Abstract
Brivaracetam (Briviact): a novel adjunctive therapy for partial-onset seizures
INTRODUCTION
Epilepsy is the fourth most common neurological disorder and affects more than 65 million individuals worldwide.1 This condition is marked by the presence of epileptic seizures, which result from an abnormal synchronous firing of excitatory neurons in the brain.1,2 When neurons fire synchronously, a wave of depolarization known as a paroxysmal depolarizing shift occurs.2 During this period, the neurons experience a lowered resistance to firing, leading to multiple action potentials that generate abnormally increased electrical activity within the brain.
There are various types of epilepsy syndromes that are defined based on a combination of symptoms. While generalized seizures begin in both hemispheres of the brain, partial-onset seizures (POS) (also called focal or localized seizures) and other forms of epilepsy originate in only one hemisphere. Patients presenting with new-onset seizures must be carefully evaluated to determine if the seizures are secondary to non-neurological causes; differential diagnoses may include hypoglycemia, alcohol withdrawal, or electrolyte abnormalities. Diagnosis of epilepsy involves ruling out these other etiologies via laboratory testing, brain imaging, and an electroencephalogram. Patients with epilepsy may have developed the condition secondary to genetic factors or other pathologies, such as brain trauma, malignancy, stroke, or neurological infection.1,2 While a majority of patients with epilepsy are able to maintain seizure control with one to two antiepileptic drugs (AEDs), many individuals require adjunctive therapy to achieve long-term remission.
Brivaracetam (Briviact, UCB, Inc.), a propyl analogue of levetiracetam, an anticonvulsant and racetam derivative, was granted Food and Drug Administration (FDA) approval as an add-on therapy in February 2016. It is indicated as adjunctive therapy for treating POS in adults and adolescents 16 years of age or older.3
MECHANISM OF ACTION
Brivaracetam is a third-generation antiepileptic racetam derivative and a 4-n-propyl analogue of levetiracetam.1–3 While the exact mechanism of action of brivaracetam is unknown, its anticonvulsant effects are believed to be due to its highly selective affinity for synaptic vesicle protein 2A (SV2A) in the brain. The SV2A glycoprotein is a protein-coding gene implicated in synaptic signal transduction.4 It is believed to play a role in the regulation of neurotransmission by stimulating vesicle fusion and maintaining a reserve of secretory vesicles.4 Studies in SV2A-deficient animals have demonstrated an increased propensity for seizures.5 Brivaracetam’s actions as an SV2A ligand lend it broad-spectrum activity against POS. Its chemical structure is shown in Figure 1.
Figure 1.
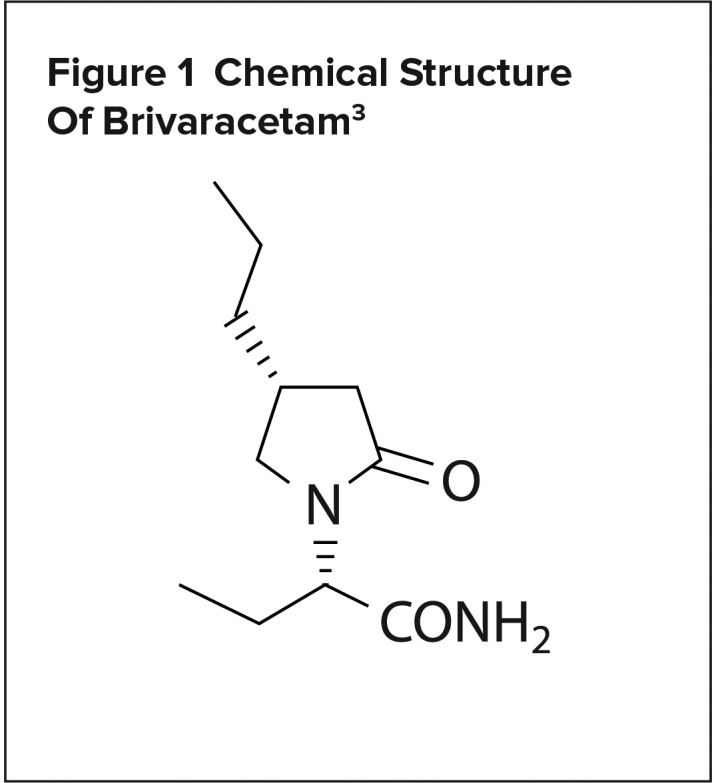
Chemical Structure Of Brivaracetam3
PHARMACOKINETICS
Brivaracetam exhibits linear and time-independent pharmacokinetics at its approved doses. It is freely soluble in water, ethanol, methanol, and glacial acetic acid.3 The drug experiences near-complete absorption after oral administration and is weakly bound to plasma proteins.3 Brivaracetam’s volume of distribution is 0.5 L/kg, and it is rapidly and evenly distributed in most tissues. In addition, the amide moiety of the drug molecule undergoes hydrolysis via hepatic and extrahepatic amidase to a carboxylic acid metabolite.3 This re action is mediated mainly by cytochrome P450 2C19 (CYP2C19). Genetic poly morphisms in CYP2C19 may cause production of the metabolite to be decreased. Poor metabolizers or patients taking concurrent CYP2C19 inhibitors may require dose reduction. Finally, brivaracetam is excreted primarily in the urine within 72 hours of intake.3
CLINICAL TRIALS
The efficacy of brivaracetam as an adjunctive therapy for POS was established in several randomized controlled trials. Phase 3 trial data follow. (See Table 1 for a summary.)
Table 1.
A Summary of Phase 3 Trials of Brivaracetam as an Adjunctive Therapy for Partial-Onset Seizures in Adults
| Study | Design | Population | Group | Number (ITT) | Male Gender (n [%]) | Age in Years (mean [SD]) | Duration of Epilepsy in Years (mean [SD]) | Median Reduction in Baseline-Adjusted POS Frequency per Week (%) |
|---|---|---|---|---|---|---|---|---|
| Ryvlin et al. (2014)6 (NCT00490035) | Prospective, multicenter, doubleblind, randomized, placebocontrolled | Patients with uncontrolled focal seizures despite treatment with 1–2 AEDs | Placebo | 100 | 54 (54.0) | 36.4 (13.0) | 20.4 (12.3) | 17.0 |
| 20 mg | 99 | 61 (61.6) | 35.7 (12.5) | 22.1 (13.6) | 30.0 (P = 0.019) | |||
| 50 mg | 99 | 54 (54.5) | 38.9 (13.6) | 22.3 (13.0) | 26.8 (P = 0.092) | |||
| 100 mg | 100 | 58 (58.0) | 38.0 (13.1) | 22.1 (12.8) | 32.5 (P = 0.004) | |||
| Biton et al. (2014)7 (NCT00464269) | Prospective, multicenter, randomized, doubleblind, placebocontrolled, parallelgroup, fixeddose | Patients with wellcharacterized partial epilepsy not fully controlled despite treatment with 1–2 AEDs | Placebo | 98 | 43 (43.9) | 37.5 (12.6) | 24.3 (12.2) | 17.8 |
| 5 mg | 97 | 49 (50.5) | 38.9 (11.6) | 22.2 (12.1) | 20.0 | |||
| 20 mg | 100 | 52 (52.0) | 37.3 (13.3) | 22.9 (14.0) | 22.5 | |||
| 50 mg | 101 | 51 (50.5) | 38.9 (12.3) | 26.2 (12.0) | 30.5 (P = 0.003) | |||
| Klein et al. (2014)8 (NCT00490035) | Prospective, multicenter, doubleblind, randomized, placebocontrolled | Patients with uncontrolled POS despite ongoing treatment with 1–2 AEDs | Placebo | 259 | 133 (50.9) | 39.8 (12.5) | 22.7 (13.3) | 17.6 |
| 100 mg | 252 | 102 (40.3) | 39.1 (13.4) | 22.2 (13.3) | 37.2 (P < 0.001) | |||
| 200 mg | 249 | 133 (53.2) | 39.8 (12.8) | 23.4 (14.6) | 35.6 (P < 0.001) | |||
| Kwan et al. (2014)9 (NCT00504881) | Prospective, multicenter, randomized, doubleblind, placebocontrolled, flexible dose | Patients with focal or generalized epilepsy uncontrolled on 1–3 AEDs | Placebo | 121 | 69 (57.0) | 36.5 (11.5) | – | 18.9 |
| BRV | 359 | 181 (50.4) | 35.6 (11.5) | – | 26.9 (P = 0.070) |
AEDs = antiepileptic drugs; BRV = brivaracetam; ITT = intention to treat; POS = partialonset seizure; SD = standard deviation.
Ryvlin et al.6
A phase 3, double-blind, randomized, placebo-controlled trial conducted across 88 centers throughout Europe and India evaluated brivaracetam versus placebo in 399 adults with POS. The objective of the study was to evaluate the efficacy, safety, and tolerability of brivaracetam versus placebo in patients with uncontrolled POS despite adequate therapy with one or two concomitant AEDs.
Eligible patients were randomized to receive brivaracetam 20 mg per day (BRV20), 50 mg per day (BRV50), 100 mg per day (BRV100), or placebo, administered twice daily in equal doses. The primary endpoint was percent reduction in baseline-adjusted POS frequency per week over the 12-week treatment period versus placebo. Secondary endpoints included median percent reduction from baseline in POS frequency per week, 50% or greater responder rate, and seizure freedom from all seizure types.
Ultimately, the study did not meet its primary efficacy endpoint. Percent reduction in baseline-adjusted POS frequency per week over placebo was 6.8% for BRV20 (P = 0.239), 6.5% for BRV50 (P = 0.261), and 11.7% for BRV100 (P = 0.019). However, median percent reduction from baseline in POS frequency per week was 30.0% for BRV20 (P = 0.019), 26.8% for BRV50 (P = 0.092), and 32.5% for BRV100 (P = 0.004), compared with 17% for placebo. Adverse events are listed in Table 2. The study concluded that while the primary efficacy analysis based on the BRV50 dose was not statistically significant, BRV100 significantly reduced POS frequency per week versus placebo.
Table 2.
Safety Data for Brivaracetam (100 mg per day)
| Adverse Event (Incidence ≥ 5%) | Rate (%) | |
|---|---|---|
| Ryvlin et al.6 | Klein et al.8 | |
| Somnolence | 8.0 | 19.4 |
| Dizziness | 5.0 | 10.3 |
| Fatigue | 8.0 | 7.5 |
| Headache | 9.0 | 6.7 |
| Urinary tract infection | N/R | 5.1 |
| Nasopharyngitis | 1.0 | N/R |
| Vertigo | 2.0 | N/R |
| Nausea | 1.0 | N/R |
| Irritability | 5.1 | N/R |
N/R = not reported.
Biton et al.7
A phase 3, prospective, multicenter, randomized, double-blind, placebo-controlled, parallel-group, fixed-dose trial conducted across 85 centers in Australia, Brazil, Canada, Mexico, and the U.S. evaluated brivaracetam versus placebo in 400 patients. The purpose of the study was to evaluate the efficacy, safety, and tolerability of brivaracetam compared with placebo in patients with uncontrolled POS.
Eligible patients were randomized to receive BRV5, BRV20, BRV50, or placebo, administered twice daily in equal doses. The primary endpoint was percent reduction over placebo in baseline-adjusted POS frequency per week over the 12-week treatment period. Secondary endpoints included median percent reduction from baseline in POS frequency per week and 50% or greater responder rate.
Percent reduction in POS frequency per 28 days over placebo reached statistical significance for BRV50 (22.0%; P = 0.004), but not for the other dose groups (BRV5 or BRV20). In addition, statistical significance was achieved for the 50% or greater responder rate in the BRV50 group compared with placebo (32.7% versus 16.7%; P = 0.008). BRV50 also displayed benefits with percent reduction in POS frequency from baseline compared with placebo (30.5% versus 17.8%; P = 0.003). The study concluded that adjunctive therapy with BRV50 offers significant reductions in the frequency of POS when compared with placebo.
Klein et al.8
A randomized, double-blind, placebo-controlled, multicenter trial conducted across 147 sites in 27 countries throughout North America, Europe, Latin America, and Asia evaluated brivaracetam versus placebo in 768 patients with uncontrolled POS despite treatment with one or two AEDs. Patients receiving concomitant levetiracetam were excluded.
Eligible patients were randomized to receive BRV100, BRV200, or placebo, administered twice daily in equal doses. The coprimary efficacy endpoints were percent reduction over placebo in 28-day adjusted POS frequency and 50% or greater responder rate based on percent reduction in POS frequency from baseline.
The study met both of its primary efficacy endpoints. Percent reduction in POS frequency per 28 days over placebo was 22.8% for BRV100 (P < 0.001) and 23.3% for BRV200 (P < 0.001). Similarly, the 50% or greater responder rate was 21.6% for placebo, 38.9% for BRV100 (P < 0.001), and 37.8% for BRV200 (P < 0.001).
Treatment-related adverse events occurred in 155 of 261 (59.4%) placebo patients versus 340 of 503 (67.6%) brivaracetam patients. (Table 2) Discontinuation rates due to treatment-related adverse effects were 3.8% for placebo, 8.3% for BRV100, and 6.8% for BRV200. The study concluded that adjunctive therapy with BRV100 and BRV200, without the concomitant use of levetiracetam, was beneficial in reducing POS frequency in patients with focal seizures, without resulting in significant safety or tolerability issues.
Kwan et al.9
A phase 3, double-blind, randomized, placebo-controlled, flexible-dose trial conducted across 74 sites in 15 countries throughout Europe and Asia evaluated varying doses of brivaracetam versus placebo in 480 patients with uncontrolled epilepsy (431 with POS, 49 with generalized epilepsy).
Eligible patients were randomized to receive placebo or brivaracetam, administered twice daily in equal doses. The brivaracetam was initiated at BRV20 and increased, as needed, to BRV150 during an eight-week period. This dose-finding period was followed by an eight-week fixed-dose maintenance period. The primary efficacy endpoint was percent reduction in baseline-adjusted POS frequency per week.
From October 2007 through December 2008, 90.0% of BRV-treated patients and 91.7% of placebo-treated patients completed the study. Baseline characteristics were largely similar between the two treatment groups. The study met its primary efficacy endpoint. In patients with POS, percent reduction in POS frequency from baseline was 26.9% for brivaracetam versus 18.9% for placebo (P = 0.070). The study concluded that adjunctive therapy with brivaracetam given at individualized doses ranging from 20–150 mg per day was well tolerated and effective at reducing seizure frequency in patients with uncontrolled epilepsy.
Summary of Meta-Analyses
Three meta-analyses reviewing the efficacy and safety of brivaracetam as an adjunctive therapy for POS were identified. The first included six randomized, placebo-controlled, single-or double-blind add-on trials involving 2,399 patients (1,715 receiving brivaracetam and 684 receiving placebo). The following endpoints were assessed: 50% or greater reduction in seizure frequency, seizure freedom, incidence of treatment-related adverse events, and treatment withdrawal. In regard to all of the primary endpoints, an x2 test indicated no significant statistical heterogeneity between the trials. It was determined that 45% of levetiracetam-naïve patients responded to brivaracetam and 19% to placebo, suggesting a 25% real response rate that was not attributable to placebo. Brivaracetam was found to be more effective than placebo in reducing seizure frequency by 50% or more when added to concomitant AEDs in patients with refractory partial epilepsy. While there was insufficient data to perform a dose–response regression analysis, the results of the trials suggest that a dose-dependent effect saturated when the dose of brivaracetam reached 50 mg per day. The authors concluded that brivaracetam was effective as an add-on treatment in adults with refractory focal epilepsy and may offer additional benefits in those patients who are levetiracetam-naïve.1
The second meta-analysis included five randomized, double-blind, placebo-controlled, parallel-group trials that assessed the efficacy and safety of brivaracetam compared with placebo as adjunctive therapy for patients with POS. Patients in the trials must have received at least one concomitant AED at a stable and optimal dosage prior to study commencement. Brivaracetam at doses of 20, 50, 100, and 150 mg per day was associated with significantly higher 50% responder rates. Brivaracetam 5 mg per day was not associated with any significant difference in 50% responder rate when compared with placebo. In addition, treatment-related adverse events varied depending on the dose. Brivaracetam dosed at 150 mg per day was more associated with somnolence than any other dose. Similarly, fatigue and irritability were associated with brivaracetam 50 mg per day. In conclusion, it was determined that the use of brivaracetam at doses greater than 5 mg per day resulted in statistically significant reductions in seizure frequency with respect to the 50% responder rate. Brivaracetam was mostly well tolerated, with the exception of some irritability and somnolence associated with the 50-mg and 150-mg per day doses, respectively.10
The third meta-analysis included five randomized, placebo-controlled, single- or double-blind add-on trials that investigated the efficacy and safety of brivaracetam at varying doses. The following endpoints were assessed: 50% or greater reduction in seizure frequency and seizure-free rates. Overall, the 50% responder rates of patients receiving brivaracetam 20, 50, or 100 mg per day were significantly higher than those receiving placebo (20 mg: risk ratio [RR] = 1.63, P = 0.003; 50 mg: RR = 2.00, P < 0.00001; 100 mg: RR = 1.80, P = 0.01). In addition, patients in all brivaracetam groups experienced higher seizure-free rates when compared with placebo regardless of dosage (RR = 4.11, P = 0.01). Patients receiving brivaracetam of any dosage experienced significantly higher rates of adverse effects compared with those receiving placebo, specifically somnolence (P = 0.02) and fatigue (P = 0.009). The authors concluded that brivaracetam demonstrated efficacy as an adjunctive treatment for refractory POS, as indicated by its statistically significant increases in the 50% responder rate (P < 0.00001) and seizure-free rate (P = 0.01).11
WARNINGS AND PRECAUTIONS
AEDs may increase the risk of suicidal behaviors or thoughts in patients taking these medications for any indication. Patients taking brivaracetam should be monitored for depression, suicidal ideations, or any unusual changes in mood and behavior.3
Brivaracetam may also cause dose-dependent increases in somnolence and adverse effects such as fatigue, malaise, sedation, and lethargy. In the phase 3 controlled, adjunctive epilepsy trials, these adverse effects were seen in 25% of patients randomized to receive at least 50 mg per day of brivaracetam compared with 14% of patients receiving placebo.3
Treatment with brivaracetam is associated with dizziness and disturbances in gait and coordination, such as vertigo, ataxia, and nystagmus. In the phase 3 controlled adjunctive epilepsy trials, these adverse reactions were reported in 16% of patients randomized to receive at least 50 mg per day of brivaracetam compared with 10% of patients receiving placebo. The risk of gait disturbances is greatest early in treatment, but may occur at any time throughout therapy.3
Brivaracetam is also associated with psychiatric adverse events, including nonpsychotic symptoms, such as irritability, anxiety, aggression, anger, agitation, and depression, and psychotic symptoms, such as paranoia and acute psychosis. In the phase 3 controlled, adjunctive epilepsy trials, these adverse reactions were reported in 13% of patients randomized to receive at least 50 mg per day of brivaracetam compared with 8% of patients receiving placebo.3
Brivaracetam is also associated with hypersensitivity reactions, namely bronchospasm and angioedema. The medication should be discontinued in patients who develop hypersensitivity reactions after being treated with brivaracetam.3
DRUG–DRUG INTERACTIONS
Due to the potential for CYP2C19 induction, coadministration with rifampin decreases the plasma concentrations of brivaracetam. The dose may need to be doubled in patients receiving concomitant treatment with rifampin.3
Coadministration with carbamazepine may increase exposure to its active metabolite, carbamazepine-epoxide. While existing data did not reveal any safety concerns in patients receiving concomitant treatment with carbamazepine, the dose of carbamazepine may need to be reduced if tolerability issues arise during therapy.3
Because brivaracetam may increase the plasma concentrations of phenytoin, phenytoin levels should be monitored when brivaracetam is added to or removed from ongoing phenytoin therapy.3
When coadministered with levetiracetam, brivaracetam provided no additional therapeutic benefit.3
SPECIAL POPULATIONS
Pregnancy and Lactation
Brivaracetam is in pregnancy category C, and there are currently no well-controlled studies in pregnant women. However, in animal studies, there was evidence of developmental toxicity at plasma exposures greater than clinical exposures. Therefore, brivaracetam should only be used in pregnant patients if the potential benefit outweighs the risk to the fetus. In addition, pregnant patients taking brivaracetam are advised to enroll in the North American Antiepileptic Drug Pregnancy Registry at 1-888-233-2334 or www.aedpregnancyregistry.org. No data are available on the excretion of brivaracetam in human milk. However, in rat studies, it was found that brivaracetam is excreted in milk.3
Pediatric and Geriatric Use
The safety and efficacy of brivaracetam has not been established in patients younger than 16 years of age. However, in juvenile rats and dogs, potential adverse effects on postnatal growth and development were observed. In addition, in the double-blinded, placebo-controlled epilepsy trials, there were too few patients ages 65 years or older to assess the medication’s efficacy. However, dose selection for elderly patients should begin at the lower end of the dosing range and should be made with careful consideration of the patient’s hepatic function, renal function, and other drug therapy.3
Renal and Hepatic Impairment
Patients with impaired renal function do not require dose adjustments of brivaracetam. However, the medication is not recommended in patients with end-stage renal disease receiving dialysis because there are no data in this patient population. For patients with any stage of hepatic impairment, the recommended starting dose of brivaracetam is 25 mg twice daily and the recommended maximum dose is 75 mg twice daily.3
DOSAGE AND ADMINISTRATION
The recommended starting dose for brivaracetam is 50 mg twice daily (100 mg total daily dose).3 Gradual dose escalation is not necessary when initiating treatment. The dosage may be adjusted down to 50 mg daily or up to 200 mg daily depending on patient tolerability and therapeutic response.2 Brivaracetam is available as an oral tablet (10 mg, 25 mg, 50 mg, 75 mg, and 100 mg), oral solution (10 mg/mL), and intravenous (IV) injection (50 mg/mL). If oral administration of brivaracetam is not feasible, the injectable form may be administered at the same dosage and frequency as the tablets and oral solution. However, it is important to note that the clinical study experience with brivaracetam injection is limited to four consecutive days of therapy.3
The oral tablets and solution may be taken with or without food. Brivaracetam tablets should be swallowed whole with liquid and not chewed or otherwise crushed. The oral solution should be measured out and delivered with a calibrated measuring device in order to accurately deliver the prescribed dose. The oral solution does not need to be diluted and may be administered using a nasogastric or gastrostomy tube. Any unused brivaracetam oral solution should be discarded after five months of opening the bottle.3
Brivaracetam injection is for IV use and is single-dose only. The injection does not need to be diluted, though it may be mixed with the following diluents: 0.9% sodium chloride injection USP, lactated Ringer’s injection, or 5% dextrose injection USP. The injection should be administered over two to 15 minutes. If diluted, the solution may be stored in PVC bags, but must not be stored for more than four hours at room temperature. Generally, the medication may be stored at 25°C (77°F), with excursions permitted between 15°C to 30°C (59°F to 86°F). The injection and oral solution formulations should not be frozen.3
COST
Brivaracetam is supplied in three formulations: 10-mg, 25-mg, 50-mg, 75-mg, and 100-mg tablets; 10-mg/mL oral solution; and 10-mg/mL injection for IV administration.3 The 10-mg tablets are available for dose titration. The average wholesale price (AWP) for a 60-tablet package of all dosages of the tablet formulation or for the 300-mL bottle of oral solution is $1,092.12 The AWP for a package of 10 single-dose 5-mL vials for IV administration is $468.12
P&T COMMITTEE CONSIDERATIONS
Brivaracetam is an FDA-approved medication indicated as adjunctive therapy in patients with POS. Clinical studies have evaluated the safety and efficacy of brivaracetam in comparison with treatment with placebo and found that brivaracetam (dosed 50 mg per day, 100 mg per day, or 200 mg per day) demonstrates significant reductions in POS frequency across all doses (P < 0.01 for all arms). Brivaracetam is available in tablet, oral solution, and injection formulations with a price that is comparable to other FDA-approved therapies for adjunctive treatment of POS. The oral formulations are available with flat pricing; therefore, all strengths would likely need to be added to a drug formulary.
Despite promising data from clinical studies, there is a lack of evidence suggesting that brivaracetam offers any benefit over other AEDs, such as levetiracetam. While the available data suggests brivaracetam may provide some benefit over placebo, this is not sufficient cause for it to be included on hospital formularies. Brivaracetam may have a role as an adjunctive therapy for patients whose epilepsy remains uncontrolled despite taking one to two concomitant AEDs.
CONCLUSION
Brivaracetam is a racetam derivative and SV2A ligand approved as adjunctive therapy for the treatment of POS in adults and adolescents 16 years of age and older. This medication has shown promise in patients with epilepsy whose seizures persist despite adequate treatment. Brivaracetam was well tolerated throughout all three phase 3 trials, which led to its FDA approval. The drug offers improved seizure control with minimal safety risks for patients with epilepsy.
Footnotes
Disclosure: The authors report no financial or commercial relationships in regard to this article.
REFERENCES
- 1.Lattanzi S, Cagnetti C, Foschi N, et al. Brivaracetam add-on for refractory focal epilepsy: a systematic review and meta-analysis. Neurology. 2016;86(14):1344–1352. doi: 10.1212/WNL.0000000000002545. [DOI] [PubMed] [Google Scholar]
- 2.Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 3.Briviact (brivaracetam) prescribing information. Smyrna, Georgia: UCB, Inc.; 2016. [Google Scholar]
- 4.Synaptic vesicle glycoprotein 2A gene (protein coding) GeneCards Human Gene Database. [Accessed May 16, 2016]. Available at: www.genecards.org/cgi-bin/carddisp.pl?gene=SV2A.
- 5.Kaminski RM, Gillard M, Klitgaard H. Targeting SV2A for discovery of antiepileptic drugs. In: Noebels JL, Avoli M, Rogawski MA, et al., editors. Jasper’s Basic Mechanisms of the Epilepsies [Internet] 4th ed. Bethesda, Maryland: National Center for Biotechnology Information (US); 2012. [Accessed May 16, 2016]. Available at: www.ncbi.nlm.nih.gov/books/NBK98183. [PubMed] [Google Scholar]
- 6.Ryvlin P, Werhahn KJ, Blaszczyk B, et al. Adjunctive brivaracetam in adults with uncontrolled focal epilepsy: results from a double-blind, randomized, placebo-controlled trial. Epilepsia. 2014;55(1):47–56. doi: 10.1111/epi.12432. [DOI] [PubMed] [Google Scholar]
- 7.Biton V, Berkovic SF, Abou-Khalil B, et al. Brivaracetam as adjunctive treatment for uncontrolled partial epilepsy in adults: a phase III randomized, doubleblind, placebo-controlled trial. Epilepsia. 2014;55(1):57–66. doi: 10.1111/epi.12433. [DOI] [PubMed] [Google Scholar]
- 8.Klein P, Schiemann J, Sperling MR, et al. A randomized, double-blind, placebo-controlled, multicenter, parallel-group study to evaluate the efficacy and safety of adjunctive brivaracetam in adult patients with uncontrolled partial-onset seizures. Epilepsia. 2015;56(12):1890–1898. doi: 10.1111/epi.13212. [DOI] [PubMed] [Google Scholar]
- 9.Kwan P, Trinka E, Van Paesschen W, et al. Adjunctive brivaracetam for uncontrolled focal and generalized epilepsies: results of a phase III, double-blind, randomized, placebo-controlled, flexible-dose trial. Epilepsia. 2014;55(1):38–46. doi: 10.1111/epi.12391. [DOI] [PubMed] [Google Scholar]
- 10.Tian X, Yuan M, Zhou Q, et al. The efficacy and safety of brivaracetam at different doses for partial-onset epilepsy: a meta-analysis of placebo-controlled studies. Expert Opin Pharmacother. 2015;16(12):1755–1767. doi: 10.1517/14656566.2015.1058360. [DOI] [PubMed] [Google Scholar]
- 11.Ma J, Huang S, You C, et al. Adjunctive brivaracetam for patients with refractory partial seizures: A meta-analysis of randomized placebo-controlled trials. Epilepsy Res. 2015;114:59–65. doi: 10.1016/j.eplepsyres.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 12.Red Book Online. Ann Arbor, Michigan: Truven Health Analytics; [Accessed December 19, 2016]. [Google Scholar]


