Abstract
Introduction:
Consensual ophthalmotonic reaction (COR) was first described in 1924. Studies following monocular application of glaucoma drops and laser trabeculoplasty showed a drop in fellow eye intraocular pressure (IOP). However, studies following monocular surgery showed heterogeneous results. The purpose of this study was to investigate the COR in Chinese patients who have received monocular filtration surgery.
Methods:
A noncomparative retrospective study of 65 eyes undergoing filtration surgery in Queen Mary Hospital was conducted. The IOP was obtained at baseline and postoperative days 1, 3, 7 and 14. Patient's age, sex, type of glaucoma and surgery, preoperative medications, postoperative bleb status, and number of interventions were tabulated. The postoperative IOP measurements over both eyes were obtained, and the readings were averaged to decrease the chances of extreme readings being a one-off event and allow for regression to the mean bias.
Results:
COR was observed in the unoperated fellow eye. The mean preoperative IOP and averaged postoperative IOP were 17.2 ± 5.2 mm Hg and 20.1 ± 8.9 mm Hg, respectively (P < 0.04). All medications were continued in the fellow eye or even stepped up. Twenty-three percent of patients demonstrated fellow eye IOP rise >30% from baseline, while none showed IOP drop >30% from baseline.
Discussion:
Following monocular penetrating filtration surgery, our Chinese population demonstrated a significant fellow eye IOP increase in the early postoperative period. We should bear in mind the influence of COR and take care to measure the fellow eye IOP following monocular surgery.
Keywords: consensual ophthalmotonic reaction, ExPRESS shunt, glaucoma surgery, intraocular pressure, trabeculectomy
1. Introduction
Consensual ophthalmotonic reaction (COR) is a phenomenon whereby alterations of intraocular pressure (IOP) in one eye are accompanied by a corresponding pressure change in the fellow eye. This phenomenon was first described in 1924 by Weekers[1] through animal studies.
In human studies, COR following monocular application of IOP-lowering medications has been documented. A retrospective review by Gibbens[2] studied the fellow eye IOP response after monocular application of glaucoma eyedrops in 13 normal and 13 ocular hypertensive subjects. A consensual fall in the fellow eye IOP was observed, but only reached significant levels in hypertensive and not in normotensive subjects. COR was also observed in the Ocular Hypertensive Treatment Study, where monocular application of timolol resulted in statistically significant fellow eye IOP reduction.[3] The degree of fellow eye IOP reduction was found to be associated with both the degree of IOP reduction in the treated eye and the baseline IOP of the fellow eye.
A similar COR has also been observed 6 months after monocular selective laser trabeculoplasty (SLT) application,[4] and also after argon laser trabeculoplasty,[5] with the fellow eye demonstrating IOP reduction.
For COR following surgery, the incidence has been reported to be around 10%. Intriguingly, COR following trabeculectomy have shown diverse outcomes, with studies having shown an increase, decrease or no change in fellow eye IOP.[6–8] This may be due to differences in the type of glaucoma, preoperative IOP, surgical technique, anti-metabolite dosage and duration, timing of postoperative measurements, and also outflow facility of the fellow eye.
2. Materials and methods
The purpose of our study was to investigate COR in Chinese patients who had received either augmented trabeculectomy or ExPRESS shunt implantation. The study adhered to the tenets of the Declaration of Helsinki and has been approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
A retrospective review of all glaucoma surgeries performed at Queen Mary Hospital from January 2014 to January 2015 was conducted. A total of 65 glaucoma surgeries were conducted. All trabeculectomies and ExPRESS shunt implantations were performed by surgeons from our glaucoma team with a standardized technique. Topical anesthesia with 0.4% Novain with or without the addition of subtenon anesthesia with 1% lignocaine was applied. All conjunctival flaps were fornix-base. A partial-thickness scleral flap of size 4 × 3 mm was created. Mitomycin C (MMC, 0.4 mg/mL) was then applied subconjunctivally and underneath the sclera flap for 3 minutes, followed by irrigation with 50 mL of balanced salt solution. A paracentesis wound was created with a 15 degree stab knife at the temporal clear cornea. For trabeculectomy, the anterior chamber was entered with a 15 degree stab knife from just behind the hinge of the scleral flap. This entrance was then enlarged with a Kelly punch and a surgical peripheral iridectomy was created. For ExPRESS shunt implantation, the shunt model P50 was used. A 25 or 27 gauge needle was used to enter the anterior chamber just anterior to the scleral spur and the ExPRESS shunt was then implanted. The scleral flap was then closed with 10–0 nylon sutures and the conjunctiva was closed with either 8–0 or 9–0 vicryl. Postoperative topical medications included 0.5% levofloxacin 4 times a day and 1% prednisolone acetate 6 to 8 times a day. The patients were then seen postoperatively at 1 day, 3 days, 1 week, and 2 weeks. Inclusion criteria were Chinese patients who received either augmented trabeculectomy or ExPRESS shunt implantation. Exclusion criteria included patients who underwent trabectome, nonpenetrating surgeries, and glaucoma drainage device insertions. Patients who underwent simultaneous bilateral trabeculectomy or glaucoma surgeries were excluded. Patients with a phthisical fellow eye were excluded due to difficulty in obtaining a fair fellow eye IOP measurement. Patients with known steroid response, uveitic glaucoma and congenital or juvenile glaucoma were excluded to decrease confounding factors.
The patient's age, sex, type of glaucoma, type of surgery, preoperative medications, postoperative index eye bleb status, and number of interventions were tabulated. The IOP was recorded preoperatively and at postoperative days 1, 3, 7, and 14 by either noncontact tonometry or goldmann applanation tonometry to obtain a fair estimation of the early postoperative IOP, decrease the effect of one-off events contributing to extreme measurements and to allow for the regression to the means, postoperative IOP measurement was averaged over the 4 time points mentioned above, and those with incomplete data on the fellow eye IOP for 2 postoperative visits were excluded from analysis. After accounting for the above exclusion criteria, 25 eyes from 22 subjects were available for analysis. As 3 of these subjects subsequently underwent filtration surgery for their fellow eye, these 3 sets of data were excluded to avoid bias of double counting.
In analysis of postoperative IOP change, we adopted the cut-offs of 30% and 50% change from baseline to reflect a significant change from baseline.[6]
Data are presented as mean ± standard deviation. A statistical analysis of the data was conducted with SPSS version 20 (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Wilcoxon signed rank test was used to compare preoperative and postoperative IOP. A P value <0.05 was considered to reflect significance.
3. Results
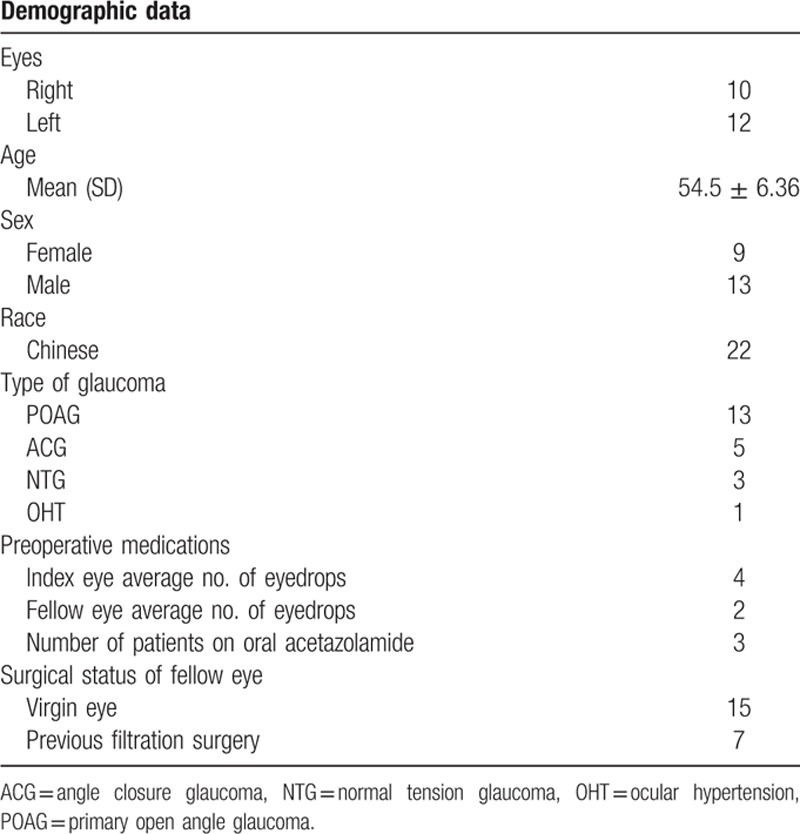
Demographic preoperative data, the type of glaucoma, and preoperative medications are shown in Table 1.
Table 1.
Demographic data, type of glaucoma, and preoperative medications of subjects.
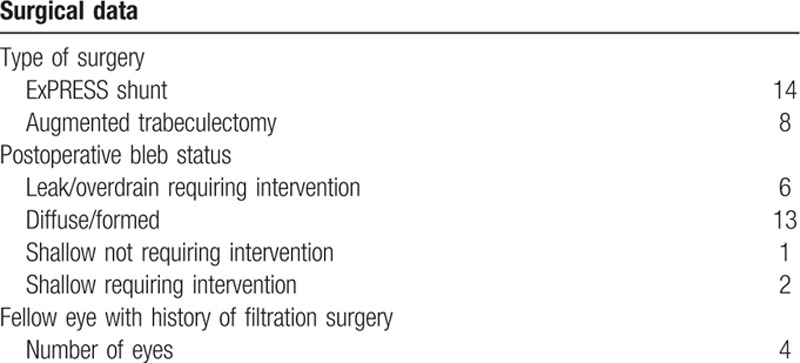
The type of surgery conducted and postoperative bleb status of the index operated eye are shown in Table 2. Intervention for a postoperative leaking or overdraining bleb consisted of anterior chamber reformation and bleb revision within 1 month. Intervention for a postoperative shallow bleb consisted of laser suturelysis or needling within 1 month.
Table 2.
Surgical data—type of surgery, postoperative bleb status of index operated eye, fellow eye history of filtration surgery.
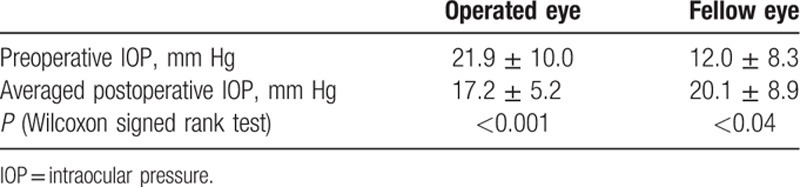
The preoperative and postoperative IOP for the operated eye and fellow eye is shown in Table 3. For the operated eye, the preoperative IOP was 21.9 ± −10.0 mm Hg. The postoperative IOP averaged over 2 weeks was 12.03 ± 8.3mm Hg, showing a significant difference (P < 0.001, Wilcoxon signed ranks test). Indications for filtration surgery included suboptimal disease control with present IOP and medication intolerance. For the fellow eye, the preoperative IOP was 17.2 ± 5.2 mm Hg. The postoperative IOP averaged over 2 weeks was 20.1 ± 8.9 mm Hg, also showing a significant difference (P < 0.04, Wilcoxon signed ranks test).
Table 3.
Preoperative and postoperative IOP of the operated eye and fellow eye.
For the operated index eye, all glaucoma medications were discontinued postoperatively. For the unoperated fellow eye, all glaucoma medications were either continued or even stepped up during the study period.
In our study, 23% of patients demonstrated fellow eye IOP rise >30% from baseline. Among these patients, two-thirds had bleb leak or overdrainage in the operated eye, to the extent that intervention was required. The remaining one-third had diffuse or formed blebs. None of those who demonstrated fellow eye IOP rise >30% had shallow blebs. Half of these patients underwent trabeculectomy and half underwent ExPRESS shunt implantation. Previous filtration surgery for the fellow eye was performed in 40% of these patients.
Nine percent of patients showed fellow eye IOP rise >50% from baseline. None of our patients demonstrated fellow eye IOP drop >30% from baseline.
Tables 4 and 5 show the outcome of subgroup analysis. Subgroup analysis was performed on the fellow eye in subjects who underwent augmented trabeculectomy and ExPRESS shunt, respectively. The difference between preoperative IOP and postoperative IOP averaged over 2 weeks was statistically significant in those that underwent augmented trabeculectomy (P = 0.017) but fell short of significance in those that underwent ExPRESS shunt implantation.
Table 4.
Subgroup analysis of COR presence according to surgery type.
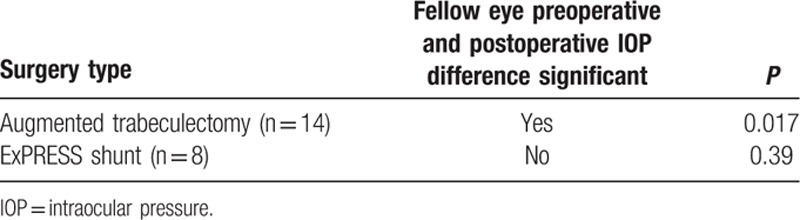
Table 5.
Subgroup analysis of COR presence according to surgery status of fellow eye.
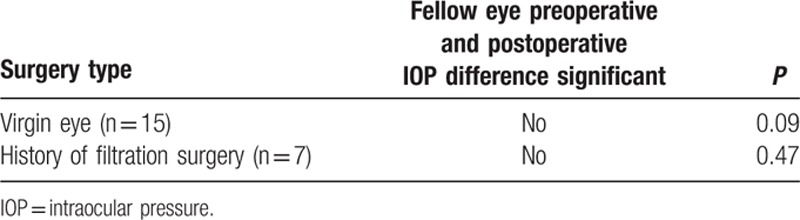
Subgroup analysis was also performed on subjects with virgin fellow eyes and fellow eyes with history of filtration surgery, respectively, comparing the difference in fellow eye preoperative and postoperative IOP. While subjects with fellow virgin eyes showed a difference that fell short of reaching statistical significance (P = 0.09), subjects with fellow eyes history of filtration surgery showed no significant difference (P = 0.47).
Spearman correlation test was performed for the drop in IOP of the index eye and the rise in IOP of the unoperated fellow eye. Spearman correlation coefficient suggests a positive correlation, although it was short of reaching statistical significance (r = 0.22, P = 0.16).
4. Discussion
Many hypotheses have been put forth to explain COR, and among them is a central nervous reflex mechanism. The sympathetic nervous system has been suggested to play a role, with the COR being blunted by pretreatment with guanethidine and also in patients with Horner syndrome.[9] Animal studies show a role of the parasympathetic nervous system as well, with the COR not observed in atropinized rabbits.[10] Regarding COR occurring after monocular application of medication, we cannot exclude the effects of systemic absorption and also contamination of the other eye. For COR occurring after monocular laser trabeculoplasty, one needs to take into account the effects of systemic release of humoral agents such as matrix metalloproteinase, and also improved medication compliance following laser.
While COR triggered by medications and laser seem to show a similar pattern, COR following glaucoma surgery has shown heterogeneous results.[6–8] When contemplating these results, it might be helpful to take note that IOP is not the only parameter that is affected bilaterally after a unilateral inciting event. Koktekir et al[11] reported a case of bilateral severe anterior uveitis occurring 3 weeks after unilateral application of SLT in an open angle glaucoma patient. A classic example of the status of one eye triggering a response in the fellow eye would be sympathetic ophthalmia.
IOP regulation has been shown to be influenced by neural, vascular, hormonal, and also humoral factors, which in turn is regulated by a central mechanism. Both mechanical and chemical triggers have been observed in COR. Beitch et al[12] had observed that intracameral prostaglandin injection into one eye could trigger IOP rise in both the index and fellow eye, while the miotic effect was observed in only the index eye. Diestelhorst et al[13] measured the aqueous flow of the unoperated fellow eye before and 5 days after trabeculectomy using fluorophotometry. A significant rise in aqueous flow was reported, without any significant change in IOP. These findings suggest that the central regulation of IOP may target aqueous secretion, and the IOP response is also dependent on whether the outflow facility is sufficient for the increased outflow. Yarangumeli et al[6] reported an increase in fellow eye IOP. In their case series, all of the fellow eyes were virgin eyes. In contrary to our findings, Vysniauskiene et al[7] reported a reduction in fellow eye IOP. In their case mix, half of the patients received previous trabeculectomy on their fellow eye, and among them, COR was also less pronounced. However, in our study population, subgroup analysis comparing fellow virgin eyes and those with history of filtration surgery showed no difference in COR. The authors believe the above examples suggest that there is a myriad of factors in play affecting COR after surgery, rendering the situation more complicated when compared with COR after mediation and laser application.
Our results show a significant increase in postoperative fellow eye IOP. When interpreting these results, note that an average of the postoperative IOP measurements over 2 weeks were taken. During this period, fellow eye medications had been either maintained or stepped up. Thus, the rise in fellow eye IOP was not due to any one-off events or stepping down of glaucoma medications. Moreover, after receiving monocular filtration surgery, 3 patients had developed uncontrolled IOP in the fellow eye to the extent that filtration surgery was required for the fellow eye. This was done 5 weeks postoperatively for 2 patients and 3 months postoperatively for 1 patient. Although subsequent data of these 3 eyes were excluded, 1 subject developed fellow eye raise in IOP of >130% from baseline.
Our study is unique and different from previous studies in several aspects. Our study population is Chinese. Culturally Chinese patients tend to be more conservative when confronted with the choice of surgery. Indeed, all of our subjects were on either topical or systemic medications for the operated eye, while for some quoted studies, a portion of patients underwent filtration surgery as first line of glaucoma management, and were not on preoperative medications. Our study was the first to include ExPRESS shunt surgeries in our analysis. ExPRESS shunt has been shown to have a lower incidence of overfiltration due to its small internal diameter limiting flow.[14] This may account for the preoperative and postoperative IOP in fellow eyes of patients being statistically different in those undergoing augmented trabeculectomy but not those undergoing ExPRESS shunt implantation. Our study's analysis also involved an averaged postoperative IOP, and tabulated the operated eye's postoperative bleb status. The majority of patients showing fellow eye IOP rise required intervention for a leaking or overdraining bleb. This is in line with Diestelhorst's hypothesis that a collapse in anterior chamber had resulted in a compensatory rise in aqueous flow in attempt to achieve homeostasis.
Limitations of our study include its retrospective nature and small sample size. Different surgeons were involved in the surgeries. Also, IOP measurement was obtained by different machines (noncontact or goldmann applanation tonometry), different investigators, and at different times throughout the day.
When reviewing the literature, the authors note that postsurgical COR seems to occur at an earlier time frame than postlaser COR. This may suggest mechanical triggers play a heavier role than chemical triggers in postsurgical COR. Further studies are needed to confirm the above hypothesis.
In conclusion, it is pertinent not to overlook the fellow eye IOP in the early postoperative stage following a penetrating glaucoma filtration surgery. Potential factors at play in affecting postoperative fellow eye IOP may include, but are not limited to the following: the type and number of preoperative medications, the magnitude of IOP drop, the postoperative bleb status of the operated eye, the outflow facility of the fellow eye, inflammatory changes, uveal blood circulation changes, timing of measurement, and also improved drug compliance. Future prospective studies and a more macroscopic overview are suggested to further delineate the underlying mechanisms of postsurgical COR.
Footnotes
Abbreviations: COR = consensual ophthalmotonic reaction, IOP = intraocular pressure, SLT = selective laser trabeculoplasty.
Authorship: All authors have made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors have been involved in drafting the manuscript or revising it critically. All authors have given final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding/support: The study received no funding.
The authors report no conflicts of interest in this work and they have no proprietary interests.
References
- 1.Weekers L. Modification expérimentales de l’ophtalmotonous. Reaction ophtalmotonique consenuelle. Arch Opthalmol (Paris) 1924; 41:641–658. [Google Scholar]
- 2.Gibbens MV. The consensual ophthalmotonic reaction. Br J Ophthalmol 1988; 72:746–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piltz J, Gross R, Shin DH, et al. Contralateral effect of topical beta-adrenergic antagonists in initial one-eyed trials in the ocular hypertension treatment study. Am J Ophthalmol 2000; 130:441–453. [DOI] [PubMed] [Google Scholar]
- 4.Rhodes KM, Weinstein R, Saltzmann RM, et al. Intraocular pressure reduction in the untreated fellow eye after selective laser trabeculoplasty. Curr Med Res Opin 2009; 25:787–796. [DOI] [PubMed] [Google Scholar]
- 5.Brooks AM, West RH, Gillies WE. Argon laser trabeculoplasty five years on. Aust N Z J Ophthalmol 1988; 16:343–351. [DOI] [PubMed] [Google Scholar]
- 6.Yarangumeli A, Koz OG, Kural G. The effect of trabeculectomy on the intraocular pressure of the unoperated fellow eye. J Glaucoma 2003; 12:108–113. [DOI] [PubMed] [Google Scholar]
- 7.Vysniauskiene I, Shaarawy T, Flammer J, et al. Intraocular pressure changes in the contralateral eye after trabeculectomy with mitomycin C. Br J Ophthalmol 2005; 89:809–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Detorakis ET, Tsiklis N, Pallikaris IG, et al. Changes in the intraocular pressure of fellow untreated eyes following uncomplicated trabeculectomy. Ophthalmic Surg Lasers Imaging 2011; 42:138–143. [DOI] [PubMed] [Google Scholar]
- 9.Gibbens MV. Sympathetic influences on the consensual ophthalmotonic reaction. Br J Ophthalmol 1988; 72:750–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prijot EL, Stone HH. On the ophthalmotonic consensual reaction and its relationship to aqueous humor dynamics. Am J Ophthalmol 1956; 42:50–58. [DOI] [PubMed] [Google Scholar]
- 11.Koktekir BE, Gedik S, Bakbak B. Bilateral severe anterior uveitis after unilateral selective laser trabeculoplasty. Clin Experiment Ophthalmol 2013; 41:305–307. [DOI] [PubMed] [Google Scholar]
- 12.Beitch BR, Eakins KE. The effects of prostaglandins on the intraocular pressure of the rabbit. Br J Pharmacol 1969; 37:158–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diestelhorst M, Krieglstein G. The effect of trabeculectomy on the aqueous humor flow of the unoperated fellow eye. Graefes Arch Clin Exp Ophthalmol 1991; 229:274–276. [DOI] [PubMed] [Google Scholar]
- 14.Wang W, Zhou M, Huang W, et al. Ex-PRESS implantation versus trabeculectomy in uncontrolled glaucoma: a meta-analysis. PLoS One 2013; 8:e63591. [DOI] [PMC free article] [PubMed] [Google Scholar]


