Abstract
Background:
Hemiplegic shoulder pain (HSP) is one of the most common comorbidities in stroke patients with flaccid shoulders. The pain limits functional motor recovery and affects the activities of daily living after acute stroke. This study investigated the effects of hyaluronic acid (HA) injection on pain reduction and motor function in subacute stroke patients with HSP and injury.
Methods:
A randomized, double-blinded controlled trial was conducted in a medical center. Twenty-six subacute stroke patients were enrolled and randomly divided into 2 groups: the experimental group (n = 16) received ultrasound-guided, subacromial HA injections once per week for 3 weeks and conventional rehabilitation, whereas the control group (n = 10) received 0.9% sodium chloride injections once per week for 3 weeks and conventional rehabilitation. Shoulder pain and motor function were evaluated before and after the intervention using the visual analog scale (VAS) and the Fugl–Meyer assessment for the upper extremity (FMA-UE), respectively.
Results:
In the experimental group, significant differences were found in VAS (P = 0.003), shoulder flexion (P = 0.03) and abduction (P = 0.02), and FMA-UE (P = 0.003) after treatment. In the control group, there were significant differences in VAS (P = 0.007), shoulder flexion (P = 0.035), and FMA-UE (P = 0.042) after treatment. The comparison of the changes in the parameters between the experimental and control groups, after each intervention, revealed a significant difference in VAS (P = 0.001).
Conclusion:
Subacromial HA injection could result in positive effects on shoulder pain and shoulder abduction in subacute stroke patients with HSP and injury.
Keywords: hemiplegic shoulder, hyaluronic acid, pain, stroke
1. Introduction
Hemiplegic shoulder pain (HSP) is one of the most common complications after acute stroke. A stroke patient with a flaccid shoulder also has a high likelihood of experiencing HSP during rehabilitation and daily life.[1–5] HSP has negative effects on poststroke functional recovery, activities of daily living, quality of life, and length of hospital stay.[3,6,7] Several interventions, including physical modalities, exercise, medication, and local injections, have been used to treat HSP in patients with stroke.[8–15] Rotator cuff injury may play an important role in HSP after acute stroke.[4,16] The physician may prescribe steroid or hyaluronic acid (HA) injections to alleviate pain associated with rotator cuff lesions.[10,13,17–19] Although immediate pain reduction can be significant, the long-term side effects of steroid injections include tissue degeneration and tendon rupture.[20] Therefore, HA injection is an alternative intervention for reduction of pain and inflammation; HA protects the cartilage and inhibits degeneration, and improves the metabolism in synovial fluid, tendons, and ligaments. Meloni et al[21] found that intraarticular HA injection in patients with supraspinatus tendinitis resulted in positive effects on shoulder pain and motion and activities of daily living. In previous studies, researchers found that subacromial HA injection in patients with rotator cuff injury resulted in significant pain reduction for 6 to 12 weeks.[18,22] To the best of our knowledge, no studies have explored the effects of HA injection in patients with HSP, or the treatment of rotator cuff tears in stroke patients with hemiplegia. The aim of this study was to investigate the effects of HA injection for pain reduction and motor function recovery in subacute stroke patients with hemiplegic shoulder injury and pain.
2. Materials and methods
The study was a double-blind, randomized controlled trial (clinical trial registration number NCT02465853). A parallel-group design with allocation concealment was used in this study. We did not estimate the sample size because this was a pilot study to investigate HA effects on HSP for stroke patients with rotator cuff dysfunction. The participants were enrolled between February 2015 and May 2016, at a rehabilitation unit of a single medical center.
Of the 115 stroke patients admitted to our rehabilitation unit for an inpatient rehabilitation program, 26 stroke patients with a hemiplegic shoulder met the inclusion criteria and completed the procedures of this study (Fig. 1). The inclusion criteria were as follows: stroke patients with unilateral hemiplegia (stroke onset within 6 months), hemiplegic shoulder injuries (on sonography), and pain (visual analog scale [VAS] ≥3). The exclusion criteria were shoulder pain or injury before stroke, systemic neuromuscular disease, or poor cognition leading to difficulty in understanding study procedures. The study was approved by the Institutional Review Board at our hospital. We followed the ethical principles for medical research involving human subjects according to the Declaration of Helsinki 2013. The patients understood the study procedures and provided written informed consent before the assessments and interventions.
Figure 1.
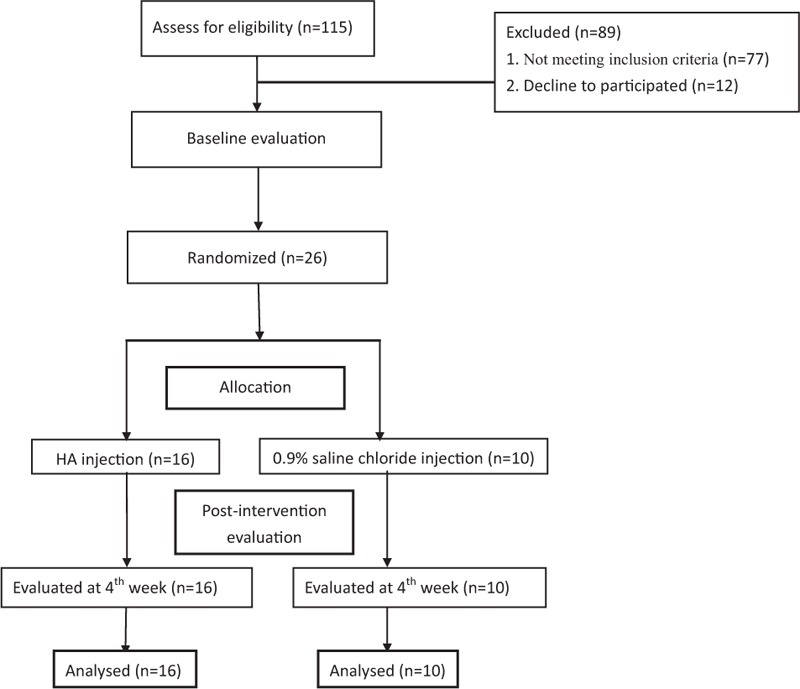
Flow diagram of eligible patients selected for this study.
We randomly divided the patients with stroke into 2 groups before treatment. Randomization was performed by a research assistant using sequentially numbered, sealed, and opaque envelopes. In the experimental group, 16 patients with stroke received a 2.5 mL sodium hyaluronate injection (ARTZ Dispo, Seikagaku, Tokyo, Japan) into the subdeltoid bursa under ultrasound guidance (Fig. 2) once per week, for 3 weeks, and were also enrolled in a regular inpatient rehabilitation program (1 hour of physical therapy and 1 hour of occupational therapy/d, 5 days/wk). In the control group, 10 patients who were also enrolled in the inpatient rehabilitation program received a 0.9% sodium chloride injection (2.5 mL) into the subdeltoid bursa. The injections were administered by the same physiatrist, who was experienced in ultrasound-guided injections. The enrolled patients with stroke were blinded to the content of the local injections in this study.
Figure 2.
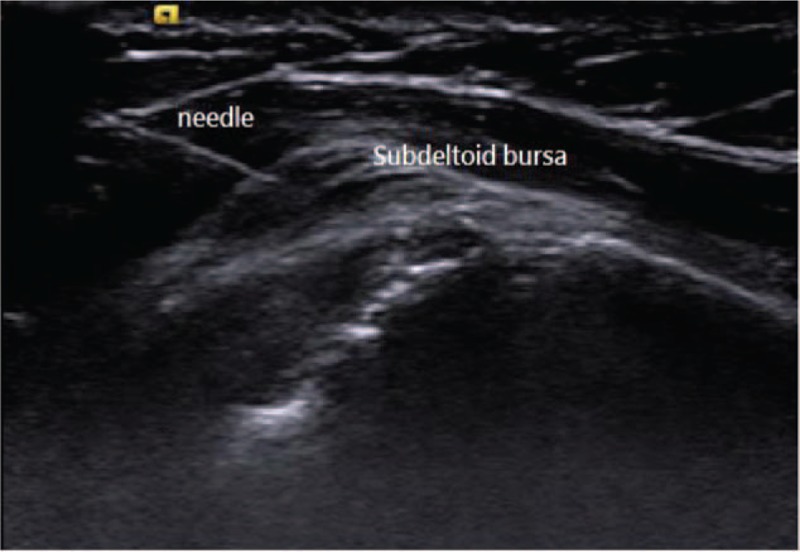
Subdeltoid hyaluronic acid injections under ultrasound guidance.
A physical therapist, who was blinded to the interventions, assessed the following parameters before and after treatment: shoulder spasticity, measured by the modified Ashworth scale (MAS)[23,24]; shoulder subluxation, with a fingerbreadth of displacement between the acromion and humeral head; pain-free range of motion of the hemiplegic shoulder, as measured with a goniometer; Fugl–Meyer assessment of the upper extremity (FMA-UE)[25]; and HSP. The presence of HSP was determined when a patient felt shoulder pain at rest, or during passive movement of the hemiplegic shoulder, and the severity of HSP was evaluated using a 10-cm VAS for each patient.
2.1. Statistics
Categorical variables between groups were compared using Fisher exact test. Continuous variables (median [IQR]) were compared by Mann–Whitney U test. Variables before and after each treatment were compared by the Wilcoxon signed-rank test. A P-value less than 0.05 was defined as statistically significant. All statistical tests were performed using SPSS 19.0 (SPSS, Inc., Chicago, IL).
3. Results
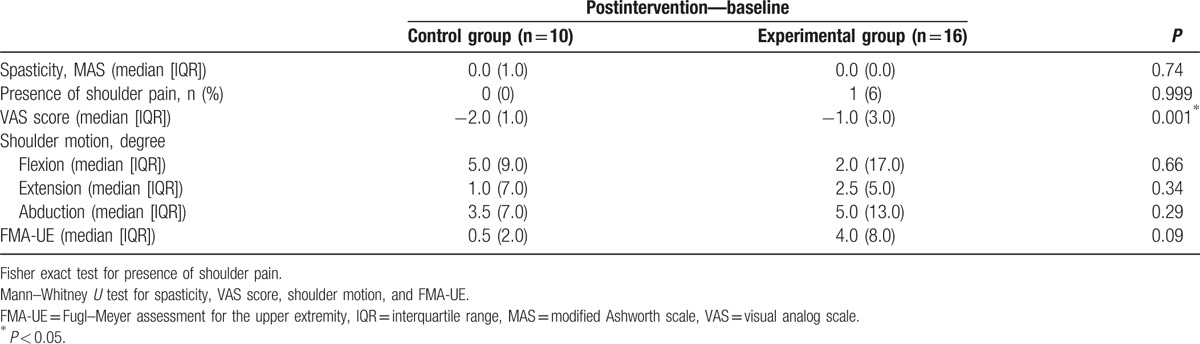
The trial ended in May 2016 when the participants completed the course of interventions and postintervention evaluations. There were no reports of adverse effects in participants receiving HA or normal saline injections. Table 1 shows the clinical characteristics of participants, which were not significantly different between the experimental and control groups. There were no significant differences in the physical findings between these 2 groups before treatment (Table 2). In the experimental group (Table 2), there were significant differences in VAS scores (P = 0.03); in shoulder movements, including flexion (P = 0.03) and abduction (P = 0.02); and in the FMA-UE scores (P = 0.003) following treatment. In the control group (Table 2), there were significant differences in VAS scores (P = 0.007), shoulder flexion (P = 0.035), and FMA-UE scores (P = 0.042) after treatment. A comparison of parameters before and after treatment in the experimental and control groups revealed a significant difference in the VAS scores (P = 0.001) (Fig. 3), with the FMA-UE showing a trend toward significant improvement (P = 0.09) (Table 3).
Table 1.
Clinical characteristics of the stroke patients in the control and experimental groups.
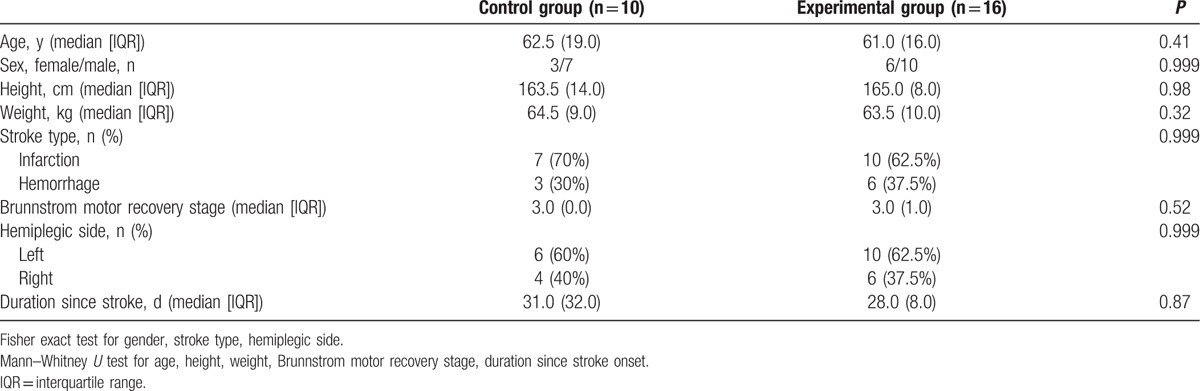
Table 2.
Comparison of the physical findings of the experimental and control groups.
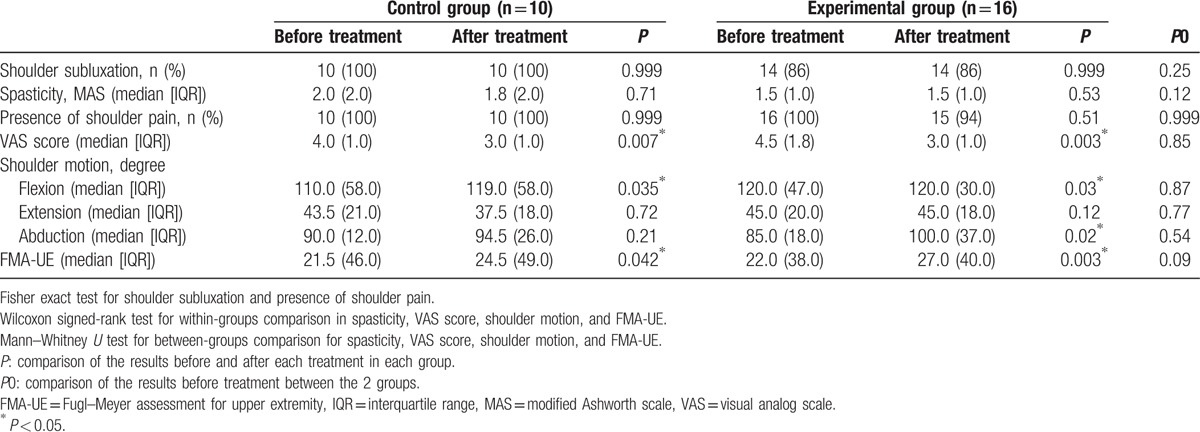
Figure 3.
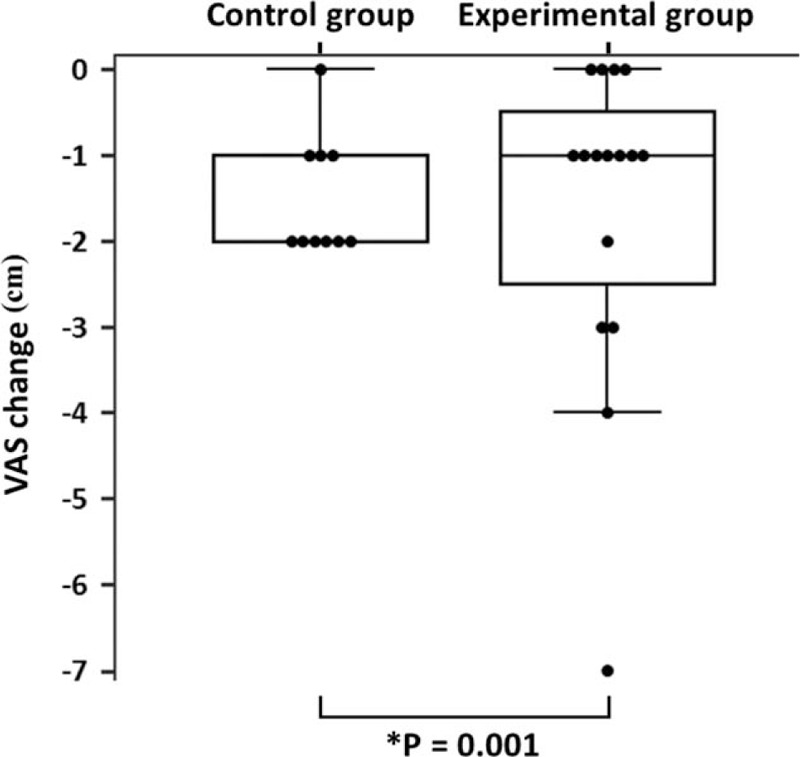
VAS score change (postintervention vs baseline) in the control and experimental groups. VAS = visual analog scale.
Table 3.
Comparison of the changes in hemiplegic shoulder pain and functional outcomes between the control and experimental groups.
4. Discussion
Conventional rehabilitation and medication could result in significant pain reduction and improved shoulder motor function in subacute stroke patients with hemiplegia. A greater reduction in HSP was evident following treatment with HA injections, compared to that observed in the control group. Additionally, HA may also be beneficial for reducing HSP in subacute stroke patients with rotator cuff injury. Our study showed that patients with stroke exhibited significantly improved shoulder flexion and abduction following HA treatment. In contrast, only shoulder flexion appeared to improve significantly following treatment with placebo. Chou et al[18] and Merolla et al[19] reported that subacromial HA injections were effective in alleviating shoulder pain and improving shoulder function in patients with rotator cuff injury or tendinopathy. Similarly, our findings revealed a beneficial effect for hemiplegic shoulder function and pain reduction after HA injection in stroke patients with HSP and shoulder injury.
HA may provide antiinflammatory effects in patients with rotator cuff injuries by inhibiting the mRNA expression of proinflammatory cytokines and cyclooxygenase-2/prostaglandin E2 production.[26] Therefore, the inhibitory effects of HA on inflammatory cells may lead to superior pain management in subacromial bursitis associated with rotator cuff injury.[18,26] In our study, we also found that subacute stroke patients with rotator cuff lesions showed better pain management following HA injection. Additionally, shoulder abduction significantly improved after subacromial HA injections, which were also associated with further reductions of HSP.
Similar improvements in motor function were also evident from the FMA-UE scores in both groups after 3 weeks of conventional inpatient rehabilitation. A tendency toward improvement was noted in the FMA-UE scores of patients with stroke who received subacromial HA injections, compared to the scores in the placebo group; however, this was not statistically significant. This may be accounted for by the reduction in HSP following HA injections, which would lead to improved upper extremity function and mobility, as the patient would no longer be limited by pain. Nonetheless, we considered that conventional rehabilitation might have also played a major role in the recovery of upper extremity motor function in the subacute stage after stroke.
The limitations of this study included the following. First, a small sample size of patients with stroke was obtained from only 1 source: a rehabilitation unit at a single medical center. Second, the details of the physical modalities used for HSP pain management were not recorded in this study. Third, we did not include a more extensive follow-up period in our study protocol for patients with stroke who received HA injections; long-term observation of structural changes in the rotator cuff muscles is needed. In the future, multicenter studies with a long-term follow-up period should be performed to explore the clinical benefits of subacromial HA injections in the management of hemiplegic shoulders with pain and soft tissue injuries.
5. Conclusions
In summary, HA injections could provide an additive effect for reduction of HSP, and may improve shoulder abduction in subacute stroke patients with HSP and injury.
Acknowledgments
The authors would like to thank Professor Hsuen-Wen Chang for statistical guidance, Dr. Po-Cheng Chen for drawing the figures, and Mr. Chia-Wen Wu for data collection at the Chang Gung Memorial Hospital.
Footnotes
Abbreviations: FMA-UE = Fugl–Meyer assessment for the upper extremity, HA = hyaluronic acid, HSP = hemiplegic shoulder pain, MAS = modified Ashworth scale, VAS = visual analog scale.
Funding: This study was supported by grants from Chang Gung Memorial Hospital (CMRPG8C0771).
The authors have no conflicts of interest to disclose.
References
- [1].Najenson T, Yacubovich E, Pikielni SS. Rotator cuff injury in shoulder joints of hemiplegic patients. Scand J Rehabil Med 1971;3:131–7. [PubMed] [Google Scholar]
- [2].Wanklyn P, Forster A, Young J. Hemiplegic shoulder pain (HSP): natural history and investigation of associated features. Disabil Rehabil 1996;18:497–501. [DOI] [PubMed] [Google Scholar]
- [3].Lindgren I, Jonsson AC, Norrving B, et al. Shoulder pain after stroke: a prospective population-based study. Stroke 2007;38:343–8. [DOI] [PubMed] [Google Scholar]
- [4].Huang YC, Liang PJ, Pong YP, et al. Physical findings and sonography of hemiplegic shoulder in patients after acute stroke during rehabilitation. J Rehabil Med 2010;42:21–6. [DOI] [PubMed] [Google Scholar]
- [5].Gamble GE, Barberan E, Bowsher D, et al. Post stroke shoulder pain: more common than previously realized. Eur J Pain 2000;4:313–5. [DOI] [PubMed] [Google Scholar]
- [6].Chae J, Mascarenhas D, Yu DT, et al. Poststroke shoulder pain: its relationship to motor impairment, activity limitation, and quality of life. Arch Phys Med Rehabil 2007;88:298–301. [DOI] [PubMed] [Google Scholar]
- [7].Gilmore PE, Spaulding SJ, Vandervoort AA. Hemiplegic shoulder pain: implications for occupational therapy treatment. Can J Occup Ther 2004;71:36–46. [DOI] [PubMed] [Google Scholar]
- [8].Chae J, Yu DT, Walker ME, et al. Intramuscular electrical stimulation for hemiplegic shoulder pain: a 12-month follow-up of a multiple-center, randomized clinical trial. Am J Phys Med Rehabil 2005;84:832–42. [DOI] [PubMed] [Google Scholar]
- [9].Chantraine A, Baribeault A, Uebelhart D, et al. Shoulder pain and dysfunction in hemiplegia: effects of functional electrical stimulation. Arch Phys Med Rehabil 1999;80:328–31. [DOI] [PubMed] [Google Scholar]
- [10].Penning LI, de Bie RA, Walenkamp GH. The effectiveness of injections of hyaluronic acid or corticosteroid in patients with subacromial impingement: a three-arm randomised controlled trial. J Bone Joint Surg Br 2012;94:1246–52. [DOI] [PubMed] [Google Scholar]
- [11].Ada L, Foongchomcheay A. Efficacy of electrical stimulation in preventing or reducing subluxation of the shoulder after stroke: a meta-analysis. Aust J Physiother 2002;48:257–67. [DOI] [PubMed] [Google Scholar]
- [12].Lim JY, Koh JH, Paik NJ. Intramuscular botulinum toxin-A reduces hemiplegic shoulder pain: a randomized, double-blind, comparative study versus intraarticular triamcinolone acetonide. Stroke 2008;39:126–31. [DOI] [PubMed] [Google Scholar]
- [13].Lakse E, Gunduz B, Erhan B, et al. The effect of local injections in hemiplegic shoulder pain: a prospective, randomized, controlled study. Am J Phys Med Rehabil 2009;88:805–11. quiz 804–812, 851. [DOI] [PubMed] [Google Scholar]
- [14].Koog YH, Jin SS, Yoon K, et al. Interventions for hemiplegic shoulder pain: systematic review of randomised controlled trials. Disabil Rehabil 2010;32:282–91. [DOI] [PubMed] [Google Scholar]
- [15].Poduri KR. Shoulder pain in stroke patients and its effects on rehabilitation. J Stroke Cerebrovasc Dis 1993;3:261–6. [DOI] [PubMed] [Google Scholar]
- [16].Turner-Stokes L, Jackson D. Shoulder pain after stroke: a review of the evidence base to inform the development of an integrated care pathway. Clin Rehabil 2002;16:276–98. [DOI] [PubMed] [Google Scholar]
- [17].Shibata Y, Midorikawa K, Emoto G, et al. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. J Bone Joint Surg Am 2001;10:209–16. [DOI] [PubMed] [Google Scholar]
- [18].Chou WY, Ko JY, Wang FS, et al. Effect of sodium hyaluronate treatment on rotator cuff lesions without complete tears: a randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am 2010;19:557–63. [DOI] [PubMed] [Google Scholar]
- [19].Merolla G, Bianchi P, Porcellini G. Ultrasound-guided subacromial injections of sodium hyaluronate for the management of rotator cuff tendinopathy: a prospective comparative study with rehabilitation therapy. Musculoskelet Surg 2013;97suppl 1:49–56. [DOI] [PubMed] [Google Scholar]
- [20].Halpern AA, Horowitz BG, Nagel DA. Tendon ruptures associated with corticosteroid therapy. West J Med 1977;127:378–82. [PMC free article] [PubMed] [Google Scholar]
- [21].Meloni F, Milia F, Cavazzuti M, et al. Clinical evaluation of sodium hyaluronate in the treatment of patients with sopraspinatus tendinosis under echographic guide: experimental study of periarticular injections. Eur J Radiol 2008;68:170–3. [DOI] [PubMed] [Google Scholar]
- [22].Moghtaderi A, Sajadiyeh S, Khosrawi S, et al. Effect of subacromial sodium hyaluronate injection on rotator cuff disease: a double-blind placebo-controlled clinical trial. Adv Biomed Res 2013;2:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 1987;67:206–7. [DOI] [PubMed] [Google Scholar]
- [24].Ashworth B. Preliminary trial of carisoprodol in multiple sclerosis. Practitioner 1964;192:540–2. [PubMed] [Google Scholar]
- [25].Fugl-Meyer AR, Jaasko L, Leyman I, et al. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med 1975;7:13–31. [PubMed] [Google Scholar]
- [26].Mitsui Y, Gotoh M, Nakama K, et al. Hyaluronic acid inhibits mRNA expression of proinflammatory cytokines and cyclooxygenase-2/prostaglandin E(2) production via CD44 in interleukin-1-stimulated subacromial synovial fibroblasts from patients with rotator cuff disease. J Orthop Res 2008;26:1032–7. [DOI] [PubMed] [Google Scholar]


