Abstract
Several studies have shown the safety and feasibility of laparoscopic common bile duct exploration (LCBDE) as a minimally invasive treatment options for choledocholithiasis. Use of T-tube or biliary stent drainage tube placement after laparoscopic choledochotomy for common bile duct (CBD) stones is still under debate. This study tried to confirm the safety of spontaneously removable biliary stent in the distal CBD after LCBDE to allow choledochus primary closure. A total of 47 patients with choledocholithiasis underwent LCBDE with primary closure and internal drainage using a spontaneously removable biliary stent drainage tube (stent group, N = 22) or T-tube (T-tube group, N = 25). Operative parameters and outcomes are compared. Surgical time, intraoperative blood loss, length of hospital stay, drainage tube removal time, postoperative intestinal function recovery, and cost of treatment were all significantly lower in the stent group as compared to that in the T-tube group (P < 0.05 for all). Otherwise, Bile leakage between the two groups had no significant difference (P > 0.05). The biliary stent drainage tube was excreted spontaneously 4 to 14 days after surgery with the exception of one case, where endoscopic removal of biliary tube was required due to failure of its spontaneous discharge. LCBDE with primary closure and use of spontaneously removable biliary stent drainage showed advantage over the use of traditional T-tube drainage in patients with choledocholithiasis.
Keywords: choledocholithiasis, laparoscopes, stent drainage, T-tube drainage
1. Introduction
Laparoscopic bile duct exploration has been shown to be a safe and feasible method for treatment of extra-hepatic bile duct stones.[1,2] Traditionally, postoperative T-tube drainage after common bile duct exploration is a standard practice to avoid bile leakage from site of choledochotomy. In laparoscopic common bile duct exploration (LCBDE), the available drainage options include T-tube placement, common bile duct (CBD) primary closure or primary closure plus placement of biliary stent. A consensus on the best option is yet to be reached. Long-term retention of T-tube is associated with risk of track infection and bile leakage besides being an uncomfortable accessory for the patient.[3–5] Primary closure is associated with risk of stenosis and recurrent cholangitis.[6] For this reason, a biliary stent that is amenable to spontaneous removal in a reasonable time, without the need for any further intervention, is an attractive option, which may avoid the aforementioned complications. For this reason we evaluated the use of spontaneously removed biliary stent after LCBDE.
2. Materials and methods
2.1. Clinical information and materials
This study was conducted from September 2014 to September 2015 in the Second Affiliated Hospital of Dalian Medical University. The study protocol was approved by the Institutional Ethics Committee; written informed consent was obtained from all patients before their enrolment. A total of 47 patients with choledocholithiasis were randomly assigned to 1 of 2 groups (stent drainage group and T-tube drainage group). All 47 patients underwent preoperative abdominal magnetic resonance cholangiopancreatography, computed tomography, or ultrasound to confirm cholelithiasis and choledocholithiasis. Both groups underwent LCBDE. To minimize bias, all surgeries were performed by the same surgeon. Biliary stent drainage was achieved with a 15 to 20 cm segment of paracentesis drainage tube (Leadgem Medical Co., serial number FY0825) (Fig. 1). It contains a curved tip and a series of holes on the sidewalls to allow drainage. The size of stent used ranged between 8.5 and 10 French depending on the CBD diameter.
Figure 1.
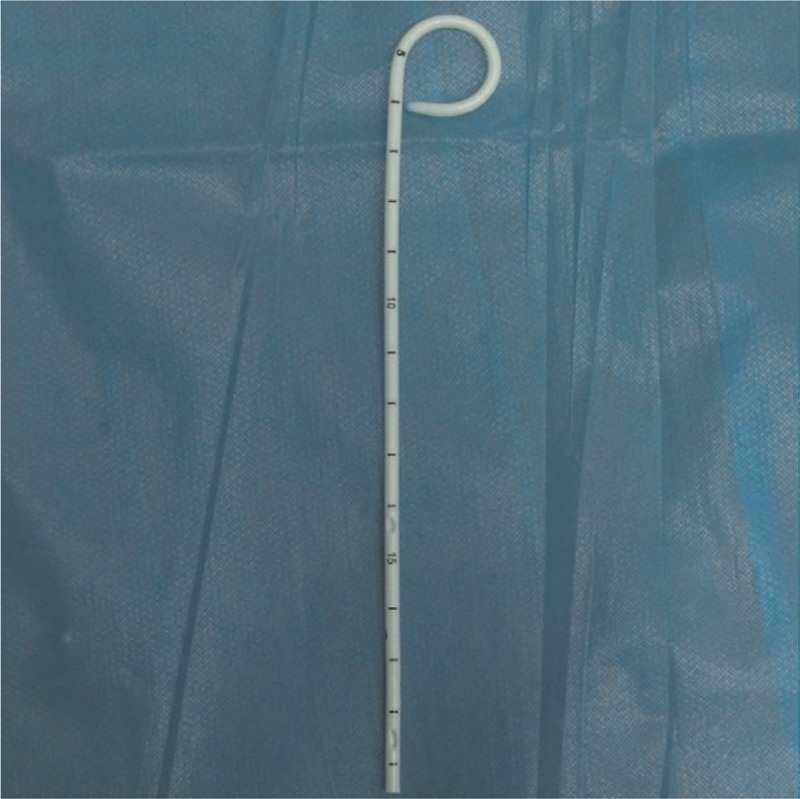
Schematic view of biliary stent drainage tube.
2.2. Surgical procedure
Surgery was performed in the standard way under general anesthesia. Four trocars of 12 mm (umbilical and subxiphoid ones) and 5 mm (subcostal and in right flank) were used. The cystic artery and the cystic duct were dissected and ligated using absorbable clips. Then, the artery was divided with scissors or electrocautery, but the cystic duct was left intact to aid in retraction (Fig. 2A). CBD was dissected along its anterior surface for about 2.5 cm and choledochotomy performed with a longitudinal incision (8–10 mm) with electrocautery (Fig. 2B). Exploration of biliary tree including hepatic ducts, common hepatic duct, and CBD was performed with a choledochoscope (Olympus, Tokyo, Japan) (Fig. 2C). CBD stones were removed using a Dormia basket, (Cook Medical Co., Bloomington, IN). After removal of stones, choledochoscope was used twice to confirm the absence of stones from ampulla of Vater up to hepatic ducts. Before choledochus closure, a T-tube or biliary stent drainage tube was placed. In the stent drainage group, a guide was inserted into CBD through choledochoscope and advanced across the papilla into duodenum, after that the stent was advanced into the duodenum and the guide removed (Fig. 2D and E). Choledochoscope was used to confirm the correct positioning of the stent; choledochotomy was closed with 4–0 absorbable suture (Fig. 2F and G).
Figure 2.
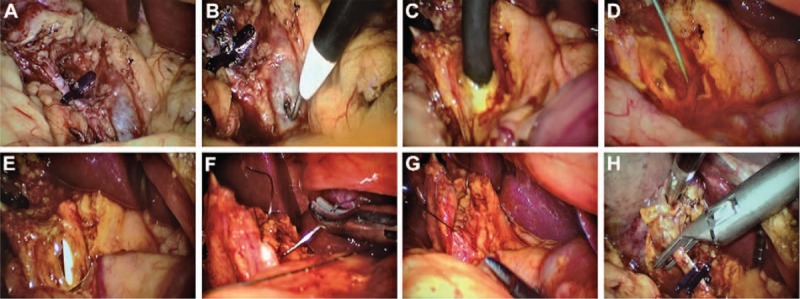
(A) The cystic artery and cystic duct were dissected and ligated using absorbable clips, but for retraction purposes; the cystic duct was not divided. (B) The anterior surface of the CBD was carefully dissected for about 2.5 cm, and the CBD was performed with a longitudinal incision (8–10 mm) made with electrocautery. (C) Choledochoscope was inserted in the CBD and the left and right hepatic ducts and the distal common bile duct explored. (D) The guidewire was placed into the CBD through the choledochoscope and advanced across the papilla into the duodenum. (E) Then the guidewire was removed out until the distal end of the spontaneously removable biliary stent drainage tube entered the duodenum and the proximal end remained in the CBD. (F) The longitudinal choledochotomy was closed with 4–0 absorbable suture. (G) Bile duct suture was completed. (H) The cystic duct was divided. CBD = common bile duct.
In the T-tube drainage group, the T-tube was placed in the CBD. Then the cystic duct was divided in both cases and cholecystectomy completed with ultrasonic harmonic scalpel (Fig. 2H). A subhepatic drainage tube was placed for all patients, which was removed after 2 to 4 days, if the drainage was less than 10 mL/d. The T-tube was removed between days 14 and 21 postoperatively after confirming no remnant stones or stricture of CBD with T-tube cholangiogram. The biliary stent drainage tube gets expelled by defecation without any special intervention.
2.3. Clinical parameters
The following variables were compared between the 2 groups: preoperative general information: gender, age, diameter of CBD, and clinical symptoms; perioperative parameters: surgical time, intraoperative blood loss, postoperative bowel function recovery time, abdominal drainage time, length of hospital stay, total cost, and postoperative complications (bile leak).
2.4. Statistical analysis
All statistical analyses were performed using SPSS 17.0 software (SPSS, Inc., Chicago, IL). Data on normally distributed variables are presented as frequencies; between-group differences were assessed using chi-square test. Data on continuous variables are presented as mean ± standard deviation, and compared using Student t test. If not, we were measured by median and range and compared with Mann–Whitney test. P value <0.05 was considered statistically significant.
3. Results
Of a total of 47 patients, 22 patients were in the stent drainage group and 25 patients in the T-tube drainage group. There was no perioperative mortality. No significant between-group differences were observed with respect to gender, age, CBD diameter (Table 1); clinical characteristics (fever, jaundice, hypertension, coexisting diabetes, and history of pancreatitis) (Table 2). The median operation time was 100 minutes (50–125 minutes) in the stent drainage group and 120 minutes (80–260 minutes) in the T-tube drainage group; the between-group difference was statistically significant (P < 0.05) (Table 3).
Table 1.
Baseline characteristics of patients by study group.
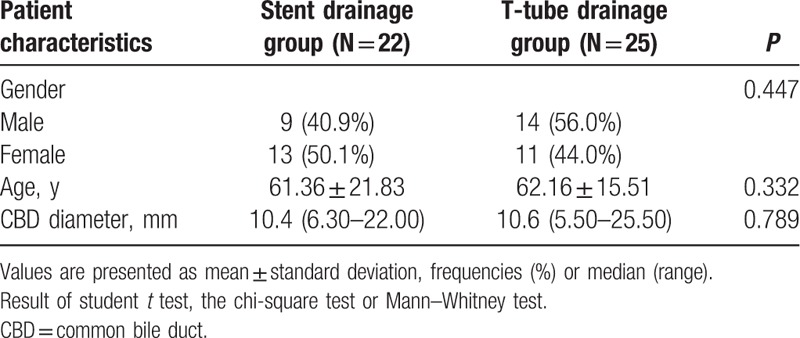
Table 2.
Preoperative clinical characteristics by study group.
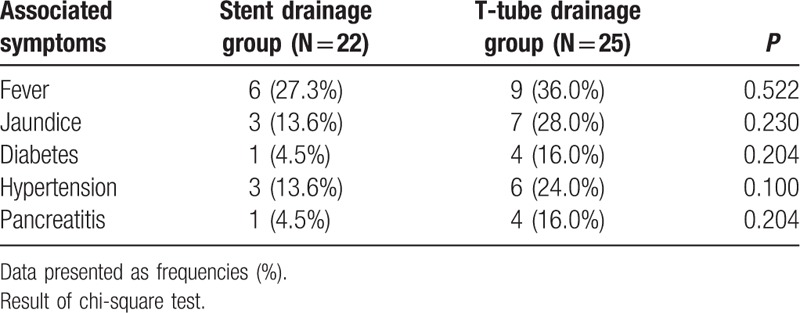
Table 3.
Intraoperative findings and postoperative outcomes by study group.
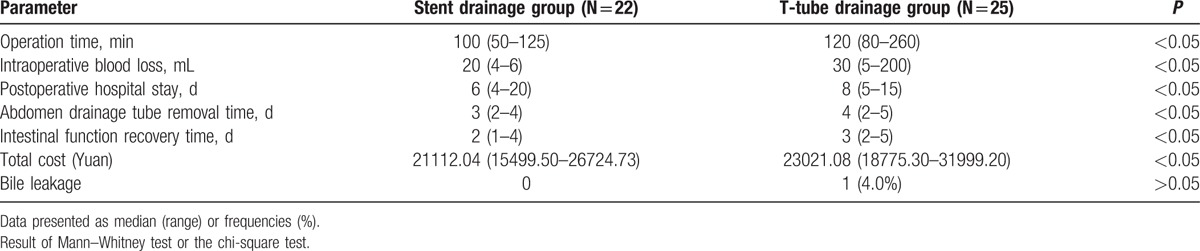
Intraoperative blood loss was significantly lower in the stent drainage group as compared to that in the T-tube drainage group (P < 0.05). Further, postoperative hospital stay, subhepatic drainage extraction times (3 [2–4] days vs 4 [2–5] days), postoperative bowel function recovery time, and total cost of treatment was significantly lower in the stent drainage group as compared to that in the T-tube drainage group (P < 0.05 for all).
There was no significant difference in postoperative bile leakage between the 2 groups. The average excretion time for the biliary stent drainage tube was 6.6 days (range: 4–14). In one patient, the biliary stent drainage tube was taken out by duodenoscope after 1 month, due to failure of spontaneous excretion. None of the patients in the biliary stent drainage group developed postoperative pancreatitis, abdominal pain, intestinal obstruction, cholangitis, or drainage tube blockage. A patient with bile leakage in the T-tube drainage group recovered after simple drainage without needing reoperation.
4. Discussion
Our study proved that the use of spontaneously removable biliary stent drainage is relatively simple, is associated with shorter operation time and lower intraoperative blood loss. The spontaneous excretion of biliary stent decreased the time required for postoperative recovery of bowel function and hospital stay, as previous reported.[22] We think the only clinically relevant difference is in operative time and postoperative hospital stay. Differences in intraoperative blood loss and intestinal function recovery time, even though statistically significant, are not of much clinical significance.
We consider that the using of T-tube after LCBDE will lead to loss of bile, affect the absorption function of bowel, and slow down the intestinal peristalsis. However, with the spontaneously removed biliary stent, the biliary pressure is reduced without loss of bile, and this may help decrease postoperative complications.[23] In fact, in our study, none of the cases showed any biliary leakage.
A key advantage with use of biliary stents is their spontaneous removal without the need for a second procedure, which reduces the risk of complications and treatment expenses.[24] The biliary decompression surgery should not be ignored in consideration of the potential for temporary obstruction at the lower end of the CBD in the first few days after manipulations to extract duct calculi or retained stones. In our study, the average retention time of the biliary stent drainage tube was 6.6 days, which effectively prevented this complication.
However, the possibility of retention of biliary stent is a shortcoming that may necessitate endoscopic procedures with the associated risk of biliary atresia and cholangitis caused by the migration of stent, and remnant stones after surgery may not be removed readily. In our study, the biliary stent was not removed spontaneously in one case and an additional duodenum endoscopic procedure was performed one month after surgery. We consider that the time of spontaneous removal of stent is associated with the postoperative mental state of patient, activity, diet, and gastric motility. Moreover, previous studies have shown that in patients with intestinal adhesion or intestinal diverticulum, intestinal perforation occurs due to stent migration.[25] Therefore, use of stent drainage for patients with intestinal adhesion or intestinal diverticulum should be avoided.
Around 8% to 15% of patients with cholecystitis develop choledocholithiasis with in the first year after surgery.[7] If choledocholithiasis is not treated in time, it would progress to obstructive jaundice, acute cholangitis, pancreatitis thus increasing morbidity, and mortality.[8] Endoscopic and laparoscopic treatments of CBD stones are the well-known minimally invasive treatment options. However, endoscopic retrograde cholangiopancreatography is associated with serious complications such as pancreatitis, hemorrhage, duodenal perforation (5%–11%), and mortality of up to 1%.[9] LCBDE has the advantage of managing CBD stones associated with gallbladder stones in a single-stage procedure and avoids the need for endoscopic retrograde cholangiopancreatography and all its attendant complications.[10] LCBDE by choledochotomy provides unrestricted access to CBD and common hepatic duct, thus enabling access to difficult stones.[11] The LCBDE approach avoids Oddi sphincter manipulation, which can be particularly important in young patients.[12] At present, LCBDE has become one of the preferred treatment options for patients with choledocholithiasis.[1,2,13]
Traditionally, T-tube insertion has been applied most widely because of the advantage of decompressing the bile duct efficiently as well as for assessing and removing remnant CBD stones.[14] However, this method is not only more difficult, but also prone to bile leakage, bleeding, and a series of complications.[14–16] T-tube drainage could lead to excessive bile and electrolyte loss, affect the patient's recovery, prolong hospital stay, and increase treatment costs.[17,18] The use of minimally invasive techniques could reduce surgical trauma, hasten recovery, and reduce length of hospital stay. Indeed, the traditional T-tube drainage seems to negate the benefits of laparoscopic surgery at this time.
Primary closure of the CBD without biliary drainage has been performed for several years.[3,11] Although primary closure may avoid complications associated with T-tube placement, there is no conclusive data favoring one technique over the other.[19,20] Furthermore, secondary to instrumentation of the CBD and maneuvers for stone extraction, papilla could develop edema and increase biliary tree pressure, and the associated risk of bile leakage.[21] Insertion of a spontaneously removable biliary stent may be an alternative that can satisfy both conditions.
Despite the results and their statistical significance, the single-center scope of this study is a limitation. Large-scale randomized controlled trials are required to provide robust data on efficacy and safety of use of bile stent drainage in the future.
5. Conclusion
Primary closure of CBD with spontaneously removable biliary stent placement is safe and feasible after laparoscopic choledochotomy in suitable patients, and which is consistent with the aims of minimally invasive surgery. Our results show benefits of this approach in terms of shorter surgical time and lower associated costs. This innovation can improve the quality of life and increase overall patient satisfaction, while minimizing the risk of biliary complications. Therefore, we support the use of a spontaneously removable biliary stent insertion after LCBDE.
Acknowledgments
This work was supported by the funds from the National Natural Science Foundation of China (81272368 and 81471755) and the clinical capability construction project for Liaoning provincial hospitals (LNCCC-B03–2014).
Footnotes
Abbreviations: CBD = common bile duct, LCBDE = laparoscopic common bile duct exploration.
YX and CD contributed equally to this work.
The authors have no conflict of interests to disclose.
References
- 1.Savita KS, Bhartia VK. Laparoscopic CBD exploration. Indian J Surg 2010; 72:395–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shively EH, Richardson M, Romines R, et al. Laparoscopic common duct exploration in 90-bed rural hospital. Am Surg 2010; 76:626–629. [PubMed] [Google Scholar]
- 3.Ahmed I, Pradhan C, Beckingham IJ, et al. Is a T-tube necessary after common bile duct exploration? World J Surg 2008; 32:1485–1488. [DOI] [PubMed] [Google Scholar]
- 4.Abellan Morcillo I, Qurashi K, Abrisqueta Carrion J, et al. Laparoscopic common bile duct exploration. Lessons learned after 200 cases. Cir Esp 2014; 92:341–347. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed M, Diggory RT. Case-based review: bile peritonitis after T-tube removal. Ann R Coll Surg Engl 2013; 95:383–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu JS, Soper NJ. Comparison of laparoscopic choledochotomy closure techniques. Surg Endosc 2002; 16:1309–1313. [DOI] [PubMed] [Google Scholar]
- 7.Cuschieri A, Lezoche E, Morino M, et al. E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc 1999; 13:952–957. [DOI] [PubMed] [Google Scholar]
- 8.Lambou-Gianoukos S, Heller SJ. Lithogenesis and bile metabolism. Surg Clin North Am 2008; 88:1175–1194.vii. [DOI] [PubMed] [Google Scholar]
- 9.Coelho-Prabhu N, Shah ND, Van Houten H, et al. Endoscopic retrograde cholangiopancreatography: utilisation and outcomes in a 10-year population-based cohort. BMJ Open 2013; 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nathanson LK, O’Rourke NA, Martin IJ, et al. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg 2005; 242:188–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khaled YS, Malde DJ, de Souza C, et al. Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg Endosc 2013; 27:4164–4170. [DOI] [PubMed] [Google Scholar]
- 12.Lu J, Cheng Y, Xiong XZ, et al. Two-stage vs single-stage management for concomitant gallstones and common bile duct stones. World J Gastroenterol 2012; 18:3156–3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tinoco R, Tinoco A, El-Kadre L, et al. Laparoscopic common bile duct exploration. Ann Surg 2008; 247:674–679. [DOI] [PubMed] [Google Scholar]
- 14.Zhu QD, Tao CL, Zhou MT, et al. Primary closure versus T-tube drainage after common bile duct exploration for choledocholithiasis. Langenbecks Arch Surg 2011; 396:53–62. [DOI] [PubMed] [Google Scholar]
- 15.Tuvignon N, Liguory C, Ponchon T, et al. Long-term follow-up after biliary stent placement for postcholecystectomy bile duct strictures: a multicenter study. Endoscopy 2011; 43:208–216. [DOI] [PubMed] [Google Scholar]
- 16.Wei Q, Hu HJ, Cai XY, et al. Biliary drainage after laparoscopic choledochotomy. World J Gastroenterol 2004; 10:3175–3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wills VL, Gibson K, Karihaloot C, et al. Complications of biliary T-tubes after choledochotomy. ANZ J Surg 2002; 72:177–180. [DOI] [PubMed] [Google Scholar]
- 18.Angel Mercado M, Chan C, Orozco H, et al. Bile duct injuries related to misplacement of “T tubes”. Ann Hepatol 2006; 5:44–48. [PubMed] [Google Scholar]
- 19.Gurusamy KS, Samraj K. Primary closure versus T-tube drainage after laparoscopic common bile duct stone exploration. Cochrane Database Syst Rev 2007; CD005641. [DOI] [PubMed] [Google Scholar]
- 20.Ha JP, Tang CN, Siu WT, et al. Primary closure versus T-tube drainage after laparoscopic choledochotomy for common bile duct stones. Hepatogastroenterology 2004; 51:1605–1608. [PubMed] [Google Scholar]
- 21.Holdsworth RJ, Sadek SA, Ambikar S, et al. Dynamics of bile flow through the human choledochal sphincter following exploration of the common bile duct. World J Surg 1989; 13:300–304. [DOI] [PubMed] [Google Scholar]
- 22.Kelly MD. Results of laparoscopic bile duct exploration via choledochotomy. ANZ J Surg 2010; 80:694–698. [DOI] [PubMed] [Google Scholar]
- 23.Lee JS, Yoon YC. Laparoscopic common bile duct exploration using V-Loc suture with insertion of endobiliary stent. Surg Endosc 2015. [DOI] [PubMed] [Google Scholar]
- 24.Huang J, Zhu J. Spontaneously removed endobiliary J stent drainage after laparoscopic common bile duct exploration. Surg Endosc 2009; 23:1398–1402. [DOI] [PubMed] [Google Scholar]
- 25.Lenzo NP, Garas G. Biliary stent migration with colonic diverticular perforation. Gastrointest Endosc 1998; 47:543–544. [DOI] [PubMed] [Google Scholar]


