Radiol. 2007;62(1):16–26. doi: 10.1016/j.ejrad.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 79.Siegal DS, Wu JS, Brennan DD, Challies T, Hochman MG. Plantar vein thrombosis: a rare cause of plantar foot pain. Skelet Radiol. 2008;37(3):267–269. doi: 10.1007/s00256-007-0419-y. [DOI] [PubMed] [Google Scholar]


