Abstract
Previous studies have shown differences in the psychosocial factors related to chronic localized pain (CLP) and chronic widespread pain (CWP). However, no studies have done an evaluation of differences between CLP and CWP from the viewpoint of family functioning. We did a cross-sectional study in a tertiary care setting to investigate possible differences in the relation of CWP and CLP to family functioning.
Patients with CLP (N = 126) or CWP (N = 75) were assessed for family functioning by the Family Assessment Device (FAD) and a comparison was done. Logistic regression analysis was used to estimate associations of family functioning subscales with pain status (CWP vs CLP), controlling for demographic variables, pain variables; pain duration, pain ratings, pain disability, and psychological factors; depression, anxiety, and catastrophizing. The odds ratios (ORs) for the presence of CWP were calculated.
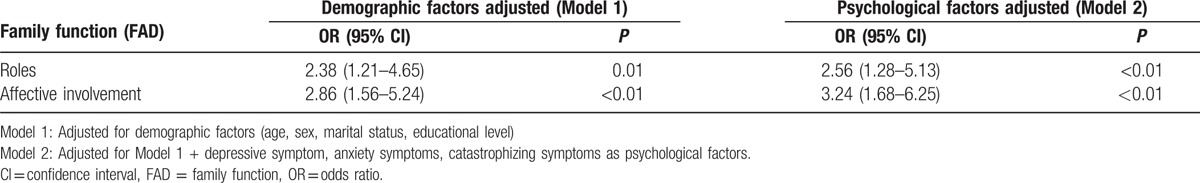
Compared to patients with CLP, patients with CWP showed a lower functional status for Roles and Affective Involvement. The ORs for CWP were significantly higher in lower functioning Roles (OR: 2.38, 95% CI: 1.21–4.65) and Affective Involvement (OR: 2.86, 95% CI: 1.56–5.24) after adjusting for demographic variables. The significant association of CWP to Roles and Affective Involvement remained after controlling for the pain variables and psychological factors.
This study shows that the families of patients with CWP have poorer family functioning than those with CLP. Our findings suggest that early identification and interventions for the family dysfunction of chronic pain patients are important to the treatment and prevention of CWP.
Keywords: chronic localized pain, chronic widespread pain, FAD, Family Functioning
1. Introduction
Chronic pain is a major public health problem that is accompanied by disability and psychological distress.[1,2] Chronic widespread pain (CWP) is defined as pain in both the left and right sides of the body, above and below the waist, and in the axial skeleton.[3] A number of studies have shown that patients with CWP present with higher levels of disability and psychological distress and lower quality of life than do patients with chronic localized pain (CLP), which is localized to 1 or a few body regions.[4–6]
Current cohort studies have reported that patients with CLP can develop CWP, both in population and patient sample studies. A systematic review[7] indicated that transition from CLP to CWP was experienced by 18% (median) of the participants. The review, based on 7 studies, demonstrated the following risk factors for CWP: female, higher age, depression, number of pain sites, and family history of pain. However, whether CWP and CLP have different mechanisms remains to be elucidated.
It is known that psychological factors such as depression, catastrophizing, anxiety, and social factors are related to chronic pain.[2,8,9] Of the social factors, the family is an important unit with complex psychosocial interactions,[10] and various family systems theories have been proposed.[11] However, insufficient attention has been paid to the role of the family in adult chronic pain.[12] To our knowledge, no studies have done an evaluation of the differences between the general classifications CLP and CWP from the viewpoint of family functioning.
Although a systematic review of youth with chronic pain showed impairment of family functioning and an association between family dysfunction and worsened physical and psychological functioning,[13] the relation between adult chronic pain and family functioning has not been studied adequately. Some studies of chronic pain that have used the Family Environment Scale (FES), a measure of family functioning, have reported a relation to specific aspects of impaired family functioning, such as low cohesion,[14–16] high control,[16,17] and high conflict,[14,15,17] but the results of these studies are inconsistent. Our background study found only 1 that assessed chronic pain using the Family Assessment Device (FAD),[18] the most commonly used measures of family functioning worldwide.[19] It reported family dysfunction related to specific diseases; adult fibromyalgia compared to osteoarthritis.[20]
To clarify possible differences in the relation of CWP and CLP to family functioning, FAD was used in a cross-sectional study in a tertiary care setting to identify the related impaired family functioning dimensions. Additionally, we controlled for demographics, pain variables, psychological factors, depression, anxiety, and catastrophizing, each of which has been suggested to be associated to family functioning,[21–23] as potential confounding factors.
2. Methods
2.1. Participants
The participants were first visit consecutive Japanese patients with chronic pain (pain of at least 3-months duration) seen in the outpatient clinic of the department of psychosomatic medicine at Kyushu University Hospital in Japan from January 2011 to October 2013.
To participate in the study, patients were required to be at least 18 years old and not have symptoms of dementia or other significant cognitive deficits or severe psychopathology (i.e., suicidal, severe depression, or psychosis). All of the 217 eligible patients seen in the clinic during this time period agreed to participate. Of them, 16 did not provide complete responses to the study questionnaires (92.6% response rate), which left the data of 201 participants available for analysis.
2.2. Procedures
The study participants were asked to fill out self-administered questionnaires concerning demographic characteristics, psychological features, pain variables, and medical history information while waiting to be examined. The study design was approved by the Kyushu University Institutional Review Board.
2.3. Demographic variables
Age, sex, marital status, and education level were collected as background information. Education level was classified into low and high: low levels of education covered compulsory education (9 years), whereas high education was defined as >9 years of schooling. Marital status was classified as: single (never married, widowed, divorced, or separated) versus married or cohabiting.
3. Measures
3.1. Family functioning
Family functioning was assessed by use of the Family Assessment Device (FAD).[18] FAD is based on the McMaster Model of Family Functioning (MMFF), “a clinically oriented conceptualization of families.”[18] FAD focuses on dimensions of family functioning “having the most impact on the emotional and physical health or problems of a family member.”[24] FAD consists of a 60-item self-report questionnaire that evaluates 6 dimensions of family functioning and overall general family functioning. The 6 dimensions of family functioning are as follows: problem solving (the family's ability to resolve problems), communication (how family members exchange verbal information), roles (the clearness and appropriateness of the allocation of family roles. In an unhealthy family, 1 or more family members are overloaded with family tasks.), affective responsiveness (the extent to which family members experience appropriate affect over a range of stimuli), affective involvement (the extent to which family members are interested in and value each other's activities and concerns), and behavior control (how family members express and maintain standards of behavior). The participants were asked to indicate the degree to which they agree with a statement on a 4-point Likert scale, with low scores indicating good family functioning and high scores indicating poor functioning. The Japanese version of FAD has shown adequate reliability and validity.[25]
3.2. Pain status
CWP was defined using the definition in the 1990 American College of Rheumatology (ACR) criteria for fibromyalgia.[3] CWP must be present in both the left and right sides of the body and above and below the waist, including the axial skeleton. If participants did not meet the criteria, they were categorized as having CLP. All participants were asked to rate the pain duration and to indicate the primary site. Both groups selected from a list of 10 sites that included the head and face, neck, shoulder, arms and hands, chest, abdomen, upper back, lower back, buttocks, lower limbs, and other sites, and these data were used to count the total number of chronic pain sites.
3.3. Pain ratings
The Short-Form McGill Pain Questionnaire (SF-MPQ) assesses sensory and affective dimensions of pain experience.[26] SF-MPQ consists of 15 items, with each item scored on a 4-point Likert intensity scale. The reliability and validity of the Japanese version of the SF-MPQ has been confirmed.[3]
3.4. Pain disability
The Pain Disability Assessment Scale (PDAS) evaluates the degree to which chronic pain interfered with various daily activities during the past week.[2] It contains 20 items demonstrating pain interference in 3 domains of functioning: activities of daily living, social activities, and activities using the low back. Each item is rated on a 4-point Likert scale. The range for the PDAS total score is from 0 to 60. Higher scores are indicative of greater levels of pain interference. The PDAS has been shown to have adequate validity and reliability.[27]
3.5. Depression
The Center for Epidemiologic Studies Depression Scale (CES-D) is a 20-item instrument that assesses the frequency of depressive symptoms in the past week on a scale from 0 (rarely or none of the time) to 3 (most or all of the time).[28] Total scores for the CES-D range from 0 to 60, with higher scores indicating a higher level of depression. A score of 16 or greater is regarded as clinically significant depression. The reliability and validity of the Japanese version of the CES-D has been documented.[29]
3.6. Trait anxiety
The trait anxiety level was assessed by the trait scale of the State Trait Anxiety Inventory (STAI).[30] This scale includes 20 items that indicate the emotional condition. Each item is scored from 1 to 4 on a Likert scale and higher scores indicate more severe anxiety. The Japanese version of the STAI has been validated.[31]
3.7. Pain catastrophizing
Pain catastrophizing was measured using the Pain Catastrophizing Scale (PCS),[32] which contains 13-items regarding 3 domains of pain-catastrophizing cognitions, including rumination, magnification, and helplessness. Respondents indicate the degree to which they experience each catastrophizing thought on a 5-point scale from (0) not at all to (4) all the time. The Japanese version of the PCS has been demonstrated to have adequate validity and reliability.[33]
3.8. Statistical analysis
CLP and CWP were compared with respect to demographic factors (age, sex, marital status, level of education), pain variables (pain duration, the number of pain sites, pain ratings, pain disability), and psychological features (depression, anxiety, catastrophizing). Family functioning scales were also compared between CLP and CWP. Normality of data distribution was assessed with the Kolmogorov–Smirnov test. Student's t-test was performed for parametric continuous variables (age, depression, anxiety) and Mann–Whitney U test was used to examine nonparametric variables (pain variables, catastrophizing, family functioning). χ2 analysis was used to compare sex, marital status, and education level. Logistic regression analysis was used to estimate associations of family functioning subscales with pain status (CWP vs CLP). These results were summarized using odds ratios (ORs) and their confidence intervals (CIs).
First, we adjusted for demographic variables (Model 1: age, sex, marital status, education level), pain duration (Model 2: model 1 + pain duration), and pain outcomes (Model 3: model 2 + pain ratings, pain disability). Next, after adjusting for demographic variables (Model 1: age, sex, marital status, education level), we controlled for psychological factors (Model 2: Model 1 + depression, anxiety, catastrophizing). The analyses were performed with the SPSS 17.0 Statistical Package. The level of significance was set at P < 0.05.
4. Results
4.1. Pain characteristics
Based on the American College of Rheumatology (ACR) criteria for fibromyalgia,[3] 75 participants were categorized as having CWP and 126 as having CLP. Of the patients with CWP, 52 (69.3%) were diagnosed with fibromyalgia, 11 (14.6%) with myofascial pain syndrome, and 12 (16.0%) with other. Of the patients with CLP, the primary pain sites were the head and face for 25 (19.8%), neck for 11 (8.7%), shoulder for 6 (4.8%), arms and hands for 5 (4.0%), chest for 5 (4.0%), abdomen for 10 (7.9%), upper back for 13 (10.3%), lower back for 16 (12.6%), buttocks for 9 (7.1%), lower limbs for 22 (17.4%), and other sites for 4 (3.2%).
4.2. Relation between pain status and mediating factors
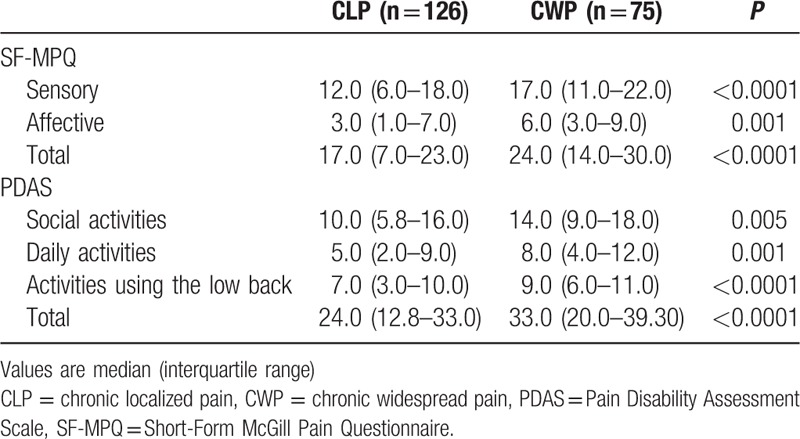
Pain variables and demographic and psychological factors are compared for CLP and CWP in Table 1. The participants with CWP were significantly younger and more likely to be female than were those with CLP. There was no significant difference between the groups in marital status, education level, pain duration, or psychological features (depression, anxiety, catastrophizing). CWP subjects were more likely to report a higher number of pain sites than those with CLP. Table 2 shows the results of pain ratings (SF-MPQ) and pain disability (PDAS) as pain outcomes. The median scores for the participants with CWP were higher than for those with CLP on both the SF-MPQ and PDAS.
Table 1.
Characteristics.
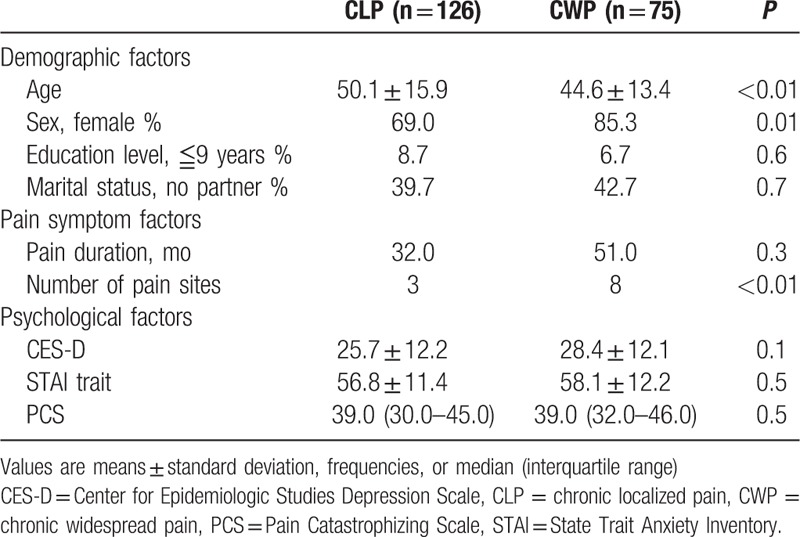
Table 2.
Pain outcomes.
4.3. Family functioning
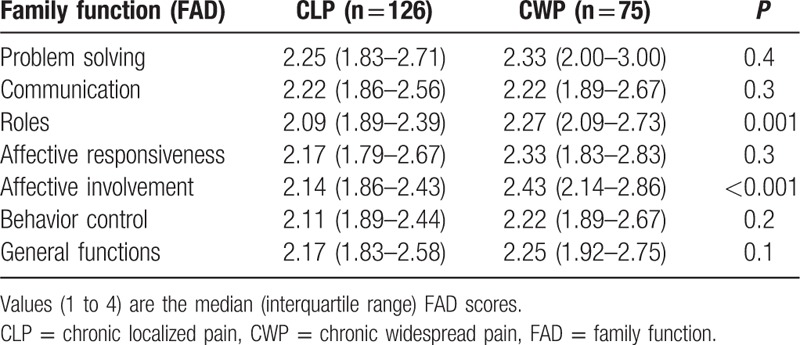
Substantial differences in the FAD subscales were found between CLP and CWP. Both the Roles and Affective Involvement scores were significantly higher for participants with CWP than for those with CLP (Table 3), which demonstrates a lower functional status for Roles and Affective Involvement.
Table 3.
Family function.
4.4. Regression results
The relation between family functioning and the presence of CWP was examined by a logistic regression analysis that focused on the family functioning subscales Roles and Affective Involvement. CWP increased significantly with incremental score increases for Roles and Affective Involvement when adjusted for the demographic variables (Model 1). After adjustment for the covariates in Model 1 plus pain duration (Model 2: model 1 + pain duration) and pain outcomes (Model 3: model 2 + pain ratings, pain disability), the relations remained significant (Table 4). When controlled for psychological factors (Model 2: model 1+ depression, anxiety, catastrophizing), the significant association of CWP to Roles and Affective Involvement remained (Table 5).
Table 4.
Odds ratios for CWP (dependent variable) according to the incremental scores for family functioning (independent variable) adjusted by pain variables.
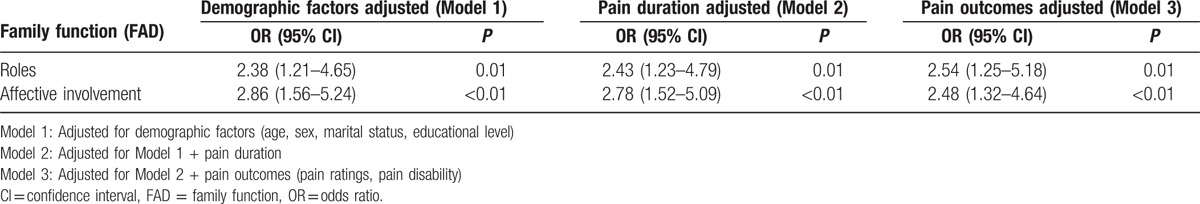
Table 5.
Odds ratios for CWP (dependent variable) according to the incremental scores for family functioning (independent variable) adjusted by psychological factors.
5. Discussion
To our knowledge, this is the first study that has shown more dysfunction in the families of patients with CWP than in those with CLP. In this study, Roles and Affective Involvement of FAD for CWP were identified as factors of family functioning that were significantly impaired. Moreover, we demonstrated that these 2 types of family dysfunction significantly associated to the presence of CWP after adjusting for demographic (age, sex, education level, marital status), pain variables (pain duration, pain ratings, pain disability), and psychological factors (depression, anxiety, catastrophizing).
Interestingly, our findings that the role factor was more impaired in patients with CWP than with CLP is consistent with a previous study[20] that showed more impaired functioning of Roles and Affective Responsiveness in a group of patients with fibromyalgia than was found for patients with osteoarthritis. As far as we know, no other study has used FAD to investigate the family functioning of a cohort of adults with chronic pain. In order to confirm our results, further study will be needed.
Payne described family roles as being rigid in the families of patients with chronic pain (Payne, B.A. unpublished data, 1982): the families of chronic pain patients generally appear to be inflexible. Based on our results, we can assume that the families of CWP patients are more inflexible than those of CLP. A personal trait of chronic pain seems to be that it is related to roles dysfunction. Young et al[34] reported that “self-sacrifice schema” is commonly seen in chronic pain, based on the early maladaptive schema (EMS) concept, which supports the idea that early childhood experiences lay the basis for a person's identity and relationships with others. The Young report found that self-sacrifice is a feature that drives a person to focus voluntarily on fulfilling the needs of others at the expense of one's own gratification. Furthermore, Saariaho et al[35] demonstrated that patients with chronic pain showed high “self-sacrifice schema” based on the EMS concept. They also reported that “self-sacrifice schema” was associated with higher pain disability in a group of women with chronic pain. The above descriptions of self-sacrifice appear to be consistent with our clinical impression that patients with CWP often take on an intra-family role of self-sacrifice. Whether or not patients with CWP are more prone to having the property of self-sacrifice compared to patients with CLP will be an interesting topic for further investigation.
This is the first study to report impaired Affective Involvement in family functioning for CWP. Some studies have related an impaired emotional relationship with family members to chronic pain. It has been reported that chronic pain patients have poor emotional relationships with both parents during childhood, particularly those with fibromyalgia.[36] Our result of impaired Affective Involvement in family functioning for CWP may reflect poor emotional relationships with family members over the long term, in the form of repeated perceived social stress, even though a current impaired relationship may be responsible, to some extent, for the pain behaviors of the patient.
An additional factor is maltreatment. Previous studies have shown a relation between maltreatment and chronic pain.[37–39] In particular, a higher prevalence of victimization has been reported for patients with CWP (mainly fibromyalgia) than for other pain diseases.[40,41] Emotional abuse and neglect, aspects of maltreatment, have also been reported in CWP. Moreover, it was reported that the most frequent culprits in victimization are the family of origin and the partner.[41] Although we did not investigate maltreatment in this study, it is reasonable to think that maltreatment would be a factor in the family dysfunction of chronic pain patients.
The mechanism by which the identified impaired family functioning contributes to CWP is unclear. One possible factor mediating/underlying family dysfunction and CWP is overactivity. Van Houdenhove et al[42] defined an overactive lifestyle seen in patients with chronic fatigue syndrome (CFS) and fibromyalgia (FM) as “action proneness.” They reported that “action proneness” may be a factor that makes people more vulnerable to CFS/FM and that initiates and perpetuates the disease because of physical overburdening created by a tendency toward attempting to exceed physical limits. It has also been reported that patients tend to push their physical limits to seek approval to compensate for low self-esteem and to prevent negative emotion, especially for patients who were maltreated in childhood.[41,42] Considering the above, “action proneness” may be related to CWP.
Our result that the percentage of women with CWP is significantly higher than that of CLP is consistent with previous studies.[7,40] However, contrary to previous studies, depression, anxiety, catastrophizing, and higher age were not significantly related to CWP. The reason may be that this study was done in a tertiary care setting that specializes in psychosomatic medicine, where higher prevalence rates of psychological distress tend to be found through the process of referral. This may reduce the differences in the psychological factors and reflect a bias toward demographic factors; thus, care must be taken in generalizing these findings.
Chronic pain and family functioning could mutually influence each other. Therefore, there is the possibility that poor functioning, pain disability, and psychological factors influence the family functioning of patients with CWP; however, our results suggest that the contribution of family dysfunction to CWP was not strongly affected by the current pain disability, psychological factors, depression, anxiety, or catastrophizing. One possible interpretation of our findings is that family dysfunction may have a more intimate involvement in the development and experience of CWP than it does for CLP, as mentioned above. The most important limitation is that we are not able to draw a conclusion of causality between family dysfunction and the development of CWP because of the cross-sectional design.
Our findings show that family functioning is more impaired in CWP compared to CLP. From a psychological point of view, our results suggest that early identification and targeted interventions for the family dysfunction of chronic pain patients is important to the treatment and prevention of CWP. Also, it would be beneficial to provide intervention to develop individual interpersonal skills and introspective ability, in addition to family intervention, in a comprehensive program for the treatment of chronic pain because of the reciprocal nature of family functioning and personal traits. Further study will be required to clarify the associations of family functioning with the development of CWP in different settings, such as longitudinal, primary settings.
Footnotes
Abbreviations: CES-D = Center for Epidemiologic Studies Depression Scale, CFS = chronic fatigue syndrome, CIs = confidence intervals, CLP = chronic localized pain, CWP = chronic widespread pain, EMS = early maladaptive schema, FAD = Family Assessment Device, FM = fibromyalgia, ORs = odds ratios, PCS = Pain Catastrophizing Scale, PDAS = Pain Disability Assessment Scale, SF-MPQ = Short-Form McGill Pain Questionnaire, STAI = State Trait Anxiety Inventory.
Funding: This research was supported by JSPS KAKENHI Grant Number 25460903 and the Research Project on Elucidation of Chronic Pain from the Japan Agency for Medical Research and Development, AMED.
The authors have no conflicts of interest to disclose.
References
- [1].Smith BH, Elliott AM, Chambers WA, et al. The impact of chronic pain in the community. Fam Pract 2001;18:292–9. [DOI] [PubMed] [Google Scholar]
- [2].Tunks ER, Crook J, Weir R. Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Can J Psychiatry 2008;53:224–34. [DOI] [PubMed] [Google Scholar]
- [3].Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 1990;33:160–72. [DOI] [PubMed] [Google Scholar]
- [4].Hoffman DL, Dukes EM. The health status burden of people with fibromyalgia: a review of studies that assessed health status with the SF-36 or the SF-12. Int J Clin Pract 2008;62:115–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia compared with rheumatoid arthritis: I. Psychiatric diagnoses and functional disability. Psychosom Med 1997;59:565–71. [DOI] [PubMed] [Google Scholar]
- [6].Bergman S. Psychosocial aspects of chronic widespread pain and fibromyalgia. Disabil Rehabil 2005;27:675–83. [DOI] [PubMed] [Google Scholar]
- [7].Larsson B, Björk J, Börsbo B, et al. A systematic review of risk factors associated with transitioning from regional musculoskeletal pain to chronic widespread pain. Eur J Pain 2012;16:1084–93. [DOI] [PubMed] [Google Scholar]
- [8].Keefe FJ, Rumble ME, Scipio CD, et al. Psychological aspects of persistent pain: current state of the science. J Pain 2004;5:195–211. [DOI] [PubMed] [Google Scholar]
- [9].Gupta A, Silman AJ, Ray D, et al. The role of psychosocial factors in predicting the onset of chronic widespread pain: results from a prospective population-based study. Rheumatology 2006;46:666–71. [DOI] [PubMed] [Google Scholar]
- [10].Litman TJ. The family as a basic unit in health and medical care: a social-behavioral overview. Soc Sci Med 1974;8:495–519. [DOI] [PubMed] [Google Scholar]
- [11].Turk DC, Flor H, Rudy TE. Pain and families. I. Etiology, maintenance, and psychosocial impact. Pain 1987;30:3–27. [DOI] [PubMed] [Google Scholar]
- [12].Turk DC, Rudy TE, Flor H. Why a family perspective for pain? Int J Fam Ther 1985;7:223–34. [Google Scholar]
- [13].Lewandowski AS, Palermo TM, Stinson J, et al. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain 2010;11:1027–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dura JR, Beck SJ. A comparison of family functioning when mothers have chronic pain. Pain 1988;35:79–89. [DOI] [PubMed] [Google Scholar]
- [15].Naidoo PP. Correlations among general stress, family environment, psychological distress, and pain experience. Percept Mot Skills 1994;78:1291–6. [DOI] [PubMed] [Google Scholar]
- [16].Romano JM, Turner Ja, Jensen MP. The family environment in chronic pain patients: comparison to controls and relationship to patient functioning. J Clin Psychol Med Settings 1997;4:383–95. [Google Scholar]
- [17].Feuerstein M, Sult S, Houle M. Environmental stressors and chronic low back pain: life events, family and work environment. Pain 1985;22:295–307. [DOI] [PubMed] [Google Scholar]
- [18].Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. J Marital Fam Ther 1983;9:171–80. [Google Scholar]
- [19].Hamilton E, Carr A. Systematic review of self-report family assessment measures. Family Process 2015;55:16–30. [DOI] [PubMed] [Google Scholar]
- [20].Kugu N, Kaptanoglu E, Kavakci O, et al. Psychopathology, family functioning and marital relationship in female patients with fibromyalgia syndrome. Neurol Psychiat Br 2010;16:83–90. [Google Scholar]
- [21].Keitner GI, Miller IW. Family functioning and major depression: an overview. Am J Psychiatry 1990;147:1128–37. [DOI] [PubMed] [Google Scholar]
- [22].Wang J, Chen Y, Tan C, et al. Family functioning, social support, and quality of life for patients with anxiety disorder. Int J Soc Psychiatry 2016;62:5–11. [DOI] [PubMed] [Google Scholar]
- [23].Jastrowski Mano KE, Khan KA, Ladwig RJ, et al. The impact of pediatric chronic pain on parents’ health-related quality of life and family functioning: reliability and validity of the PedsQL 4.0 Family Impact Module. J Pediatr Psychol 2011;36:517–27. [DOI] [PubMed] [Google Scholar]
- [24].Ryan CE, Epstein NB, Keitner GI, et al. Evaluating and Treating Families: The McMaster Approach. Taylor & Francis, 2005. [Google Scholar]
- [25].Saeki T, Asukai N, Miyake Y, et al. Reliability and validity of the Japanese version of the Family Assessment Device (FAD). Arch Psychiatr Diagn Clin Evaluation 1997;8:181–92. [Google Scholar]
- [26].Melzack R. The short-form McGill Pain Questionnaire. Pain 1987;30:191–7. [DOI] [PubMed] [Google Scholar]
- [27].Yamashiro K, Arimura T, Iwaki R, et al. A multidimensional measure of pain interference. Clin J Pain 2011;27:338–43. [DOI] [PubMed] [Google Scholar]
- [28].Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Meas 1977;1:385–401. [Google Scholar]
- [29].Shima S, Shikano T, Kitamura T, et al. New self-rating scale for depression (in Japanese). Clin Psychiatry 1985;27:717–23. [Google Scholar]
- [30].Spielberger CD, Gorusch RL, Lushene R. State-Trait Anxiety Inventory Manual. Palo Alto: Consulting Psychologists Press; 1970. [Google Scholar]
- [31].Nakazato K, Mizuguchi K. Studies on psychometric char-acteristics of depression in the field of internal medicine. (in Japanese). Shinshin-Igaku 1982;22:107–12. [Google Scholar]
- [32].Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assessment 1995;7:524–32. [Google Scholar]
- [33].Matsuoka H, Sakano Y. Assessment of cognitive aspect of pain: development, reliability, and validation of Japanese version of Pain Catastrophozing Scale (in Japanese). Jpn J Psychosom Med 2007;47:95–102. [Google Scholar]
- [34].Young JE, Klosko JS, Weishaar ME. Schema Therapy: A Practitioner's Guide. Guilford Press, 2003. [Google Scholar]
- [35].Saariaho THJ, Saariaho ASI, Karila Ia, et al. Early maladaptive schemas in Finnish adult chronic male and female pain patients. Scand J Pain 2010;1:196–202. [DOI] [PubMed] [Google Scholar]
- [36].Imbierowicz K, Egle UT. Childhood adversities in patients with fibromyalgia and somatoform pain disorder. Eur J Pain (London, England) 2003;7:113–9. [DOI] [PubMed] [Google Scholar]
- [37].Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? Clin J Pain 2005;21:398–405. [DOI] [PubMed] [Google Scholar]
- [38].Lampe A, Doering S, Rumpold G, et al. Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res 2003;54:361–7. [DOI] [PubMed] [Google Scholar]
- [39].Walker Ea, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia compared with rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosom Med 1997;59:572–7. [DOI] [PubMed] [Google Scholar]
- [40].Kindler LL, Jones KD, Perrin N, et al. Risk factors predicting the development of widespread pain from chronic back or neck pain. J Pain 2010;11:1320–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Van Houdenhove B, Neerinckx E, Lysens R, et al. Victimization in chronic fatigue syndrome and fibromyalgia in tertiary care: a controlled study on prevalence and characteristics. Psychosomatics 2001;42:21–8. [DOI] [PubMed] [Google Scholar]
- [42].Van Houdenhove B, Neerinckx E, Onghena P, et al. Premorbid “overactive” lifestyle in chronic fatigue syndrome and fibromyalgia: an etiological factor or proof of good citizenship? J Psychosom Res 2001;51:571–6. [DOI] [PubMed] [Google Scholar]


