Supplemental Digital Content is available in the text
Keywords: association, Beijing, blood pressure, generalized estimating equations, platelet indices, quadratic inference functions
Abstract
The quadratic inference function (QIF) method becomes more acceptable for correlated data because of its advantages over generalized estimating equations (GEE). This study aimed to evaluate the relationship between platelet indices and blood pressure using QIF method, which has not been studied extensively in real data settings.
A population-based longitudinal study was conducted in Beijing from 2007 to 2012, and the median of follow-up was 6 years. A total of 6515 cases, who were aged between 20 and 65 years at baseline and underwent routine physical examinations every year from 3 Beijing hospitals were enrolled to explore the association between platelet indices and blood pressure by QIF method. The original continuous platelet indices were categorized into 4 levels (Q1–Q4) using the 3 quartiles of P25, P50, and P75 as a critical value. GEE was performed to make a comparison with QIF.
After adjusting for age, usage of drugs, and other confounding factors, mean platelet volume was negatively associated with diastolic blood pressure (DBP)
in males and positively linked with systolic blood pressure (SBP)
. Platelet distribution width was negatively associated with SBP
. Blood platelet count was associated with DBP
in males.
Adults in Beijing with prolonged exposure to extreme value of platelet indices have elevated risk for future hypertension and evidence suggesting using some platelet indices for early diagnosis of high blood pressure was provided.
1. Introduction
Elevated blood pressure is a leading modifiable risk factor for the premature death and cardiovascular disease (CVD), which leads to at least 1.1 million deaths per year in the globe, and hypertension has been possessing as a major public health challenge by World Health Organization.[1,2] Considering the severity of hypertension, 3 states of blood pressure (normal blood pressure, prehypertension, and hypertension) have been set up according to the individual's blood pressure level.[3,4] It has been wildly acknowledged that if diagnosis is done in an early stage of hypertension with effective methods, it can be prevented from CVD and reduce the burden of morbidity and mortality so far.[5–8]
Indices from the physical examination are early diagnostic biomarkers, wherein platelet indices are the potentially useful markers for the early diagnosis of thromboembolic disease. Platelet indices comprise platelet distribution width (PDW), mean platelet volume (MPV), plateletcrit (PCT), and blood platelet count (PLT). MVP and PDW are the simple platelet indices, which increase during platelet activation. MPV is one of the most commonly primary measurements of the average size of platelets in the blood sample, which is included in blood tests as part of completed blood count.[9] The larger platelets are more aggregate and reactive compared to the smaller size. Several studies have advised that MPV is significantly increased in CVD patients.[10,11] Likewise, PDW is a simple as well as a practical and specific marker of activation of coagulation, which is used to decide the heterogeneity of platelet size. Several studies have reported that platelet activation has a relationship with cardiovascular morbidity and mortality.[12–14] Increased platelet activation and aggregation are involved in the pathogenesis of elevated blood pressure, which is also associated with hypertensive risk factors.[15–18] Many researchers have illustrated that the platelet occupy was an important position in mediating immune response and maintaining the vascular homeostasis, atherosclerosis, and an inflammation.[19–23] Moreover, the use of antiplatelet management therapies in the high blood pressure, the platelets play a pivotal role in the pathogenesis of hypertension.[24–27] Thus, assessments of platelet indices and their bioactivity may be of vital importance for monitoring the occurrence and progression of hypertension. Asgari et al[28] used the quadratic inference functions (QIFs) to determine the factors associated with obesity from the STEPS Survey in Iran. But to our knowledge, using QIF, studies on the correlation between platelet indices and blood pressure are relatively limited, especially in the large-scale population-based longitudinal study.
Therefore, a longitudinal study with 6515 participants who have undergone 6 repeated health check-ups has been established in Beijing to evaluate the relationship between platelet indices and blood pressure using QIF method, which has not been studied extensively in real data settings.
2. Methods
1.1. Study population
A total of 6515 cases of data, aged 20 to 65 years were obtained from the Beijing Tongren Hospital, Beijing Electric Power Hospital, and Beijing Xiaotangshan Hospital for the longitudinal analysis from 2007 to 2012, 6 years of follow-up. Individuals with a previous diagnosis of CVD, cerebral infarction, or gastric cancer, or those who had undergone coronary artery bypass surgery, coronary stenting surgery, or gastrectomy, and those who had hypertension or took any drugs at baseline were excluded. The study was approved by the Ethics Committee of Capital Medical University (approval number: 2015SY33). Written consent was obtained from all participating subjects.
1.2. Data collection and measurements
All individuals in the study who took routine physical examinations underwent anthropometrically and laboratory tests every year. Weight and height were measured without shoes, and body mass index (BMI) was calculated as the weight (kg) divided by squaring the height (m). Blood samples were collected from an antecubital vein into tubes containing EDTA in the morning after an overnight fasting. PLT, PDW, MPV, PCT, fasting plasma glucose (FPG), triglyceride (TG), high-density lipoprotein (HDL), white blood cell (WBC), red blood cell (RBC), hemoglobin (HGB), red blood cell specific volume (HCT), and erythrocyte mean corpuscular volume (MCV) were measured by an auto analyzer (Sysmex SE-9000, Kobe, Japan). The information of drug usage was obtained from individuals’ medical history. Drug information was adjusted in the analysis, including the use of anti-hypertensive drugs, anti-dyslipidemia drugs, anti-diabetic drugs, and anti-platelet drugs. All analyses were performed in accordance with the manufacturer's recommendations.
1.3. Approach for blood pressure measurement
Blood pressure was measured by a trained nurse on the right arm of participants (after at least 5-minute rest) during hospitalization using the WHO classification criteria.[29] During 30-minute proceeding, the measurements of the participants were required to refrain from smoking or consuming caffeine. A standard mercury sphygmomanometer was used to measure the blood pressure of participant with 1 of 4 cuff sizes (pediatric, regular adult, large adult, or thigh) based on the participant's arm circumference. Three readings of each systolic blood pressures (SBPs) and diastolic blood pressures (DBPs) were recorded with an interval of 1 minute at least, and an average of the last 2 measurements was used for the data analysis.
1.4. Statistical analysis
There have been several appropriate statistical methods for analyzing repeated measures, including GEE and multilevel mixed linear model. Whereas, in comparison to the GEE approach, QIF has the following advantages. First, the application of GEE requires more model assumptions than QIF method.[30,31] Second, QIF method constructs more estimating functions than the number of parameters, so extra degrees of freedom are available to perform the goodness-of-fit test.[30–32] Therefore, some model selection criteria such as Akaike information criterion (AIC) and Bayesian information criterion (BIC) can be established in QIF. The AIC and BIC are measures of the relative quality of statistical models for a given set of data. Hence, AIC and BIC provide a means for model selection. When fitting models, it is possible to increase the likelihood by adding parameters, but doing so may result in overfitting. Both AIC and BIC resolve this problem by introducing a penalty term for the number of parameters in the model. The model with the lowest AIC and BIC is preferred. GEE methods are unavailable to perform such types of procedures. Moreover, because of the fact that QIF does not need to estimate the parameters in a given correlation structure, especially when the working correlation is misspecified, the QIF estimator of beta is more efficient than the GEE estimator.[30,33,34] Finally, GEE is not robust and very sensitive to influential data cases, whereas the QIF estimators are robust with a bounded influence function against unduly large outliers or contaminated data points.[30,35,36]
The original continuous platelet indices were categorized into 4 levels (Q1, Q2, Q3, and Q4) using the 3 quartiles of P25, P50, and P75 as a critical values, with ≤P25 for Q1, >P25 and P50 for Q2, >P50 and ≤P75 for Q3, and >P75 for Q4, respectively. To better clarify the relationship between elevated blood pressure and platelet indices, some confounding factors were adjusted in QIF model. Three QIF models have been estimated to check whether the correlation existed or not. In model 2, FPG, TG, HDL, and BMI were adjusted in QIF model. In model 3, FPG, TG, HDL, BMI WBC, RBC, HGB, HCT, MCV, and the use of anti-hypertensive drugs, anti-dyslipidemia drugs, anti-diabetic drugs, and anti-platelet drugs were adjusted in QIF model.
Summary of the statistics was used to illustrate the characteristics of variables’ distribution in each repeated survey. Student t test was used for continuous variables to detect the statistical significances and compared with the first survey (baseline). The results were presented as an estimate indices
 |
and standard errors. Parameters of GOF test, including AIC, BIC, and value of χ2 of QIF were calculated for model assessment.
To account for missing values, multiple imputation (MI) was performed. Markov Chain Monte Carlo (MCMC) method was chosen for missing values of multiple imputed variables without loss of generality. This method was employed in SAS (Version 9.2; SAS Institute Inc., Cary, NC) followed with the procedure of MI. After imputation, all variables had <10% missing observations, in particular, <2% of the platelet indices and blood pressure variables. All the analyses were completed in the SAS 9.2 statistical software, wherein statistical significance was set at the 0.05 level and all P values were 2-sided.
2. Results
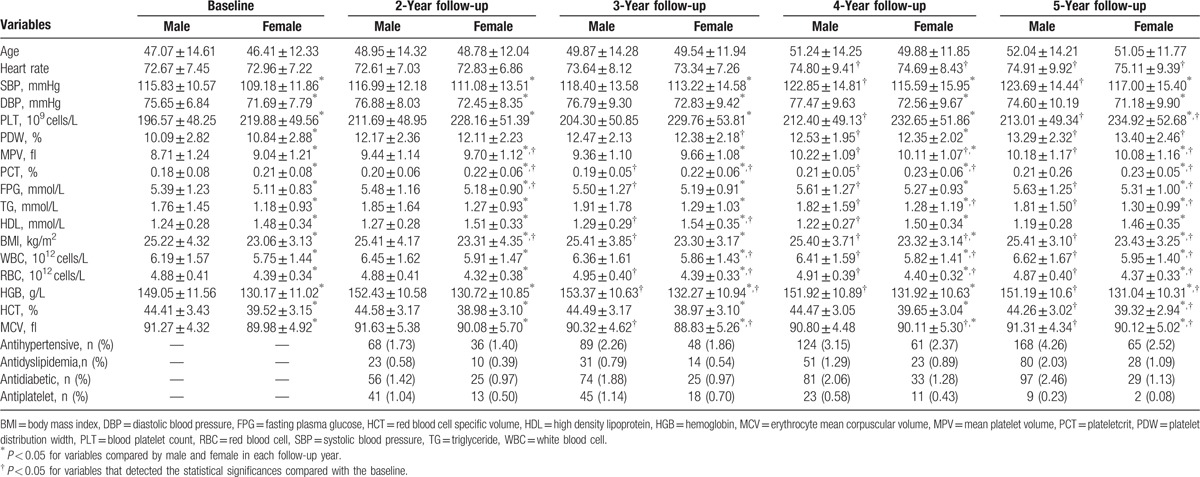
Table 1 shows the characteristics of SBP and DBP together with the potential confounding factors at baseline with each follow-up year. Although tests of some factors did not reach statistical significance, it indicated that they were higher than baseline generally and blood pressure increased in a steady trend. QIF analysis was performed to explore the sex distributions in every follow-up year separately. Table S1 and S2 summarize the distributions of blood pressure of male and female in detail.
Table 1.
Distribution of blood pressure and other potential confounding factors.
According to the GOF test, the smaller AIC, BIC, and larger χ2 values indicated the better fit of the QIF model. Table 2 shows that the most suitable correlation working matrix was an exchangeable model for both sexes in term of DBP. As for SBP, the most suitable related working matrix for female is the unstructured model and exchangeable model for male population.
Table 2.
GOF test information among 3 models in selecting the most suitable working correlation matrix.
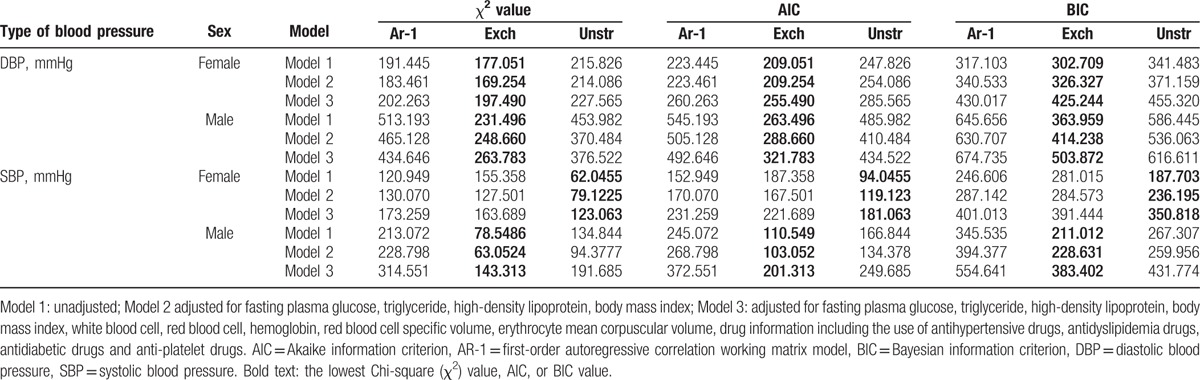
In the present study, table S3–S8 show an explicit comparison of parameter estimation for GEE and QIF by fitting Model 1 to 3. According to the lowest AIC and BIC, QIF can choose the best model with appropriate working correlation matrix, whereas AIC and BIC are not available in GEE model. QIF produced smaller standard errors compared with GEE in most situations even with the same working correlation matrix, which implies that parameters of QIF model are more reliable and efficient than that of GEE.
Figures 1 and 2 show that after adjusting the potential confounders by QIF method, PDW was negatively associated with SBP. Setting Q1 as the reference, for male,
 |
95% confidence interval [CI] = −1.2096 to −0.2768; P = 0.00179) and
were significant. Whereas for female, levels of
and
were significant. We could hardly find associations between PDW and DBP, except for male
.
Figure 1.
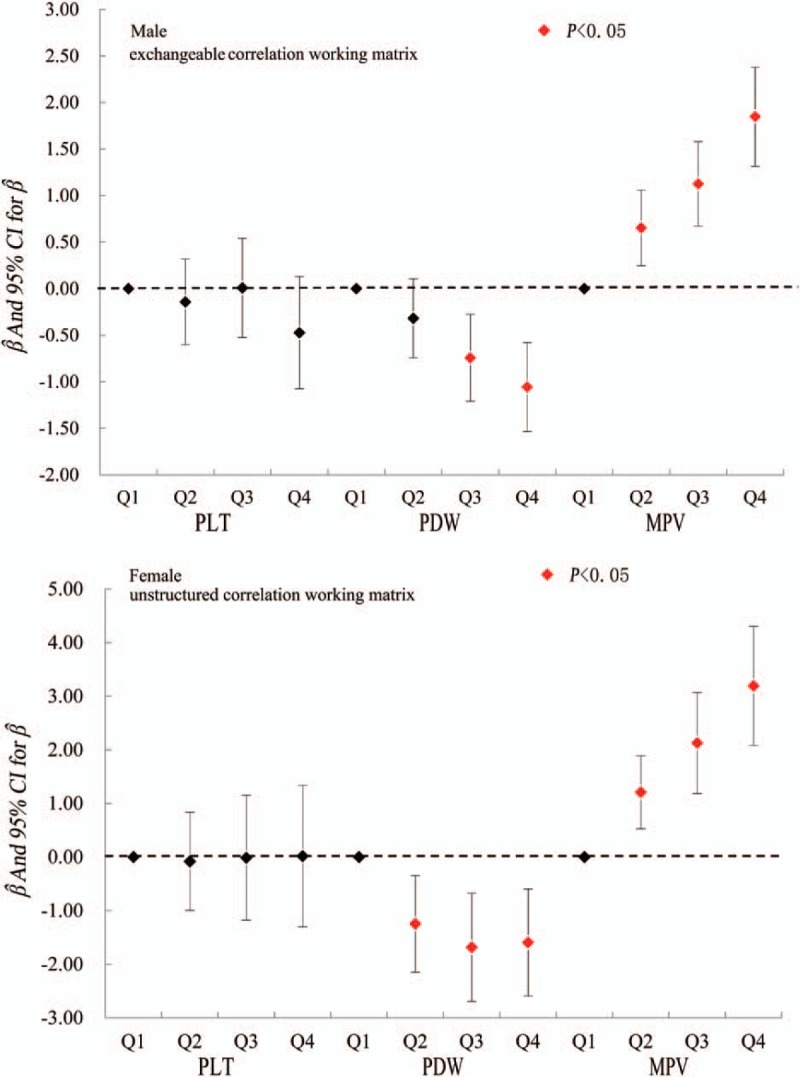
Risk factors associated with evaluated SBP. MPV = mean platelet volume, PDW = platelet distribution width, PLT = blood platelet count, SBP = systolic blood pressure.
Figure 2.
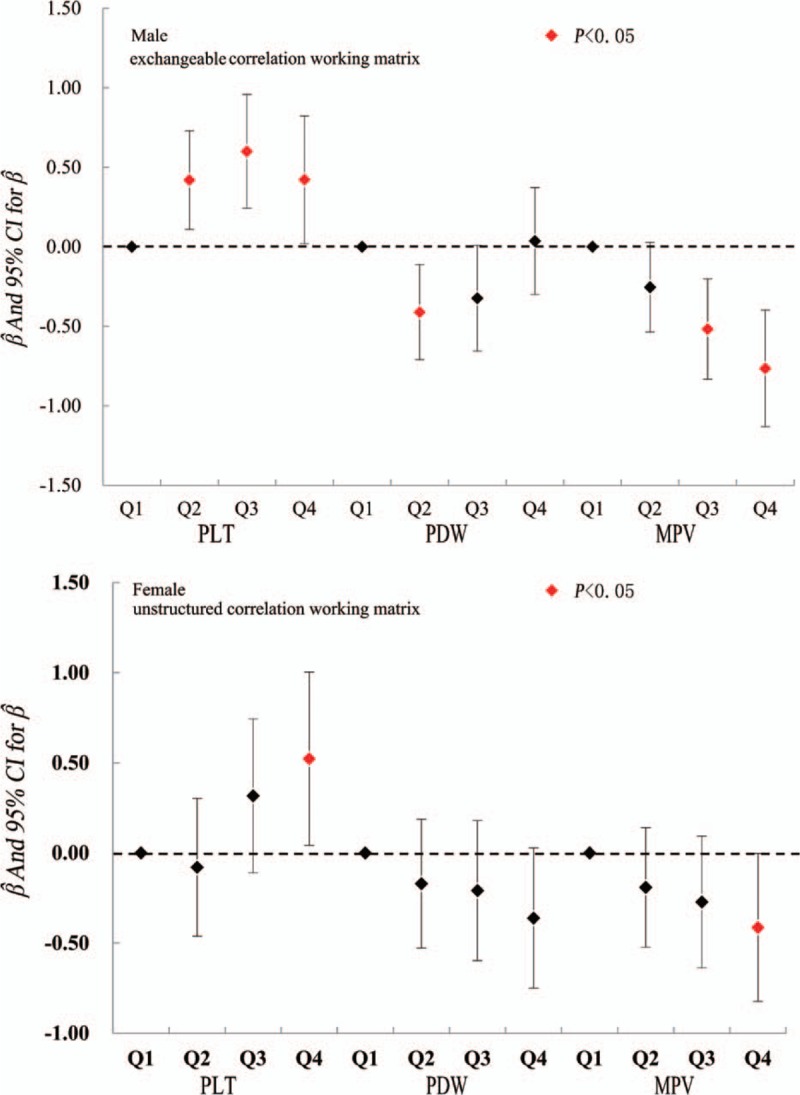
Risk factors associated with evaluated DBP. DBP = diastolic blood pressure, MPV = mean platelet volume, PDW = platelet distribution width, PLT = blood platelet count.
MPV had a positive association with SBP. Setting Q1 as the reference, for male,
and
were significant, and for female,
and
were significant, However, a negative connection was observed between MPV and DBP for male,
and
 |
were scientific significant, and for female
.
PLT showed a positive relationship with DBP. Setting Q1 as the reference, for male,
and
were scientific significant and for female
There has been no relationship between PCT and blood pressure as our result displayed.
3. Discussion
Concern about the increased prevalence of elevated blood pressure has lightened the interests to explore an association between some convenient, fast, and effective indices with blood pressure among healthy populations in Beijing, and we found PDW MPV and PLT are those indices that can help diagnose evaluated blood pressure and then hypertension. Some desirable features of the QIF method in a real world with longitudinal data have been illustrated. The GOF statistic from QIF model also facilitates an optimal selection of the correlation structure among several plausible choices. We obtained similar parameter estimations from GEE and QIF analyses using the dataset of health check-up in 3 hospitals in Beijing from 2007 to 2012. In terms of SBP, the most suitable working correlation matrix for male was exchangeable model. Additionally, exchangeable model was the suitable matrices for male and unstructured model for female. Our findings are consistent with the findings of Qu et al,[31] which stated that QIFs have the greater efficiency of parameter estimates in comparison to GEE, and made more reliable results in conjunction with GEE.
PDW and MPV are 2 indicators of platelet, which reflect the size and variability, respectively.[37,38] According to Zheng et al,[18] the larger platelets are more active compared to smaller ones both metabolically and enzymatically, which is more likely to be thrombotic potential. Earlier findings have established that raised PDW and MPV levels are an independent risk factor for myocardial infarction including coronary heart diseases.[39–41] Increased platelet size is a risk factor for cardiovascular as well as diabetes and atherosclerosis disease, which have also been reported by some researchers, while increased MPV levels have shown in several inflammatory syndromes, such as, periodontitis, osteoarthritis and systemic sclerosis.[42,43]
Pathophysiology of elevated blood pressure is multifaceted including vasoconstriction, vascular wall remodeling, and in situ thrombosis.[18,44] Earlier researches stated that an elevated platelet aggregation and activation rose along with the process of hypertension.[18,45,46] Our study experienced that the MPV was significantly associated with higher estimator in SBP, regardless of sex, whereas a negative correlation was observed between MPV and DBP. These findings are consistent with previous studies of Ucar et al [47] and Pusuroglu et al.[48] Additionally, there are 2 possible mechanisms that may contribute to increased platelet parameter levels during high blood pressure as suggested by some studies,[47,48] such as firstly, pulmonary vascular endothelial dysfunction was linked with the path mechanisms of hypertension, which might lead to the platelet activation and local thrombosis. And secondly, systemic inflammation and immune dysfunction in patients with high blood pressure might cause platelet activation.[18]
Our study established that PLT had a positive relationship with DBP for both sexes, whereas there was no relationship found between PCT and blood pressure. Previous studies have shown that there was a sex effect on the relationship of blood pressure and platelet indices.[18,49–51] Those studies suggested that only partial indicators of platelet indices reflect the disease severity. From our findings, we can suggest that an elevated MPV and PDW might be an indication to recognize the part of platelet activation in the interpretation of the cause of hypertension. There could be possible 2 things, activated platelets might conglutinate the wall of injured pulmonary vessels and facilitate the growth of in situ thrombosis, and they may possibly secrete several growth factors and cytokines that influence during remodeling of the pulmonary vessel.[18]
There are some limitations which should be acknowledged in our study. First, we enrolled participants from 3 hospitals only for this study, so the results of this study may be a boundary for the generalization to the other population. Secondly, in the presence of young platelets, specific platelet activation was not measured by measuring reticulated platelets or immature platelet fraction. In addition, the information about lifestyles of a person was not included in the present study, and the multivariate model was not adjusted for these factors. Therefore, further study will be advised including the lifestyle variables along with the general population.
4. Conclusion
Our study confirmed that QIF was better compared to GEE. MPV was negatively associated with DBP in male, where PDW was a negative association with SBP. PLT was associated with male's DBP. Our findings lay the basis of QIF method running into a real world longitudinal study and provided further evidence using some platelet indices for early diagnosis of hypertension.
Acknowledgments
The authors thank all the investigators, the staff of those 3 hospitals, and the participants of the present study for their valuable contributions.
Supplementary Material
Footnotes
Abbreviations: AR-1 = first-order autoregressive correlation working matrix model, BMI = body mass index, DBP = diastolic blood pressure, Exch = exchangeable correlation working matrix model, FPG = fasting plasma glucose, GEE = generalized estimating equations, HCT = red blood cell specific volume, HDL = high-density lipoprotein. WBC = white blood cell, HGB = hemoglobin, MCV = erythrocyte mean corpuscular volume, MPV = mean platelet volume, PCT = plateletcrit, PDW = platelet distribution width, PLT = blood platelet count, QIF = quadratic inference function, RBC = red blood cell, SBP = systolic blood pressure, TG = triglyceride, Unstr = unstructured correlation working matrix model.
KY and LXT contributed to the analysis and interpretation of the data, drafting of the article, critical revision of the article, and statistical analysis. LXT performed the initial analyses, KY prepared the first draft of the article. XHG and GM provided an advice and edited the first draft. XG and ZP had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors gave their final approval for publication.
All funding sources were independent and had no influence on the study design; the collection, analyses, and interpretation of our data; the writing of this report; or the decision to submit the article for publication.
KY and LT contributed equally to the work.
The study is funded by the National Natural Science Foundation of China (Serial Number: 81530087, 81502886, 81373099), Young core personal project & Beijing outstanding talent training project (Serial Number: 2014000020124G150), Key Projects in the National Science & Technology Pillar Program in the Twelfth Five-year Plan Period of China (Serial Number: 2014ZX10004005-001).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- 1.World Health Organization. “A global brief on hypertension: silent killer, global public health crisis”. World 2015. [Google Scholar]
- 2.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 4.Rahman MM, Gilmour S. Prevention and control of hypertension in different countries. Jama 2014; 311:418–419. [DOI] [PubMed] [Google Scholar]
- 5.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 6.Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117:e510–e526. [DOI] [PubMed] [Google Scholar]
- 7.Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens 2015; 28:355–361. [DOI] [PubMed] [Google Scholar]
- 8.Gupta AK, Nasothimiou EG, Chang CL, et al. Baseline predictors of resistant hypertension in the Anglo-Scandinavian Cardiac Outcome Trial (ASCOT): a risk score to identify those at high-risk. J Hypertens 2011; 29:2004–2013. [DOI] [PubMed] [Google Scholar]
- 9.Arevalo-Lorido JC, Carretero-Gomez J, Alvarez-Oliva A, et al. Mean platelet volume in acute phase of ischemic stroke, as predictor of mortality and functional outcome after 1 year. J Stroke Cerebrovasc Dis 2013; 22:297–303. [DOI] [PubMed] [Google Scholar]
- 10.Kaya MG, Elcik D, Akpek M, et al. Mean platelet volume levels predict pulmonary artery hypertension in patients with atrial septal defect. Acta Cardiol 2014; 69:161–166. [DOI] [PubMed] [Google Scholar]
- 11.Lippi G, Franchini M. Platelets and immunity: the interplay of mean platelet volume in health and disease. Exp Rev Hematol 2015; 8:555–557. [DOI] [PubMed] [Google Scholar]
- 12.Vagdatli E, Gounari E, Lazaridou E, et al. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. Hippokratia 2010; 14:28–32. [PMC free article] [PubMed] [Google Scholar]
- 13.Demirtunc R, Duman D, Basar M, et al. The relationship between glycemic control and platelet activity in type 2 diabetes mellitus. J Diabetes Complications 2009; 23:89–94. [DOI] [PubMed] [Google Scholar]
- 14.Goto S, Hasebe T, Takagi S. Platelets: small in size but essential in the regulation of vascular homeostasis - translation from basic science to clinical medicine. Circ J 2015; 79:1871–1881. [DOI] [PubMed] [Google Scholar]
- 15.Arevalo-Lorido JC. Mean platelet volume: When the size does matter. Anatol J Cardiol 2015; 15:853–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang KJ, Lu QY, Li P, et al. [Significance of platelet parameters and lactate dehydrogenase level in differential diagnosis for thrombocytosis]. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2010; 18:972–975. [PubMed] [Google Scholar]
- 17.Carlioglu A, Durmaz SA, Kibar YI, et al. Mean platelet volume in a patient with male hypogonadotropic hypogonadism: the relationship between low testosterone, metabolic syndrome, impaired fasting glucose and cardiovascular risk. Blood Coagul Fibrinolysis 2015; 26:811–815. [DOI] [PubMed] [Google Scholar]
- 18.Zheng YG, Yang T, Xiong CM, et al. Platelet distribution width and mean platelet volume in idiopathic pulmonary arterial hypertension. Heart Lung Circ 2015; 24:566–572. [DOI] [PubMed] [Google Scholar]
- 19.Rodrigues SF, Almeida-Paula LD, Granger DN. Synergistic effects of high blood cholesterol and hypertension on leukocyte and platelet recruitment in the cerebral microcirculation. Hypertension 2014; 63:747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Opie LH. Hypertension, platelets, and inflammatory responses. Cardiovasc Drug Ther 2014; 28:291–292. [DOI] [PubMed] [Google Scholar]
- 21.Guven A, Caliskan M, Ciftci O, et al. Increased platelet activation and inflammatory response in patients with masked hypertension. Blood Coagul Fibrinolysis 2013; 24:170–174. [DOI] [PubMed] [Google Scholar]
- 22.Inanc T, Kaya MG, Yarlioglues M, et al. The mean platelet volume in patients with non-dipper hypertension compared to dippers and normotensives. Blood Press 2010; 19:81–85. [DOI] [PubMed] [Google Scholar]
- 23.Yaoita N, Shirakawa R, Fukumoto Y, et al. Platelets are highly activated in patients of chronic thromboembolic pulmonary hypertension. Arterioscler Thromb Vasc Biol 2014; 34:2486–2494. [DOI] [PubMed] [Google Scholar]
- 24.Surgit O, Pusuroglu H, Erturk M, et al. Assessment of mean platelet volume in patients with resistant hypertension, controlled hypertension and normotensives. Eurasian J Med 2015; 47:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giovanetti TV, do Nascimento AJ, de Paula JP. Platelet indices: laboratory and clinical applications. Rev Bras Hematol Hemoter 2011; 33:164–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Santimone I, Di Castelnuovo A, De Curtis A, et al. White blood cell count, sex and age are major determinants of heterogeneity of platelet indices in an adult general population: results from the MOLI-SANI project. Haematologica 2011; 96:1180–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Gaetano G, Santimone I, Gianfagna F, et al. Variability of platelet indices and function: acquired and genetic factors. Handb Exp Pharmacol 2012; 395–434. [DOI] [PubMed] [Google Scholar]
- 28.Asgari F, Biglarian A, Seifi B, et al. Using quadratic inference functions to determine the factors associated with obesity: findings from the STEPS Survey in Iran. Ann Epidemiol 2013; 23:534–538. [DOI] [PubMed] [Google Scholar]
- 29.Whitworth JA, Chalmers J. World health organisation-international society of hypertension (WHO/ISH) hypertension guidelines. Clin Exp Hypertens 2004; 26:747–752. [DOI] [PubMed] [Google Scholar]
- 30.Qu A, Lindsay BG, Li B. Improving generalised estimating equations using quadratic inference functions. Biometrika 2000; 87:823–836. [Google Scholar]
- 31.Qu A, Song PXK. Assessing robustness of generalised estimating equations and quadratic inference functions. Biometrika 2004; 91:447–459. [Google Scholar]
- 32.Westgate PM, Braun TM. The effect of cluster size imbalance and covariates on the estimation performance of quadratic inference functions. Stat Med 2012; 31:2209–2222. [DOI] [PubMed] [Google Scholar]
- 33.Tian R, Xue L, Liu C. Penalized quadratic inference functions for semiparametric varying coefficient partially linear models with longitudinal data. Journal of Multivariate Analysis 2014; 132:94–110. [Google Scholar]
- 34.Dashnyam O, Cho GY. Quadratic inference functions in marginal models for longitudinal data with time-varying stochastic covariates. Journal of the Korean Data and Information Science Sociaty 2013; 24:651–658. [Google Scholar]
- 35.Lai P, Li G, Lian H. Quadratic inference functions for partially linear single-index models with longitudinal data. Journal of Multivariate Analysis 2013; 118:115–127. [Google Scholar]
- 36.Leng C, Zhang W. Smoothing combined estimating equations in quantile regression for longitudinal data. Stat Comput 2014; 24:123–136. [Google Scholar]
- 37.Akpinar I, Sayin MR, Gursoy YC, et al. Plateletcrit. A platelet marker associated with saphenous vein graft disease. Herz 2014; 39:142–148. [DOI] [PubMed] [Google Scholar]
- 38.Nadaud S, Poirier O, Girerd B, et al. Small platelet microparticle levels are increased in pulmonary arterial hypertension. Eur J Clin Invest 2013; 43:64–71. [DOI] [PubMed] [Google Scholar]
- 39.Beyan C, Beyan E. Is mean platelet volume actually significantly higher in patients with nonalcoholic fatty liver disease? J Clin Gastroenterol 2015; 49:888. [DOI] [PubMed] [Google Scholar]
- 40.Elbasan Z, Gur M, Sahin DY, et al. Mean platelet volume and abnormal left ventricle geometric patterns in patients with untreated essential hypertension. Platelets 2013; 24:521–527. [DOI] [PubMed] [Google Scholar]
- 41.YukselKalkan G, Gur M, Baykan AO, et al. Mean platelet volume is associated with aortic intima-media thickness in patients without clinical manifestation of atherosclerotic cardiovascular disease. Anatol J Cardiol 2015; 15:753–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gasparyan AY, Stavropoulos-Kalinoglou A, Toms TE, et al. Association of mean platelet volume with hypertension in rheumatoid arthritis. Inflamm Allergy Drug Targets 2010; 9:45–50. [DOI] [PubMed] [Google Scholar]
- 43.Hoffmann JJ, Nabbe KC, van den Broek NM. Effect of age on mean platelet volume: Does it exist? Exp Gerontol 2015; 69:41–42. [DOI] [PubMed] [Google Scholar]
- 44.Taguchi H, Kataoka M, Yanagisawa R, et al. Platelet level as a new prognostic factor for idiopathic pulmonary arterial hypertension in the era of combination therapy. Circ J 2012; 76:1494–1500. [DOI] [PubMed] [Google Scholar]
- 45.Zheng Y, Hong H, Reeves HM, et al. Absolute immature platelet count helps differentiate thrombotic thrombocytopenic purpura from hypertension-induced thrombotic microangiopathy. Transfus Apher Sci 2014; 51:54–57. [DOI] [PubMed] [Google Scholar]
- 46.Kim ES, Mo EY, Moon SD, et al. Mean platelet volume is closely associated with serum glucose level but not with arterial stiffness and carotid atherosclerosis in patients with type 2 diabetes. J Clin Endocrinol Metab 2015; 100:3502–3508. [DOI] [PubMed] [Google Scholar]
- 47.Ucar H, Gur M, Gozukara MY, et al. Relationship between mean platelet volume and morning blood pressure surge in newly diagnosed hypertensive patients. Anatol J Cardiol 2015; 15:107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pusuroglu H, Cakmak HA, Erturk M, et al. Assessment of the relation between mean platelet volume, non-dipping blood pressure pattern, and left ventricular mass index in sustained hypertension. Med Sci Monit 2014; 20:2020–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ates I, Bulut M, Ozkayar N, et al. Association between High Platelet Indices and Proteinuria in Patients with Hypertension. Ann Lab Med 2015; 35:630–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boeke CE, Pauly ME, Stock HH, et al. The association of gender, age, body mass index, and vital signs in healthy plateletapheresis donors. Transfus Apher Sci 2009; 41:175–178. [DOI] [PubMed] [Google Scholar]
- 51.Shimodaira M, Niwa T, Nakajima K, et al. Gender differences in the relationship between serum uric acid and mean platelet volume in a Japanese general population. Platelets 2014; 25:202–206. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


