Abstract
Rationale:
Retrograde drilling is a well accepted procedure for osteochondral lesion of the talus and subchondral cyst with intact overlying cartilage. It has good results in most reports. Compared to anterograde drilling, retrograde drilling can protect the integrity of the articular cartilage. The purpose of this study was to evaluate the suitability of using retrograde drilling for osteochondral lesion with subchondral cyst and discuss the mechanism involved in the development of subchondral cyst.
Patient concerns:
We report a 53-year-old man who had complained left ankle pain that lasted over 6 months which was exacerbated by walking.
Diagnoses:
We diagnosed it as osteochondral lesion of the talus with subchondral cyst.
Interventions:
Plain X-ray, computed tomography, and magnetic resonance imaging (MRI) of the ankle.
Outcomes:
He undertook retrograde drilling without debridement of cartilage. After the surgery, the pain had been subsided for 1 year, although arthritic change had progressed. However, after 5 years of retrograde drilling, he revisited our hospital due to severe ankle pain. Plain X-ray and MRI showed arthritic change of the ankle and multiple cystic formation of talus.
Lessons:
Retrograde drilling has some problem because this procedure is not theoretically correct when the development of a subchondral cyst in osteochondral lesion of the talus is considered. In addition, retrograde drilling may impair uninjured bone marrow of the talus, resulting in the development of multiple cystic formations.
Keywords: osteochondral lesion of talus, retrograde drilling, subchondral cyst
1. Introduction
Osteochondral lesion of the talus (OLT) is an injury or abnormality of the talar articular cartilage and adjacent bone.[1] The incidence of OLT has been reported to be ranging from 0.09% of all talar fractures to 6.5% of ankle sprains. Patients typically present with chronic ankle pain along with intermittent swelling, stiffness, instability, and giving way.
Treatment for OLT depends on the size and location of the lesion as well as the activity level of the patient.[2] There is a wide variety of treatment strategies for osteochondral defects of the ankle.[3] Standard management protocol is usually accepted as follows: nonoperative management is typically used for acute and nondisplaced lesion, while operative treatment is used for chronic and displaced lesions. Generally, for small-sized lesions (<1.5 cm2), marrow-inducing reparative techniques such as antegrade drilling (transmalleolar drilling) or retrograde drilling (transtalar drilling) might be ideal treatment. For large-sized lesions (>1.5 cm2), restorative techniques such as osteochondral autologous transfer system and autologous chondrocyte implantation are ideal treatment methods.
Retrograde drilling is used for primary OLT and subchondral cyst with intact overlying cartilage.[4,5] It is also indicated when the defect is difficult to reach through usual arthroscopic portals.[5] Most surgeons have reported that the use of retrograde percutaneous drilling has good results in 81% to 100% of patients.[5,6]
We present a patient with advanced arthritic change and multiple cyst formation of talus after retrograde drilling for OLT with subchondral cyst. The purpose of this study was to evaluate if the retrograde drilling was an appropriate treatment for OLT with subchondral cyst by looking at the mechanism involved in the development of the subchondral cyst.
2. Consent
The patient signed informed consent for the publication of this case report and any accompanying images. Ethical approval of this study was waived by the ethics committee of Chonbuk National University Hospital because it was a case report.
3. Case report
A 53-year-old man (height of 172 cm, weight of 70 kg, body mass index of 23.6, office clerk) presented to our outpatient clinic with left ankle pain due to hyperextension of that ankle about 6 months ago. The pain was exacerbated by walking but improved by resting. He had not been treated for ankle pain in other hospitals. He did not have any specific history or family history with ankle pain. The symptom repeatedly got better and worse. It then got worse.
On examination, there were mild swelling and direct tenderness over the anterior aspect of ankle without any locking or impingement with foot movement. He had full range of motions. There was no positive sign of other examinations such as varus or valgus instability of the left ankle.
Plain anteroposterior (AP) and lateral radiographs of the left ankle showed a radiolucent lesion at the central portion of the talus. In computed tomography (CT), there was a subchondral cystic lesion (7 × 7 × 10 mm sized) on the central portion of the talus and multiple small subchondral cystic lesions on the medial side of the talus. T2-weighted coronal and sagittal magnetic resonance imaging (MRI) showed bone marrow edema on talus and subchondral cysts with high-signal intensity (Fig. 1A and B). The overlying cartilage on the osteochondral lesion was relatively intact. Based on CT and MRI, we diagnosed it as OLT with subchondral cyst and degenerative arthritis (Anderson stage 2A). Laboratory data showed normal values of white blood cell (WBC), neutrophil, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels (8700/μL, 5200/μL, and 9 and 0.2 mg/dL, respectively).
Figure 1.
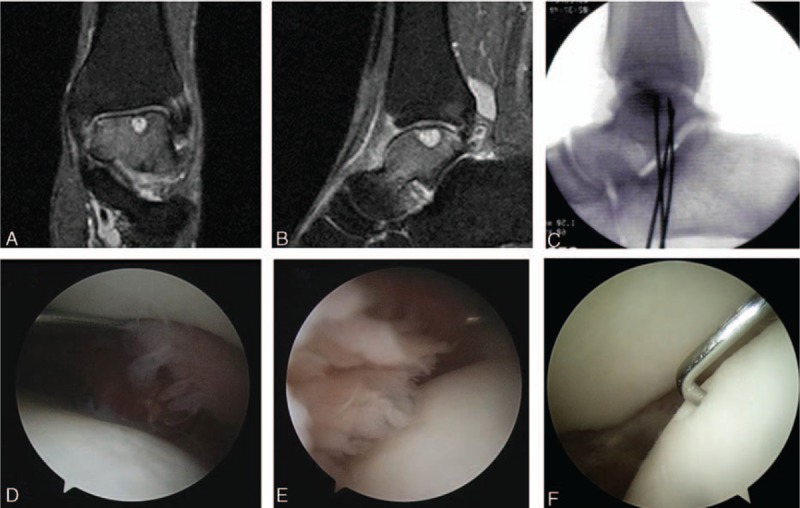
T2-weighted coronal (A) and sagittal (B) magnetic resonance images demonstrating bone marrow edema on talar body and osteochondral lesion with subchondral cyst. Retrograde drilling was performed using K-wires under C-arm image intensifier. (C) Arthroscopic finding showing synovitis surrounding subchondral cyst and relatively intact and stable talar cartilage (D—medial side, E—lateral side, F—central portion).
In spite of conservative treatment (short leg splint, medication for pain relief) with medication for about 3 months, symptoms persisted. Therefore, we decided to perform arthroscopic surgery.
In arthroscopic findings, there was synovitis surrounding the subchondral cyst in ankle joint (Fig. 1D–F). However, the cartilage on the osteochondral lesion was relatively intact with mild delamination (Fig. 1D–F). We performed arthroscopic synovectomy for nonspecific inflammatory synovium (meniscoid-like lesion). We performed retrograde drilling using K-wires (0.062 inch) for OLT without penetrating the subchondral bone with C-arm image intensifier (Fig. 1C). Pathologist reported the biopsy results of the synovium. It showed hyalinized connective tissue consistent with meniscoid-like lesion.
During 1 year of follow-up, AP radiographs of the left ankle revealed that the depression of the cartilage was gradually increased. However, he no longer complained ankle pain. He stopped visiting the outpatient department in our hospital. However, he revisited our outpatient clinic at 5 years after the surgery. At the time, he complained left ankle pain (9 point of visual analog scale [VAS]) that started about 4 months ago. It was more severe than the first symptom. He complained that it was difficult to walk because of the severe pain of the left ankle.
AP and lateral radiographs revealed subchondral sclerosis and osteophyte formation of the left ankle. T2-weighted sagittal and coronal MRI showed multiple cystic lesions, bone marrow edema in talus, and thin talar articular cartilage (Fig. 2A–C).
Figure 2.

T2-weighted coronal (A, B) and sagittal (C) magnetic resonance images showing multiple cystic lesions, bone marrow edema on subchondral, and body of the talus with thin talar articular cartilage. Arthroscopic finding showing fibrillated articular cartilage in whole talar dome, indicating degenerative change of the ankle (D, E).
Laboratory data showed normal values of WBC, neutrophil, and ESR (7400/μL, 4700/μL, and 10, respectively). His CRP was slightly elevated to 0.5 mg/dL (normal value ≤0.3 mg/dL). We performed additional laboratory tests to evaluate rheumatoid arthritis. However, rheumatoid factor and anticyclic citrullinated peptide antibody (anti-CCP Ab) were within normal range (RF = 6.62 IU/mL, anti-CCP Ab = 2.2 U/mL). On joint fluid analysis, WBC count was 350/mm3. There were about 25% polymorphonuclear leukocytes. The amount of glucose was almost the same as serum glucose level. The appearance of joint fluid was relatively clear with yellow color similar to that of normal joint fluid. Joint fluid was culture negative for any bacteria.
In arthroscopic findings, there were loose bodies and extensive degenerative change of the articular cartilage of the tibia and talus (Fig. 2D and E). We performed arthroscopic synovectomy and chondroplasty to remove the loose bodies. At 1 year after the surgery, pain of the ankle was reduced to 3 point in VAS. However, degenerative change of the left ankle gradually got worse in radiographs.
4. Discussion
To date, retrograde drilling is a well-accepted procedure for osteochondral lesion of talus with subchondral cyst and intact cartilage covering.[4,5] Compared with anterograde drilling, its advantage is that it can protect the integrity of the articular cartilage.[5]
The OLT with subchondral cyst in this case was an accurate indication of retrograde drilling because articular cartilage was relatively intact in primary surgery. However, multiple cystic formation and the osteoarthritis of the talus developed after the primary surgery. The mechanism involved in the development of subchondral cyst is discussed below.
Currently, there are 2 theories (mechanism and mucoid degeneration)[7–9] involved in the development of subchondral cyst with OLT. According to valve mechanism, subchondral cyst is caused by damaged cartilage functioning as a valve. It may allow intrusion of joint fluid from the joint space into the subchondral bone, but not in the opposite direction.[8,9] For this reason, Lui has suggested that debridement for articular cartilage of the osteochondral lesion should be a component of surgical treatment to remove the valve.[8] Another theory is mucoid degeneration of intramedullary connective tissue probable preceded by focal ischemia or aseptic necrosis.[7,9]
According to these theories, if the damaged cartilage is not debrided (retrograde drilling only), the subchondral cyst might recur because the damaged cartilage still can work as a valve. In addition, retrograde drilling can impair uninjured bone marrow of the talus through drilling tract. Therefore, the cystic formation might be caused by mucoid degeneration due to the development of focal ischemia along the drilling tracts. Moreover, it is difficult to target the lesion using fluoroscopic 2D imaging.[10] If accurate targeting to the cystic lesion is not accomplished, multiple intramedullary cysts might be caused by mucoid degeneration. Considering these theories, we need to keep in mind that retrograde drilling does not always induce a good result. It can show a contrary result (multiple cystic formation) like in this case.
The most common sites of OLT are medial and lateral talar dome.[2] However, in this case, the lesion was placed on the central area, indicating that there might be other causes of the osteochondral lesions such as rheumatoid arthritis. However, laboratory test and pathologic report showed general findings of degenerative arthritis and meniscoid-like lesion.
This article has some limitations. This is just 1 case report. Therefore, we cannot conclude that retrograde drilling is unsuitable for OLT by this case alone. However, we need to reconsider if retrograde drilling is indicated for osteochondral lesion of talus with cyst because of the mechanism of cyst formation and additional injury of normal talus caused by drilling.
In conclusion, retrograde drilling has some problem because this procedure is not theoretically correct considering the development of a subchondral cyst in OLT. In addition, retrograde drilling may impair uninjured bone marrow of the talus, resulting in the development of multiple cystic formations.
Footnotes
Abbreviations: Anti-CCP ab = anticyclic citrullinated peptide antibody, CRP = C-reactive protein, CT = computed tomography, ESR = erythrocyte sedimentation rate, MRI = magnetic resonance imaging, OLT = osteochondral lesion of the talus, RF = rheumatoid factor, WBC = white blood cell.
S-YJ and J-KK are equally contributed to this work.
This study was supported by a grant (CNUH-BRI-2012-02-005) of the Biomedical Research Institute of Chonbuk National University Hospital (CNUH-BRI), Republic of Korea.
The authors have no conflicts of interest to disclose.
References
- [1].Klammaer G, Maquieira GJ, Spahn S, et al. Natural history of nonoperatively treated osteochondral lesions of the talus. Foot Ankle Int 2015;36:24–31. [DOI] [PubMed] [Google Scholar]
- [2].Savage-Elliott I, Ross KA, Smyth NA, et al. Osteochondral lesions of the talus: a current concepts review and evidence-based treatment paradigm. Foot Ankle Spec 2014;7:414–22. [DOI] [PubMed] [Google Scholar]
- [3].Badekas T, Takvorian M, Souras N. Treatment principles for osteochondral lesions in foot and ankle. Int Orthop (SICOT) 2013;37:1697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hyer CF, Berlet GC, Philbin TM, et al. Retrograde drilling of osteochondral lesions of the talus. Foot Ankle Spec 2008;1:207–9. [DOI] [PubMed] [Google Scholar]
- [5].Corominas L, Sanpera I, Jr, Masrouha K, et al. Retrograde percutaneous drilling for osteochondritis dissecans of the head of the talus: case report and review of the literature. J Foot Ankle Surg 2014;55:328–32. [DOI] [PubMed] [Google Scholar]
- [6].Zengerink M, Struijs PA, Tol JL, et al. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc 2010;18:238–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Oqilvie-Harris DJ, Sarrosa EA. Arthroscopic treatment of post-traumatic cysts of the talus. Arthroscopy 2000;16:198–201. [DOI] [PubMed] [Google Scholar]
- [8].Lui TH. Arthroscopic bone grafting of talar bone cyst using posterior ankle arthroscopy. J Foot Ankle Surg 2013;52:529–32. [DOI] [PubMed] [Google Scholar]
- [9].Han SH, Lee JW, Lee DY, et al. Radiographic changes and clinical results of osteochondral defects of the talus with and without subchondral cysts. Foot Ankle Int 2006;27:1109–14. [DOI] [PubMed] [Google Scholar]
- [10].O’Louqhlin PF, Kendoff D, Pearle AD, et al. Arthroscopic-assisted fluoroscopic navigation for retrograde drilling of a talar osteochondral lesion. Foot Ankle Int 2009;30:70–3. [DOI] [PubMed] [Google Scholar]


