Abstract
In many European countries, migrants utilize cancer screening less often than non-migrants. In Germany, in contrast, higher rates of utilization among migrants as compared with non-migrants have been reported. The role of demographic and socioeconomic factors potentially confounding the association between migration status and participation in screening, however, could not be studied. The present study aims to investigate the utilization of cancer screening among migrant and nonmigrant women residing in Germany, adjusting for potential confounders.
We used self-reported information from women surveyed on whether they have ever participated in screening for cancer (n = 11,709). The data was collected as part of a cross-sectional representative telephone survey conducted by the Robert Koch-Institute in 2010. We distinguished between three groups of women: (1) respondents of non-German nationality, those who had immigrated to Germany after their birth or those who have two foreign-born parents (“migrants with two-sided migration background”), (2) respondents who only have one foreign-born parent (“migrant with one-sided migration background”), and (3) all others (“non-migrants”).
To account for confounders, logistic regression analysis was performed. Only individuals proficient in German were included in the survey, allowing to control for a bias arising from poor language proficiency.
84.9% of nonmigrant women, 82.1% of women with a one-sided, and 70.5% of women with a two-sided migration background had utilized screening for cancer at least once in their lifetime before the survey. The adjusted odds ratios (OR) as compared with nonmigrant women were 0.99 (95% confidence interval [95% CI]: 0.77–1.27) and 0.55 (95% CI: 0.47–0.64), respectively.
The study shows that migrant women with a two-sided migration background residing in Germany utilize screening for cancer less often than nonmigrant women—independently of demographic and socioeconomic factors. This is in line with findings from other countries. Likely, barriers that migrant women encounter limit them from taking informed choices. These barriers need to be identified and appropriate measures aiming to enhance informed decision making must be implemented.
Keywords: cancer, Germany, immigrants, minority, screening
1. Introduction
Migrants constitute an increasing share of the population in many European countries.[1] In Germany, around one fifth of the population is considered to have a “migration background.”[2] This comprises non-German nationals as well as German nationals whose parents or who themselves immigrated to Germany from another country after 1949.
Migrants and non-migrants differ from each other in many aspects of health. This includes differences in health status and health care outcomes[3–5] as well as in the utilization of health care services. Whereas studies have reported a higher utilization of general practitioner, hospital, and emergency outpatient ward care in migrants as compared with nonmigrant populations,[6,7] the situation is different for preventive services, which migrants utilize less frequently than non-migrants. This is particularly the case for migrant women[8] and is also reflected in the utilization of screening for cancer.[9–11]
Similar to other measures of secondary prevention, the rationale of cancer screening is to improve treatment outcomes through early diagnosis. Although cancer screening is associated with harms and benefits,[12–14] screening for several types of cancer is recommended by stakeholders on the global[15,16] and European[17–19] levels. In many countries, migrant women utilize cancer screening less often than the respective majority populations. For instance, a register-based study from the Netherlands reported that only 63% of “non-Western” national women utilize the national breast cancer screening program as compared with 83% of Dutch women.[9] Also using register-based data, Kristiansen et al[20] showed that migrant women from non-Western countries as compared with Danish-born women had a 45% and migrant women from Western countries had a 28% lower chance of participating in mammography screening. Similarly, self-reported data from the Swiss Health Survey 2002 show that 34.1% of Swiss women utilized mammography in the year before the survey. The respective proportions were considerably lower among non-Swiss women, ranging from 31.7% in Spaniards to 16.7% in nationals from Former Yugoslavia.[21] Comparable findings were reported from the United States,[22] Canada,[23,24] and Australia.[25] Studies which took into account the effect of confounding factors show that differences between migrant and nonmigrant women in the utilization of cancer screening are not only attributable to the influence of demographic and socioeconomic factors such as age, income, and education, commonly known to affect preventive behavior including the utilization of screening for cancer.[20,21,23–30] Aside from these factors, it is likely that barriers which migrants experience in the health care system resulting from poor language proficiency, discrimination, and cultural beliefs not sufficiently taken into account by health care institutions contribute to this differential.[31–33]
In Germany, the regular utilization of several screening and early detection measures is recommended for women of different age groups above the age of 20, addressing cervix, breast, and colorectal cancers.[34] Migrants with a residence status (this includes all migrants except refugees and asylum seekers[35,36]) are entitled to use these measures of secondary prevention as well as health care services in general free of charge as part of their social insurance. Although studies conducted in Germany—similar to those conducted in other countries—showed that migrants utilize preventive services such as vaccination[37,38] and rehabilitative care[39,40] less often than the majority population, little is known about the utilization of cancer screening in this population group. Berens et al[41] conducted a small-scale register-based study and examined the participation of women of Turkish and non-Turkish origin (aged 50–69 years) in a breast cancer screening program in five cities in Germany. Contradictory to most other studies in Europe, they found out that women of Turkish origin had a 17% higher chance of utilizing breast cancer screening than women of non-Turkish origin. The respective chances differed considerably with age. Women in the age group of 50 to 54, 55 to 59, and 60 to 64 years were at a 50%, 45%, and 12%, respectively, higher chance of participating in breast cancer screening than nonmigrant women of the same age. A lower proportion of utilization was only observed for women aged 65 to 69 years. Socioeconomic and other factors potentially confounding the association between migration status and participation in cancer screening could not be adjusted for by the authors. This contradictory finding warrants further research into the utilization of cancer screening among migrant women in Germany.
The aim of the present study was to examine the self-reported utilization of cancer screening among migrant and nonmigrant women in Germany. Unlike other studies, we focus on the lifetime participation in cancer screening in general in order to identify those who are particularly vulnerable by not using services on cancer screening at all. Aside from investigating whether potential differences in the rates of utilization are attributable to the influence of demographic and socioeconomic factors we also aimed to examine whether a similar age pattern as identified by Berens et al can be observed in self-reported data.
2. Methods
2.1. Data source
The study uses data from the “Health in Germany Updated 2010” survey (Gesundheit in Deutschland aktuell 2010, GEDA 2010), a nationally representative cross-sectional survey based on computer-assisted telephone interviews (CATI) carried out from September 2008 to July 2009 by the Robert Koch Institute, a body of the Federal Ministry of Health in Germany.[42] It is made available by the Robert Koch Institute for research purposes. The population from which the random sample was drawn comprises all adults in Germany aged ≥18 years who live in a private household with a landline telephone. The Galber–Häder method was employed, which is a modified version of the random-digit dialing (RDD) sampling design for telephone interviews. This method takes into account the specific structure of telephone numbers in Germany in order to achieve a representative sample. The overall sample size was 22,050 respondents of which 12,483 were women. The survey was conducted in German language. Therefore, it can only be considered representative for those migrants who are proficient in the German language. This allows us to exclude poor language proficiency as a potential covariate confounding the association between the utilization of screening and migration status. The survey was approved by the responsible commissioner for data protection on the federal and state levels and follows all necessary requirements and data-protection guidelines of the Federal data protection act. As the survey was fully anonymous, voluntary, and did not involve any experiments, no further ethical approval was necessary.[43]
2.2. Outcome and group variable
We assessed if the respondent has ever participated in a cancer screening (0 = no, 1 = yes). Only women who were ≥20 years were included in the analysis, which resulted in a sample consisting of 12,037 cases. Following the approach of other studies in the field, we distinguished between three groups of women: (1) respondents of non-German nationality, those who had immigrated to Germany after their birth or those who have two foreign-born parents (“migrants with two-sided migration background”), (2) respondents who only have one foreign-born parent (“migrant with one-sided migration background”), and (3) all others (“non-migrants”).
2.3. Covariates
We took into account common demographic, socioeconomic, and health variables which usually differ between migrants and non-migrants and which are also associated with the uptake of preventive services. Respondents’ age was considered as a variable with 10-year categories (20–29,…,70–79) (the dataset did not allow us to account for age as a continuous variable as this information was not available). In order to operationalize socioeconomic status (SES), we used three variables. These comprised the educational level (lower secondary, intermediate secondary, higher secondary, other [including primary], school dropout, and still enrolled/no degree), the occupational status (blue-collar, white-collar, civil service, self-employed/freelancer, other, and still enrolled/trainee/no vocational degree/never worked), and the monthly equivalized income in Euros (the variable was log-transformed in order to take into account the nonlinear relationship between income and many health-related outcomes). For relationship status we used a 6-category variable (married, divorced/widowed/separated, never married, in a relationship, and cohabiting). Finally, we took into account possible health differences between the population groups by controlling for self-rated health (very good, good, moderate, poor/very poor), the presence of chronic diseases (yes and no), smoking status (daily, sometimes, past, and never), and a prior cancer diagnosis (yes and no), each based on self-reported information.
All independent variables had <2% of missing values.
2.4. Statistical analysis
First, we compared the numbers and shares between migrants with two-/one-sided migration background and non-migrants regarding their participation rates in cancer screening, their socioeconomic, demographic, and health characteristics. To test for differences between migrants and non-migrants, χ2-square tests and analysis of variance (ANOVA) were used depending on the measurement level of variables.
To adjust for covariates, we fitted two logistic regression models. The first model included the migrant status variable, age, relationship status, and the health status variables. The second model additionally included the three socioeconomic variables. In a third model, we added an interaction term between the group and age variables to examine whether differences between the three groups in terms of the utilization of cancer screening differ with age.
As comparisons of odds ratio (OR) between models may be biased by unobserved heterogeneity,[44] we present average marginal effects (AME) along ORs in the results section.
3. Results
Of all women aged ≥20 years, 11,709 had valid information for the outcome and all independent variables. Table 1 shows the means and distributions of all variables stratified by the three groups of interest. Descriptive statistics revealed that women with a two-sided migration background differed from nonmigrant women with respect to almost all variables, whereas women with one-sided migration background were very similar to nonmigrant women regarding the majority of the variables.
Table 1.
Shares and means of participation in cancer screening and independent variables for women (aged ≥20 years) by migrant status.
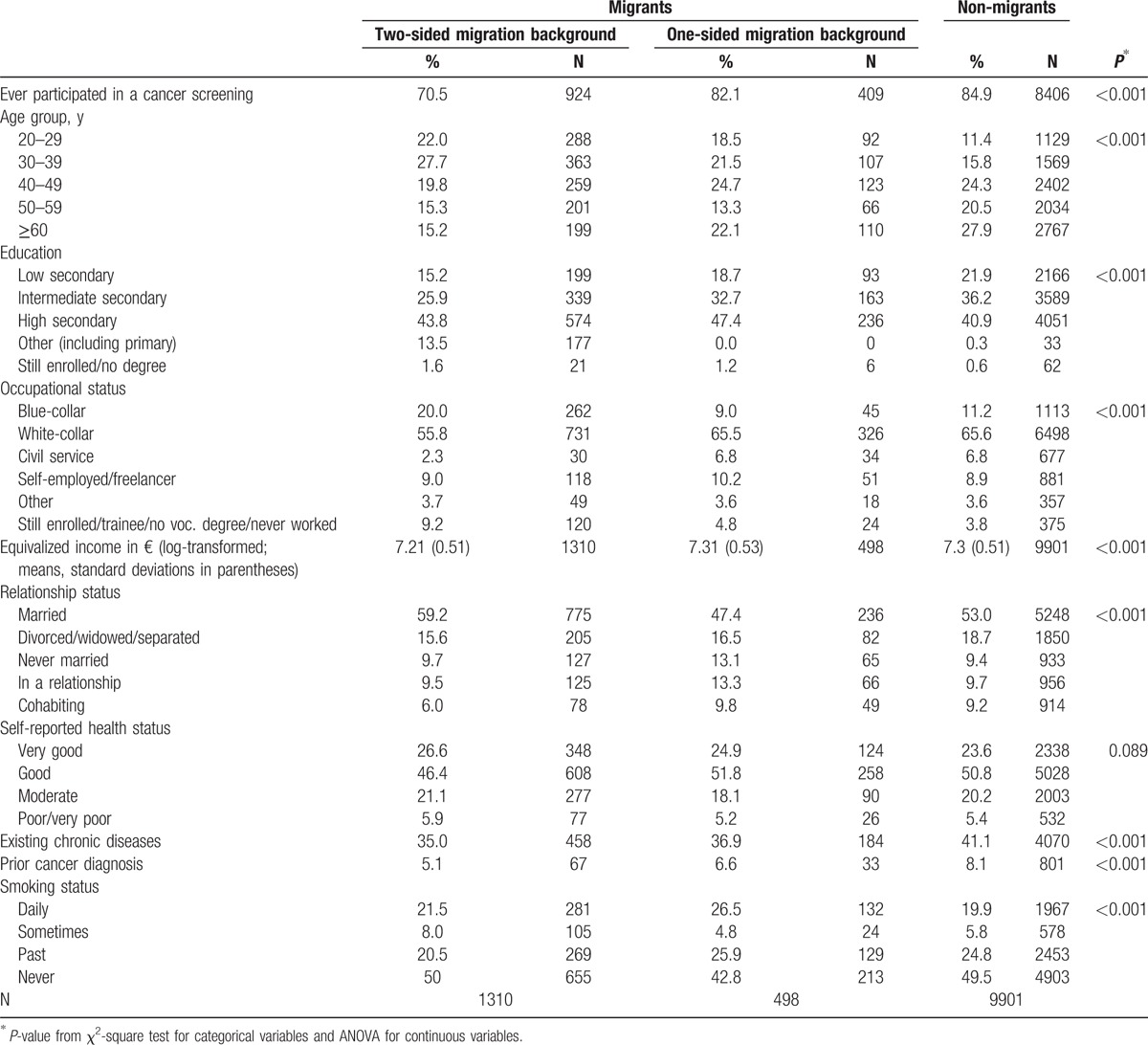
Women with two-sided migration background were younger than nonmigrant women and had a lower SES which became evident in a higher proportion of blue-collar workers and a lower income. In terms of health status, they reported a lower number of chronic diseases and previous cancers than nonmigrant women. The proportion of daily or occasional smokers, in contrast, was slightly higher than for non-migrants.
Regarding the utilization of cancer screening, nonmigrant women and women with a one-sided migration background reported a similar utilization (84.9% and 82.1%, respectively). Women with a two-sided migration background had significantly lower proportions of lifetime utilization (70.5%) meaning that about one third had never participated in any type of cancer screening.
Model 1 in Table 2 shows the results of the multivariable logistic regression for lifetime participation in cancer screening. All independent variables except SES were included. Migrant women with a two-sided migration background had a significantly lower chance than nonmigrant women for having participated in a cancer screening at least once in their lifetime (OR = 0.48). Again, no differences between non-migrants and migrants with a one-sided migration background could be observed (OR = 0.99). All covariates were significantly associated with the outcome. Age had a nearly linear and positive effect except for the oldest category (≥60 years) for which the participation rate decreased but still was significantly higher than for the reference group. A previous diagnosis of cancer, the presence of a chronic disease, being married, reporting a good health status, and not being a daily smoker increased the chance of the utilization of cancer screening significantly.
Table 2.
Odds ratios and average marginal effects from logistic regression models predicting the life-time participation in cancer.
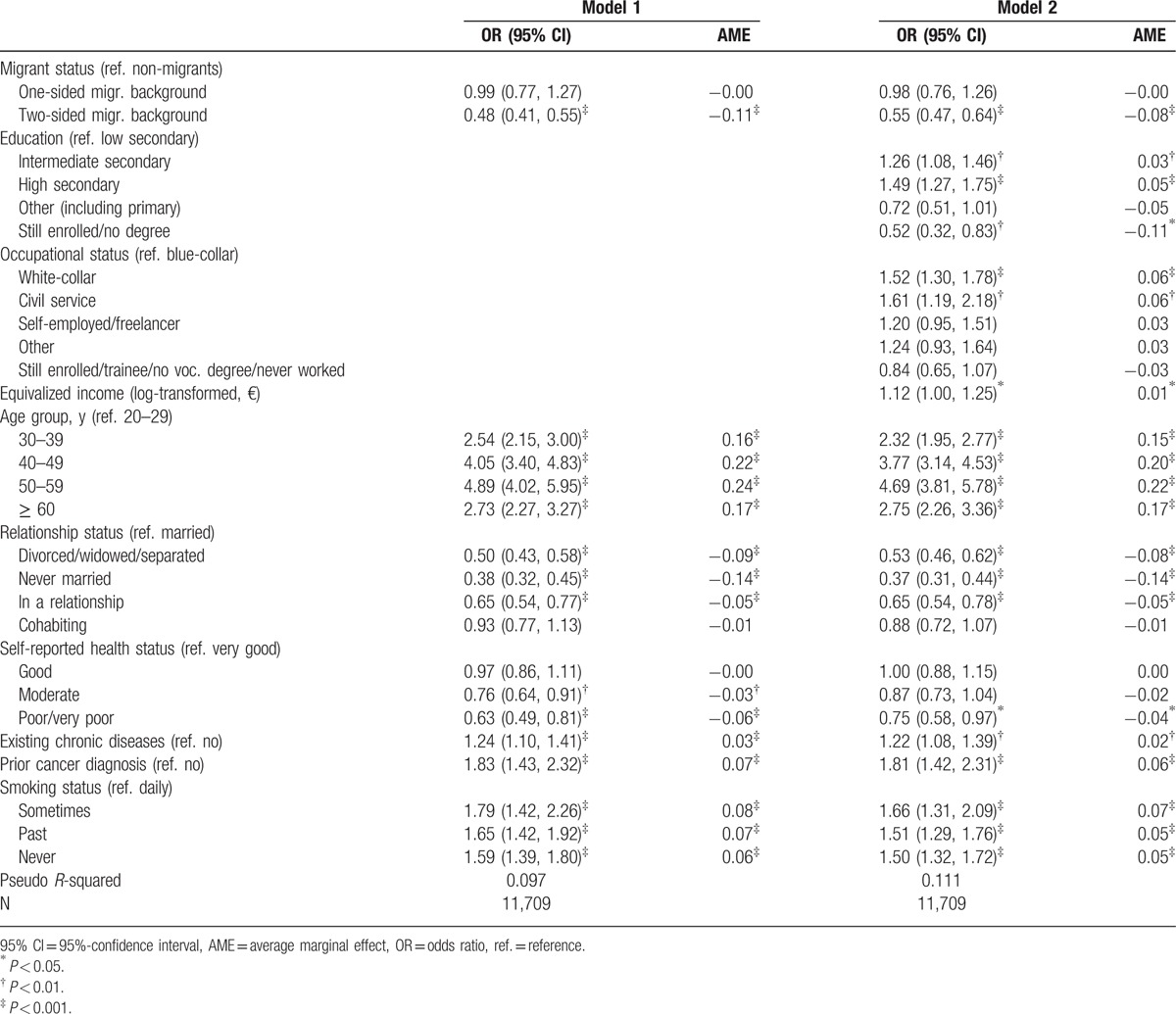
In Model 2, we additionally included the three socioeconomic variables, which were all significantly associated with lifetime participation in cancer screening. Respondents with intermediate and high secondary educational degrees had a higher chance of participation compared with those with a lower secondary degree, whereas the chance was lower for persons belonging to the category “other” which also includes individuals with a primary degree. Concerning the occupational status, blue-collar workers had a significantly lower chance of ever having participated in a cancer screening than white-collar employees and civil servants. Most importantly, adjusting for the socioeconomic variables could not explain the different participation rates between nonmigrant women and women with a two-sided migration background as the latter still had about half the chance of a lifetime participation than the former (OR = 0.55). In both models, AMEs were in line with ORs, indicating that unobserved heterogeneity between the models did not bias model comparison.
We also tested for interactions between age and the group variable in order to examine different age trends of participation rates between migrants and non-migrants. No significant interactions were identified (results not shown).
4. Discussion
Migrants utilize preventive services, including cancer screening, less often than non-migrants. Whereas also for Germany a lower utilization of preventive services among migrants as compared with non-migrants has been reported, little is known about the utilization of cancer screening. Unlike other studies in Europe, the only available study for Germany showed that women of Turkish origin had a higher chance of utilizing breast cancer screening than women of non-Turkish origin. The role of socioeconomic factors as confounding variables could not be taken into account.[41]
Based on data from a large national sample survey, our study, in contrast, shows that women with a two-sided migration background residing in Germany utilize cancer screening less often than nonmigrant women. The findings cannot be explained by a different distribution of demographic or socioeconomic factors between both population groups or by differences in the self-reported health status. Even after adjusting for these factors, women with a two-sided migration background still had about half the chance of ever having participated in any kind of cancer screening. Our results are in line with European and studies from other countries conducted on the utilization of cancer screening in migrant communities, most of which reported lower rates of utilization of cancer screening in this population groups as compared with the respective majority populations.[20,21,23–30] Our investigation adds to existing research by focusing on the lifetime participation in cancer screening in general thus allowing to identify those who are particularly vulnerable by not using services on cancer screening at all. Our study has further shown that women with a one-sided migration background are very similar to the autochthonous population in terms of their utilization of cancer screening. This corresponds to findings from other studies on the health and health care utilization of migrants in Germany.[45,46]
The lower utilization of cancer screening among women with a two-sided migration background may have several reasons. Migrants experience different barriers in the health care system, potentially reducing their access to health services. These barriers include a poor cultural sensitivity of health services, discrimination, and insufficient community resources.[47–49] Also, barriers and a limited health literacy resulting from poor proficiency of the language of the host country have been identified to limit access to preventive services for migrants, including cancer screening.[11,50] As the GEDA survey that we used for our study is conducted in German language and only respondents with sufficient language skills are included,[42] poor language proficiency, however, cannot explain our results.
A lower uptake of screening for cancer can also reflect differences in illness perceptions. Migrants tend to have less stronger perceptions of the risk and consequences associated with cancer.[11] Kristiansen et al[20] hypothesize that this may be attributable to the lower incidence of cancer in the countries where migrants originate from, resulting in an overall lower awareness toward the disease.
The decision to undergo early detection for cancer is a complex process. Not using such services can also result from an informed decision-making process in which individuals weigh the harms and benefits of screening and decide for or against utilizing such services. In this case, lower rates of utilization would not be indicative of health disparities. However, knowledge about screening for cancer is usually low,[51] particularly among migrants.[52] In Germany, the proportion of women aged ≥50 years who were invited to attend mammography in a specialized center and who made informed choices for or against participation was considerably lower among migrants than among non-migrants.[53]
Age is a known determinant of screening uptake,[20,21] which was also the case in our study. Unlike previous research,[41,54] we did not observe that the effect of age differed for migrants and non-migrants (or, conversely, that the participation rates for migrants and non-migrants differed with age). One reason for age-specific difference between migrants and non-migrants in preventive behavior is that older migrants tend to be particularly prone to poor proficiency of the host country's language. A possible explanation that we did not identify any interaction therefore is that the sample of migrants included in our data was proficient in German.
With respect to the diverging results as compared with the study by Berens et al,[41] it has to be considered that the respective authors used data from five selected cities in Germany. In contrast, our investigation is based on data from a national sample survey. Differences in the rates of utilization between the two studies could therefore also reflect the role of regional variation of participation rates in cancer screening which studies in Germany[55] and other countries[9,56] have observed.
Some limitations of our study must be taken into account. First, we examined the utilization of cancer screening in general and did not distinguish between screenings for different types of cancers. This could also explain differences to other investigations that specifically focus on screening for selected types of cancer. Second, as we were only able to compare rather broad categories of migrants, the diversity of the population in terms of culture, religion, origin, length of stay, and acculturation could not be considered—a limitation which is frequently encountered in studies based on secondary data in Germany. Studies from other countries have shown that these factors may be significantly related to participation in cancer screening and other health services.[49,52,57] Future investigations, therefore, also need to examine their role among migrants in Germany in order to devise appropriate patient-oriented services. Third, households without a landline telephone were not included in the sample. This is a potential source of selection bias. Around 7% of the population are estimated to be users of mobile phones only[58] and therefore cannot be reached by surveys which are based on landline phone sampling. However, as a comparison with official statistics shows, the demographic and socioeconomic distribution of the survey data is very similar to that of the population in Germany.2 Therefore, we do not consider this source of bias to distort our results substantially. In addition, for our investigation focusing solely on women, a potential bias is further minimized by the fact that two thirds of all people who use mobile phones exclusively are reported to be male.[59] Future telephone surveys, nonetheless, need to make use of more sophisticated sampling techniques which also allow reaching individuals who do not have landline telephones.[60] Fourth, our analysis is restricted to migrants with good German-language proficiency, as this was one of the inclusion criteria, which had to be met by respondents in order to be included in the survey. Therefore, the sample of migrants included in the survey cannot be considered representative for all migrants in Germany.[42] This is also reflected in the socioeconomic profile, which in our study is higher for migrants than according to official statistics. Thus, our analyses were based on a migrant population better educated, having a better occupational position, and experiencing less language barriers than the actual population of migrants residing in Germany. All of these factors are strong positive predictors of cancer screening participation, so differences in participation rates in favor of the autochthonous population that were revealed in our study can be expected to be even larger in the actual migrant population of Germany.
5. Conclusion
Migrant women with a two-sided migration background utilize cancer screening less often than nonmigrant women in Germany, independently of demographic and socioeconomic factors. This is in line with findings from other countries. Available evidence suggests that differences in the utilization of cancer screening additionally are caused by barriers that migrants experience in the health care process which potentially prevent them from taking informed choices. Appropriate measures aiming to enhance informed decision making need to be implemented. Migrants not only need to be able to access health information in languages they understand, these information—same as the services as such—in addition must be sensitive toward their needs in order to allow informed decision making.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, AME = average marginal effect, CATI = computer-assisted telephone interviews, GEDA = Gesundheit in Deutschland aktuell, OR = odds ratio, RDD = random-digit dialing, ref. = reference, SD = standard deviation, SES = socioeconomic status.
Funding: The publication costs of this article were funded by the German Research Foundation/DFG and the Technische Universität Chemnitz in the funding program Open Access Publishing.
The authors have no conflicts of interest to disclose.
References
- 1.European Commission: Migrants in Europe—A statistical portrait of the first and second generation. Luxembourg: Publications Office of the European Union; 2011. [Google Scholar]
- 2.Statistisches Bundesamt. Bevölkerung und Erwerbstätigkeit. Bevölkerung mit Migrationshintergrund. Ergebnisse des Mikrozensus 2013 (Fachserie 1 Reihe 2. 2). Wiesbaden: Statistisches Bundesamt; 2014. [Google Scholar]
- 3.Solé-Auró A, Crimmins EM. Health of immigrants in European countries. Int Migr Rev 2008; 42:861–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rechel B, Mladovsky P, Ingleby D, et al. Migration and health in an increasingly diverse Europe. Lancet 2013; 381:1235–1245. [DOI] [PubMed] [Google Scholar]
- 5.Brzoska P, Razum O. Migration and occupational health: high work-related burden. Public Health Forum 2015; 23:113–115. [Google Scholar]
- 6.Norredam M, Nielson SS, Krasnik A. Migrants’ utilization of somatic healthcare services in Europe—a systematic review. Eur J Public Health 2009; 20:555–563. [DOI] [PubMed] [Google Scholar]
- 7.Solé-Auró A, Guillén M, Crimmins EM. Health care usage among immigrants and native-born elderly populations in eleven European countries: results from SHARE. Eur J Health Econ 2012; 13:741–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Norredam M, Krasnik A. Rechel B, Mladovsky P, Deville W, et al. Migrants’ access to health services. Migration and Health in the European Union. Berkshire: Open University Press; 2011. 67–78. [Google Scholar]
- 9.Vermeer B, Van den Muijsenbergh M. The attendance of migrant women at the national breast cancer screening in the Netherlands 1997–2008. Eur J Cancer Prev 2010; 19:195–198. [DOI] [PubMed] [Google Scholar]
- 10.Lagerlund M, Maxwell A, Bastani R, et al. Sociodemographic predictors of non-attendance at invitational mammography screening—a population based register study (Sweden). Cancer Causes Control 2002; 13:73–82. [DOI] [PubMed] [Google Scholar]
- 11.Andreeva VA, Pokhrel P. Breast cancer screening utilization among Eastern European immigrant women worldwide: a systematic literature review and a focus on psychosocial barriers. Psychooncology 2013; 22:2664–2675. [DOI] [PubMed] [Google Scholar]
- 12.Myers ER, Moorman P, Gierisch JM, et al. Benefits and harms of breast cancer screening: a systematic review. JAMA 2015; 314:1615–1634. [DOI] [PubMed] [Google Scholar]
- 13.Moyer VA. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2012; 156:880–891. [DOI] [PubMed] [Google Scholar]
- 14.Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin 2012; 62:147–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 16.World Health Organization. WHO Position Paper on Mammography Screening. Geneva: World Health Organization; 2014. [PubMed] [Google Scholar]
- 17.Segnan N, Patnick J, von Karsa L. European Guidelines for Quality Assurance in Colorectal Cancer Screening and Diagnosis. Luxembourg: Publications Office of the European Union; 2010. [Google Scholar]
- 18.Arbyn M, Anttila A, Jordan J, et al. European Guidelines for Quality Assurance in Cervical Cancer Screening. Luxembourg: Publications Office of the European Union; 2008. [Google Scholar]
- 19.Perry N, Broeders M, de Wolf C, et al. European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis. Luxembourg: Publications Office of the European Union; 2006. [Google Scholar]
- 20.Kristiansen M, Thorsted BL, Krasnik A, et al. Participation in mammography screening among migrants and non-migrants in Denmark. Acta Oncol 2012; 51:28–36. [DOI] [PubMed] [Google Scholar]
- 21.Fontana M, Bischoff A. Uptake of breast cancer screening measures among immigrant and Swiss women in Switzerland. Swiss Med Wkly 2008; 138:752–758. [DOI] [PubMed] [Google Scholar]
- 22.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer 2000; 89:696–705. [DOI] [PubMed] [Google Scholar]
- 23.Xiong H, Murphy M, Mathews M, et al. Cervical cancer screening among Asian Canadian immigrant and nonimmigrant women. Am J Health Beh 2010; 34:131–143. [DOI] [PubMed] [Google Scholar]
- 24.Vahabi M, Lofters A, Kumar M, et al. Breast cancer screening disparities among urban immigrants: a population-based study in Ontario, Canada. BMC Public Health 2015; 15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weber MF, Banks E, Smith DP, et al. Cancer screening among migrants in an Australian cohort; cross-sectional analyses from the 45 and Up Study. BMC Public Health 2009; 9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Damiani G, Federico B, Basso D, et al. Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: a cross sectional study. BMC Public Health 2012; 12:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanson K, Montgomery P, Bakker D, et al. Factors influencing mammography participation in Canada: an integrative review of the literature. Curr Onco 2009; 16:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Labeit A, Peinemann F, Baker R. Utilisation of preventative health check-ups in the UK: findings from individual-level repeated cross-sectional data from 1992 to. BMJ Open 2013; 3:e003387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schoueri-Mychasiw N, McDonald PW. Factors associated with underscreening for cervical cancer among women in Canada. Asian Pac J Cancer Prev 2013; 14:6445–6450. [DOI] [PubMed] [Google Scholar]
- 30.Lagerlund M, Maxwell A, Bastani R, et al. Sociodemographic predictors of non-attendance at invitational mammography screening— a population-based register study (Sweden). Cancer Causes Control 2002; 13:73–82. [DOI] [PubMed] [Google Scholar]
- 31.Scheppers E, van Dongen E, Dekker J, et al. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract 2006; 23:325–348. [DOI] [PubMed] [Google Scholar]
- 32.Priebe S, Sandhu S, Dias S, et al. Good practice in health care for migrants: views and experiences of care professionals in 16 European countries. BMC Public Health 2011; 11:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gil-Gonzalez D, Carrasco-Portino M, Vives-Cases C, et al. Is health a right for all? An umbrella review of the barriers to health care access faced by migrants. Ethn Health 2014; 20:523–541. [DOI] [PubMed] [Google Scholar]
- 34.Gemeinsamer Bundesausschuss. Richtlinie des Gemeinsamen Bundesausschusses über die Früherkennung von Krebserkrankungen [Guidelines of the Federal Joint Committee for the early detection of cancer]. Bundesanzeiger 2014. 1–51.AT 31.12.2014 B4. [Google Scholar]
- 35.Bozorgmehr K, Razum O. Effect of restricting access to health care on health expenditures among asylum-seekers and refugees: a quasi-experimental study in Germany, 1994–2013. PLoS One 2015; 10:e0131483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Norredam M, Mygind A, Krasnik A. Access to health care for asylum seekers in the European Union - a comparative study of country policies. Eur J Public Health 2006; 16:285–289. [DOI] [PubMed] [Google Scholar]
- 37.Keller A, Baune B. Impact of social factors on health status and help seeking behavior among migrants and Germans. J Public Health 2005; 13:22–29. [Google Scholar]
- 38.Zeeb H, Baune BT, Vollmer W, et al. Gesundheitliche Lage und Gesundheitsversorgung von erwachsenen Migranten—ein Survey bei der Schuleingangsuntersuchung. Gesundheitswesen 2004; 66:76–84. [DOI] [PubMed] [Google Scholar]
- 39.Brzoska P, Voigtländer S, Spallek J, et al. Utilization and effectiveness of medical rehabilitation in foreign nationals residing in Germany. Eur J Epidemiol 2010; 25:651–660. [DOI] [PubMed] [Google Scholar]
- 40.Maier C, Razum O, Schott T. Muthny FA, Bermejo I. Migration und rehabilitative Versorgung in Deutschland—Inanspruchnahme von Leistungen der medizinischen Rehabilitation und Rehabilitationserfolg bei Personen mit türkischem Migrationshintergrund. Interkulturelle Medizin. Laientheorien, Psychosomatik und Migrationsfolgen. Köln: Deutscher Ärzte Verlag; 2008. 85–103. [Google Scholar]
- 41.Berens E-M, Stahl L, Yilmaz-Aslan Y, et al. Participation in breast cancer screening among women of Turkish origin in Germany—a register-based study. BMC Women's Health 2014; 14:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Robert Koch-Institut. Gesundheit in Deutschland aktuell 2010. Public USE File GEDA 2010. Dokumentation des Datensatzes. Berlin: Robert Koch-Institut; 2012. [Google Scholar]
- 43.Robert Koch-Institut. Daten und Fakten: Ergebnisse der Studie »Gesundheit in Deutschland aktuell 2010«. Berlin: Robert Koch-Institut; 2012. [Google Scholar]
- 44.Mood C. Logistic regression: why we cannot do what we think we can do, and what we can do about it. Eur Sociol Rev 2010; 26:67–82. [Google Scholar]
- 45.Poethko-Möller C, Krug S. Social and health related risk factors for low cardio respiratory fitness in German adolescents: results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). J Public Health 2014; 22:187–196. [Google Scholar]
- 46.Böhmer MM, Walter D, Krause G, et al. Determinants of tetanus and seasonal influenza vaccine uptake in adults living in Germany. Hum Vaccines 2011; 7:1317–1325. [DOI] [PubMed] [Google Scholar]
- 47.Bermejo I, Hölzel LP, Kriston L, et al. Subjektiv erlebte Barrieren von Personen mit Migrationshintergrund bei der Inanspruchnahme von Gesundheitsmaßnahmen. Bundesgesundheitsblatt–Gesundheitsforschung–Gesundheitsschutz 2012; 55:944–953. [DOI] [PubMed] [Google Scholar]
- 48.Yilmaz-Aslan Y, Brzoska P, Bluhm M, et al. Illness perceptions in Turkish migrants with diabetes: a qualitative study. Chronic Illness 2014; 10:107–121. [DOI] [PubMed] [Google Scholar]
- 49.Scheppers E, Van Dongen E, Dekker J, et al. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract 2006; 23:325–348. [DOI] [PubMed] [Google Scholar]
- 50.Berens EM, Yilmaz-Aslan Y, Spallek J, et al. Determinants of mammography screening participation among Turkish immigrant women in Germany—a qualitative study reflecting key informants’ and women's perspectives. Eur J Cancer Care 2015; 50:38–48. [DOI] [PubMed] [Google Scholar]
- 51.Hoffmann TC, Del Mar C. Patients’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Int Med 2015; 175:274–286. [DOI] [PubMed] [Google Scholar]
- 52.Pons-Vigues M, Puigpinos-Riera R, Serral G, et al. Knowledge, attitude and perceptions of breast cancer screening among native and immigrant women in Barcelona, Spain. Psychooncol 2012; 21:618–629. [DOI] [PubMed] [Google Scholar]
- 53.Berens EM, Reder M, Razum O, et al. Informed choice in the German mammography screening program by education and migrant status: survey among first-time invitees. PLoS One 2015; 10:e0142316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Visser O, Van Peppen AM, Ory FG, et al. Results of breast cancer screening in first generation migrants in Northwest Netherlands. Eur J Cancer Prev 2005; 14:251–255. [DOI] [PubMed] [Google Scholar]
- 55.Vogt V, Siegel M, Sundmacher L. Examining regional variation in the use of cancer screening in Germany. Soc Sci Med 2014; 110:74–80. [DOI] [PubMed] [Google Scholar]
- 56.Stamenic V, Strnad M. Urban–rural differences in a population-based breast cancer screening program in Croatia. Croat Med J 2011; 52:76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pons-Vigues M, Puigpinos-Riera R, Rodriguez D, et al. Country of origin and prevention of breast cancer: beliefs, knowledge and barriers. Health Place 2012; 18:1270–1281. [DOI] [PubMed] [Google Scholar]
- 58.Busse B, Fuchs M. The components of landline telephone survey coverage bias. The relative importance of no-phone and mobile-only populations. Qual Quant 2012; 46:1209–1225. [Google Scholar]
- 59.Graeske J, Kunz T. Häder M, Häder S. Stichprobenqualität der CELLA-Studie unter besonderer Berücksichtigung der Mobile-onlys. Telefonbefragungen über das Mobilfunknetz. Konzept, Design und Umsetzung einer Strategie zur Datenerhebung. Wiesbaden: Springer; 2009. 57–70. [Google Scholar]
- 60.von der Lippe E, Schmich P, Lange C. Advance letters as a way of reducing non-response in a National Health Telephone Survey: Differences between listed and unlisted numbers. Survey Res Methods 2011; 5:103–116. [Google Scholar]


